Abstract
Purpose
Our aim was to report the characteristics and long-term surgical outcomes of three subgroups of horizontal strabismus in a single institution (divided by strabismus subtype) in a developing country and look into pre-operative factors predictive of surgical success.
Methods
Two hundred and forty-four complete charts of patients, divided into 152 esotropes (ET) and 92 exotropes (XT) who had undergone horizontal strabismus surgeries, were retrospectively reviewed. Charts of patients with muscle palsy, Duane syndrome and consecutive strabismus were excluded; 172 patients were included divided into partially accommodative ET, congenital ET and intermittent XT. Surgical success was defined as a post-operative angle deviation of 12 prism diopters or less.
Results
The mean follow-up period of all patients was 31.64 ± 23.12 months. The subgroups were divided into partially accommodative ET (60 patients), congenital ET (60 patients), and intermittent XT (52 patients). Esotropes (both partially accommodative and congenital) presented earlier (p < 0.001). Also, partially accommodative ET had a significantly higher spherical equivalent (SE) compared to congenital ET patients, who had a higher SE than intermittent XT (p < 0.001). Congenital ET patients had a significantly larger angle of deviation (for both far and near) than both partially accommodative ET and intermittent XT patients (p < 0.001). The overall success rate was 72.67% for the whole group with no significant differences among subgroups. Success rate of partially accommodative ET surgery was 78.33% compared to that of congenital ET at 66.67% and intermittent XT at 73.07%. Significant post-operative improvement in sensory fusion was observed mainly for patients with partially accommodative esotropia and intermittent exotropia.
Conclusion
Our results showed that esotropes (both partially accommodative and congenital) presented earlier, with a higher spherical equivalent in the partially accommodative ET subgroup, while the congenital ET subgroup had the largest angle of deviation for both distance and near. The overall surgical success rate for horizontal strabismus surgery was 72.67% with the 3 subgroups having similar success rates. A younger age at presentation and absence of amblyopia were positively correlated with surgical success in the partially accommodative esotropia group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Strabismus is a frequently encountered ophthalmological condition with a prevalence of 3–5% [1,2,3,4,5]. It can present at any age and can lead to detrimental effects including loss of stereoacuity and binocularity [6]. Additionally, it has several psychosocial sequelae on the affected individual [7]. When the magnitude is significant, management is mostly surgical with bilateral rectus recession or unilateral recession and resection of opposite recti muscles [8].
Studies have reported success rates of horizontal strabismus surgeries varying between 53 and 83% [5, 9,10,11]. One study compared strabismus surgery success rates of attending and resident surgeons and found these values to be 58% and 69% respectively, without any significant differences between the two provider groups [12]. Although in one study, a comparison of the surgical success rates of esotropia and exotropia did not show a significant difference [5], several studies on the individual subtypes of esotropia and exotropia reported more promising outcomes in accommodative and early-surgery infantile esotropia than in intermittent exotropia [13,14,15,16,17,18].
A number of studies have also investigated the factors influencing surgical success. A pre-operative deviation angle of more than 30 prism diopters was associated with a lower chance of surgical success. Additionally, patients below the age of 6 were found to have a better outcome than their older counterparts [5]. Esotropia and the absence of amblyopia were reported to be predictive factors of surgical success [11]. One study linked non-compliance with post-operative prescribed treatments (glasses or atropine/patching) with a poorer surgical outcome [9]. Although ample literature exists on strabismus management, individual reports invariably address a specific subtype reporting its characteristics, surgical treatment and outcomes. Few have reported horizontal strabismus surgery outcomes as one group and compared subgroups.
Our aim in this study was to report the characteristics and long-term surgical outcomes of horizontal strabismus in a single institution (divided by strabismus subtypes) in a developing country and look into pre-operative factors predictive of surgical success.
