Abstract
Purpose
To find out the rate of suture requirement and post-operative hypotony in a series of 23-gauge pars plana vitrectomy cases and analyze the factors affecting post-operative hypotony and leakage of sclerotomy leading to suture placement.
Methods
This is a single-center retrospective interventional case series. Eighty-four eyes underwent 23-gauge vitrectomy. Primary endpoint measures were rate of leakage of 23-gauge sclerotomies requiring suture placement at the end of surgery and rate of early post-operative hypotony. Secondary endpoint measures were risk factors for early hypotony and leakage requiring suture placement at the end of surgery.
Results
Suture placement in at least one sclerotomy because of sclerotomy leakage was required in 28.6 % (24 of 84) of eyes at the end of surgery. Early post-operative hypotony was seen in 14.3 % (12 of 84). Silicone oil endotamponade and single-step surgery were found as factors increasing the risk of sclerotomy leakage leading to suture placement. Suture placement was the only significant factor increasing the risk of early post-operative hypotony.
Conclusion
Sclerotomy sutures may be required in 23-gauge surgery, more frequently in cases of single-step sclerotomy and/or silicone oil endotamponade. Meticulous suturation of leaking sclerotomies may decrease the rate of post-operative hypotony.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transconjunctival sutureless 23-gauge vitrectomy has been a significant development in vitreoretinal surgery. By decreasing the need for suture placement, this technique reduces the operating time and post-operative patient dyscomfort. But there are still questions regarding the issues like wound leakage, post-operative hypotony, and endophthalmitis. In the original report by Eckardt [1], sclerotomies were performed by two-step system and neither leakage requiring sclerotomy wound sutures nor post-operative hypotony was reported. Since its introduction, 23-gauge sutureless vitrectomy has been used widely including complicated surgeries [2]. Nevertheless, there have been reports of suture requirement and post-operative hypotony with varying frequencies [3–9]. In this study, we aimed to find out the rate of suture requirement and post-operative hypotony in a series of 23-gauge vitrectomy cases and analyze the factors affecting post-operative hypotony and leakage of sclerotomy leading to suture placement.
Materials and methods
This study was performed according to the tenets of Declaration of Helsinki. Information about the surgical procedure was given to all patients. All patients had signed an informed consent before surgery. We retrospectively evaluated the charts of 84 operations performed on 81 consecutive patients who were operated using the 23-gauge vitrectomy system beginning from the year 2008 to 2010. Patient’s age, gender, indication for surgery, and lens status were recorded. All surgeries were performed by the same surgeon (D.K.). Patients older than 18 who were followed for post-operative first month were included in the study. Only cases of initial pars plana vitrectomy were included, and cases who had a pars plana vitrectomy operation previously were excluded. Primary endpoint measures were rate of leakage of 23-gauge sclerotomies requiring suture placement at the end of surgery and rate of early post-operative hypotony. Secondary endpoint measures were risk factors for early hypotony and leakage requiring suture placement at the end of the surgery.
The intraoperative data regarding the surgical procedure, microcannula insertion method, presence of sutured sclerotomies, and type of tamponade agent used were recorded. Intraocular pressure was measured pre- and post-operatively by applanation tonometry in all eyes. Intraocular pressure of 6 mmHg or lower was defined as hypotony.
Surgical method
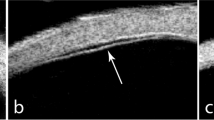
Surgeries were performed using Alcon Accurus 23-gauge one-step vitrectomy system (Accurus, Alcon Surgical, TX) or Dorc 23-gauge one- or two-step vitrectomy systems (DORC, Zuidland, Holland). Excluding the cases where a scleral buckle was placed at the same session, conjunctiva was displaced anteriorly at all times and a pressure plate (DORC, Zuidland, Holland) was used for two-step sclerotomies to fixate the globe for performing the tunnel incision. For one-step sclerotomies, a pressure plate was used to fixate the globe and the trocar was first inserted tangentially through the sclera and parallel to the limbus and then it was oriented perpendicularly. The microcannula was inserted via penetration of the conjunctiva and sclera with the trocar. For two step sclerotomies, the sclerotomy was performed using an angled stiletto blade before the insertion of microcannula. The trocar and microcannula were inserted through the scleral tunnel. Cases in which scleral buckling was performed at the same session, the sclerotomies were performed through bare sclera. Standard three-port sclerotomies were performed; two of which were at superior nasal and temporal and the third was inferior temporal quadrants in all eyes.
