Abstract
Purpose
To evaluate the efficacy of micropulse transscleral cyclophotocoagulation (MP-TSCPC) considering different characteristics: glaucoma subtypes and lens status.
Methods
A retrospective case-series study was designed to evaluate intraocular pressure (IOP), and the number of IOP-lowering medications, used by glaucoma patients treated with MP-TSCPC between 2016 and 2019. Cases had a follow-up period of 12 months. Achieving an IOP reduction higher than 20%, or the decrease of at least one IOP-lowering medication, was considered a successful outcome. The same population was analyzed by classifying them in two groups as: glaucoma subtypes and lens status. The baseline spherical equivalent (SE) was also calculated for considering association with the achieved IOP.
Results
A total of 86 eyes were included. In most cases, IOP and IOP-lowering medications were decreased with a statistically significant difference (p < 0.0001), and all of them had a successful outcome. The percentage of IOP drop oscillated between 25.9% (open-angle glaucoma sub-group) and 37.5% (pseudoexfoliative glaucoma sub-group), 12 months after surgery. The difference between the groups was not statistically significant (p 0.20 and 0.32 for glaucoma subtypes and lens status, respectively). The Pearson’s coefficient obtained was low for the SE and IOP association, at the 12 -month postoperative mark (− 0.009; p < 0.001).
Conclusions
The MP-TSCPC treatment was successful in decreasing IOP and IOP-lowering medications, in different glaucoma subtypes. Differences between groups (glaucoma subtypes, phakic and pseudophakic eyes) were not statistically significant. No association was found between the SE and the IOP achieved value after MS-TSCPC treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The options for treating patients with glaucoma are growing. Beyond traditional eye drops, trabeculoplasty, and surgery, there are new medical therapies [1,2,3] and more surgical options that are coming along mostly through minimally invasive glaucoma techniques and devices [3,4,5]. All of these treatments have a common objective, which is to decrease intraocular pressure (IOP) through different mechanisms. An effective technique to decrease IOP is by “transscleral diode laser cyclophotocoagulation (TSCPC), which is specifically recommended for refractory glaucoma, but has several side effects [6, 7]. To avoid this, a new technique called “micropulse transscleral cyclophotocoagulation (MP-TSCPC) was developed. It consists of a micropulse laser energy delivered to the ocular tissue for a short period of time [8]. This is a cyclodestructive technique, which minimizes ocular tissue thermal damage, and seems to be a safe and effective IOP-lowering procedure [9,10,11,12,13].
The scientific evidence shows that MP-TSCPC can be useful, not only in decreasing IOP and lowering IOP medication for refractory glaucoma, but also for different glaucoma subtypes [14, 15]. However, some aspects regarding its efficacy in treating different ocular conditions remain unclear. The purpose of this study was to evaluate the success rate MP-TSCPC had in decreasing IOP and the number of IOP-lowering medications that were used, considering cases with different characteristics, regarding glaucoma subtypes, and lens status, as phakic or pseudophakic.
Methods
Study design
A retrospective case-series study was designed to evaluate the clinical outcomes in glaucoma patients treated with MP-TSCPC using the equipment “MicroPulse P3 probe, Iridex® Cyclo G6 laser system, Mountain View, U.S.A. (Cyclo G6), between October, 2016, and May, 2019. The study was conducted following the Helsinki tenets in a private clinic in Buenos Aires (Centro de Ojos Quilmes), Argentina, after the Institutional Review Board approved the study protocol. All participants gave their informed consent.
Participants, parameters, and procedures
The participants’ electronical clinical records were reviewed. In order to be included, patients had to be at least 18 years old, with a confirmed diagnosis of glaucoma, who were unable to reach the target IOP with the maximum topical treatment, or with a topical intolerance to the treatment, or patients whose previous glaucoma surgical procedures (trabeculectomy or non-penetrating deep sclerectomy) had failed. Cases of neovascular, congenital and/or traumatic glaucoma, and patients who failed scheduled follow-up visits or had a follow-up of less than 12-months were excluded.