Methods
Study population
This study was approved by the Institutional Review Board (IRB) at the American University of Beirut Medical Center and abided by the principles of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study. The list of potential patients was gathered using strabismus surgery billing codes. The charts were then screened to exclude patients who had a predominantly vertical component of strabismus or those that presented for nystagmus surgeries (Kestenbaum procedures). Charts with incomplete data or with a follow-up of less than 6 months were likewise excluded. Two hundred and forty-four complete charts of patients who had undergone horizontal strabismus surgeries from January 2007 to January 2020 were reviewed. These were then divided into 92 patients with exotropia (XT) and 152 patients with esotropia (ET). We further excluded patients with Duane syndrome or cranial nerve palsies as well as those presenting with consecutive cases. 172 patients were included divided into subgroups of strabismus: partially accommodative ET (60 patients), congenital ET (60 patients) and intermittent XT (52 patients). Demographic parameters recorded included age, gender, ophthalmological and non-ophthalmological disorders, past surgeries and current medications, number and types of strabismus surgery (bilateral rectus recession vs unilateral recession and/ or resection).
Eye exam
All patients underwent thorough eye examinations pre-and post-operatively. Visit parameters recorded included visual acuity, cycloplegic refraction, slit lamp and fundoscopy examinations, motility exam, stereoacuity, and Worth-4-Dot test results to assess fusion. Visual acuity was tested using “central, steady & maintained” testing for preverbal children and vision charts for verbal children (Allen pictures and Early Treatment Diabetic Retinopathy charts).
Motility examinations were carried out by an orthoptist and then repeated by the attending ophthalmologist. Alternate cover testing was used to measure the maximum angle of deviation (in prism diopters—PD). Fundoscopy and manual retinoscopy were performed after using Mydriacyl 1% and Cyclopentolate 1% (applied twice 10 min apart) to achieve complete cycloplegia. As for stereoacuity, the Titmus stereotest was utilized (Titmus Optical Co, Petersburg, Virginia, USA). Patients who could not see the fly wings or could only see the fly wings at best were marked as having poor (gross) stereopsis (4000 arcsec). Those who could see 1, 2 or 3 animals were marked as having good stereopsis. Worth-4-Dot testing was deployed to assess fusion at distance and near, and results were recorded as: suppression (right or left), fusion and diplopia. Amblyopia was defined as a difference in visual acuity of at least two lines between fellow eyes or a visual acuity less than 20/30 in the affected eye.
Surgeries and outcomes
Patients typically underwent bilateral rectus recession surgeries or unilateral resection and recession surgeries. Surgeries were performed by 3 surgeons using a similar surgical approach, most of the time via a limbal approach unless conjunctival scarring precluded limbal dissection. The rectus muscle was hooked first by a small hook followed by a Jameson hook; a double armed 6–0 Vicryl suture was interwoven in the muscle tendon at 1 mm from its scleral insertion (for recession/ advancement surgery) or in the muscle belly at the resection length (for resection surgery) and double locked on each side. The needles were then taken into partial thickness sclera at the recession site for recession surgery or at the muscle insertion site for resection/ advancement surgery. Conjunctiva was re-approximated using 8–0 Vicryl sutures. Post-operatively, a topical antibiotic and steroid combination was given for 2 weeks. Surgical success was defined as a post-operative deviation of 12 prism diopters or less. Patients were considered “overcorrected” in the case of more than 12 prism diopter reversal of angle of deviation at the end of the follow-up period.
Analysis
Data were entered into SPSS V25 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp., USA). Means and standard deviations were calculated for continuous demographic and eye examination parameters. Means of continuous variables were compared using one-way ANOVA (analysis of variance). Categorical variables were analyzed using Chi square test. Results of stereoacuity and Worth-4-Dot tests were tallied and reported as categorical variables. Additionally, success rates were computed for the whole group after 1, 2 and 3 or more surgeries and for partially accommodative esotropia, congenital esotropia and intermittent exotropia patients separately. To investigate predictive factors of surgical success for each strabismus subgroup, a multivariate logistic regression was conducted with the following independent variables: age, gender, logMAR vision, angle of deviation at distance and at near, fusion at distance and at near, stereoacuity and amblyopia. For all statistical analyses, a p value of 0.05 or less was considered statistically significant.
