Abstract
Purpose
Potential factors influencing stereopsis were investigated in patients with both refractive accommodative esotropia (RAE) and amblyopia.
Materials and methods
A retrospective chart review was performed to find out all patients with the diagnosis of both RAE and amblyopia. Patients are classified into two groups: group 1 (with stereopsis) and group 2 (without stereopsis). Onset age of RAE, history of strabismus in family members, time of amblyopia treatment, mean spherical equivalent, anisometropia, ocular movement disorders, especially, overaction of inferior oblique (IO) muscle, visual acuity difference (VAD) between eyes, best-corrected visual acuity (BCVA) levels of amblyopic and normal eyes and the presence of alternation of fixation (AOF) were investigated as possible factors. These factors were compared statistically between groups.
Results
Groups 1 and 2 consisted of 21 and 26 patients, respectively. There was no statistical significant difference in terms of onset age of RAE, family history, amblyopia treatment, BCVA of normal eyes and anisometropia. IO overaction and higher VAD were found to be statistically different between groups (p: 0.019, p: 0.022, respectively). Besides, there was significant difference in terms of AOF and better BCVA in amblyopic eyes (p: 0.000, p: 0.009, respectively).
Conclusion
IO overaction, BCVA in amblyopic eyes, VAD and AOF were found to be potential risk factors for the development of stereopsis in patients with both RAE and amblyopia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Refractive accommodative esotropia (RAE) can be defined as a result of an abnormal activation of the accommodation reflex required to overcome blurring caused by uncorrected hyperopia [1]. The onset of RAE usually occurs 18–48 months of age, and RAE often presents as an intermittent deviation so normal binocular vision can be experienced by these children. Despite the later age of onset and intermittent stage of disease, RAE is frequently associated with the abnormal binocular sensory function [2, 3]. Berk et al. [4] reported that 67.7% of patients with RAE had measurable stereoacuity, but only 24.4% had 40–100 s of arc. Many authors investigated possible factors affecting stereopsis in patients with RAE. Amblylopia, anisometropia, longer duration of esodeviation, residual esodeviation were found to be potential factors affecting stereopsis in patients with RAE [5,6,7,8,9].
Amblyopia can be defined as a neuro-developmental disorder of the visual cortex that arises from abnormal visual experience early in life, affecting between 1 and 4% of the general population [10]. Amblyopia is strongly associated with poor stereoacuity especially in patients with strabismus, recovery of stereoacuity may require more active treatment in strabismic than in anisometropic amblyopia, and strabismic amblyopes do not fare as well as anisometropes in recovering stereoacuity [11]. On the other hand, stereopsis might have been protected in different degrees in patients with RAE and amblyopia together.
In our study, potential factors influencing stereopsis were investigated in patients with both RAE and amblyopia.
Materials and methods
This study was conducted at the Department of Ophthalmology. Prior approval from the institutional review board was taken, and written informed consent was obtained from the parents of each subject. The study was performed in adherence to the Declaration of Helsinki.
A retrospective chart review was performed to find out all patients with the diagnosis of both RAE and amblyopia. Refractive accommodative esotropia was diagnosed when an esodeviation of 10 prism diopters or more was decreased with full-correction glasses and the residual esodeviations both at distance and at near under full correction were smaller than 10 prism diopters. Amblyopia was diagnosed when the uncorrectable difference between best-corrected visual acuities (BCVA) of the patient was two or more Snellen lines.
Stereoacuity was tested using the Titmus test (Stereo Optical, Chicago, IL). Patients viewed the stereogram at a distance of 40 cm while wearing polarizing glasses. The patient was asked to grab the wings of the fly and point to the animal and circle that seemed to “jump off the Page.” The examiner verified results by turning the book upside down to confirm the reversal of the response. If a correct response was made on the preceding target, that target’s disparity was used as the measurement. If that response was incorrect, steps farther back from the target series were made until the correct response was obtained. The last correct target identified was used as the patient’s stereopsis measurement. If the largest disparity could not be passed, it was accepted that there was no stereoacuity. All patients are classified into two groups according to the status of stereopsis. Group 1 consisted of patients with measurable stereopsis, and group 2 was consisted of patients without stereopsis.
The cycloplegic refraction examination was performed by instillation of 1 a drop of 1% cyclopentolate three times in 15 min. Retinoscopy was made 30 min after the last drop. The mean of the spherical equivalent (SE) in both eyes was calculated and used for the statistical analysis. The hyperopic refractive error was fully corrected as initial treatment. Anisometropia was described as more than 1 diopter (D) of refractive error between eyes and noted. The refractive correction was changed when necessary during follow-up time. Visual acuity was measured by using Snellen chart. The differences between visual acuities (VAD) of eyes were noted. Six hours a day, occlusion treatment was prescribed in patients with amblyopia who were younger than 10 years.
