Abstract
Purpose
We performed a systematic review and meta-analysis to assess the role of prophylactic laser retinopexy in preventing rhegmatogenous retinal detachment (RRD) in acute retinal necrosis (ARN).
Methods
Pubmed, Embase and Cochrane databases were searched for eligible studies from inception to July 2020. Comprehensive clinical demographics were extracted from each study by two independent investigators. A random effects model was selected to analyze the OR of RRD risk and visual outcome with 95%CI. Subsequent subgroup and sensitivity analysis were conducted to evaluate the source of heterogeneity.
Results
A total of eight studies and 247 eyes (111 prophylactic laser retinopexy eyes and 136 eyes receiving antiviral treatment) were included in this analysis. There was moderate statistical heterogeneity across all studies. When compared with routine antiviral treatment alone, RRD risk decreased in patients receiving prophylactic laser retinopexy, however, this was not statistically significant (P = 0.09, OR = 0.42, 95%CI: 0.15–1.15). There was significant improvement in BCVA during the follow-up period in the prophylactic laser retinopexy subgroup (P = 0.01, WMD = − 0.98, 95%CI: − 1.74, − 0.22).
Conclusion
Based on current analysis, our results did not support convincing evidence of prophylactic laser in preventing RRD. Future studies featuring high-quality, multicenter trials will be required to correct baseline characteristics.
Trial registration
This meta-analysis has been retrospectively registered in Prospero (registration number: CRD42020201008).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
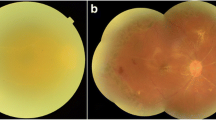
Acute retinal necrosis (ARN) is a viral, infectious retinitis characterized by confluent areas of retinal necrosis, vitritis and anterior inflammation. First reported in the 1970s, ARN potentially causes devastating ocular complications and irreversible visual loss in one or both eyes [1]. This destructive uveitis entity occurs most commonly in immunocompetent individuals, but has also been described in immunocompromised hosts. Varicella zoster virus (VZV) and herpes simplex virus (HSV) have both been presumed to be the predominant pathogens leading to ARN [2], while Epstein–Barr virus (EBV) and cytomegalovirus (CMV) have also been implicated [3, 4].
Globally, approaches to treat ARN have focused on intravenous acyclovir (10 mg/kg every 8 h) and oral valacyclovir at disease onset. In recent years, novel antiviral treatments including intravitreal ganciclovir and foscarnet [5] as well as oral valganciclovir or acyclovir have also been considered [6]. Despite these standard therapies, the visual outcome of ARN patients remains poor [7]. Rhegmatogenous retinal detachment (RRD), macula and optic nerve involvement by vasculature destruction have been identified as the main causes of unsatisfactory clinical prognosis, followed by proliferative vitreoretinopathy, macular hole formation and epiretinal membrane [2, 8, 9].
Given the relatively high risk of RRD in ARN, some scholars advocated prophylactic laser retinopexy to reduce the incidence of RRD while several studies opposed [10,11,12,13,14,15,16,17]. However, the design of most previous studies is single-center, retrospective and observational, limiting the reliability and repeatability of conclusion. Taking the rarity of ARN into account, performing multicenter random controlled trials is deemed impracticable [18]. To shed light on this issue, present meta-analysis was conducted to assess the efficacy of prophylactic laser retinopexy in ARN patients.
Methods
The present meta-analysis was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) statement [19].
Search strategy and inclusion criteria
Two independent researchers (SPF and DL) performed the literature search in PubMed, EMBASE databases and Cochrane library from inception to July 2020 using the terms (acute retinal necrosis OR retinal necrosis) AND (laser OR endolaser OR photocoagulation). Reference lists from resulting publications were scanned to avoid omitting relevant citations. Inclusion criteria were as follows: (1) original investigations including retrospective cohort series, interventional and cross-sectional studies, (2) research focused on acute retinal necrosis and prophylactic laser, (3) articles with detailed information regarding baseline characteristics and clinical outcomes. Pre-specified exclusion criteria were as follows: lack of full text manuscript, studies lacking sufficient data, case reports, letters and editorials.