Results
Two hundred and forty- four patients divided into 152 esotropes and 92 exotropes were included in this study. The exotropia subtypes were intermittent (n = 52), sensory (n = 10), congenital (n = 5) and exotropia due to other conditions such as third cranial nerve palsy (n = 7). Only the intermittent subgroup was included. For esotropia, these were partially accommodative (n = 60) and congenital (n = 60); excluded were patients with Duane syndrome (n = 4) and other less common subtypes including consecutive esotropia and sixth cranial nerve palsy (n = 28). Table 1 represents the demographics of the included patients. The mean age of patients in the partially accommodative ET group was 6.78 ± 8.60 years (1 to 55 years), that of the congenital ET was 4.66 ± 6.44 years (1 to 33 years), while in the intermittent XT group, mean age was 12.14 ± 11.32 years (1 to 59 years). The average age of the entire group was 7.66 ± 9.36 years, with the esotropia group (both partially accommodative and congenital) being significantly younger than the intermittent exotropia group (p < 0.001). The mean follow-up period of all patients was 31.64 ± 23.12 months, without any significant differences between groups. Spherical equivalent differed significantly among groups, with partially accommodative ET patients having a significantly higher spherical equivalent (SE)—that is were more hyperopic—compared to congenital ET, who had a higher SE than intermittent XT (p < 0.001). Angles of deviation were different among the subgroups. Congenital ET patients had a significantly larger angle of deviation (for both far and near) than both partially accommodative ET and intermittent XT patients (who had similar angles) (p < 0.001). The mean distance deviation angle for congenital ET was 39.30 ± 13.89 PD (6 to 85 PD) versus 25.95 ± 10.93 PD (2 to 50 PD) for partially accommodative ET and 25.79 ± 9.48 PD (9 to 50 PD) for intermittent XT (p < 0.001). This also applied to the near angle of deviation: 41.98 ± 14.16 PD (2 to 85 PD) for congenital ET versus 29.63 ± 10.47 PD (2 to 50 PD) for partially accommodative ET and 26.81 ± 9.31 PD (12 to 52 PD) for intermittent XT, (p < 0.001). 16.28% of all participants had amblyopia on presentation with no significant differences between study groups (12 patients in the partially accommodative ET group, 10 in the congenital ET group and 6 in the intermittent XT group). Pre-operative management of amblyopia was done in these patients. The post-operative improvement in visual acuity in the amblyopic eye was not statistically significant (p = 0.505). With regards to stereoacuity at presentation, poor stereoacuity was encountered in accommodative ET and congenital ET with 100% of tested patients with partially accommodative ET and 75% of tested congenital ET patients having only poor stereopsis. This is compared to 27.27% in the intermittent exotropia group with poor stereopsis, with a significant difference mainly between partially accommodative ET and the intermittent XT subgroups (p < 0.001). Of note is that only a small number of patients had a stereoacuity test result in their charts, as many patients were preverbal or uncooperative.
The final post-operative visit parameters are portrayed in Table 2. The same significant difference in the spherical equivalent between the three groups was also seen post-operatively with the partially accommodative esotropia group having a significantly higher hyperopic SE. The post-operative angle of deviation was significantly different between the three groups for distance and near (p = 0.026). The mean distance deviation angle post-operatively for congenital ET was 7.25 ± 9.23 PD versus 3.97 ± 4.81 PD and 6.92 ± 7.49 PD for partially accommodative esotropes and intermittent exotropes, respectively (p = 0.026). This also applied to the near angle of deviation (9.27 ± 9.35 PD for congenital ET versus 5.38 ± 5.82 PD for partially accommodative ET and 6.94 ± 7.92 PD for intermittent XT, p = 0.026). Post-operatively, intermittent exotropia patients had better stereoacuity with 89.65% having good stereopsis compared to only 16.67% and 30% in partially accommodative and congenital esotropes, respectively (p < 0.001).
Table 3 demonstrates the overall post-operative success rates as well as that of the respective subgroups. The overall success rate was 72.67% for the whole group. For the 3 groups, success rates were similar. Among esotropes, the highest success rate was seen in partially accommodative ET with a value of 78.3% (with their refractive correction). This was followed by congenital ET (66.67%). In intermittent XT the success rate was 73.07%. Eleven percent underwent unilateral surgery while 89% underwent bilateral horizontal strabismus surgery. For each subgroup of strabismus, we compared success rates between bilateral and unilateral surgery in a cross table. Success rates were as follows for the specific subgroups: in partially accommodative ET patients, 83.33% of bilateral surgeries done were successful while 33.33% of unilateral surgeries were successful. In congenital ET, 65.52% of bilateral surgeries were successful and 100% of unilateral surgeries were successful. For intermittent XT, 68.29% of bilateral surgeries were successful, while 90.90% of unilateral surgeries were successful. We found out that only for partially accommodative ET, bilateral surgery was significantly more successful than unilateral surgery (p = 0.005). Most patients who achieved surgical success did so after their first surgery. Six patients (3.49%) needed to be re-operated once, and 3 (1.74%) had 3 or more procedures. The proportion of patients who were overcorrected was 9.88%, with no significant difference between the groups (13.33% in congenital ET, vs 11.67% in partially accommodative ET and 3.85% in intermittent XT).