A wide-angle viewing system [EIBOS (Haag Streit)] was used. Vitreous base was trimmed by scleral depression in addition to core vitrectomy in all patients. At the end of the operation, microcannulas were removed and leakage from the wound was checked after the conjunctiva overlying the sclerotomy wound was pressed and rubbed to close the scleral tunnel incision for a while using a cotton tipped applicator or forceps. If any leakage was observed, the same procedure was repeated and sutures were placed in cases where wound leakage was present after the second attempt for closure. If phacoemulsification was combined to vitrectomy surgery, the scleral incisions were performed and trocars were placed prior to the anterior segment intervention.
Data analysis
Data were entered into and analyzed with SPSS Statistics for Windows, version 17.0 (SPSS Inc., Chicago, USA). The mean and standard deviation (SD) were calculated for quantitative variables, and proportions (%) were calculated for categorical variables. Fisher exact test was used for the comparison of categorical variables. A p value less than 0.05 was accepted as statistically significant. Logistic regression analysis was also performed to find out risk factors for suture requirement and early post-operative hypotony.
Results
There were 84 eyes of 81 patients to be analyzed fulfilling the inclusion criteria. Mean age of patients was 54.7 ± 16.1 (range 20–84), and 55.6 % were male (45 of 81 patients). Majority of the pathologies leading to pars plana vitrectomy were proliferative diabetic retinopathy, rhegmatogenous retinal detachment, and proliferative vitreoretinopathy (Table 1). The others group in this table included patients operated for dropped nucleus, dislocated intraocular lens, endophthalmitis, intraocular foreign body, macular hole, and vitreous hemorrhage not related to diabetes mellitus.
In 10.7 % of eyes (9 of 84), scleral buckling was performed at the same session with vitrectomy. Cataract extraction with phacoemulsification was combined to pars plana vitrectomy in 16.7 % (14 of 84 eyes), and one patient had a secondary IOL implantation, 34.5 % of eyes (29 of 84) were pseudophakic or aphakic previous to vitreoretinal surgery.
In majority of cases, one-step sclerotomies were performed; 72.6 % (61 of 84). Distribution of single-step and two-step sclerotomies and endotamponade used at the end of surgery are shown in Table 2.
Suture placement was needed in at least one sclerotomy due to sclerotomy leakage in 28.6 % (24 of 84) of eyes at the end of surgery. Thirty-six percent (22 of 61) of cases operated by one-step sclerotomies and 8.7 % (2 of 23) of cases operated by two-step sclerotomies required suture placement at the end of surgery. The rate of suture requirement was significantly higher in cases operated via one step compared to two-step system (p = 0.015, Fischer’s exact test) (Table 3). The rate of suture placement was 44.1 % (15 of 34) in patients with silicone tamponade and 18.0 % (9 of 50) in patients with C3F8 gas, air, or fluid tamponade. This difference was statistically significant (p = 0.014, Fischer’s exact test) (Table 3). In 44.4 % (4 of 9) of eyes with scleral buckling at the same session and 26.7 % (20 of 75) of eyes without scleral buckling at the same session required sclerotomy suture. This difference was not statistically significant (p > 0.05, Fischer’s exact test).