The prism cover test was used to measure the angle of deviation in all patients. The presence of alternation of fixation (AOF) was noted on each examination and used in statistical analysis.
The possible influencing factors, which were investigated, were onset age of RAE, history of strabismus in family members, time of amblyopia treatment, SE, anisometropia, ocular movement disorders, especially, overaction of inferior oblique muscle, VAD, visual acuity levels of amblyopic and normal eyes and the presence of AOF. These factors were compared between group 1 (patients with stereopsis) and group 2 (patients without stereopsis).
Statistical analysis was performed by using SPSS 21.0 (Statistical Package for Scientific Studies for Windows, SPSS Inc., Chicago, IL). Nonparametric tests were used. Spearman’s rho correlation test, Fisher exact test and Pearson Chi-square test were used for statistical analysis. p < 0.05 was assumed significant for all analysis.
Results
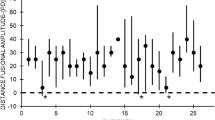
Ten female and 11 male, totally 21, patients were in group 1, and 15 female and 11 male, totally 26, patients were in group 2. The mean ages of group 1 and group 2 were 9.2 ± 2.4 and 7.9 ± 2.9 years, respectively. In group 1, mean stereoacuity was measured as 91.4 ± 93.3 s/arc. The mean follow-up time was measured as 2.5 ± 1.5 years in all patients.
Table 1 reveals the comparisons of possible factors that might have been affected stereoacuity status. The presence of overaction of the inferior oblique muscle was found to relate negatively with stereopsis.
Patients with the presence of alternation of fixation were tended to have stereopsis.
The mean difference between visual acuities of amblyopic and healthy eyes was statistically higher in group 2.
Patients with better BCVA in their amblyopic eyes were found to have stereopsis. However, the number of patients with anisometropia was higher in group 2, and there was no significant statistical difference between groups.
There was no statistical difference in terms of familial strabismus and amblyopia history between groups (p: 0.903)
Discussion
In our study, we investigated potential factors influencing stereopsis in patients with both RAE and amblyopia. We found that the presence of fixation preference was strongly related to loss of stereopsis. Hakim et al. [12] and Erkan Turan et al. [13] found that strong fixation preference was not an indicator for amblyopia in patients with horizontal misalignment. In our study, we also observed that fixation preference does not affect the development of amblyopia because the number of amblyopic patients with fixation preference was less than patients without fixation preference. Fixation preference may not affect amblyopia, but our study revealed that it may effect stereopsis. There were studies investigated stereopsis and RAE, but in our knowledge, it is the first time the investigation was made on fixation preference and its effect on stereopsis.
We knew that the development of stereopsis occurs approximately 15 weeks of age, and 30–100 s of arc stereoacuity was achieved by 40 weeks [14, 15]. The mean onset age of RAE is 18–48 month. So normal stereopsis might be expected in these patients, but many studies stated that the binocular sensory function is not normal in patients with RAE [4, 6, 9]. The relationship between the mean onset age of the RAE and stereopsis was investigated previously. Fawcett et al. [16] found minor influence of onset age on stereopsis. Üretmen et al. [6] did not find significant correlation between mean onset age and stereopsis. We also did not find significant difference in patients with both RAE and amblyopia. The information about the onset age of the RAE was obtained from parents of patients. The onset age at correction of refractive error might be more important in these patients. But parents of patients told that when they realized esotropia, they went to ophthalmologist and took glasses. These unreliable answers of parents could be the cause of different and challenging results.
The relationship between refractive error and stereopsis was investigated previously in patients with RAE, and the authors did not find any relation between these parameters [5, 6, 9]. In our study, in patients with both RAE and amblyopia, there was not a relationship between these parameters, too. The number of patients with anisometropia was lower in patients with stereopsis in our study, but it is not statistically significant. Lee et al. [17] suggested that anisometropia might cause abnormal binocular sensory function in patients with RAE. Each of anisometropia, amblyopia and RAE was poor prognostic factors for stereopsis, but patients with the diagnosis of all might have stereopsis. This item must be investigated in further studies with larger sample size.
In our study, BCVA in amblyopic eyes with stereopsis was found to be better than amblyopic eyes without stereopsis. Güçlü et al. [5] also found a significant relationship between visual acuity and stereopsis. So we can say that amblyopia treatment and full hyperopia correction are essential for the development of stereopsis in patients with both RAE and amblyopia.
We investigated factors which may affect stereopsis in patients with both RAE and amblyopia. So we included patients who had amblyopia. During follow-up, mean BCVA in amblyopic eyes was improved, but the difference between amblyopic and healthy eyes was not decreased below 2 Snellen lines. Üretmen et al. [6] did not find a significant relationship between amblyopia and stereopsis. They also did not find any relationship with amblyopia treatment, whereas Güçlü et al. [5] found significant relationship between amblyopia and poor stereoacuity. In our study, the number of patients who had stereopsis was lower than the number of patients who did not have stereopsis. We also did not find a relationship with amblyopia treatment. But we found statistically significant difference among groups in terms of the difference between visual acuity of amblyopic and healthy eyes. This result suggested us that not amblyopia itself, but the depth of amblyopia might be an influencing factor in these patients. Besides, additional factors should have been existed in patients with amblyopia and RAE and without stereopsis.
