Abstract
Purpose
To explore the associations between central anterior chamber depth (CACD) and other anterior segment biometric parameters and to determine the possible determinants of CACD in short, normal, and long eyes.
Methods
The biometric data of pre-operation patients aged 50–80 years with coexisting cataract and primary angle-closure disease or senile cataract were reviewed. Axial length (AL), CACD, lens thickness (LT), central corneal thickness (CCT), and white-to-white distance (WTW) were measured by Lenstar optical biometry (Lenstar 900). The data of 100 normal eyes (AL = 22 to 26 mm), 100 short eyes (AL ≤ 22 mm), and 100 long eyes (AL ≥ 26 mm) were consecutively collected for subsequent analyses.
Results
The mean age of the subjects was 66.60 ± 7.85 years, with 25.7% of the sample being men. Both CACD and WTW were found to be smallest in short eyes and were smaller in normal eyes than in long eyes (F = 126.524, P < 0.001; F = 28.458, P < 0.001). The mean LT was significantly thicker in short eyes than in normal and long eyes (4.66 mm versus 4.49 mm versus 4.40 mm; F = 18.099, P < 0.001). No significant differences were observed in CCT between the three AL groups (F = 2.135, P = 0.120). Stepwise regression analysis highlighted AL, LT, and WTW as three independent factors associated with CACD in the normal AL group. In the short AL group and long AL group, LT and WTW were independent factors associated with CACD.
Conclusions
CACD increases as AL elongates and reaches a peak when AL exceeds 26 mm. Furthermore, CACD showed inverse correlation with LT and positive correlation with WTW. A relatively small WTW results in an anteriorly positioned lens, and thus, a decrease in CACD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary angle-closure glaucoma (PACG) affects approximately 26% of the glaucoma population worldwide, but accounts for half of all glaucoma-related blindness [1]. The central anterior chamber depth (CACD) is a basic ocular anatomical parameter that is a major variable for PACG; specifically, a shallow anterior chamber has been proposed as one of the main anatomical features of PACG [2]. Therefore, determining the potential relationship between CACD and other ocular parameters could further the current level of understanding regarding the underlying mechanism behind shallow anterior chamber, and thus, contribute to the development of a more effective method of prevention or treatment for PACG.
Lowe reported that growth and thickening of the lens are associated with a shallowing of the anterior chamber by approximately 0.35–0.50 mm over a 50-year period [3], but the decrease in CACD cannot be fully explained by this age-related increase in lens thickness (LT) [4]. Instead, previous studies have suggested that forward movement of the lens leads to shallowing of the anterior chamber [5,6,7]. Our theory of “trans-lens pressure differential and relative cilio-lenticular block” [8] suggests that a pressure differential between the posterior and anterior lens surfaces causes the forward movement of the lens. Specifically, as the available cilio-lenticular space becomes smaller, the resistance of ciliary flow will increase, thereby limiting the flow of aqueous humor from the posterior to the anterior of the lens. This promotes forward movement of the lens and causes shallow anterior chamber. White-to-white distance (WTW) refers to the corneal diameter. A relatively small WTW may imply minimal space between the ciliary processes and the lens equator. Positive correlation between the WTW and CACD would partially verify our theory of “trans-lens pressure differential and relative cilio-lenticular block” [8].
Previous studies have also identified a significant positive correlation between the axial length (AL) and CACD [9,10,11]. However, Hosny et al. found this correlation to be weaker in patients with an increasingly high AL [12]. It was also confirmed by Hoffmann et al. that the strong statistical correlation between the AL and CACD in normal eyes did not apply to long eyes or short eyes [13]. The ocular determinants of CACD are not yet comprehensively known, and it is possible that they may vary depending on AL ranges. Therefore, this study aimed to explore the associations between CACD and each ocular parameter, as well as to further assess the possible determinants of CACD in short, normal, and long eyes in terms of AL.
Methods
Ethical approval
This study adhered to the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of the Wenzhou Medical University prior to study commencement (Number: 2021-101-K-85).