Logistic regression analysis was also performed to find out risk factors for suture requirement and early post-operative hypotony. The variables tested were age, gender, silicone tamponade, C3F8 gas tamponade, air–fluid tamponade, single-step or two-step sclerotomy systems, vitreoretinal pathology leading to surgery, and experience in 23-gauge surgery by analysis with respect to date of the operation. Among these variables tested, silicone oil tamponade and single- or two-step surgery were found to be the only statistically significant factors effecting leakage of sclerotomy leading to suture placement. The odds ratio was higher when tested for silicone oil endotamponade and one-step surgery together than each tested independently (Table 4).
Early post-operative hypotony was seen in 14.3 % (12 of 84) of eyes. Hypotony recovered in all the eyes in the first week. Age, gender, silicone tamponade, C3F8 gas tamponade, air–fluid tamponade, vitreoretinal pathology leading to vitreoretinal surgery, one- or two-step surgery, experience in 23-gauge surgery, and placement of sclerotomy suture for 23-gauge sclerotomy were the variables tested for hypotony (Table 5). The requirement of sclerotomy suture was the only significant factor increasing the risk of early post-operative hypotony (Odds Ratio 4.5, CI 1.3–16.1, p = 0.02).
Discussion
Since Eckardt’s [1] original report of 23-gauge transconjunctival vitrectomy with no suture requirement and hypotony, this surgical technique has acquired widespread use. The rate of sclerotomy leakage requiring suture placement has been reported to range from zero to 38.5 %, and hypotony up to 20 % have been encountered [3–11]. To date, there have been few studies addressing the possible risk factors to find out the features leading to the discrepancy between series for suture requirement and hypotony [5, 6, 11].
Compared to most previous reports [1, 3–6, 8, 9], where the use of silicone oil tamponade was low, we had a much higher rate (40.5 %). This is thought to be due to greater number of complex vitrectomy cases in our series and our preference of silicone endotamponade in such cases as complicated diabetic retinopathy and PVR for longer tamponade effect. Having used both silicone oil and other endotamponade media and both one-step and two-step sclerotomy techniques in the same case series, this study distinguishes from others because we could analyze the risks of suture requirement and post-operative hypotony associated with different sclerotomy techniques and endotamponade media.
There are few studies comparing one- or two-step sclerotomy techniques in 23-gauge vitrectomy. In a study by Choi et al. [12] these two techniques were compared. They found that linear and slit-like sclerotomy wounds formed by MVR blade in two-step procedure are more watertight and more effectively self-sealing compared to the sclerotomy wounds formed by trocar blades of the one-step sclerotomy technique. We used one-step surgery in 72.6 % of our cases, and our rate of suture requirement was 28.6 %. We also found that one-step sclerotomy formation is associated with higher risk of leakage and suture requirement compared to the two-step technique in which MVR blade is used for sclerotomy wound construction.
It should be kept in mind that our cases were recruited between 2008 and 2010. Now, some of the newer one-step trocar systems also features microvitreoretinal stiletto-style blade which can perform a slit-like incision. Some systems use blades with cutting edge which are thougt to form flat, linear incisions and better wound closure. Also, some of the one-step systems include lancet-pointed needle that would have remarkable low piercing and cutting forces. These devlopments may lead to smooth trocar insertion and more efficient wound closure [16]. We see that most of these innovations try to improve wound architecture by changing the blade structures and shapes and achieve a shape similar to MVR blades used in two-step sclerotomy technique. Further studies are needed to compare these newer one-step 23-gauge trocar systems with the two-step systems.