Patients with overaction of the inferior oblique muscle were tended to have poor stereopsis, in our study. Üretmen et al. [6] found no significant relation between RAE and overaction of inferior oblique muscle. Weakley et al. observed that especially asymmetric overaction of the inferior oblique muscle was related to amblyopia in patients with esotropia. In this study, esotropia did not classify [18]. We observed that additional vertical deviations might affect stereopsis in patients with both RAE and amblyopia. But we did not assess degrees of overaction of inferior oblique muscle and did not differ which eye had overaction: amblyopic or healthy eye? Further studies are needed on this item.
The main limitations of our study were retrospective design and small sample sizes of groups. Besides, residue deviations after full hyperopia correction were not noted and investigated for a potential factor influencing stereopsis although degrees of inferior oblique overaction were not assessed.
In conclusion, depth of amblyopia, BCVA of the amblyopic eye, strong fixation preference and additional overaction of inferior oblique muscle might be potential factors influencing stereopsis, negatively. More detailed studies should be done to understand better this item.
References
Rutstein RP (2008) Update on accommodative esotropia. Optometry 79:422–431
Birch EE (2003) Binocular sensory function in accommodative esotropia. J AAPOS 7:369–373
Birch EE, Wang J (2009) Stereoacuity outcomes following treatment of infantile AND accommodative esotropia. Optom Vis Sci 86(6):647–652
Berk T, Koçak N, Ellidokuz H (2004) Treatment outcomes in refractive accommodative esotropia. J AAPOS 4:384–388
Güçlü H, Gürlü VP, Özal SA, Özkurt ZG (2015) Prognostic factors for stereopsis in refractive accommodative esotropia. Pak J Med Sci 31(4):807–811
Uretmen O, Köse S, Öztaş S, Eğrilmez S (2007) Factors influencing stereoacuity in refractive accommodative esotropia. Can J Ophthalmol 42(4):600–604
Weakley DR Jr, Birch E, Kip K (2001) The role of anisometropia in the development of accommodative esotropia. J AAPOS 5:153–157
Matsuo T, Yamane T, Fujiwara H, Ohtsuki H, Watanabe Y (2005) Predictive factors for long term outcome of stereoacuity in Japanese patients with pure accommodative esotropia. Strabismus 13:79–84
Fawcett SL, Birch EE (2003) Risk factors for abnormal binocular vision after successful alignment of accommodative esotropia. J AAPOS 7:256–262
Ciuffreda KJ, Levi DM, Selenow A (1991) Amblyopia: basic and clinical aspects. Butterworth-Heinemann, Stoneham
Dennis ML, David CK, Daphne B (2015) Stereopsis and amblyopia: a mini-review. Vis Res 114:17–30
Hakim OM (2007) Association between fixation preference testing and strabismic pseudoamblyopia. J Pediatr Ophthalmol Strabismus 44(3):174–177
Erkan Turan K, Taylan Sekeroglu H, Karahan S, Sanac AS (2017) Fixation preference test: reliability for the detection of amblyopia in patients with strabismus and interexaminer agreement. Int Ophthalmol 37:1305–1310
Birch EE, Petrig B (1996) FPL and VEP measures of fusion, stereopsis and stereoacuity in normal infants. Vis Res 36:1321–1327
Birch EE, Fawcett S, Morale S, Jeffrey B, O’Connor A (2002) Measurement of stereoacuity outcomes during infancy: infant random dot stereocards. Invest Ophthalmol Vis Sci 43:A2937
Fawcett S, Leffler J, Birch EE (2000) Factors influencing stereacuity outcomes in accommodative esotropia. J AAPOS 4:15–20
Lee HJ, Kim S-J, Yu YS (2017) Stereopsis in patients with refractive accommodative esotropia. J AAPOS. https://doi.org/10.1016/j.jaapos.2017.05.009
Weakley DR Jr, Urso RG, Dias CL (1992) Asymmetric inferior oblique overaction and its association with amblyopia in esotropia. Ophthalmology 99(4):590–593
Acknowledgements
The statistical analysis was made by Saliha Yılmaz. Thanks for her work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Human and animal rights
Human participants in this study were in accordance with the ethical standards of institutional research committee. Written informed consent was obtained from the parents of each subject in this study. The study was performed in adherence to the 1964 Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Çakır, B., Bursalı, Ö., Özmen, S. et al. Factors influencing stereopsis in patients with both refractive accommodative esotropia and amblyopia. Int Ophthalmol 39, 1263–1267 (2019). https://doi.org/10.1007/s10792-018-0937-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-0937-8