In order to evaluate efficacy, two main outcomes were considered: IOP (measured by Goldman tonometry: three consecutive times and average was registered) and the number of IOP-lowering medications used in every case. To evaluate whether the treatment was successful or not, at least one of the following goals had to be achieved: an IOP reduction higher than 20% compared to the baseline, or a decrease of one or more IOP-lowering medications with stable target IOP. The IOP reduction was calculated in mm Hg, and also as a percentage of the IOP change compared to the baseline during the follow-up. The need for a complementary systemic treatment with acetazolamide to get the IOP target was also considered as a secondary outcome. Acetazolamide was preoperatively used (at least since 3 months) by patients with maximum topical treatment, who cannot achieve the IOP target. If IOP decreases after MPTSCP treatment, this was the first complementary medication to be suspended. The parameters were a preoperative baseline IOP, and then at 24 h, 3 months, 6 months, and 12 months months after surgery. If IOP was not completely controlled after the MP-TSCPC procedure, even with the addition of a topical or systemic treatment, cases were excluded from the study and went to glaucoma surgery (trabeculectomy or aqueous drainage device). This became another aspect to be reviewed. Considering that IOP target in each case can be different, for the present study, we have considered of obtaining at least one of the both efficacy outcomes. If not, topical and/or systemic complementary medications were maintained or added.
We also evaluated baseline SE refraction. Refractive errors were measured under cycloplegic conditions with an auto-refractor-keratometer (ACCUREF K-900;Shin-Nippon), and a correlation test was used to evaluate the association with IOP values. For pseudophakic eyes, SE was calculated with the cycloplegic refractive values that were registered before the patients underwent cataract surgery. For patients with a history of corneal refractive surgery, preoperative SE values were considered. The appearance of any intraoperative or postoperative MP-TSCPC complications was also analyzed. Therefore, any surgical complication was registered, and postoperative slit-lamp evaluation was performed in order to detect complications in the anterior segment, as well as complications at the ocular fundus (anterior chamber reaction, corneal disease, cystoid macular edema, choroidal detachment, or other ocular).
To evaluate the results, the data obtained from the overall population study were processed together, and cases were sorted in two different groups to be analyzed separately accordingly to glaucoma subtype (group A) and lens status (group B). For group A (gA), cases were classified in four sub-groups: gA1: narrow-angle glaucoma; gA2: pseudoexfoliative glaucoma; gA3: open-angle glaucoma; and gA4: cases with previous glaucoma surgical. For group B (gB), cases were classified according to lens status, either pseudophakic (gB1) or phakic (gB2). Narrow-angle glaucoma were cases with a gradual or partial closure of the drainage angle (also defined as defined as chronic narrow-angle glaucoma). The main outcomes were analyzed and compared to overall eyes, and to the two different groups, at baseline and 12 months after treatment.
Characteristics about the surgical procedure and postoperative management
The MP-TSCPC treatments were performed by two surgeons (VZ and CL) using the same standardized procedure. Patients received 1 mg of lorazepam and 10 mg of ketorolac sublingual as preoperative treatment. Procedures were performed in the surgical room, under monitored general anesthesia with sevoflurane and ocular topical gel of lidocaine 2%, which facilitates the probe movement. A P3 probe was used, with an infrared wavelength of 810 nm, with an action cycle of 31.33% and 2000 mW of power, programmed with cycles of 0.5 ms, and 1.1 ms of on/off. The total time of treatment was 180 s. The P3 probe is for single use, and the optic fiber can indent the eye and work at 3 mm from the limbus, over the pars plana. It was sliced slowly (for about 10–15 s) perpendicular to the ocular surface, between the “3 and 9 o’clock globe position,” between 70 and 90 s by hemispheres, without touching the 3 and 9 o’clock areas, to avoid affecting the neuro-vascular ciliary innervation. A strabismus hook (like the Jameson hook) was used to expose the surface to obtain the adequate position for the probe, without the aid of the blepharostats. Finally, for postoperative treatments, prednisolone acetate 1% was indicated every 4 h during the first week, and then every 8 h, for up to 2 weeks. Meanwhile, the IOP-lowering medication used by patients was gradually suspended, according to their evolution.
