Abstract
Aim
To analyze the efficacy of navigated focal laser photocoagulation (FLP) of microaneurysms in diabetic macular edema (DME) planned using en face optical coherence tomography (OCT) as against fluorescein angiography (FA).
Methods
Twenty-six eyes of 21 DME patients (12 males, 9 females, 69.5 ± 12.3 years) with mean BCVA of 0.52 ± 0.44 LogMAR were included. En face OCT images of deep capillary plexus slab and FA images were used to plan FLP targeting of leaky microaneurysms. The primary outcome measures were central retinal thickness (CRT) and macular volume. The secondary outcome measure was best-corrected visual acuity (BCVA).
Results
The difference in the change of CRT and macular volume between en face OCT and FA-planned FLP after 1 month and at the end of follow-up was not statistically significant (p > 0.05), except for a higher CRT reduction in the en face OCT-planning group (p = 0.007) at the end of mean follow-up of 2.6 ± 0.9 months. There was no difference in BCVA change between the two planning options (p = 0.42).
Conclusion
En face OCT is a non-inferior alternative for FA in the planning of navigated FLP of microaneurysms in DME.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Although anti-vascular endothelial growth factor (VEGF) therapy is the first-line treatment for diabetic macular edema (DME), laser photocoagulation remains an effective option for controlling DME in selected cases [1,2,3]. However, laser treatment, except for micropulse laser therapy, is potentially damaging for retinal tissue since it leads to partial loss of RPE and photoreceptors. The evolution of technologies has also made conventional laser therapy less harmful to the retina. This was achieved with navigated laser technology, which minimizes the deviation of the laser beam leading to the reduction of collateral damage to the retina along with an increased microaneurysm hit rate [4, 5].
One disadvantage of the use of laser therapy in DME treatment is the need for additional diagnostic data when planning treatment. Despite the appearance of non-invasive diagnostic options such as optical coherence tomography (OCT) and OCT angiography, fluorescein angiography (FA) remains a standard method for identifying the source of leakage in DME [6]. This is related to the limited visualization of microaneurysms and inability to detect leakage by OCT angiography [7]. However, an additional FA procedure prior to laser treatment is time-consuming. Moreover, FA is an invasive procedure associated with the risk of adverse events [8, 9].
We showed previously that structural en face OCT is an adequate alternative to FA for displaying microaneurysms in DME, identifying more than 90% of leaky microaneurysms [10]. Planning of focal laser photocoagulation (FLP) based on en face OCT looks attractive since it turns laser treatment into a fully non-invasive technique and may ease the clinical workload. However, it is not known if the efficacy of this OCT-based approach remains non-inferior.
This study, therefore, aims to analyze the efficacy of navigated focal laser photocoagulation of microaneurysms in DME planned upon en face OCT, compared to conventional FA-based planning.
Methods
The study followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee. All individuals signed written informed consent before participating in the study.
This prospective interventional study includes patients with DME. Exclusion criteria were stage 3–5 chronic kidney disease, diabetic neuropathies, optical media opacities affecting OCT or FA imaging and/or impeding the FLP procedure, vitreoretinal interface abnormalities (vitreomacular traction syndrome or fibrosis of inner limiting membrane within central 3-mm area), intravitreal anti-VEGF therapy within 2 months or less before FLP, HbAc1 > 7.5%, any changes in systemic or topical medication, and any intraocular surgery during the follow-up period.
All patients received a comprehensive ophthalmic examination including assessment of best-corrected visual acuity (BCVA) and OCT examination. Each patient was randomly selected for the OCT or the FA-planning group. If both eyes of the patient were included in the study, the eyes were included in the separate study groups. For all eyes, a Macular Map and OCT angiography volume scan 6 × 6 mm were obtained using RTVue-XR Avanti (Optovue, Fremont, CA). Macular Map protocol included 17 horizontal (6 × 3 mm and 11 × 5 mm) and 17 vertical (6 × 3 mm and 11 × 5 mm) cross-sectional scans organized in equilateral grid with 0.5-mm interval between neighboring scans. OCT angiography volume scan included two sets of 400 repeated cross-sectional scans acquired twice in orthogonal directions. Two orthogonally acquired sets then merged in a single OCTA scan to reduce motion artifacts.
