Abstract
Headings
Multifocal electroretinography (mfERG) may be useful in the management of sector retinitis pigmentosa (SRP).
Aim
To compare multifocal electroretinographic responses in SRP, generalised retinitis pigmentosa (GRP), and healthy controls.
Methods
Eighteen patients with SRP, twelve with GRP, and fifteen controls were included in the study. All participants underwent: complete ophthalmological examination, Humphrey visual field testing, full-field ERG, and mfERG. The mean P1 amplitude, the implicit time (IT), and the mapping of the local responses were evaluated.
Results
The mean P1 amplitude was higher in the SRPs than in GRPs (p < 0.001), while it did not differ between SRPs and controls (p = 0.913). In the SRPs, the P1 amplitude in pathologic areas was higher than in the GRPs (p < 0.001). In normal areas, this parameter did not differ from the controls (p = 0.499). Moreover, in the SRPs, no differences in the P1 amplitude and the IT between pigmented and non-pigmented areas were found.
Conclusion
In the present study, the mfERG examination displayed significant differences between sector and generalised RP, showing normal values in sector RP even in pigmented areas. Considering the patients included in this study, SRP seems to represent a favourable variant of the disease, characterised by a limited retinal involvement and apparently mild functional damage. It is still unclear how these results can be extended to other forms of SRP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sector retinitis pigmentosa (SRP) is a rare form of RP, accounting for less than 2% of the total RPs [1] and first described by Bietti in 1937 [2]. This variant is characterised by typical pigmentary changes limited to one or two retinal quadrants and visual field defects consistent with the fundus appearance [3,4,5]. It is assumed that SRP has a better visual prognosis than generalised RP (GRP), because it is typically stable and progresses very seldom to GRP [6].
Previous electrophysiological studies, conducted by full-field ERG (ffERG), have shown subnormal amplitudes of the b-wave in SRP eyes. Anyway, the alterations on ffERG are usually less severe than in GRP [7,8,9,10]. Multifocal ERG (mfERG) is a technique which provides a map of central retinal electrophysiological activity allowing to assess localised photopic function, therefore defining macular involvement in several diseases, including RP and its variants. Contrasting data on mfERG findings in SRP are currently available; however, reports have suggested a role for mfERG in the clinical management of patients with SRP [11,12,13,14,15,16,17,18,19].
The present study was conducted to evaluate and compare the mfERG responses in patients with sector or generalised retinitis pigmentosa and in healthy controls.
Materials and methods
Medical records of eighteen patients affected by SRP, twelve with GRP, and fifteen healthy controls recruited through the Hereditary Retinal Degenerations Referring Centre of the Azienda Ospedaliero-Universitaria Careggi, Firenze, Italy, were retrospectively reviewed and included in the study. One eye of each subject was randomly chosen for the examinations, as the clinical features were similar in both eyes of all the subjects. The inclusion criteria for the patients were: diagnosis of GRP and SRP based on typical ophthalmoscopic fundus appearance, consistent visual field defects on Humphrey 30-2 testing, and ffERG findings. In particular, we classified as sector RP only the cases in whom both morphological (fundus appearance) and functional (visual field) abnormalities were consistent and limited to one or two fundus sectors. The exclusion criteria were: Snellen best-corrected visual acuity < 0.8 decimals, myopia or hyperopia ≥ 3 diopters, astigmatism ≥ 1.5 diopters, media opacities, cystoid macular oedema, and any other ocular disorders than RP. The tenets of the Declaration of Helsinki were upheld, and the protocol was approved by the local ethics committee. A written informed consent was obtained by each participant.
All the studied subjects underwent a standard ophthalmological examination including Snellen visual acuity evaluation, intraocular pressure measurement, anterior and posterior segment biomicroscopy.
After pupillary dilation with 1% tropicamide and correction of refractive errors, a standard ffERG was obtained by a protocol in accord with the ISCEV guidelines [20].