Data extraction and quality assessment
The following data were independently extracted by two investigators (SPF and DL) from each eligible study: leading author name, publication year, sample size, survey period, demographic characteristics of participants, prevalence of RRD and visual outcome at final visit, in accordance with pre-designed inclusion and exclusion criteria. The quality of selected studies was assessed by two independent reviewers (SPF and DL) based on the Newcastle–Ottawa Quality Assessment Scale (NOS). The NOS consists of eight items, divided into three dimensions including selection, comparability and follow-up outcomes. Each item was given one score while the item “comparability of cohorts on the bias of the design or analysis” was given one or two scores according to the baseline characteristics of included studies. If any disagreement occurred, it was resolved through consensus or discussion with a third researcher (YQW). Visual acuity was expressed as logMAR for further comparison and analysis. We converted finger counting, hand motion, light perception and no light perception into logMAR (1.6, 2.0, 2.5 and 3.0, respectively) if the results of best corrected visual acuity (BCVA) were not directly displayed [14].
Statistical analysis
The clinical outcomes including odds ratio (OR) value of RRD incidence and weighted mean difference (WMD) of visual outcome were calculated using random effects model. Cochran’s Q test and I2 test were performed to assess heterogeneity between included studies. In accordance with meta-analysis principle, I2 < 50% indicated low heterogeneity. Subgroup analysis was conducted according to sample size. In addition, sensitivity analysis was used to identify the origin of heterogeneity by sequentially removing one investigation at a time. Egger’s test was adopted to evaluate the publication bias. Meta-analyses were conducted using Stata software (version 12.0, Stata Corp, College Station, TX, USA). Statistical significance was set as p < 0.05 for a two-tailed test.
Results
Study inclusion
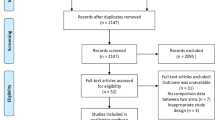
In total, 160 citations relevant to our topic were identified from the PubMed (74) and Embase (86) databases. As shown in Fig. 1, after removing 60 duplicated records, 100 studies were screened with title and abstract for eligibility. Consequently, 25 articles were reviewed with full texts. Seventeen publications were removed in present meta-analysis for the following reasons: editorial (n = 1), review (n = 3), without control group (n = 2), laser retinopexy after retinal detachment (n = 1), lacking full text article (n = 2) and lacking data of demographic characteristics and clinical outcomes (n = 8). Eight original articles fulfilling the eligibility criteria were included and subjected to meta-analysis.
Study demographics
The clinical characteristics of eligible studies are presented in Tables 1, 2 and 3. Eight investigations with 111 prophylactic laser retinopexy in combination with standard antiviral eyes and 136 eyes receiving antiviral treatment alone were retrieved in accordance with the search criteria. Prophylactic laser was performed on the normal retina posterior to necrotic areas, in cases without retinal detachment and vitrectomy. Among these studies, three were performed in American, one was conducted in China, Britain, Korea, Iran and Netherlands, respectively. All studies included in this meta-analysis were designed as retrospective owing to the low occurrence of ARN. If available, detailed demographics including age, gender, interval from onset to diagnosis and extent of retinal necrosis were recorded. The treatment protocol for antiviral and adjuvant therapies varied widely between referral centers. All trials reported the incidence of RRD eyes, whereas visual outcome was not summarized in each study. The methodological quality of most studies ranged from scores of five to six out of a total of nine, except for the investigation conducted by Risseeuw et al. [16], which corrected for the severity of the study cohort’s baseline characteristics (Tab. S1).
Statistical synthesis
There was moderate heterogeneity for RRD risk and a random effects model was selected to synthesize the data. Compared with antiviral treatment alone, the RRD rate decreased in patients receiving prophylactic laser retinopexy, without statistical significance (Fig. 2, P = 0.09, OR = 0.42, 95%CI: 0.15–1.15). In an analysis stratified by sample size, four independent studies demonstrated a notable decrease in RRD risk in the prophylactic laser retinopexy subgroup (P = 0.01, OR = 0.20, 95%CI: 0.06–0.70). No statistical difference was identified among the relatively large sample size subgroups (P = 0.55, OR = 0.64, 95%CI: 0.15–2.75). Three studies confirmed that the prophylactic laser retinopexy subgroup had significant improvement in BCVA during the follow-up period (Fig. 3, P = 0.01, WMD = − 0.98, 95%CI: − 1.74, − 0.22). As shown in Fig. 4, when sequentially excluding one retrospective cohort study to perform sensitivity analysis, the OR value of RRD risk remained stable. This finding confirmed the stability and reliability of this meta-analysis. Moreover, Egger’s test and funnel plots indicated significant publication bias of RRD risk for the eight included studies (P < 0.05).