Data collection
Data were obtained from the Eye Hospital of Wenzhou Medical University; this biometric data pertained to pre-operation patients aged 50–80 years with coexisting cataract and primary angle-closure disease (PACD) or senile cataract. Patients that had corneal opacity, any previous ocular disease (except PACD), or history of ocular surgery were excluded from the sample. Biometry measurements were taken by Lenstar optical biometry (Lenstar 900) which is based on low-coherence reflectometry, with an 820-mm superluminescent diode. A minimum of three stable tests were obtained, and the readings of AL, CACD, LT, central corneal thickness (CCT), and WTW were recorded. Data duplication was avoided by randomly selecting only one eye from each patient to be included in the sample. Eyes were then categorized based on the Lenstar AL values into either the normal group (AL = 22 to 26 mm), short eye group (AL ≤ 22 mm), or long eye group (AL ≥ 26 mm). Data were collected from 100 normal eyes, 100 short eyes, and 100 long eyes.
Statistical analysis
SPSS software (version 22.0, SPSS Inc., Chicago, IL, USA) was used to perform statistical analyses. Continuous variables were described as the mean and standard deviation (SD). ANOVA or independent student t test was used for comparisons between groups; Chi-square test was conducted for categorical variables; Pearson’s correlation and stepwise linear regression were performed to analyze the effects of correlated factors on CACD. P < 0.05 was considered as statistically significant.
Results
Of the 300 eyes from 300 participants, 77 (25.7%) were men. The mean age of the sample was 66.60 ± 7.85 years. The demographic and biometric parameters of each experimental group are shown in Table 1. The long AL subjects were generally the youngest (63.83 ± 8.30 years) relative to the short AL subjects (67.86 ± 6.97 years) and the normal AL subjects (68.12 ± 7.54 years) (F = 9.968, P < 0.001). Furthermore, there were proportionately more women in the short AL group (94.0%). In terms of the anterior segment biometric parameters, the smallest CACD and WTW values were found in the short AL group and were smaller in the normal AL group than in the long AL group (F = 126.524, P < 0.001; F = 28.458, P < 0.001). The proportion of eyes with a deep anterior chamber (CACD ≥ 2.5 mm) was 10, 49, and 83% in the short AL, normal AL, and long AL groups, respectively. The mean LT was significantly thicker in the short AL group than in the normal and long AL groups (4.66 mm vs. 4.49 mm vs. 4.40 mm; F = 18.099, P < 0.001). However, no significant differences were found between the CCT values of the three AL groups (F = 2.135, P = 0.120).
Pearson’s correlation and stepwise linear regression results of CACD and the other biometric parameters are presented in Table 2. CACD was shown to be positively correlated with AL and WTW (r = 0.628, P < 0.001; r = 0.493, P < 0.001) but was negatively correlated with age, gender, and LT (r = −0.223, P < 0.001; r = −0.219, P < 0.001; r = −0.676, P < 0.001). No significant correlation was found between CACD and CCT (r = −0.014, P = 0.803). The multivariate analysis showed AL, LT, and WTW to be independent factors associated with CACD, based on the following equation: CACD = 0.837 + 0.064*AL + 0.257*WTW-0.642*LT, which accounted for 74.4% of variability.
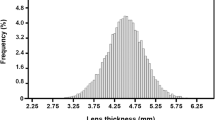
Figure 1 presents the influence of AL on the relationship between CACD and the other biometric parameters. Notably, no significant correlation was found between AL and CACD in long eyes (r = 0.002, P = 0.983); in contrast, positive correlations were found between AL and CACD in short eyes (r = 0.280, P = 0.005) and normal eyes (r = 0.419, P < 0.001). Subsequent stepwise regression analysis showed AL, LT, and WTW to be independent factors associated with CACD in the normal AL group, based on the following equation: CACD = 0.272 + 0.117*AL + 0.174*WTW-0.570*LT. In the short AL and long AL groups, LT and WTW were found to be independent factors associated with CACD, based on the following equations: CACD = 1.497 + 0.311*WTW−0.628*LT and CACD = 2.573 + 0.247*WTW−0.589*LT, respectively.
In the long AL group, 83 eyes had a deep anterior chamber (CACD ≥ 2.5 mm), which coincided with a thinner mean LT and larger mean WTW compared with normal CACD eyes (t = 5.367, P < 0.001; F = −2.884, P < 0.001). No significant differences were found in CCT and AL values between different CACD groups (t = −0.726, P = 0.469; t = 0.648, P = 0.518) (Table 3).