We compared characteristics of patients who achieved surgical success to those that did not. Separate multivariate logistic regression analyses were performed for each of the partially accommodative ET, congenital ET and for intermittent XT between predictor variables (age, gender, vision, deviation angles at far and near, fusion at far and near, stereoacuity and presence of amblyopia) and the binary dependent variable (being surgical success). Our results showed statistical significance (p < 0.05) only in the subgroup of accommodative ET and for the predictors of age and amblyopia. Patients with successful surgeries had an average age of 6 years ± 8, while those with unsuccessful surgery had an average of 9 years ± 11 (p = 0.017). Also, the rate of amblyopia in the successful group was 19.1%, while it was 23.1% in the failure group with a statistically significant difference at p = 0.021. Therefore, a younger and non-amblyopic patient had a higher success rate. All other demographic variables did not differ between the successful and unsuccessful surgery groups in each strabismus subgroup. Additionally, a comparison of pre-and post-operative Worth-4-Dot test results revealed a significant improvement in the fusion ability of partially accommodative esotropia subgroup (at both near and distance, p ≤ 0.001). For patients with partially accommodative esotropia, fusion for far significantly improved from being present in 15.38% of patients pre-operatively to 46.15% post-operatively; similarly, for near fusion it significantly improved from 23.08% to 61.54% respectively. For patients with intermittent exotropia, fusion for near significantly improved from 61.67% pre-operatively to 83.87% reporting fusion post-operatively (p = 0.049). For congenital esotropia, fusion for far and near did not improve significantly. In contrast, stereoacuity did not significantly change post-operatively in all the subgroups. Table 4 summarizes the comparison between pre-operative and post-operative parameters highlighting the statistically significant ones.
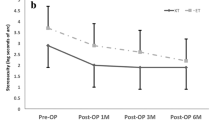
For the intermittent XT group, success rate tended to decrease with time. At 6 months to 1 year, it was 60%, it decreased to 35.29% at 2 to 3 years follow up and reached 23.08% at 4–6 years follow up. However, this change was not statistically significant (p = 0.271).
Discussion
This study investigated the characteristics and long-term surgical outcomes of horizontal strabismus in a single institution in a developing country and looked into predictive factors of surgical success in different strabismus subgroups. Comparison between groups revealed that esotropes (both partially accommodative and congenital) presented and were operated on earlier than intermittent exotropes. Partially accommodative ET patients had significantly more hyperopia compared to congenital ET and intermittent XT. Congenital ET patients had a significantly larger angle of deviation (for both far and near) than both partially accommodative ET and intermittent XT.
Moreover, a greater proportion had poor stereoacuity on presentation in the esotropia group. Final spherical equivalent, fusion and stereoacuity showed similar patterns to those on presentation. The surgical success rate was 72.67% for the entire group, with no significant difference between strabismus subtypes; for intermittent exotropia (73.07%), for partially accommodative esotropia (78.33%) and congenital esotropia (66.67%). Post-operatively, an improvement in fusion was observed in the 3 groups. As for predictive factors of surgical success, only in partially accommodative esotropia patients, surgical success was associated with a younger age at surgery and absence of amblyopia.