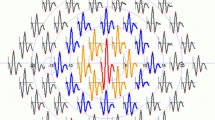
A multifocal ERG (mfERG) by means of RETI-scan 201 B4 (Roland Consult, Brandenburg, Germany) was then performed, to better evaluate the central retinal function. The electroretinographic responses were elicited at a viewing distance of 33 cm using an array of 61 hexagons covering a visual field of 30° around the fixation site. The radius of the central hexagonal element was 2°. The stimuli were presented monocularly on a monitor with a frame rate of 75 Hz and a mean luminance of 51.8 cd/m2. A 2-mm-diameter red central fixation cross was used. During the stimulation, each element was either black or white (93% contrast). The responses were recorded using silver HK-loop electrodes. Each recording session was subdivided into eight recording phases of 60-s duration for each eye. The signal was 100,000 times amplified and band-pass filtered between 10 and 100 Hz. For the analysis of the mfERG amplitudes, the peak amplitude, which is the difference between the first negative deflection (N1) and the subsequent positive deflection (P1), was calculated. In the text, this parameter will be named P1 amplitude. For the mfERG timing, the implicit time (IT) of P1 was considered. The mean value of the P1 amplitude and of the IT in all the 61 stimulated points was registered in the three groups. In the SRP group, the mean P1 amplitude and the IT were calculated in each retinal quadrant in order to compare the electrophysiological findings in the normal areas to the ones in the pathological areas, as detected by fundoscopy.
An Excel database (Microsoft Excel 2010, Microsoft Office Professional Plus 2010) was used to record all the data. The data, presented as mean ± standard deviation (SD), were analysed by means of Stata 13.1 software (StataCorp LP, College Station, TX, USA), using the Student’s t test and the Wilcoxon rank sum test. The intergroup comparisons and the ones between pigmented and non-pigmented sectors were conducted using linear mixed models accounting for correlated data at the subject and eye levels. The statistical significance was set at a p value < 0.05.
Results
The demographic and clinical characteristics of the study population are outlined in Table 1.
In the SRP group, thirteen patients (72.22%) showed only one altered sector, while in five patients (27.78%), two sectors were altered.
Table 2 details the full-field ERG results, showing that the amplitudes were lower in the GRPs than in the SRPs and the controls, while the implicit times were comparable across the three groups. Post hoc analyses revealed that the combined and scotopic ERG amplitudes were decreased in the GRPs compared to the SRPs and in the SRPs compared to the controls (p < 0.05 for all comparisons). Of note, subjects with SRP and controls did not differ in terms of photopic ERG amplitude (p = 0.611).
Regarding the mfERG, the mean P1 amplitude was lower and the mean IT time higher in the GRPs than in the SRPs and the controls (3.20 ± 1.43 μV/deg2, 11.84 ± 4.90 μV/deg2, 12.38 ± 4.17 μV/deg2, p < 0.001, and 41.41 ± 6.91 ms, 39.12 ± 4.97 ms, 37.87 ± 5.36, p < 0.001). Post hoc analyses disclosed that the mean P1 amplitude was greater in the SRPs than in the GRPs (p < 0.001), while it did not differ between the SRPs and the controls (p = 0.505). The mean IT was longer in the GRPs than in the SRPs (p = 0.037), not in the SRPs compared to the controls (p = 0.167).
Subsequently, we analysed the mfERG measures in the four quadrants, in order to compare the ophthalmoscopically altered (pigmented) sectors to the normal (non-pigmented) ones.
In the SRP group, we found no differences in the P1 and IT between pigmented and non-pigmented sectors (see Table 1). The comparisons between the mfERG measures in pigmented and non-pigmented sectors across the three different groups are outlined in Table 3.
The mean P1 amplitude in pigmented sectors of the SRPs was significantly higher in comparison with the GRPs. (p < 0.001). Conversely, the mean value of the apparently normal areas of the SRPs did not differ from the controls (p = 0.371). No statistically significant differences were found when comparing the mean IT in pigmented sectors of the SRPs to the GRPs and in non-pigmented sectors of the SRPs to the controls. The IT measures in the pigmented quadrants did not differ significantly from the non-pigmented ones. Results are shown in Figs. 1 and 2.
Discussion
In the present study, a multifocal ERG examination was performed to compare the responses in sector retinitis pigmentosa (SRP), generalised retinitis pigmentosa (GRP), and controls.
Our results showed that the mean P1 amplitude measured in the SRPs was significantly higher than in GRPs and only slightly reduced, with no statistical significance, when compared to the controls.
Moreover, in the SRPs, the mean P1 amplitude in ophthalmoscopically altered areas was comparable to the normal ones. Conversely, this parameter significantly differed between the GRPs and the SRPs, being markedly greater in the latter group.
Retinitis pigmentosa comprises a variety of clinical entities, associated with very different visual outcomes. SRP is considered a relatively benign variant of the disease, characterised by a mild visual impairment and a rare progression to GRP [3].