Descriptive statistical results were presented as mean, standard deviation, and range. Data normality was checked using the Kolmogorov–Smirnov test. To compare differences between means at different time points, analysis of variance (ANOVA) single factor was used. A statistically significant result was considered with a p-value of less than 0.05. To evaluate the associations between IOP and SE, a Pearson’s correlation test was used, for all eyes together and also evaluating separately phakic and pseudophakic eyes. A statistical analysis was performed with the XLMiner Analysis ToolPak software (Frontline Systems Inc.). Data were registered at “Centro de Ojos Quilmes” and are available upon request to the corresponding author.
Results
A total of 86 eyes from 75 patients (a 43/32 female/male ratio) reached the 12-month follow-up period with no failures to attend previous visits. Initially, electronic medical records of 134 operated eyes had been identified; however, 48 of them missed scheduled visits (attending untimely or missing the third and 6-month follow-ups). Thus, although they were kept under control in our center, having an incomplete data record, they were not included in our final evaluation. The mean age of the overall population study was 69.7 ± 12.3 years old (28–96), and their mean SE values were − 4.0 ± 7.8 D (− 23–2.8). The mean value of the spherical equivalent in the pseudophakic eye group was -5.7 ± 8.4 D (− 23–3) and in the phakic eye group, it was 0.4 ± 1.2 D (− 2–2.25), with a statistically significant difference (p < 0.001). No intraoperative or postoperative complication was found across the study.
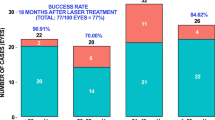
The complete data results of the different groups and sub-groups are shown in Tables 1, 2, presenting the efficacy information (IOP and the number of lowering medications, respectively). Based on results obtained 12 months after treatment (Tables 1, 2), we can see that IOP and IOP-lowering medications decreased with a statistically significant difference (P < 0.001). Successful outcomes were achieved for all groups. Analyzing results separately in the group of glaucoma sub-types (Fig. 1), “pseudoexfoliation glaucoma” cases obtained a higher IOP decrease, whereas “open-angle glaucoma” had a lower IOP decrease, without statistical difference between subgroups at month 12 (p 0.20). This group, however, obtained a higher decrease of IOP-lowering medications (with statistically significant difference; p < 0.001). Considering the group of lens status, results were similar between both phakic and pseudophakic eyes.
In Table 2, the worst value was observed in the “previous glaucoma surgery” sub-group, where the number of IOP-lowering medications was decreased only to 0.8 (25%). Nevertheless, as we can see in Table 1, successful goals were achieved for all proposed groups and sub-groups, as no one failed to reach at least one of the two proposed parameters considered to be successful (a 20% IOP reduction, or the reduction of one IOP-lowering medication). Figures 1, 2 show the “IOP” value obtained at each time point and the statistical comparison between subtypes of glaucoma (Fig. 1) and lens status (Fig. 2). In both figures was observed a statistically significance difference between subtypes of glaucoma and also between eyes regarding their lens status, at two time points: day 1 and month 6. However, at month 12, the differences are no statistically significant. Figures 3, 4 show the “number of lowering IOP medication” for the different groups (glaucoma subtypes and lens status, respectively). Differences observed were without statistical significance, between phakic and pseudophakic eyes. Interestingly, a statistically significant difference was observed at most time points, with a higher effect for eyes with open-angle glaucoma (decreasing 77.4% one year after treatment) and having the weaker effect in eyes with previous surgery, as was previously mentioned. Figure 5 shows the number of eyes that need “acetazolamide” as a systemic complementary medication. It is possible to show how in all the groups it was decreased. Regarding the group of subtypes of glaucoma, it was decreased at 50% in A1 and A2 (narrow-angle glaucoma and pseudo exfoliation glaucoma, respectively). The sub-group of open-angle glaucoma decreased from 5 to 3 eyes, and the sub-groups A4 (previous surgery) decreased from 16 to 4 eyes who needed acetazolamide. However, no difference was found when all the sub-groups were compared (p 0.79). Something similar was observed in Group B (lens status). In both sub-groups (phakic and pseudophakic), decrease in the number of eyes treated with acetazolamide was observed, but the difference between both was not statistically significant (p 0.3). Figure 6 shows the distribution of the total number of cases taking into account the SE and IOP values at 12 months. Regarding the correlation between SE and IOP obtained, the Pearson’s coefficient was very low (− 0.009; p < 0.001). When evaluating the same coefficient considering the state of the crystalline lens, the values were also very low (R2: 0 for pseudophakic and R2: 0.051 for phakic).
