Abstract
The purpose of this study was to describe the incidence, clinical characteristics, and outcome of eccentric macular holes presenting after vitrectomy and internal limiting membrane (ILM) peeling for the treatment of macular pathology and discuss the pathogenesis of holes formation. A retrospective, noncomparative, interventional case-series study of five patients who developed eccentric macular holes postoperatively following vitrectomy in 198 consecutive patients who underwent ILM peeling for idiopathic macular hole and epiretinal membrane formation between 2008 and 2015. Five patients (2.5 %) developed full-thickness eccentric macular holes postoperatively. Three patients presented with a single eccentric macular hole, one patient had an eccentric hole after a failed idiopathic macular hole surgery and one patient developed four eccentric macular holes. The mean diameter of the holes was 584 μm (range 206–1317 μm) and the average time of holes formation after vitrectomy was 27.7 weeks (range 1–140 weeks). Postoperative best-corrected visual acuity ranged from “counting fingers” to 20/25. The eyes with the holes distant from the fovea had the best final visual acuity. No further intervention was attempted and no complications occurred. The mean follow-up time was 26.8 months. The postoperative macular holes after vitrectomy and ILM peeling were variable in number, size, and time of appearance but remained stable and were not associated with any complications. The pathogenesis of macular holes is most consistent with contraction of the residual ILM or secondary epimacular proliferation probably stimulated by ILM peeling.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The postoperative eccentric macular hole formation is a rare complication after vitrectomy with internal limiting membrane (ILM) peeling for epiretinal membrane (ERM) or macular hole (MH) treatment. Iatrogenic full-thickness macular holes were first described by Rubinstein et al. [1] in 2005 and since then only a small number of cases have been reported [2–7]. Postoperative macular holes may be either lamellar or full-thickness and located centrally [5], paracentrally [2, 4], or eccentrically [1, 3, 5–7]. Several theories have been proposed concerning the pathogenesis implicated, including ILM removal itself [2], mechanical surgical trauma of nerve fiber layer [1, 3], contraction of residual ILM [3], and cystoid macular edema [2] but no general consensus exists.
The aim of this study is to present the incidence, clinical characteristics, and outcome of postoperative macular holes following the ILM removal for the treatment of idiopathic epimacular membranes and macular holes, and discuss the possible mechanisms of occurrence.
Methods
A retrospective, noncomparative, interventional case-series study of five patients who postoperatively developed full-thickness eccentric macular holes, following vitrectomy and ILM peeling. The notes of 198 patients who underwent 23-gauge and 25-gauge pars plana vitrectomy with ILM removal for ERM (114 eyes) and MH (84 eyes) treatment were reviewed. All operations were performed by a single surgeon (D.B.) between 2008 and 2015. Core vitrectomy was followed by surgical creation of posterior vitreous detachment, if not already detached. Indocyanine green (ICG) dye (0.05 %) was used to help ILM peeling in all cases.
In MH surgery, gas tamponade with 20 % sulfur hexafluoride (SF6) was used, and postoperatively patients were postured face down for three days.
Five patients (5 eyes) were found to have postoperative full-thickness eccentric macular holes; two cases presented after ERM surgery and three cases following MH surgery. The term “eccentric macular holes” was used for all the holes located outside the fovea but within the macula. The characteristics of macular holes were studied with fundoscopy, fundus photography, autofluorescence, and optical coherence tomography (OCT, Stratus or Spectralis). The data collected concerning the eyes with macular holes were based on both patients’ notes and surgical video records. The parameters studied were hole location, hole diameter, time interval between operation and macular hole appearance, follow-up period, preoperative and postoperative best-corrected visual acuity (BCVA), additional operations, and age and gender of patients.
Descriptive statistics were performed and values are presented as mean with range (lower–upper value).
Results
The mean age of patients, who developed postoperative eccentric macular holes, was 69.4 years with a range from 65 to 73 years and a male to female ratio 4:1. No other ocular diseases were present except for the idiopathic ERM or MH in the patients. The mean follow-up time was 26.8 months (range 6–56 months). Postoperative macular holes occurred in five cases (incidence 2.5 %). The characteristics of the patients are shown in Table 1.
Three patients presented with a single eccentric macular hole, one patient (case 4) with two macular holes and one patient (case 5) developed four eccentric macular holes (Fig. 1a–c). Case 4, which had a preoperative idiopathic macular hole, presented with a central macular hole which failed to close postoperatively and an eccentric macular hole was located temporally to the original macular hole. Macular holes were located temporally to the fovea in three cases, inferiorly in one case and superiorly in one case.