Similar to the literature, both of our esotropia subgroups presented at an early age [19,20,21,22], hence the lower average age than that of intermittent exotropes. Age at presentation of congenital esotropia found in the literature was mostly in the first year of life and that of accommodative esotropia was 2–4 years [20, 23] while age at presentation of intermittent exotropia (the most common XT subtype) was in late infancy or early childhood [24, 25]. Along the same line, the ET group had a higher spherical equivalent, as significant hyperopia is invariably associated with accommodative esotropia [26,27,28], this was also observed in our study. The fact that congenital esotropes in our study presented with a higher angle of deviation is in contrast with other studies that reported a greater deviation angle on presentation in exotropes [10, 29]; possibly due to our later age at presentation and surgery. Later presentation was most likely related to cultural differences with parents from our region assuming that strabismus could improve on its own or resolve spontaneously. A study from Nepal reported a presenting deviation angle of 48.2 ± 14.8 PD in esotropes and 57.8 ± 14.2 PD in exotropes [31]. Similarly, another study in Taiwan reported these values to be 38.4 ± 15.7 PD and 45.9 ± 12.6 PD for esotropia and exotropia, respectively [10]. Patients with partially accommodative esotropia in our cohort had a deviation angle at distance of 26 to 30 PD. A study from Ireland on accommodative esotropia reported a median deviation angle of 30 prism diopters [30]. Our measured deviation angles were larger in congenital esotropia (39 to 42 PD at distance), in agreement with the literature: Mohney et al. reported greater deviation angle in congenital esotropes (35.4 PD) than in accommodative esotropes (27.7 PD) [31]. The ranges for pre-operative deviation angles of each subgroup in our study were wide. This could be explained by low pre-operative measurements due to distance/near discrepancy, high or low AC/A ratio, or re-operations for small residual angles.
Our overall success rate was 72.67% with no significant differences between esotropes and exotropes. This value is comparable with published literature [5, 9,10,11]. A similar study reported surgical success rate of 71.0% at 6 months, where surgical success was similarly defined as a post-operative angle of 12 PD or less [9]. Others reported variable success rates of horizontal strabismus surgery ranging from 53.4% to 83% with post-operative success defined as an angle of 10 PD or less [10]. Our surgical success rate of intermittent exotropia was 73.07%, somehow higher than similar literature where success rate varied and was reported at 55% [18], 49.6% [17], 46.3% [13] and 70.2% [13]. In partially accommodative and congenital esotropia, our success rate values were at 78.33% and 66.67%, respectively. Kushner similarly reported success rate of 86.4% in accommodative esotropia [16]. Recently, a study addressing the outcomes of esotropia surgery in 2 tertiary hospitals in Cameroon unveiled a high success rate of 91.5% at the end of 3 months [15]. A study from Saudi Arabia reported “excellent” (less than 10 PD angle deviation) outcomes in 70.7% of patients at their first follow-up visit and 57.6% at their final visit [32]. With regards to infantile esotropia, surgical success rates in existing literature ranged from 83–94% in patients undergoing early surgery (by 6 months of age) [14] to values as low as 23% in those with a large angle of deviation (≥ 55 PD) [22]. Twenty-eight of our 172 patients (16.28%) patients required re-operation. A similar value of 12.9% as the proportion of patients requiring further surgery within one year was reported in the study from Thailand [5]. Re-operation after esotropia surgery is common in congenital ET where inferior oblique overaction and dissociated vertical deviations usually manifest in the second and third year of life and require further eye muscle surgery [33]. Intermittent exotropia is notorious for post-operative recurrence with studies showing recurrence rates ranging from 21.3% and up to 50% in different cohorts [17, 34,35,36].
In our cohort, esotropes had significantly poorer stereoacuity on presentation and at their final visit compared to the exotropes. Chen et al. similarly reported that exotropes had better stereopsis pre-operatively and post-operatively [10]. Patients with the intermittent type invariably have a close to normal stereoacuity, especially at near [37, 38]. The ocular misalignment at near in this condition is usually well controlled as compared to constant esotropes where most of the time binocularity is disrupted even after surgical motor re-alignment due to early disruption of fusion [39]. The lack of significant improvement in stereoacuity in both esotropes and exotropes may have several causes. In the intermittent XT group, most of the post-operative improvement is usually observed in distance stereoacuity [40, 41]. Our study assessed only near stereoacuity using the Titmus test which is usually within normal for patients with intermittent exotropia, especially the basic and divergence excess types. Our cohort consisted mostly of basic type intermittent XT. Later age at first surgery has been associated with a poorer stereoacuity in infantile and accommodative ET; and even after that, normal stereoacuity was quite a rare outcome [14, 39, 42, 43]. In the partially accommodative ET group, mean age at surgery in our cohort was 6.78 years ± 8.60; while that of congenital ET was 4.66 years ± 6.44.