Discussion
In the present work, the efficacy of the MP-TSCPC in decreasing IOP and IOP-lowering medications was evaluated in eyes with different conditions, regarding glaucoma subtype and lens status (phakic or pseudophakic). Treatment showed good results for all groups, achieving the goals deemed to be successful.
The action mechanism of MP-TSCPC is still under study, and is possibly multifactorial. IOP reduction can be produced, in part, by increasing the trabecular and the uveoscleral outflow, and by the constriction of ciliary muscles [16]. This is a secondary effect of the shortening of the ciliary muscle, the scleral spur rotation, which produces a trabecular meshwork movement, changing the Schlemm’s canal angle [8, 16]. A more recent experimental study performed in rabbits postulates another complementary mechanism for IOP reduction, by the aqueous humor transport dysfunction due to the non-pigmented epithelial cells of the pars plicata, and the destruction of basal infoldings [17]. Evaluating the efficacy of MP-TSCPC in eyes with different conditions, as was previously mentioned, can be useful to increase the knowledge about the action mechanism of this treatment.
Firstly, the MP-TSCPC was considered only for refractory glaucoma patients, as Tan et al. [8] published in 2010, and was confirmed by the same group, in a study published by Aquino et al. [9]. A recent study was published by de Crom et al. [15], evaluating treatment safety and efficacy even after a 2 year follow-up for different glaucoma subtypes: primary glaucoma, secondary glaucoma, and eyes with prior glaucoma surgery. They also considered lens status (phakic or pseudophakic), and finally concluded the treatment was safe and efficient in reducing IOP and IOP-lowering medications, starting with 141 eyes, and finalizing their study with 50 eyes, 2 years later. Also, our group has a previously published study in which we evaluated results in eyes with different glaucoma subtypes with a follow-up of 12 months [14].
The present work has some similarities with that of de Crom et al.’s study [15]. We have also included eyes with different glaucoma subtypes, such as cases with narrow-angle glaucoma (all of them, have laser peripheral iridotomies previously performed) pseudoexfoliative glaucoma, open-angle glaucoma, and eyes that have undergone prior glaucoma surgery. Eyes were also evaluated according to their lens status. In our study, the goals deemed to be successful were the same ones as de Crom et al. (IOP decreases of at least 20%, or a drop in IOP-lowering medication). We also evaluated the need to use acetazolamide oral therapy as one more additional treatment to control IOP. Moreover, we have analyzed and described our results in a different way: first, the overall eyes (all together); after that, eyes were classified in two groups, with different sub-groups. Interestingly, as a “clinical result,” successful goals were always achieved after a 12-month follow-up. In the present series, we do not have eye that repeated the treatment with MP-TSCPC, which is another difference with the series presented by de Crom et al.
Sarrafpour et al. [18] performed an interesting study, obtaining a very good IOP reduction 1 year after treatment, principally in open-angle glaucoma cases. They have also evaluated visual acuity and four different laser power parameters and they concluded that IOP reduction follows a dose–response pattern related to power used (up to 2500 mW). In our work, we have used 2000 mW for all the cases and we found a percentage of IOP reduction between 15.5 and 41.5%. The lower value was found in the open-glaucoma sub-group, whereas the higher one was found in the pseudoexfoliative glaucoma sub-group. Moreover, IOP-lowering medication also decreased in all groups and sub-groups: the reduction percentage oscillated between 16.1 (in the previous glaucoma surgery sub-group) and 86.6% (in the phakic eyes sub-group). Considering the accuracy of the treatment for overall cases, we observed a good performance in decreasing IOP, as well as in IOP-lowering medications, in all situations. However, we can see that there is one group where the treatment seems to be less effective, which is the open-angle glaucoma group although the mean lowering IOP medication used also resulted in a significant reduction after one year of treatment.