Discussion
It has previously been evidenced that in the eyes of people affected by primary angle closure (PAC), they had a significantly shallower CACD, thicker lens, and shorter AL compared with normal eyes [14, 15]. However, CACD is regarded as the key parameter associated with PACG. A study by Lowe indicated that the CACD threshold for risk of PACG was 2.5 mm, and PACG became rarity when CACD above this level [3]. In the current study, 82% of short eyes, 51% of normal eyes, and 17% of long eyes fit into this “at risk” category; this implies an increasing risk of angle closure from long eyes to normal eyes to short eyes. Although positive correlation between AL and CACD has previously been reported [9,10,11], studies by Sedaghat et al. and Hoffmann et al. specifically detected this relationship in normal eyes but found its absence in short and long eyes [13, 16]. As such, this study supposes that the CACD is determined by anterior segment biometric parameters, but that these factors may vary in different AL groups. To verify this hypothesis, the associations between CACD and these anterior segment biometric parameters were analyzed in different AL groups, which were based on Lenstar measurements of pre-operation patients aged 50–80 years.
The long AL patients were slightly younger than the other two groups, which corroborates the observed pattern of longer ALs in younger people [17, 18]. It can also be explained by the phenomenon that high myopia with increased AL predisposes to the development of cataract at a younger age [19]. In agreement with previous researches [9, 20]. CACD was found to be negatively correlated with age in the current subjects. After controlling for other factors in the multivariate analysis, it was established that age is not associated independently with CACD, thereby indicating a cohort effect as a result of the anterior segment biometric parameters. Overall, the observed age trend in CACD is most likely due to an age-related increase in LT [9, 21]. As presented in earlier studies, women are three times more likely to develop PAC than men [22, 23]; women having a shallower CACD [24, 25] may be the anatomical basis for this. However, this study found the association between gender and CACD to be statistically insignificant after adjustment for LT, AL, and WTW. We propose that the observed gender difference in CACD was likely confounded by anatomical variations in the anterior segment [11, 26].
The mean value of LT measured by Lenstar 900 in the pre-operation cataractous eyes was 4.55 ± 0.45 mm, which was akin to that of Chinese age-related cataract patients measured by the IOLMaster 700 (4.51 ± 0.46 mm [21], 4.51 ± 0.44mm [18]). This study has identified LT as a strong determinant of CACD [21], whereby a thicker LT correlated with a shallower CACD, which persisted after adjustment for the impact of AL.
We found the average WTW to be 11.43 ± 0.52 mm, which was smaller than that of subjects in previous studies, including young Chinese myopic adults aged 18–40 years (WTW = 11.65 ± 0.38 mm) [27], Chinese cataract patients aged 30–99 years (WTW = 11.69 ± 0.46 mm) [28], and normal Indian subjects aged 40–64 years (WTW = 11.79 ± 0.67 mm) [26]. Larger WTW measurements at younger ages [29] may partially explain this variance between studies. Also, the measurement methods and devices used in the studies may have affected the level of agreement between their findings. Nonetheless, the positive relationship between AL and WTW remained consistent across prior studies [28, 29]. In the current study, the long AL group presented the largest WTW (11.67 ± 0.50 mm), while the short AL group (11.43 ± 0.55 mm) had the shortest WTW; these findings agreed with the aforementioned research. Of note, a large WTW is possibly linked to the development of larger anterior segments [21]. In our study, WTW was shown to be positively correlated with CACD, which corroborated previous reports [12, 27, 28, 30]. Singh et al. suggested that a smaller WTW in women relative to men may be of significance, as women are more likely to experience angle-closure glaucoma [26].