In the FA-planning group, the patients received FA with F-10 scanning laser ophthalmoscope (NIDEK, Gamagori, Japan). The values of central retinal thickness (CRT), macular volume, and mean thickness of sectors of the EDTRS retinal thickness chart were taken for analysis. Central retinal thickness was defined as the mean distance from retinal pigment epithelium segmentation line to segmentation line of the inner limiting membrane within the central subfield of ETDRS Map-centered on the center of the fovea. Macular volume was defined as the sum of the volumes of all sectors and the central subfield of ETDRS map. Since patients in this study typically demonstrated focal DME, retinal exudation was additionally evaluated as change of retinal thickness in individual ETDRS sectors and change of macular volume, rather than CRT only. Each ETDRS sector was defined as “treated” if at least one microaneurysm treated with laser was presented in this sector. If no microaneurysms treated with laser were presented, a sector was defined as “non-treated”. Follow-up examination was performed at month 1 after FLP and 2–3 months after FLP. Primary outcome measures were CRT and macular volume at 1 month after FLP and at the end of follow-up. Secondary outcome measure was BCVA.
Since our previous study showed a high correlation between FA and en face images obtained in the deep capillary plexus slab, en face images for OCT-planning were obtained in this slab (IPL = 0 µm, INL = − 70 µm) [10]. After correction of automated segmentation lines (if needed), en face images were exported and downloaded in the laser system.
FA was performed on the same day as OCT and laser treatment. To plan FLP, images of the early phase of FA were used. Images taken during the late phase of FA were used for confirmation of the leaky status of microaneurysms.
All FLP procedures were performed with Navilas 577+ (OD-OS, Teltow, Germany) after mydriasis was achieved with topical tropicamide 1%. After a baseline fundus image was obtained, either en face OCT or FA image was superimposed on it by alignment of retinal vessels. FLP guided by en face OCT was performed by a single specialist (MDS) targeting all microaneurysms (defined as round or oval-shaped moderately reflective structures) in the area of accumulation of intraretinal cystic fluid [10]. When planned using FA image, FLP targeted all leaky microaneurysms within the macula. Highly reflective microaneurysms and those with capsular structure remained untreated. For FLP, we used standard settings with pulse duration of 100 ms and spot size of 100 µm. At the beginning of each treatment session, adjustment of laser power was performed until the blanching of treated microaneurysm was achieved.
Statistical analysis was performed using MedCalc 18.4.1 (MedCalc Software, Ostend, Belgium). The normality of data distribution was confirmed with Kolmogorov–Smirnov test. All data presented as a mean ± standard deviation. One-way analysis of variance (ANOVA) was used to compare difference of retinal thickness in treated and non-treated ETDRS sectors. Change in CRT, macular volume, and BCVA score before and after FLP were compared with repeated measure ANOVA. The difference in change of CRT and macular volume in study groups was compared with ANOVA. A p value of < 0.05 was considered to be statistically significant.
Results
In this study, we included 26 eyes of 21 patients (12 males and 9 females, mean age 69.5 ± 12.3 years) with mean BCVA of 0.52 ± 0.44 LogMAR (≈ 0.43 of Snellen equivalent). There was no statistically significant difference between the study groups in baseline characteristics (p > 0.05) (Table 1) as well as in the number of microaneurysms detected (p = 0.24) and laser burns applied (p = 0.35).
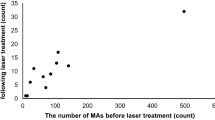
At 1 month after FLP, change of retinal thickness in treated and non-treated sectors was − 34.4 ± 32.5 µm and − 9.3 ± 22.9 µm, respectively (p = 0.01) (Fig. 1a). Change in CRT and macular volume in the whole study population was − 37.6 ± 66.0 µm (p = 0.017) and − 0.52 ± 0.7 mm3 (p = 0.005), respectively. The difference in change of CRT and macular volume between the groups of en face and FA planned FLP was not statistically significant (p = 0.09 and p = 0.19, respectively) (Fig. 2).
Box-and-whiskers plots showing change of the main outcome measures in the study groups. a Change of central retina thickness (CRT) at 1 month after focal laser photocoagulation. b Change of CRT at the end of follow-up. c Change of macular volume (MV) at 1 month after focal laser photocoagulation. d Change of MV at the end of follow-up
At the end of a mean follow-up of 2.6 ± 0.9 months, retinal thickness in the sectors treated changed by − 41.4 ± 48.1 µm, while in the non-treated sectors the change of retinal thickness was − 8.3 ± 31.0 µm (p = 0.03) (Fig. 1b). The mean change of CRT and macular volume in the whole study population was − 69.2 ± 85.6 µm (p = 0.004) and − 0.67 ± 0.9 mm3 (p = 0.007), respectively. The difference in CRT change between the study groups was statistically significant (p = 0.007); however, the change of macular volume demonstrated no statistical significance between FA and en face-planned groups (p = 0.11) (Fig. 2).
At the end of follow-up, the mean BCVA had a statistically significant increase to 0.45 ± 0.42 LogMAR (≈ 0.5 of Snellen equivalent) (p = 0.047). A comparison of different planning options did not show a statistically significant difference in the mean BCVA change (p = 0.42) (Figs. 3, 4, 5, 6).