Another way to analyze the present results is evaluating where the treatment seems to be “clinically” more effective. Considering glaucoma subtypes groups, the percentage of IOP reduction observed in the pseudoexfoliative group was very good after one year of follow-up; also, with a higher decrease of IOP-lowering medications. Finally, when we divided cases regarding lens status, we found good results, and very similar for both, and even the best IOP reduction percentages were obtained in the pseudophakic group, the reduction in IOP-lowering medication was equal at the 12-month follow-up mark (1.1 drugs decreased). It is known that cataract extraction has a lowering effect on the intraocular pressure [19]. And recently was published a study that found a greater IOP reduction in patients with glaucoma (principally open-angle glaucoma, narrow angles, and chronic closure angles) [20]. In our work, the presence of the lens (phakic group) or their absence in relation with a history of phacoemulsification has no a differential effect on the efficacy of MP-TSCPC treatment. However, this interesting aspect must be more deeply studied, in a large series with a homogeneous population.
The retrospective design of this work and the disparity in the number of cases achieved in the sub-groups are two limitations of this study. We also do not have strong evidence supporting the claim that the MP-TSCPC treatment is better for some kinds of eyes. A multivariate statistical analysis and a risk factor evaluation will be necessary, but, for that, a different study design must be developed. Nevertheless, the clinical evidence obtained in this work shows that the treatment seems to be more effective in decreasing IOP for the pseudoexfoliative glaucoma in comparison to other glaucoma subtypes. And considering lens status, the MP-TSCPC was effective in both sub-groups (phakic and pseudophakic eyes), with more IOP-lowering effect in the pseudophakic sub-group. However, results presented in this study cannot confirm that. Also, is interesting to remark that even when “pseudoexfoliation glaucoma” cases obtained a higher IOP decrease, whereas “open-angle glaucoma” had a lower IOP decrease, this last group obtained a higher decrease of IOP-lowering medications. Therefore, the less IOP reduction in the open-angle glaucoma group may be related with more lowering medication reduction. To avoid confusion in interpreting the present results, the obtained evidence showed that MP-TSCPC achieved a successful rate in all the glaucoma subtypes but without statistical difference. Also, data from our study highlight that treatment with MP-TSCPC may be useful for different subtypes of glaucoma, in addition to refractory glaucoma.
There is evidence that shows that glaucoma prevalence was associated with refractive state [21]. It is known that myopia is a risk factor for open-angle glaucoma [22,23,24], and hyperopia is a risk factor for primary angle-closure glaucoma as well [24,25,26]. In our work, we wanted to see whether the MP-TSCPC treatment was more or less effective, regarding refractive errors. Therefore, our analysis was aimed at seeing whether there was a potential association between the SE and the IOP obtained after treatment or not. We have statistically demonstrated a lack of correlation, which is an interesting and original aspect of this study. In our study, the SE data of the pseudophakic eyes used were the one they had before cataract surgery, being mainly myopic, and different from the group of phakic eyes, which were predominantly hyperopic. For such reason, we also analyzed each group separately, to evaluate whether or not there was a relationship between the IOP obtained and the SE in these cases, and we also found no relationship. For future investigations, it would be interesting to also evaluate the axial length data, but in our case, it was not possible, due to our retrospective study design and the fact that we did not have these data from phakic eyes.
With regard to the results published by Varikuti et al. [27], MP-TSCPC treatment can be prescribed not only for refractory glaucoma, but also as an alternative to other glaucoma surgeries. Our results concur with this. New protocols are being studied in order to identify what is the most effective and secure form to perform MP-TSCPC treatments, as Vig et al. published [28]. Nevertheless, new studies are exploring the effect of MP-TSCPC in a different types of several cases of glaucoma, as the article published by Laurelle et al. [29]. In that study, the same equipment was used (Cyclo G6) for treating a total of 55 eyes. Most of them had open-angle glaucoma (33 eyes) and interestingly, they also treated primary closed-angle glaucoma, juvenile, inflammatory, secondary open glaucoma, neovascular glaucoma, and 3 eyes of unknown glaucoma. They were followed up for one year. The efficacy outcomes used are the same as were described in the present work which support useful information for clinical practice. We have an open question regarding the potential higher effect of MP-TSCPC in pseudoexfoliative glaucoma, but our hypothesis needs be supported by evidence-based medicine, and for that, another study design must be necessary. Undoubtedly, this is a new option for treating glaucoma patients in a secure manner, and with effective results. We can expect many new studies analyzing its different aspects.