Silicone oil is commonly used in vitreoretinal surgery as a tamponade agent. There are several studies reporting leakage of silicone oil through the sclerotomy sites after pars plana vitrectomy. Cunha et al. [13] made histopathological examination to the conjunctival specimens of patients with prior vitreoretinal surgery and intraocular silicone oil injection. They found that silicone oil was present in 33 % of samples. Siqueira et al. [14] used silicone oil in patients operated with 23-gauge transconjuntival vitrectomy for retinal detachment and found that post-operative silicone oil leakage in subconjuntival space occured in 9.67 % of patients. In these patients, a new procedure was necessary for removal of the subconjuntival silicone and to suture the wounds. In a report presented by Gorovoy et al. [15], a patient who was previously operated with 23-gauge vitrectomy system developed post-operative hypotonia after silicone oil removal in the post-operative first week. The hypotonia resolved without treatment. They report that 6 months later the patient presented with 360° subconjunctival silicone oil droplets that extended 4 mm posterior to equator. Scarring and adhesion of the conjunctiva to the underlying tenon and sclera caused by oil prevented the removal of silicone oil in this case. We found that sclerotomy leakage and suture placement rates are significantly higher in silicone oil endotamponade-used cases compared to C3F8 gas, air, or fluid tamponade.
In this study, we found that silicone endotamponade and one-step sclerotomy were independently associated with increased rate of wound leakage and suture requirement. In addition, in cases operated by one-step technique, silicone oil endotamponade has further increased the risk of leakage and suture requirement. We think that silicone oil itself has a tendency to leak which is enhanced by the sclerotomy wound constructed by one-step technique.
Peripheral vitreous has been proposed to act as a plug preventing leakage from the wound, and therefore the amount of vitrectomy has been speculated to have a role in sclerotomy wound leakage [10]. Different results were reported in several studies. In a report of two-step 23-gauge transconjunctival vitrectomy series, suture placement rate was 11.2 % and suture requirement was more frequent in cases where peripheral vitrectomy was done [5]. In the same study, younger age and prior vitrectomy were other factors found to increase the risk for suture requirement. In another report of a series of two-step approach, suture placement rate was as low as 3.9 %, although vitreous base was removed with scleral depression. Suture placement rate with 23-gauge and two-step approach was reported by Wimpissinger et al. [7] as 26 % and hypotony as 20 %, extensive vitreous removal was done in this series. In two different reports of 23-gauge transconjunctival vitrectomy and single-step approach, the suture rates were dissimilar: 2.2 % and 29.6 % [8, 9]. In both of the series, core vitrectomy was done. [6] Peripheral vitrectomy with scleral depression was done in all the cases in our study due to the complex nature of the cases, and this may also be a factor that increased the rate of sclerotomy wound leakage and suturing in our study. We did not find an association of age and sclerotomy suturing in the current study.
In a recent study, Duval et al. [11] reported that at least 1 sclerotomy was sutured in 38.5 % of their patients. 5 different surgeons performed 23-gauge vitrectomy, and they used gas (air, SF6 or C3F8) tamponade if necessary in this series. They also divided the patient into two vitrectomy groups depending on the complexity of the surgery. They found that sclerotomy suturing was significantly related to the surgical technique which depends on the surgeon, tamponade agent with lower rate of suturing in gas tamponade-applied cases, and complexity of vitrectomy. Complex vitrectomy cases which require extensive instrument use and torquing of globe-like regmatogenous retinal detachment and proliferative diabetic retinopathy with tractional detachment were associated with high sclerotomy suturing rates in this study. Most of the cases in our study also composed of complex vitrectomy cases like proliferative diabetic retinopathy, rhegmatogenous retinal detachment, and proliferative vitreoretinopathy. We think that this is also a factor for increased rate of leakage and sclerotomy suturing in our study. We could not compare the effect of surgeon, since our cases were operated by the same surgeon, but when we looked at surgeon experience, we could not find an increased risk for hypotony and suture requirement when we compare our cases operated early and late phases of our study period.
Our rate of early post-operative hypotony (14.3 %) is higher compared to some of the previously reported series [1–6, 8, 9]. The only risk factor found for hypotony was suturation of the sclerotomy wound suggesting that sutures were inadequate. We put sutures without opening the conjunctiva in our study. Therefore, suturation should be done more meticulously and if necessary, conjunctiva should be opened to visualize the scleral wound properly in order to decrease the rate of early post-operative hypotony.