Consistent with previous reports [9,10,11], a significant decrease in CACD was observed with a decrease in AL in all 300 eyes. However, this positive correlation was weaker in short eyes and statistically insignificant in long eyes. Moreover, an increase in CACD occurred only with an elongation of AL within a certain range (AL: 22–26 mm, r = 0.419, P < 0.001). An AL value greater than 26 mm resulted in noncorrelation between the two variables [13]. As an important indicator of eye size, AL was measured as the sum of CCT, CACD, LT, and vitreous chamber depth (VCD). The human eyeball increases in size with age, thus resulting in the elongation of AL and WTW. Previous work has also confirmed the contribution of CACD and VCD to AL [31]. It is speculated that CACD may reach a peak when AL achieves a certain size (possibly 26 mm) [28] and anterior segment changes insignificantly as the AL increases. This proposed explanation is supported by the finding that VCD occupies more of the eye with increasing AL [31]. It should also be noted that both an increase in LT and a slight forward movement of the lens center with aging can result in a decrease in CACD [5,6,7]. The current study has proven the link between greater LT and shallower CACD, in corroboration with previous studies [21, 32]. A thin LT may be why children rarely develop PACG even with a short AL [33]. We hypothesize that the age-related change in the lens equator and a relatively small WTW are the primary anatomical reasoning for forward movement of the lens [8]. When the anterior ocular structures are positioned normally, the low resistance to flow from the retrolenticular space to the anterior side of the lens is barely detectable with the current instruments [34]. When there is no resistance between the posterior chamber and retrolenticular space, the posterior-anterior pressure differential on the surface of the lens is minimal [35], and as such, the lens remains in a neutral position. However, potential shrinkage of the available space between the ciliary processes and the lens equator causes an increase in the resistance to ciliary flow, resulting in a relative cilio-lenticular block. This mechanism is analogous to pupillary block and restricts the flow of aqueous humor from the posterior to the anterior of the lens. Resultantly, the posterior lens pressure increases relative to the anterior lens pressure and provokes forward movement of the lens, and causes shallow anterior chamber. It is possible that a relatively small WTW is the underlying reason for 0.05% of people with high myopia developing PAC [36].
Conclusion
Our findings have confirmed the conclusions of previous studies stating that older age, women, shorter AL, shorter WTW, and thicker lens are risk factors for shallower CACD. [3, 9,10,11,12]. While causal relationships have not been fully established in this cross-sectional study, we considered different ALs to conclude the determinants of CACD, as follows: (1) AL is the basis of CACD, whereby CACD increases with the elongation of AL and attains a peak when AL exceeds 26 mm; (2) thick LT directly decreases CACD; and (3) WTW is an indirect factor of CACD, as a relatively small WTW causes an anteriorly positioned lens, which decreases CACD.
References
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90(3):262–267. https://doi.org/10.1136/bjo.2005.081224
Xu L, Cao WF, Wang YX, Chen CX, Jonas JB (2008) Anterior chamber depth and chamber angle and their associations with ocular and general parameters: the Beijing Eye Study. Am J Ophthalmol 145(5):929–936. https://doi.org/10.1016/j.ajo.2008.01.004
Lowe RF (1969) Causes of shallow anterior chamber in primary angle-closure glaucoma. Ultrasonic biometry of normal and angle-closure glaucoma eyes. Am J Ophthalmol 67(1):87–93. https://doi.org/10.1016/0002-9394(69)90012-9
Lowe RF (1970) Anterior lens displacement with age. Br J Ophthalmol 54(2):117–121. https://doi.org/10.1136/bjo.54.2.117
Peng X, Liang Y (2015) The influence of lens in the pathogenesis of primary angle closure glaucoma. Int Rev Ophthalmol 39(6):372–375. https://doi.org/10.3760/cma.j.issn.1673-5803.2015.06.003
Lowe RF (1970) Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol 54(3):161–169. https://doi.org/10.1136/bjo.54.3.161