Conclusions
As a conclusion, the present study assessed the efficacy of the MP-TSCPC performed with the Cyclo G6 equipment, describing results in different groups and sub-groups and classifying eyes regarding their glaucoma subtypes and lens status. The percentage of IOP decrease, and of IOP-lowering medications that were used, has been evaluated in order to assess the success of the treatment. Good clinical efficacy was observed, achieving the proposed successful goals in all groups, and obtaining a statistically significant improvement considering IOP reduction, as well as a reduction of IOP-lowering medications, for most cases. Considering glaucoma subtypes, a greater effect was observed in the pseudoexfoliative glaucoma group, but without a statistically significant difference compared to the others. In the present series, baseline SE, with the IOP reduction obtained 12 months after the MP-TSCPC treatment, could not be associated. Similar efficacy was found between phakic and pseudophakic eyes. Complications did not occur intra- or post-operatively. More studies are needed to discover whether this kind of treatment is more efficient for some glaucoma subtypes, or for some specific eye characteristics.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
XLMiner Analysis Toolpak Frontline Systems Inc. was used. It is a free software to perform statistical analysis in Google Sheets.
References
Jiang Y, Ondeck (2020) A Review of new medications and future directions of medical therapies in glaucoma. Semin Ophthalmol 35:280–286
Cvenkel B, Kolko M (2020) Current medical therapy and future trends in the management of glaucoma treatment. J Ophthalmol 2020:6138132. https://doi.org/10.1155/2020/6138132
Garg A, Gazzard G (2020) Treatment choices for newly diagnosed primary open angle and ocular hypertension patients. Eye (Lond) 34:60–71
Lee RMH, Bouremel Y, Eames I (2020) Translating minimally invasive glaucoma surgery devices. Clin Transl Sci 13:14–25
Do AT, Parikh H, Panarelli JF (2020) Subconjunctival microinvasive glaucoma surgeries: an update on the Xen gel stent and the PreserFlo MicroShunt. Curr Opin Ophthalmol 31:132–138
Mistlberger A, Liebmann JM, Tschiderer H, Ritch R, Ruckhofer J, Grabner G (2001) Diode laser transscleral cyclophotocoagulation for refractory glaucoma. J Glaucoma 10:288–293. https://doi.org/10.1097/00061198-200108000-00008
Ishida K (2013) Update on results and complications of cyclophotocoagulation. Curr Opin Ophthalmol 24:102–110
Tan AM, Chockalingam M, Aquino MC, Lim ZI, See JL, Chew PT (2010) Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol 38:266–272
Aquino MC, Barton K, Tan AM, Li X, Loon SC, Chew PT (2015) Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophthalmol 43:40–46
Emanuel ME, Grover DS, Fellman RL, Godfrey DG, Smith O, Butler MR et al (2017) Micropulse cyclophotocoagulation: initial results in refractory glaucoma. J Glaucoma 26:726–729
Williams AL, Moster MR, Rahmatnejad K, Resende AF, Horan T, Reynolds M et al (2018) Clinical efficacy and safety profile of micropulse transscleral cyclophotocoagulation in refractory glaucoma. J Glaucoma 27:445–449
Sanchez FG, Lerner F, Sampaolesi J, Noecker R, Becerra N, Iribarren G et al (2018) Efficacy and safety of micropulse® transscleral cyclophotocoagulation in glaucoma. Arch Soc Esp Oftalmol 93:573–579
Zaarour K, Abdelmassih Y, Arej N, Cherfan G, Tomey KF, Khoueir Z (2019) Outcomes of micropulse transscleral cyclophotocoagulation in uncontrolled glaucoma patients. J Glaucoma 28:270–275
Logioco C, Perrone LD, Caruso D, Albertazzi R, Valvecchia G, Zanutigh V (2020) Assessment of efficacy and safety of micropulse diode laser treatment in glaucoma: one year follow-up. Arch Soc Esp Oftalmol 95:327–333