A representative example of en face planning of navigated focal laser photocoagulation in center-involved diabetic macular edema in the right eye of 67-year-old female. a Baseline fundus image with en face image overlaid. b Treatment plan. c Baseline cross-sectional image. d Cross-sectional image at the end of follow-up. Central retinal thickness and macular volume reduced from 313 to 238 µm and from 8.67 to 8.17 mm3, respectively, over a follow-up period of 3 months. Best-corrected visual acuity improved from 20/32 to 20/25
A representative example of en face planning of focal laser photocoagulation focal diabetic macular edema in the right eye of 70-year-old male. a Baseline fundus image with en face image overlaid. b Treatment plan. c Baseline cross-sectional image. d Cross-sectional image at the end of follow-up. Central retinal thickness reduced from 333 to 273 µm but macular volume remained stable (7.16 mm3 at baseline and 7.18 at the end of follow-up), over a period of 4 months. Best-corrected visual acuity improved from 20/25 to 20/20(–)
A representative example of en face planning of focal laser photocoagulation in fovea sparing diabetic macular edema in the left eye of 75-year-old female. a Baseline fundus image with en face image overlaid. b Treatment plan. c Baseline cross-sectional image. d Cross-sectional image at the end of follow-up. Central retinal thickness reduced from 290 to 255 µm over a follow-up period of 2.5 months. Macular volume reduced from 9.85 to 8.94 mm3, however, best-corrected visual acuity remained 20/32
A representative example of fluorescein angiography planning of focal laser photocoagulation in fovea involving diabetic macular edema in the left eye of 69-year-old male. a Baseline fundus image with fluorescein angiography image overlaid. b Treatment plan. c Baseline cross-sectional image. d. Cross-sectional image at the end of follow-up. Central retinal thickness reduced from 375 to 297 µm over a follow-up period of 2 months. Macular volume reduced from 8.24 to 7.85 mm3, best-corrected visual acuity improved from 20/32 to 20/25
Discussion
In this study, we showed that navigated focal laser photocoagulation in DME, when planned using en face OCT, is non-inferior to that planned using FA in terms of CRT and macular volume reduction with comparable changes in BCVA.
The primary outcome measures in this study included CRT and macular volume, while BCVA was the secondary outcome measure. We focused on the anatomical outcome for several reasons. Firstly, FLP is mostly aimed at the preservation of visual acuity rather than at functional improvement. Therefore, the detection of improvement during short-term follow-up would be hardly possible in a relatively small study population. More prolonged observation appears to be not justified since FLP typically does not allow complete resolution of macular edema and anti-VEGF therapy should be initiated or continued. However, in the whole study population, we found a statistically significant increase of visual acuity after FLP. Secondly, the visual outcome in DME substantially depends on a number of factors, including clarity of the optical media and structural changes of the neuroepithelium (disorganization of inner retinal layers and discontinuation of ellipsoid) which limit BCVA improvement. Although such patients were not included in the study, we cannot completely exclude the influence some of those factors on visual outcome. At the same time, retinal thickness is a biomarker for exudation, which is strongly associated with deterioration of visual acuity, and its evaluation is highly precise and reproducible [11, 12]. Comparison of treated and non-treated sectors confirms that changes in retinal thickness are caused by laser treatment and not by general improvement of patients’ systemic status. Non-treated sectors, therefore, serve as a control, and this leads us to conclude that changes in main outcome measures (CRT and macular volume) resulted from the laser treatment.
At 1 month after FLP, we did not find a statistically significant difference in the reduction of CRT and macular volume between the study groups. At the end of follow-up, the reduction of CRT was significantly higher in eyes where FLP was planned using en face OCT compared to those where the procedure was planned using FA. However, at the same time, there was no difference in the change of macular volume. We can, therefore, conclude that the difference in CRT reduction between study groups at the end of follow-up is likely to be accidental. It is worth noting that our previous study showed that en face OCT reveals up to 50% more microaneurysms than FA [10]. Nevertheless, there is no evidence that laser treatment planned using en face OCT is superior to conventional FA-guided FLP in terms of reduction of retinal exudation.
In this study, in the en face OCT-planning group, we targeted only microaneurysms which met the previously established OCT criteria for leaky microaneurysms [10]. These leaky microaneurysms take place in the deep capillary plexus and typically demonstrate a moderately reflective appearance and an association with intraretinal cystic fluid, but without the “ring sign”. This study showed that en face OCT is a non-inferior alternative to FA in terms of identification of leaky microaneurysms for laser treatment, particularly for navigated laser photocoagulation.