Discussion
ARN is a rare ocular disorder that is found across the world. Generally, ARN results in poor visual outcomes. A systematic review revealed the general RRD rate of ARN is 47% during the follow-up period [20]. RRD occurs in approximately 26–90% of eyes only receiving antiviral treatment and has been reported to be the most common cause of deteriorated visual acuity [2, 12,13,14, 16]. When ARN occurs, the retina turns necrotic approximately two months after disease onset, accelerating the formation of retinal tears and RRD. As previously reported, the median interval between disease onset and RRD is 53 days, but can range from 28 to 165 days [14]. Given this, the use of prophylactic laser retinopexy has been proposed to reduce RRD risk by forming chorioretinal adhesion.
There was significant publication bias in present meta-analysis, as identified by the Egger’s test. Taking various confounding factors into consideration for ARN, observative and small sample investigations with no statistical significance tend not to be submitted or accepted for publication. Moreover, meeting abstracts and dissertations could not be retrieved even if comprehensive and rigorous search was conducted. In addition, it is worthwhile to point out that retrospective design, incomplete clinical features and insufficient data analyses may lead to inevitable publication bias. Thus, the results of this meta-analysis should be interpreted with caution.
The most obvious result emerging from present meta-analysis was no significant advantage of prophylactic laser in preventing RRD. This finding was in agreement with the conclusion of two previous studies, both of which had relatively large sample size [14, 16]. Subgroup analysis by sample size demonstrated significantly reduced RRD risk in studies with small samples, indicating the potential for inaccurate conclusions in single-center studies. Patients undergoing prophylactic laser retinopexy must have relatively mild vitritis to allow clear visualization of peripheral retina. The application of laser is limited in cases with severe vitreous haze, therefore precluding any attempt at laser and leading to selection bias. Severe vitritis predisposed to accompany with wider extent of involved retina, facilitating the formation of retinal tears and increasing RRD risk [14, 21]. A possible explanation for this result is initiating agents for disease progressing remain unsettled. Pro-inflammatory cytokines and chemokines including monokine induced by interferon γ, interferon γ, interferon-γ-inducible protein-10, interleukin-6, interleukin-8 and interleukin-17 have been shown to have essential roles in the pathogenesis of ARN relative to other ocular disorders [22, 23]. The imbalance between pro- and anti-inflammatory reactions contributes to the rapid and destructive development of ARN [24]. Performance of laser retinopexy could not remove the inflammatory mediators and high viral load, which have been considered to be the predominant cause of retinitis and vitritis. The vitreous traction, another crucial factor of RRD, was also not relieved by prophylactic laser. Another noteworthy issue is photocoagulation at the previously necrotic retina may cause retinal damage and promote the formation of atrophic hole, indicating the importance of suitable laser spots [10, 15]. Although significantly improved visual outcome was observed in the prophylactic laser subgroup, only three studies have reported quantifiable results for visual prognosis, which were affected by both selection bias and small study size effects [10, 11, 17]. It is worth mentioning that the possibility of a benefit from such prophylactic effects should be considered if assessed in a multicenter study.
The antiviral regimen and adjuvant treatment varied widely among referral centers, with different treatment patterns likely leading to discrepancies in clinical outcomes. Retrospective investigations demonstrated that intravenous acyclovir significantly decreased the incidence of fellow eye involvement and accelerated disease resolution [25, 26]. Therefore, intravenous acyclovir has been the most widely adopted treatment for ARN worldwide, as described in all included studies. Recent studies recommended that oral valacyclovir or famciclovir effectively improved the visual acuity and decreased the RRD rate in ARN [27, 28]. Intravitreal ganciclovir or foscarnet has also been identified as an efficient option to alleviate inflammation [29, 30]. However, Tibbetts et al. [14] discovered that various antiviral therapies did not affect clinical visual outcome of ARN. Detailed investigations of therapeutic effects and bioavailability of various antiviral treatments will generate advanced insights for ophthalmologists.
This study had several limitations. First, the sample sizes of previous studies were relatively small, owing to low incidence of ARN. In addition, all included studies were retrospective and cross section, limiting the level of evidence owing to selection bias. Multiple studies did not control for disease severity and other influential factors such as the interval from diagnosis to laser retinopexy, follow-up period. Another essential concern is the lack of gold standard of assessment for the extent of involved retina. Various grading criteria including clock hours of involved retina, percent of necrotic areas and cumulative number of quadrants are adopted, limiting the direct comparisons among included studies. As a result, concisions from these studies are likely inconclusive. Standard definitions of treatment success also vary extensively, including RRD rate, visual and anatomic prognosis, and interval from treatment to remission. Further studies that take these variables into account will be needed in the future.