We reported a significant increase in fusion capacity in partially accommodative esotropia (for both distance and near, p < 0.001) and intermittent exotropia (for near only, p = 0.049). Sharma et al. also reported an increase in binocular single vision from 0% to 18.7% in esotropia and from 0% to 39.3% in exotropia [29]. Chen et al. showed a general increase in sensory fusion capacity in both esotropes and exotropes up to a value of about 50% at the one-month follow-up compared to 0% at presentation [10]. Similarly, Kampanartsanyakorn et al. reported almost doubling of post-operative binocular function (from 22.6% to 40.5%) [5].
Our study revealed through multivariate logistic regression that a younger age was predictive of surgical success only in partially accommodative esotropes, but not for congenital ET or intermittent XT patients. It has been previously argued that ET patients would profit more from early surgery than exotropes, in terms of ocular alignment and binocular sensory functions [10]. Similarly, an age below 6 years and a pre-operative deviation of less than 30 prism diopters were predictive of a good horizontal strabismus surgery outcome [5]. Furthermore, esotropia and the absence of amblyopia were also found to be predictive of surgical success [11]; this was replicated in our study in the partially accommodative esotropia group. Poor compliance with prescribed treatment post-operatively such as consistent wearing of glasses, patching or atropine usage (when recommended) and appropriate attendance of appointments had been correlated with a poor surgical outcome for horizontal strabismus surgeries [9]. Compliance could not be recorded in our retrospective analysis.
Limitations of this study include its retrospective nature and consequently having visits/charts with missing data. A few patients were not included in the visual acuity analysis due to their non-numerical values (such as hand motion, central steady maintained and others). Furthermore, not all patients had stereoacuity and sensory fusion assessment, possibly due to young age or unavailability of the test. The esotropia group had a younger mean age and hence more preverbal children which sometimes precluded numerical visual acuity, stereoacuity and sensory fusion testing. The strengths of this study lie in the fact that our chart review was comprehensive and compared 3 subtypes of horizontal strabismus, in addition to our moderate sample size of 172 patients and longitudinal follow-up.
Conclusion
Our results showed that, at baseline, among horizontal strabismus surgeries, esotropes (partially accommodative or congenital) presented earlier, with a higher spherical equivalent (highest in partially accommodative) and a poorer stereoacuity than exotropes. They also had a greater deviation angle (the congenital subtype). The overall surgical success rate for horizontal strabismus surgery was 72.67% with no significant differences between partially accommodative esotropes, congenital esotropes and intermittent exotropes. Sensory fusion significantly improved in the partially accommodative ET group post-operatively for both far and near; and for near only in the intermittent XT group. A younger age at presentation and absence of amblyopia were found to be positively correlated with surgical success in the partially accommodative esotropia group.
References
Arora A, Williams B, Arora AK, McNamara R, Yates J, Fielder A (2005) Decreasing strabismus surgery. Br J Ophthalmol 89(4):409–412. https://doi.org/10.1136/bjo.2004.053678
Graham PA (1974) Epidemiology of strabismus. Br J Ophthalmol 58(3):224–231. https://doi.org/10.1136/bjo.58.3.224
Preslan MW, Novak A (1996) Baltimore vision screening project. Ophthalmology 103(1):105–109. https://doi.org/10.1016/s0161-6420(96)30753-7