The navigated approach is a safe and precise technique which substantially simplifies laser treatment of retinal diseases, although FA is required for treatment planning. Now, with the introduction of OCT angiography, FA is not without an alternative for the diagnosis of many retinal diseases including diabetic retinopathy [13]. Since FA itself is an invasive and time-consuming procedure; today, it can be considered as a non-essential diagnostic option. These changes in retinal imaging simplify clinical workflow unless FA is required for any specific purpose, such as laser treatment planning. Indeed, anti-VEGF treatment requires no FA to be performed because OCT data with BCVA are a guide for the injection regimen [14,15,16]. All of these make intravitreal anti-VEGF treatment not only more effective but also a simpler option compared to laser treatment. The adoption of en face OCT for navigated focal laser photocoagulation planning may simplify laser treatment, facilitates repeat laser treatment, and makes FLP a fully non-invasive procedure.
The use of OCTA images appears to be attractive for FLP planning and the issue for imaging of microaneurysms with OCTA has been considered in several papers. However, we suggest some difficulties with the practical use of OCTA images for FLP planning. Firstly, there is considered to be no absolute agreement in the visualization of microaneurysms between OCTA and FA unless specific methods such as image averaging are used. Secondly, there is no clear indicator to differentiate the leaky status of microaneurysms on OCTA images, although retinal thickening and the form of microaneurysms may help [7]. Finally, some difficulties might be expected in overlaying OCTA image of DCP over the baseline fundus image of the navigated laser system. This problem results from the absence of terminal retinal vessels on the DCP image, which are required for image alignment, since these vessels mostly account for SCP.
In conclusion, en face OCT planning for navigated focal laser photocoagulation appears to be an adequate alternative for FA planning. Laser treatment based on this approach has a non-inferior efficacy compared to conventional FA-based planning in terms of reduction of retinal exudation.
References
Crosson JN, Mason L, Mason JO (2017) The role of focal laser in the anti-vascular endothelial growth factor era. Ophthalmol Eye Dis 9:1179172117738240
Blindbaek SL, Peto T, Grauslund J (2019) How do we evaluate the role of focal/grid photocoagulation in the treatment of diabetic macular edema? Acta Ophthalmol 97:339–346
Hirano T, Toriyama Y, Iesato Y et al (2019) Effect of leaking foveal microaneurysms on the treatment of center-involving diabetic macular edema: a pilot study. Ophthalmic Res 61:10–18
Kernt M, Cheuteu RE, Cserhati S et al (2012) Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol 6:289–296
Kozak I, Oster SF, Cortes MA et al (2011) Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology 118:1119–1124
Miwa Y, Murakami T, Suzuma K et al (2016) Relationship between functional and structural changes in diabetic vessels in optical coherence tomography angiography. Sci Rep 6:29064
Schreur V, Domanian A, Liefers B et al (2019) Morphological and topographical appearance of microaneurysms on optical coherence tomography angiography. Br J Ophthalmol 103:630–635
Yannuzzi LA, Rohrer KT, Tindel L et al (1986) Fluorescein angiography complication survey. Ophthalmology 93:611–617
Kwiterovich KA, Maguire MG, Murphy RP et al (1991) Frequency of adverse systemic reactions after fluorescein angiography. Results of a prospective study. Ophthalmology 98:1139–1142
Maltsev DS, Kulikov AN, Burnasheva MA, Kazak AA, Chhablani J (2019) Structural en face optical coherence tomography imaging for identification of leaky microaneurysms in diabetic macular edema. Int Ophthalmol [Epub ahead of print]
Ou WC, Brown DM, Payne JF, Wykoff CC (2017) Relationship between visual acuity and retinal thickness during anti-vascular endothelial growth factor therapy for retinal diseases. Am J Ophthalmol 180:8–17
Nourinia R, Ahmadieh H, Nekoei E, Malekifar P, Tofighi Z (2018) Changes in central choroidal thickness after treatment of diabetic macular edema with intravitreal bevacizumab correlation with central macular thickness and best-corrected visual acuity. Retina 38:970–975
Akil H, Karst S, Heisler M et al (2019) Application of optical coherence tomography angiography in diabetic retinopathy: a comprehensive review. Can J Ophthalmol 54:519–528
Elman MJ, Aiello LP, Beck RW et al (2010) Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 117:1064–1077
Korobelnik JF, Do DV, Schmidt-Erfurth U et al (2014) Intravitreal aflibercept for diabetic macular edema. Ophthalmology 121:2247–2254
Wells JA, Glassman AR, Ayala AR et al (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 372:1193–1203
Funding
The authors have not received any grant support for this study. The authors have no proprietary or financial interest in any aspect of this report. The authors confirm that this study has not been presented at any meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maltsev, D.S., Kulikov, A.N., Burnasheva, M.A. et al. Efficacy of navigated focal laser photocoagulation in diabetic macular edema planned with en face optical coherence tomography versus fluorescein angiography. Int Ophthalmol 40, 1913–1921 (2020). https://doi.org/10.1007/s10792-020-01363-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01363-y