The retrospective nature of this study is a limitation which can limit data analysis and allow possible biases. Also, our sample size and heterogeneity of number of cases in subgroups are other limitations of our study and should be kept in mind when interpreting the results. Prospective studies with larger sample sizes are necessary in this subject. In conclusion, our study suggests that the risk of sclerotomy leakage and suture placement is increased in 23-gauge vitrectomy cases especially with one-step sclerotomy technique and silicone oil endotamponade. Careful examination of the sclerotomy sites for leakage and appropriate suture placement is necessary especially in these cases to prevent complications.
References
Eckardt C (2005) Transconjunctival sutureless 23-gauge vitrectomy. Retina 25:208–211
Oliveira LB, Reis PA (2007) Silicone oil tamponade in 23-gauge transconjunctival sutureless vitrectomy. Retina 27:1054–1058
Lott MN, Manning MH, Singh J et al (2008) 23-Gauge vitrectomy in 100 eyes: short-term visual outcomes and complications. Retina 28:1193–1200
Fine HF, Iranmanesh R, Iturralde D, Spaide RF (2007) Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology 114:1197–1200
Woo SJ, Park KH, Hwang JM et al (2009) Risk factors associated with sclerotomy leakage and postoperative hypotony after 23-gauge transconjunctival sutureless vitrectomy. Retina 29:456–463
Parolini B, Prigione G, Romanelli F et al (2010) Postoperative complications and intraocular pressure in 943 consecutive cases of 23-gauge transconjunctival pars plana vitrectomy with 1-year follow-up. Retina 30:107–111
Wimpissinger B, Kellner L, Brannath W et al (2008) 23-Gauge versus 20-gauge system for pars plana vitrectomy: a prospective randomised clinical trial. Br J Ophthalmol 92:1483–1487
Gupta OP, Ho AC, Kaiser PK et al (2008) Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol 146:193–197
Chieh JJ, Rogers AH, Wiegand TW et al (2009) Short-term safety of 23-gauge single-step transconjunctival vitrectomy surgery. Retina 29:1486–1490
Amato JE, Akduman L (2007) Incidence of complications in 25-gauge transconjunctival sutureless vitrectomy based on the surgical indications. Ophthalmic Surg Lasers Imaging 38:100–102
Duval R, Hui JM, Rezaei KA (2014) Rate of sclerotomy suturing in 23-gauge primary vitrectomy. Retina 34(4):679–683
Choi KS, Kim HD, Lee SJ (2010) Sclerotomy site leakage according to wound shape in 23-gauge microincisional vitrectomy surgery. Curr Eye Res 35(6):499–504
Cunha LP, Primiano Júnior HP, Nakashima A, Trein Júnior JA, Ghanem RC, Santo RM, Nakashima Y (2007) Subconjunctival deposit of silicone oil after vitreoretinal surgery. Arq Bras Oftalmol 70(4):589–592
Siqueira RC, Gil AD, Jorge R (2007) Retinal detachment surgery with silicone oil injection in transconjunctival sutureless 23-gauge vitrectomy. Arq Bras Oftalmol 70(6):905–909
Gorovoy IR, Stewart JM (2013) 360° subconjunctival silicone oil after unsutured 23-gauge vitrectomy. Eye 27(7):894–895
Meyer CH, Kaymak H, Liu Z et al (2014) Geometry, penetration force, and cutting profile of different 23-gauge trocars systems for pars plana vitrectomy. Retina 34(11):2290–2299
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no commercial, proprietary, financial interest in the material presented in this manuscript.
Rights and permissions
About this article
Cite this article
Küçük, E., Yılmaz, U., Zor, K.R. et al. Risk factors for suture requirement and early hypotony in 23-gauge vitrectomy for complex vitreoretinal diseases. Int Ophthalmol 37, 989–994 (2017). https://doi.org/10.1007/s10792-016-0361-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0361-x