Jonas JB, Iribarren R, Nangia V, Sinha A, Pardhi P, Shukla R, Panda-Jonas S (2015) Lens position and age: the Central India eye and medical study. Invest Ophthalmol Vis Sci 56(9):5309–5314. https://doi.org/10.1167/iovs.15-16796
Liang Y, Lin H, Zhang S, Liu C, Xu S, Le R, Xie Y, Li G (2021) Trans-lens pressure difference and ciliary block——a new concept for the mechanism of angle closure glaucoma. Chin J Ophthalmol 30(2):89–96. https://doi.org/10.13281/j.cnki.issn.1004-4469.2021.02.003
Chen H, Lin H, Lin Z, Chen J, Chen W (2016) Distribution of axial length, anterior chamber depth, and corneal curvature in an aged population in South China. BMC Ophthalmol 16(1):47. https://doi.org/10.1186/s12886-016-0221-5
Pärssinen O, Kauppinen M, Kaprio J, Koskenvuo M, Rantanen T (2015) Heritability of anterior chamber depth and axial length: a population-based twin study among 66 to 79-year old female twins. Acta Ophthalmol 93(2):e177–e178. https://doi.org/10.1111/aos.12511
Sng CC, Foo LL, Cheng CY, Allen JC Jr, He M, Krishnaswamy G, Nongpiur ME, Friedman DS, Wong TY, Aung T (2012) Determinants of anterior chamber depth: the Singapore Chinese Eye Study. Ophthalmology 119(6):1143–1150. https://doi.org/10.1016/j.ophtha.2012.01.011
Hosny M, Alio JL, Claramonte P, Attia WH, Perez-Santonja JJ (2000) Relationship between anterior chamber depth, refractive state, corneal diameter, and axial length. J Refract Surg 16(3):336–340
Hoffmann PC, Hütz WW (2010) Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg 36(9):1479–1485. https://doi.org/10.1016/j.jcrs.2010.02.025
Wang Z, Chung C, Lin J, Xu J, Huang J (2016) Quantitative measurements of the ciliary body in eyes with acute primary-angle closure. Invest Ophthalmol Vis Sci 57(7):3299–3305. https://doi.org/10.1167/iovs.16-19558
Niu WR, Dong CQ, Zhang X, Feng YF, Yuan F (2018) Ocular biometric characteristics of Chinese with history of acute angle closure. J Ophthalmol 2018:5835791. https://doi.org/10.1155/2018/5835791
Sedaghat MR, Azimi A, Arasteh P, Tehranian N, Bamdad S (2016) The relationship between anterior chamber depth, axial length and intraocular lens power among candidates for cataract surgery. Electron Phys 8(10):3127–3131. https://doi.org/10.19082/3127
Eysteinsson T, Jonasson F, Arnarsson A, Sasaki H, Sasaki K (2005) Relationships between ocular dimensions and adult stature among participants in the Reykjavik Eye Study. Acta Ophthalmol Scand 83(6):734–738. https://doi.org/10.1111/j.1600-0420.2005.00540.x
Wong TY, Foster PJ, Ng TP, Tielsch JM, Johnson GJ, Seah SK (2001) Variations in ocular biometry in an adult Chinese population in Singapore: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci 42(1):73–80
Jivrajka R, Shammas MC, Boenzi T, Swearingen M, Shammas HJ (2008) Variability of axial length, anterior chamber depth, and lens thickness in the cataractous eye. J Cataract Refract Surg 34(2):289–294. https://doi.org/10.1016/j.jcrs.2007.10.015
Lim LS, Saw SM, Jeganathan VS, Tay WT, Aung T, Tong L, Mitchell P, Wong TY (2010) Distribution and determinants of ocular biometric parameters in an Asian population: the Singapore Malay eye study. Invest Ophthalmol Vis Sci 51(1):103–109. https://doi.org/10.1167/iovs.09-3553
Meng J, Wei L, He W, Qi J, Lu Y, Zhu X (2021) Lens thickness and associated ocular biometric factors among cataract patients in Shanghai. Eye Vis (Lond) 8(1):22. https://doi.org/10.1186/s40662-021-00245-3
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ (1996) Glaucoma in Mongolia. A population-based survey in Hövsgöl province, northern Mongolia. Arch Ophthalmol 114(10):1235–1241. https://doi.org/10.1001/archopht.1996.01100140435011
Foster PJ, Oen FT, Machin D, Ng TP, Devereux JG, Johnson GJ, Khaw PT, Seah SK (2000) The prevalence of glaucoma in Chinese residents of Singapore: a cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol 118(8):1105–1111. https://doi.org/10.1001/archopht.118.8.1105
Jonas JB, Nangia V, Gupta R, Khare A, Sinha A, Agarwal S, Bhate K (2012) Anterior chamber depth and its associations with ocular and general parameters in adults. Clin Exp Ophthalmol 40(6):550–556. https://doi.org/10.1111/j.1442-9071.2011.02748.x