Abrahamsson M, Magnusson G, Sjöstrand J (1999) Inheritance of strabismus and the gain of using heredity to determine populations at risk of developing strabismus. Acta Ophthalmol Scand 77(6):653–657. https://doi.org/10.1034/j.1600-0420.1999.770609.x
Kampanartsanyakorn S, Surachatkumtonekul T, Dulayajinda D, Jumroendararasmee M, Tongsae S (2005) The outcomes of horizontal strabismus surgery and influencing factors of the surgical success. J Med Assoc Thai 88(Suppl 9):S94–S99
Chia A, Dirani M, Chan Y-H et al (2010) Prevalence of amblyopia and strabismus in young Singaporean Chinese children. Invest Ophthalmol Vis Sci 51(7):3411–3417. https://doi.org/10.1167/iovs.09-4461
Burke JP, Leach CM, Davis H (1997) Psychosocial implications of strabismus surgery in adults. J Pediatr Ophthalmol Strabismus 34(3):159–164
Sun Y, Zhang T, Chen J (2018) Bilateral lateral rectus recession versus unilateral recession resection for basic intermittent exotropia: a meta-analysis. Graefes Arch Clin Exp Ophthalmol 256(3):451–458. https://doi.org/10.1007/s00417-018-3912-1
Dembinski RL, Collins ME, Kraus CL (2019) Outcomes following surgery for horizontal strabismus in children of lower socioeconomic backgrounds. Strabismus 27(2):47–53. https://doi.org/10.1080/09273972.2019.1626451
Chen YW, Lin SA, Lin PW, Huang HM (2019) The difference of surgical outcomes between manifest exotropia and esotropia. Int Ophthalmol 39(7):1427–1436. https://doi.org/10.1007/s10792-018-0956-5
Kumari N, Amitava AK, Ashraf M, Grover S, Khan A, Sonwani P (2017) Prognostic preoperative factors for successful outcome of surgery in horizontal strabismus. Oman J Ophthalmol 10(2):76–80. https://doi.org/10.4103/ojo.OJO_133_2016
Crouch ER Jr (1993) A comparison of the success rates of resident and attending strabismus surgery: discussion. J Pediatr Ophthalmol Strabismus 30(3):157–158
Bae GH, Bae SH, Choi DG (2019) Surgical outcomes of intermittent exotropia according to exotropia type based on distance/near differences. PLoS ONE 14(3):e0214478–e0214478. https://doi.org/10.1371/journal.pone.0214478
Birch EE, Stager DR Sr (2006) Long-term motor and sensory outcomes after early surgery for infantile esotropia. J Am Assoc Pediatric Ophthalmol Strabismus 10(5):409–413. https://doi.org/10.1016/j.jaapos.2006.06.010
Dohvoma VA, Ebana Mvogo SR, Ndongo JA, Mvilongo CT, Ebana Mvogo C (2020) Outcome of esotropia surgery in 2 tertiary hospitals in cameroon. Clin Ophthalmol 14:449–454. https://doi.org/10.2147/OPTH.S241861
Kushner BJ (2001) Fifteen-year outcome of surgery for the near angle in patients with accommodative esotropia and a high accommodative convergence to accommodation ratio. Arch Ophthalmol 119(8):1150–1153. https://doi.org/10.1001/archopht.119.8.1150
Maruo T, Kubota N, Sakaue T, Usui C (2001) Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocular Vis Strabismus Q 16(4):265–270
Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG (2009) Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J Am Assoc Pediatric Ophthalmol Strabismus 13(1):4–7. https://doi.org/10.1016/j.jaapos.2008.06.001
Berk AT, Koçak N, Ellidokuz H (2004) Treatment outcomes in refractive accommodative esotropia. J Am Assoc Pediatric Ophthalmol Strabismus 8(4):384–388. https://doi.org/10.1016/j.jaapos.2004.02.001
Archer SM, Sondhi N, Helveston EM (1989) Strabismus in infancy. Ophthalmology 96(1):133–137. https://doi.org/10.1016/S0161-6420(89)32932-0
Mohney BG, Erie JC, Hodge DO, Jacobsen SJ (1998) Congenital esotropia in olmsted county. Minnesota Ophthalmol 105(5):846–850. https://doi.org/10.1016/S0161-6420(98)95024-2
Wan MJ, Chiu H, Shah AS, Hunter DG (2018) Long-term surgical outcomes for large-angle infantile esotropia. Am J Ophthalmol 189:155–159. https://doi.org/10.1016/j.ajo.2017.11.006
Rutstein RP (2008) Update on accommodative esotropia. Optometry J Am Optometric Assoc 79(8):422–431. https://doi.org/10.1016/j.optm.2007.11.011
Hatt SR, Gnanaraj L (2013) Interventions for intermittent exotropia. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003737.pub3