According to the literature, electrophysiology particularly ERG is an important tool in the management of SRP [5, 6, 10,11,12,13,14]. The Ganzfeld electroretinographic responses have higher amplitude in SRP than in GRP ones and often are within the normality range [5,6,7,8,9,10,11]. The multifocal technique, by a simultaneous measurement of the ERG activity of many retinal locations, provides an objective, detailed assessment of the retinal function that can be useful in localised forms of RP [12,13,14,15,16,17,18,19]. In fact, the ffERG is altered when at least 30% of the photoreceptors is lost, while the mfERG discloses localised responses, so that it can differentiate between affected and non-affected retinal areas [21]. This has a high clinical relevance, because in SRP cases, the detection of the spatial extent of the retinal dysfunction is crucial to determine the severity of the condition and to follow it up. Hence, mfERG may have advantage over ffERG for the detection of a functional damage which is not yet revealed by the funduscopic examination [10, 18].
The mfERG has proved its utility in detecting preclinical alterations in RP carriers and in characterising the local retinal function in patients with early RP [22, 23]. In addition, it may be helpful in assessing the residual retinal function in severe, advanced forms of RP [24]. The usefulness of this technique in SRP should rely on the opportunity of making an early diagnosis of retinal dysfunction, in apparently healthy areas.
In the literature, there are contrasting data about the topography of retinal damage in SRP. Some investigations have showed that the severity of the ERG alterations is directly correlated with the “amount” of pigmented quadrants [2, 6]. Moreover, several studies have denied a clinical progression over a long-term follow-up, supporting the hypothesis of a stable disease [4, 7, 8].
At present, data about the mfERG examination in SRP are based on a few case reports or small case series and are inconclusive. In fact, Scholl et al. [19] observed altered mfERG features even in unaffected fundus regions in two SRP patients. Similarly, Iijima et al. [10] and Yoshii et al. [17] have showed electroretinographic abnormalities also in normally appearing retinal quadrants in their casistics of SRP. On the contrary, Palmowski et al. [18] have reported altered mfERG responses in pigmented areas and normal responses in non-pigmented ones in two SRP women, confirming the data obtained by Hood et al. [14, 15].
Our study, to our knowledge, is the first specifically aimed to investigate the mfERG responses in a group of SRP patients, in comparison with GRPs and controls. In our casistics, the mfERG examination has clearly showed significant differences among the three groups. Clinically relevant findings of this investigation are the presence of significantly greater amplitudes in SRPs than in GRPs and the detection of functionally preserved photoreceptors in retinal areas appearing both normal and altered at the fundoscopic examination. Of note, the mean P1 amplitude measured either in pathological or normal sectors of the SRPs was comparable to the controls, whereas it was significantly higher than in the GRPs. The mfERG responses were in the normality range both in pigmented and non-pigmented sectors of SRPs.
Based on our results, we believe that the relatively normal mfERG findings in the SRP group are likely due to a different severity of the disease. We assume that the SRP eyes, because of their significantly altered ffERG measures, are pathologic compared to the controls. However, a less severe form of RP in these eyes seems to account for such relatively normal mfERG measures. Analyses on a larger sample are certainly needed to confirm our present data.
Our study has some limitations. The sample size is relatively small, and the subjects are mainly young adults (mean age = ~ 35 y/o); thus, the bioelectric retinal responses might have been influenced by the age. Moreover, we recruited the patients according to strict inclusion criteria (topographically limited and consistent fundoscopy and visual field abnormalities). We excluded atypical cases, where the alterations of the fundus and the visual field were not consistent, and we did not consider longitudinal data reporting the natural history of the patients (e.g. the possible transition from SRP into GRP in the same patient). Lastly, we did not study the ERG differences between the two subgroups of SRP, with only one and with two affected quadrants, because the small sample size would have prevented from obtaining statistically reliable results.
In conclusion, our findings support the assumption that SRP should be differentiated from GRP in terms of retinal functional impairment and probably also in terms of clinical severity, as it seems to be a relatively benign type of RP. Our study confirms the clinical utility of mfERG in differentiating typical and atypical forms of the disease. Even though the exact pathogenetical mechanism is still obscure, our data might provide novel understanding of the disease and warrant further investigations. Larger studies are required to clarify whether our results could be reported in a peculiar and limited series or can be more widely generalised to the majority of SRP patients. Moreover, longitudinal studies with structure–function correlation are warranted to establish whether localised forms of RP may be considered as stable or may progress in terms of functional damage over time.