Feng X, Wang Y, Liang J, Xu Y, Ortega-Usobiaga J, Cao D (2021) Analysis of lens thickness distribution based on swept-source optical coherence tomography (SS-OCT). J Ophthalmol 2021:4717996. https://doi.org/10.1155/2021/4717996
Singh K, Gupta S, Moulick PS, Bhargava N, Sati A, Kaur G (2019) Study of distribution of white-to-white corneal diameter and anterior chamber depth in study population obtained with optical biometry using intraocular lens (IOL) master. Med J Armed Forces India 75(4):400–405. https://doi.org/10.1016/j.mjafi.2018.06.001
Xu G, Wu G, Du Z, Zhu S, Guo Y, Yu H, Hu Y (2021) Distribution of white-to-white corneal diameter and anterior chamber depth in chinese myopic patients. Front Med (Lausanne) 8:732719. https://doi.org/10.3389/fmed.2021.732719
Wei L, He W, Meng J, Qian D, Lu Y, Zhu X (2021) Evaluation of the white-to-white distance in 39,986 chinese cataractous eyes. Invest Ophthalmol Vis Sci 62(1):7. https://doi.org/10.1167/iovs.62.1.7
Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Yekta A, Fotouhi A (2015) White-to-white corneal diameter distribution in an adult population. J Curr Ophthalmol 27(1–2):21–24. https://doi.org/10.1016/j.joco.2015.09.001
Hashemi H, KhabazKhoob M, Yazdani K, Mehravaran S, Mohammad K, Fotouhi A (2010) White-to-white corneal diameter in the Tehran Eye Study. Cornea 29(1):9–12. https://doi.org/10.1097/ICO.0b013e3181a9d0a9
Takkar B, Gaur N, Saluja G, Rathi A, Sharma B, Venkatesh P, Kumar A (2019) Evaluation of the vitreous chamber depth: an assessment of correlation with ocular biometrics. Indian J Ophthalmol 67(10):1645–1649. https://doi.org/10.4103/ijo.IJO_56_19
Suwan Y, Jiamsawad S, Tantraworasin A, Geyman L, Supakontanasan W, Teekhasaenee C (2017) Qualitative and quantitative evaluation of acute angle-closure mechanisms. BMC Ophthalmol 17(1):246. https://doi.org/10.1186/s12886-017-0635-8
Shimizu Y, Nakakura S, Nagasawa T, Okamoto A, Tabuchi H, Kiuchi Y (2017) Comparison of the anterior chamber angle structure between children and adults. J aapos 21(1):57–62. https://doi.org/10.1016/j.jaapos.2016.10.005
Grant WM (1963) Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol 69:783–801. https://doi.org/10.1001/archopht.1963.00960040789022
Yang HS, Kim JG, Ko HS, Lee KS, Won HJ (2014) In vivo validation of the new Tonopen AVIA tonometer using manometers placed in the anterior chamber and the vitreous cavity under various vitreous conditions. Curr Eye Res 39(4):370–377. https://doi.org/10.3109/02713683.2013.846387
Barkana Y, Shihadeh W, Oliveira C, Tello C, Liebmann JM, Ritch R (2006) Angle closure in highly myopic eyes. Ophthalmology 113(2):247–254. https://doi.org/10.1016/j.ophtha.2005.10.006
Acknowledgments
Not applicable.
Funding
This work was supported by the Program for Zhejiang Leading Talent of S&T Innovation (2021R52012), and Key Research and Development Projects of Zhejiang Province (2022C03112).
Author information
Authors and Affiliations
Contributions
HL was involved in methodology, software, data analysis, writing-original draft, and writing-reviewing and editing; MZ participated in data analysis and creating findings tables and figures; JL, XZ, and YD helped in data acquisition; YJ was involved in data analysis; XW and YX were involved in writing-reviewing; and YL participated in conceptualization, methodology, writing-reviewing and editing, funding acquisition, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
Haishuang Lin declares that she has no conflict of interest. Mengtian Zhou declares that she has no conflict of interest. Jinxin Li declares that she has no conflict of interest. Xuanli Zheng declares that he has no conflict of interest. Yutong Ding declares that she has no conflict of interest. Yiting Ji declares that she has no conflict of interest. Xiaojie Wang declares that she has no conflict of interest. Yanqian Xie declares that she has no conflict of interest. Yuanbo Liang declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, Hs., Zhou, Mt., Li, Jx. et al. Central anterior chamber depth correlated with white-to-white distance in normal, long, and short eyes. Int Ophthalmol 44, 34 (2024). https://doi.org/10.1007/s10792-024-03014-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03014-y