Wright KW (2003) Lens abnormalities. In: Wright KW, Spiegel PH (eds) Pediatric ophthalmology and strabismus. Springer, New York. https://doi.org/10.1007/978-0-387-21753-6_27
Abrahamsson M, Fabian G, Sjöstrand J (1992) Refraction changes in children developing convergent or divergent strabismus. Br J Ophthalmol 76(12):723. https://doi.org/10.1136/bjo.76.12.723
Ingram RM, Gill LE, Goldacre MJ (1994) Emmetropisation and accommodation in hypermetropic children before they show signs of squint—a preliminary analysis. Bull Soc Belge Ophtalmol 253:41–56
Raab EL (1984) Hypermetropia in accommodative esodeviation. J Pediatr Ophthalmol Strabismus 21(5):P64–P68
Sharma AK, Thapa M, Shrestha GB, Sitaula S, Shrestha GS (2014) Outcome of horizontal strabismus surgery and parents’ satisfaction. Nepal J Ophthalmol 6(2):162–169. https://doi.org/10.3126/nepjoph.v6i2.11704
Quigley C, Cairns M, McElnea E, Doyle F, McCance J, Mullaney P (2017) A retrospective evaluation of bilateral medial rectus recession for management of accommodative esotropia according to prism-adapted motor response preoperatively. J Am Assoc Pediatric Ophthalmol Strabismus 21(2):157-159.e1. https://doi.org/10.1016/j.jaapos.2016.10.007
Mohney BG (2001) Common forms of childhood esotropia. Ophthalmology 108(4):805–809. https://doi.org/10.1016/S0161-6420(00)00639-4
Sulayem LM, Bin-Khathlan AA (2018) Outcomes of esotropia surgery in Saudi Arabia: an audit from a single center. Saudi J Ophthalmol 32(4):280–285. https://doi.org/10.1016/j.sjopt.2018.07.006
Rosenbaum AL, Santiago AP (1999) Clinical strabismus management: principles and surgical techniques. David Hunter.
Al-Haddad C, Ismail K, Houry R, Al Sayyid S, El Moussawi Z (2020) Recurrence of intermittent exotropia after bilateral lateral rectus recession. Middle East Afr J Ophthalmol 27(2):123–127. https://doi.org/10.4103/meajo.MEAJO_188_18
Koklanis K, Georgievski Z (2009) Recurrence of intermittent exotropia: factors associated with surgical outcomes. Strabismus 17(1):37–40. https://doi.org/10.1080/09273970802678750
Kim HJ, Choi DG (2016) Clinical analysis of childhood intermittent exotropia with surgical success at postoperative 2 years. Acta Ophthalmol 94(2):e85–e89. https://doi.org/10.1111/aos.12849
Hatt SR, Mohney BG, Leske DA, Holmes JM (2008) Variability of stereoacuity in intermittent exotropia. Am J Ophthalmol 145(3):556-561.e1. https://doi.org/10.1016/j.ajo.2007.10.028
Stathacopoulos RA, Rosenbaum AL, Zanoni D et al (1993) Distance stereoacuity: assessing control in intermittent exotropia. Ophthalmology 100(4):495–500. https://doi.org/10.1016/S0161-6420(93)31616-7
Birch EE, Fawcett S, Stager DR (2000) Why does early surgical alignment improve stereoacuity outcomes in infantile esotropia? J Am Assoc Pediatric Ophthalmol Strabismus 4(1):10–14. https://doi.org/10.1016/S1091-8531(00)90005-3
Yildirim C, Mehmet Mutlu F, Chen Y, Altinsoy HI (1999) Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol 128(2):222–230. https://doi.org/10.1016/S0002-9394(99)00079-3
Adams WE, Leske DA, Hatt SR et al (2008) Improvement in distance stereoacuity following surgery for intermittent exotropia. J Am Assoc Pediatric Ophthalmol Strabismus 12(2):141–144. https://doi.org/10.1016/j.jaapos.2007.09.015
Birch EE, Wang J (2009) Stereoacuity outcomes after treatment of infantile and accommodative esotropia. Optometry Vis Sci 86(6):647–652. https://doi.org/10.1097/OPX.0b013e3181a6168d
Birch EE (2003) Marshall Parks lecture. Binocular sensory outcomes in accommodative ET. J Am Assoc Pediatric Ophthalmol Strabismus 7(6):369–373. https://doi.org/10.1016/j.jaapos.2003.08.003
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dakroub, M., El Hadi, D., El Moussawi, Z. et al. Characteristics and long-term surgical outcomes of horizontal strabismus. Int Ophthalmol 42, 1639–1649 (2022). https://doi.org/10.1007/s10792-021-02159-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02159-4