References
Krill AE, Archer D, Martin D (1970) Sector retinitis pigmentosa. Am J Ophthalmol 69:977–987
Bietti G (1937) Su alcune forme atipiche o rare di degenerazione retinica (degenerazioni tapetoretiniche e quadri morbosi similari). Boll Oculist 16:1159–1244
Farber MD, Fisher GA, Weiss RA (1985) Autosomal dominantly inherited retinitis pigmentosa. Visual acuity loss by subtype. Arch Ophthalmol 103:524–528
Lessel MR, Thaler AR, Heilig P (1986) Localized forms of retinopathia pigmentosa. Wien Klin Wochenschr 98:264–269
Van Voerkom C, Ferrucci S (2005) Sector retinitis pigmentosa. Optometry 76:309–317
Moszczynska-Kowalska A, Drobecka-Brydakova E (1990) 12-year observation of atypical retinitis pigmentosa. Klin Oczna 92:28–30
Berson EL (1981) Retinitis pigmentosa and allied diseases: applications of electroretinographic testing. Int Ophthalmol 4:7–22
Berson EL (1987) Electroretinographic findings in retinitis pigmentosa. Jpn J Ophthalmol 31:327–348
Fulton AB, Hansen RM (1988) The relation of rhodopsin and scotopic retinal sensitivity in sector retinitis pigmentosa. Am J Ophthalmol 105:132–140
Iijima H, Yamaguchi S, Kogure S et al (1992) Static perimetry and temporal aspects of the photopic electroretinogram in sector retinitis pigmentosa. Nippon Ganka Gakkai Zasshi 96:243–250
Jampol LM (2006) Autofluorescence and visual field loss in sector retinitis pigmentosa. Retina 26:248–250
Kondo M, Miyake Y, Horiguchi M et al (1995) Clinical evaluation of multifocal electroretinogram. Invest Ophthalmol Vis Sci 36:2146–2150
Seeliger M, Kretschmann U, Apfelstedt-Sylla E et al (1998) Multifocal electroretinography in retinitis pigmentosa. Am J Ophthalmol 125:214–226
Hood DC, Holopigian K, Greenstein V et al (1998) Assessment of local retinal function in patients with retinitis pigmentosa using the multi-focal ERG technique. Vis Res 38:163–179
Hood DC (2000) Assessing retinal function with the multifocal technique. Prog Retin Eye Dis 19:607–646
Chan HL, Brown B (1995) Investigation of retinitis pigmentosa using the multifocal electroretinogram. Ophthal Physiol Opt 18:335–350
Yoshii M, Murakami A, Akeo K et al (1998) Visual function in retinitis pigmentosa related to a codon 15 rhodopsin gene mutation. Ophthalmic Res 30:1–10
Palmowski AM, Allgayer R, Heinemann-Vernaleken B et al (2001) A differentiated study of the retinal function in segmental retinitis pigmentosa by multifocal electroretinograms. Ophthalmologe 98:294–299
Scholl HPN, Kremers J (2003) L- and M-cone driven large-field and multifocal electroretinograms in sector retinitis pigmentosa. Doc Ophthalmol 106:171–181
Hood DC, Bach M, Brigell M, Keating D, Kondo M, Lyons JS, Marmor MF, McCulloch DL, Palmowski-Wolfe AM (2012) ISCEV standard for clinical multifocal electroretinography (2011 edition). Doc Ophthalmol 124:1–13
Jacobi PC, Miliczek K, Zrenner E (1993) Experiences with the international standard for clinical practice, interindividual and intraindividual variations and possible extensions. Doc Ophthalmol 85:95–114
Vajaranant TS, Seiple W, Szlyk JP et al (2002) Detection using the multifocal electroretinogram of mosaic retinal dysfunction in carriers of X-linked retinitis pigmentosa. Ophthalmology 109:560–568
Robson AG, Saihan Z, Jenkins SA et al (2006) Functional characterisation and serial imaging of abnormal fundus autofluorescence in patients with retinitis pigmentosa and normal visual acuity. Br J Ophthalmol 90:472–479
Gränse L, Ponjavic V, Andreásson S (2004) Full-field ERG, multifocal ERG and multifocal VEP in patients with retinitis pigmentosa and residual visual fields. Acta Ophthalmol Scand 82:701–706
Funding
This study was supported by the Ente Cassa di Risparmio di Firenze. The authors and the sponsor designed this research together.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflict of interest with the submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giambene, B., Verdina, T., Pennino, M. et al. Multifocal electroretinographic responses in sector retinitis pigmentosa. Int Ophthalmol 40, 703–708 (2020). https://doi.org/10.1007/s10792-019-01231-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01231-4