de Crom RMPC, Slangen CGMM, Kujovic-Aleksov S, Webers CAB, Berendschot TTJM, Beckers HJM (2020) Micropulse trans-scleral cyclophotocoagulation in patients With glaucoma: 1 and 2-year treatment outcomes. J Glaucoma 29:794–798
Liu GJ, Mizukawa A, Okisaka S (1994) Mechanism of intraocular pressure decrease after contact transscleral continuous-wave Nd:YAG laser cyclophotocoagulation. Ophthalmic Res 26:65–79
Tsujisawa T, Ishikawa H, Uga S, Asakawa K, Kono Y, Mashimo K et al (2020) Morphological changes and potential mechanisms of intraocular pressure reduction after micropulse transscleral cyclophotocoagulation in rabbits. Ophthalmic Res. https://doi.org/10.1159/000510596
Sarrafpour S, Saleh D, Ayoub S, Radcliffe NM (2019) Micropulse transscleral cyclophotocoagulation: a look at long-term effectiveness and outcomes. Ophthalmol Glaucoma 2:167–171
Masis Solano M, Lin SC (2018) Cataract, phacoemulsification and intraocular pressure: Is the anterior segment anatomy the missing piece of the puzzle? Prog Retin Eye Res 64:77–83. https://doi.org/10.1016/j.preteyeres.2018.01.003
Wang SY, Azad AD, Lin SC, Hernandez-Boussard T, Pershing S (2020) Intraocular pressure changes after cataract surgery in patients with and without glaucoma: an informatics-based approach. Ophthalmol Glaucoma 3(5):343–349. https://doi.org/10.1016/j.ogla.2020.06.002
Grødum K, Heijl A, Bengtsson B (2001) Refractive error and glaucoma. Acta Ophthalmol Scand 79:560–566
Marcus MW, de Vries MM, Junoy Montolio FG, Jansonius NM (2001) Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology 118:1989-1994.e2
Qiu M, Wang SY, Singh K, Lin SC (2013) Association between myopia and glaucoma in the United States population. Invest Ophthalmol Vis Sci 54:830–835
Shen L, Melles RB, Metlapally R, Barcellos L, Schaefer C, Risch N et al (2016) The association of refractive error with glaucoma in a multiethnic population. Ophthalmology 123:92–101
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S (2017) Glaucoma. Lancet 390(10108):2183–2193. https://doi.org/10.1016/S0140-6736(17)31469-1
Wang L, Huang W, Huang S, Zhang J, Guo X, Friedman DS et al (2019) Ten-year incidence of primary angle closure in elderly Chinese: the Liwan Eye Study. Br J Ophthalmol 103:355–360
Varikuti VNV, Shah P, Rai O, Chaves AC, Miranda A, Lim BA et al (2019) Outcomes of micropulse transscleral cyclophotocoagulation in eyes with good central vision. J Glaucoma 28:901–905
Vig N, Ameen S, Bloom P, Crawley L, Normando E, Porteous A et al (2020) Micropulse transscleral cyclophotocoagulation: initial results using a reduced energy protocol in refractory glaucoma. Graefes Arch Clin Exp Ophthalmol 258:1073–1079
Laruelle G, Pourjavan S, Janssens X, Marinescu-George C, Boustani G (2021) Real-life experience of micropulse transscleral cyclophotocoagulation (MP-TSCPC) in advanced and uncontrolled cases of several glaucoma types: a multicentric retrospective study. Int Ophthalmol 41(10):3341–3348. https://doi.org/10.1007/s10792-021-01896-w
Acknowledgments
The authors would like to acknowledge Rodrigo M. Torres M.D. Ph.D. for his scientific advice.
Funding
None; this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by VZ, LDP, GGC, FP, GV, and CL. The first draft of the manuscript was written by VZ and CL, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethical approval
The study was conducted following the Helsinki tenets in a private clinic in Buenos Aires (Centro de Ojos Quilmes), Argentina, after the Institutional Review Board approved the study protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zanutigh, V., Perrone, L.D., Gómez-Caride, G. et al. Success rate in micropulse diode laser treatment with regard to lens status, refractive errors, and glaucoma subtypes. Int Ophthalmol 43, 2407–2417 (2023). https://doi.org/10.1007/s10792-023-02640-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02640-2