Conclusions
In conclusion, this meta-analysis provides comprehensive and updated elucidation of prophylactic laser retinopexy in ARN. Our results do not support convincing evidence of prophylactic laser in preventing RRD. Taken present observations into consideration, a multicenter investigation with corrected extent of involved retina will be needed to explore the role of prophylactic laser retinopexy and evaluate long-term clinical prognosis.
References
Schoenberger SD, Kim SJ, Thorne JE, Mruthyunjaya P, Yeh S, Bakri SJ, Ehlers JP (2017) Diagnosis and treatment of acute retinal necrosis: a report by the American Academy of Ophthalmology. Ophthalmology 124:382–392. https://doi.org/10.1016/j.ophtha.2016.11.007
Hillenkamp J, Nölle B, Bruns C, Rautenberg P, Fickenscher H, Roider J (2009) Acute retinal necrosis: clinical features, early vitrectomy, and outcomes. Ophthalmology 116:1971-1975.e1972. https://doi.org/10.1016/j.ophtha.2009.03.029
Ganatra JB, Chandler D, Santos C, Kuppermann B, Margolis TP (2000) Viral causes of the acute retinal necrosis syndrome. Am J Ophthalmol 129:166–172. https://doi.org/10.1016/s0002-9394(99)00316-5
Schaal S, Kagan A, Wang Y, Chan CC, Kaplan HJ (2014) Acute retinal necrosis associated with Epstein-Barr virus: immunohistopathologic confirmation. JAMA Ophthalmol 132:881–882. https://doi.org/10.1001/jamaophthalmol.2014.266
Winterhalter S, Stuebiger N, Maier AK, Pleyer U, Heiligenhaus A, Mackensen F, Zierhut M, Joussen AM, Ness T (2016) Acute retinal necrosis: diagnostic and treatment strategies in Germany. Ocul Immunol Inflamm 24:537–543. https://doi.org/10.3109/09273948.2015.1034375
Baltinas J, Lightman S, Tomkins-Netzer O (2018) Comparing treatment of acute retinal necrosis with either oral valacyclovir or intravenous acyclovir. Am J Ophthalmol 188:173–180. https://doi.org/10.1016/j.ajo.2018.02.001
Paolo M, Marta Z, Stefania F, Viola T, Giacomo C, Arturo C, Stefano G, Yan GC (2020) Visual outcome and poor prognostic factors in acute retinal necrosis syndrome. Graefes Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s00417-020-04701-z
Liu S, Wang D, Zhang X (2018) The necessity and optimal time for performing pars plana vitrectomy in acute retinal necrosis patients. BMC Ophthalmol 18:15. https://doi.org/10.1186/s12886-018-0674-9
Wong RW, Jumper JM, McDonald HR, Johnson RN, Fu A, Lujan BJ, Cunningham ET Jr (2013) Emerging concepts in the management of acute retinal necrosis. Br J Ophthalmol 97:545–552. https://doi.org/10.1136/bjophthalmol-2012-301983
Sternberg P Jr, Han DP, Yeo JH, Barr CC, Lewis H, Williams GA, Mieler WF (1988) Photocoagulation to prevent retinal detachment in acute retinal necrosis. Ophthalmology 95:1389–1393. https://doi.org/10.1016/s0161-6420(88)32999-4
Chen HP, Kuo HK, Tsai SH, Chen YJ, Kao ML (2004) Acute retinal necrosis syndrome: clinical manifestations and visual outcomes. Chang Gung Med J 27:193–200
Lau CH, Missotten T, Salzmann J, Lightman SL (2007) Acute retinal necrosis features, management, and outcomes. Ophthalmology 114:756–762. https://doi.org/10.1016/j.ophtha.2006.08.037
Meghpara B, Sulkowski G, Kesen MR, Tessler HH, Goldstein DA (2010) Long-term follow-up of acute retinal necrosis. Retina 30:795–800. https://doi.org/10.1097/IAE.0b013e3181c7013c
Tibbetts MD, Shah CP, Young LH, Duker JS, Maguire JI, Morley MG (2010) Treatment of acute retinal necrosis. Ophthalmology 117:818–824. https://doi.org/10.1016/j.ophtha.2009.09.001
Kim DY, Jo J, Joe SG, Lee JY, Yoon YH, Kim JG (2019) Clinical feature and visual prognosis of acute retinal necrosis according to the initially involved zone and extent: 10-year experience. Eur J Ophthalmol 29:244–250. https://doi.org/10.1177/1120672118787438
Risseeuw S, de Boer JH, Ten Dam-van Loon NH, van Leeuwen R (2019) Risk of rhegmatogenous retinal detachment in acute retinal necrosis with and without prophylactic intervention. Am J Ophthalmol 206:140–148. https://doi.org/10.1016/j.ajo.2019.05.023
Hedayatfar A, Ebrahimiadib N, Zarei M, Ashraf Khorasani M, Mahbod M, Asgari S, Sedaghat A (2020) Acute retinal necrosis: clinical manifestation and long-term visual outcomes in a series of polymerase chain reaction-positive patients. Eur J Ophthalmol. https://doi.org/10.1177/1120672120936181
Muthiah MN, Michaelides M, Child CS, Mitchell SM (2007) Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK. Br J Ophthalmol 91:1452–1455. https://doi.org/10.1136/bjo.2007.114884
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647. https://doi.org/10.1136/bmj.g7647
Zhao XY, Meng LH, Zhang WF, Wang DY, Chen YX (2021) Retinal detachment after acute retinal necrosis and the efficacies of different interventions: a systematic review and metaanalysis. Retina 41:965–978. https://doi.org/10.1097/iae.0000000000002971
Butler NJ, Moradi A, Salek SS, Burkholder BM, Leung TG, Dunn JP, Thorne JE (2017) Acute retinal necrosis: presenting characteristics and clinical outcomes in a cohort of polymerase chain reaction-positive patients. Am J Ophthalmol 179:179–189. https://doi.org/10.1016/j.ajo.2017.05.006
de Visser L, de Boer JH, Rijkers GT, Wiertz K, van den Ham HJ, de Boer R, van Loon AM, Rothova A, de Groot-Mijnes JD (2017) Cytokines and chemokines involved in acute retinal necrosis. Invest Ophthalmol Vis Sci 58:2139–2151. https://doi.org/10.1167/iovs.16-20799
Nezu N, Usui Y, Saito A, Shimizu H, Asakage M, Yamakawa N, Tsubota K, Wakabayashi Y, Narimatsu A, Umazume K, Maruyama K, Sugimoto M, Kuroda M, Goto H (2021) Machine learning approach for intraocular disease prediction based on aqueous humor immune mediator profiles. Ophthalmology 128:1197–1208. https://doi.org/10.1016/j.ophtha.2021.01.019
Zhang P, Liu S, Wang Z, Zhou M, Jiang R, Xu G, Chang Q (2020) Immune cell status and cytokines profiles in patients with acute retinal necrosis. Ocul Immunol Inflamm. https://doi.org/10.1080/09273948.2020.1734214
Palay DA, Sternberg P Jr, Davis J, Lewis H, Holland GN, Mieler WF, Jabs DA, Drews C (1991) Decrease in the risk of bilateral acute retinal necrosis by acyclovir therapy. Am J Ophthalmol 112:250–255. https://doi.org/10.1016/s0002-9394(14)76725-x
Crapotta JA, Freeman WR, Feldman RM, Lowder CY, Ambler JS, Parker CE, Meisler DM (1993) Visual outcome in acute retinal necrosis. Retina 13:208–213. https://doi.org/10.1097/00006982-199313030-00004
Taylor SR, Hamilton R, Hooper CY, Joshi L, Morarji J, Gupta N, Lightman SL (2012) Valacyclovir in the treatment of acute retinal necrosis. BMC Ophthalmol 12:48. https://doi.org/10.1186/1471-2415-12-48
Emerson GG, Smith JR, Wilson DJ, Rosenbaum JT, Flaxel CJ (2006) Primary treatment of acute retinal necrosis with oral antiviral therapy. Ophthalmology 113:2259–2261. https://doi.org/10.1016/j.ophtha.2006.05.063
Flaxel CJ, Yeh S, Lauer AK (2013) Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syndrome (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 111:133–144
Wong R, Pavesio CE, Laidlaw DA, Williamson TH, Graham EM, Stanford MR (2010) Acute retinal necrosis: the effects of intravitreal foscarnet and virus type on outcome. Ophthalmology 117:556–560. https://doi.org/10.1016/j.ophtha.2009.08.003
Author information
Authors and Affiliations
Contributions
SPF and DL contributed to the design of review and extracted the data. SPF performed the statistical analysis and drafted the paper. YQW and RHW critically reviewed it and suggested amendments prior to submission.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fan, S., Lin, D., Wu, R. et al. Efficacy of prophylactic laser retinopexy in acute retinal necrosis: A systematic review and meta-analysis. Int Ophthalmol 42, 1651–1660 (2022). https://doi.org/10.1007/s10792-021-02131-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02131-2