In case 5, four eccentric macular holes were found after vitrectomy for ERM peeling. Initially, one hole temporally to fovea was found 1 week after surgery, and 15 weeks later, three additional eccentric holes were evident close to the first.
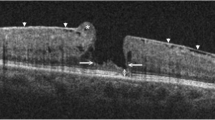
In case 4, postoperative epiretinal membrane associated with cystoid edema was developed lateral to the original macular hole, which was evident about 3 years after the operation and 2 months later it led to eccentric macular hole formation, based on OCT images (Fig. 2).
Case 4: Postoperative eccentric macular hole lateral to central macular hole that failed to close after surgery. a OCT image showing epiretinal membrane and cystoid edema lateral to central macular hole about 3 years after surgery. b Corresponding OCT image showing eccentric full-thickness macular hole lateral to the central macular hole and enlargement of the central hole 2 months later
The mean diameter of holes was 584 μm (range 206–1317 μm). The average time of holes formation after vitrectomy was 27.7 weeks with a range from 1 to 140 weeks.
Postoperative BCVA ranged from “counting fingers” to 20/25. The eyes with the holes distant from the fovea had the best final visual acuity and the case with the central and eccentric macular holes had the poorest visual acuity (counting fingers).
Fundus autofluorescence imaging revealed hyperautofluorescence at the site of macular holes (Fig. 1b), and OCT showed flat, full-thickness macular holes (Figs. 1c, 2b).
No change in size of eccentric macular holes was noted during the follow-up period. No retinal detachment occurred in any patient and no additional intervention was attempted in the postoperative period in any case.
Discussion
Postoperative macular hole formation after ILM peeling is an uncommon complication described by few studies in literature. The reported incidence ranges between 0.6 and 2.2 % [3–5]. In our study, 5 patients out of 198, who underwent vitrectomy with ILM peeling for ERM or MH treatment, developed macular holes with an incidence of 2.5 %.
Most of the reported cases with postoperative macular hole formation have described the presence of a single macular hole located either in the area of fovea [2, 4, 5] or extrafoveally [1, 3, 5–7]. However, the occurrence of multiple macular holes has been reported, to the best of our knowledge, only by Steven et al. in 2006 [2]. The authors presented two cases of multiple holes found 10 weeks after a failed macular hole operation in one case and 3 weeks after vitrectomy for epiretinal membrane in the second case. In our case 5, four eccentric macular holes were found. A single hole occurred temporal to fovea 1 week after vitrectomy for ERM peeling and, 15 weeks later, three additional eccentric holes appeared close to the first.
In our case series, the period for macular hole development after vitrectomy varied between 1 and 140 weeks. In previous reports, the onset of hole formation ranged from a few days to several months postoperatively [2, 3], with a maximum reported, up to now, onset of 15 months after surgery [2]. Therefore, the late onset of hole formation in our case 4, approximately 3 years (140 weeks) after vitrectomy, has never been reported.
Rubinstein et al. [1] suggested that eccentric macular holes may represent trauma to the retina due to grasping the ILM with the Eckhart’s forceps, either at the initial site of ILM elevation or subsequent regrasping of the membrane. However, in our case series, the review of operative notes along with surgical video records revealed no evidence of surgical trauma to the retina at the corresponding area of postoperative macular holes and seems to refute this suggestion for the pathogenesis of macular holes.
ILM peeling itself has been proposed to be responsible for weakening of the glial structure of the retina [2] caused by decapitation of Muller cells. Histopathological findings have shown fragments of Muller cells attached to the removed ILM [8]. Since the major function of Muller cells is to maintain the stability of neural retina, glial apoptosis can cause photoreceptor cell apoptosis and full-thickness retinal defects.
ICG dye for staining ILM was used in all our cases with postoperative macular hole formation. Although ICG has been reported to cause retinal pigment epithelium degeneration and photoreceptor toxicity [9, 10], the dye, to our knowledge, has never been suggested to be implicated in the pathogenesis of macular hole formation. Secondary paracentral macular holes have also been developed without the use of any intraocular dye [2, 4] and when brilliant blue [4], triamcinolone [2] or trypan blue [1] were used, which are not considered retinotoxic. It is unlikely that ICG was responsible for the occurrence of postoperative macular holes in our case series.
The contraction of residual ILM or ERM has been suggested as a possible cause of eccentric macular hole formation based mainly on the observation that the holes were located at the limits of the area of ILM peeling [3]. Furthermore, Uemoto et al. [11] reported that the injury associated with ILM peeling may stimulate glial components resulting in an epimacular proliferation response. Indeed, in our case 4, we observed postoperatively on OCT images an epimacular membrane lateral to the original macular hole, which seemed to be the cause of eccentric hole formation. The formation of epimacular membrane and the tangential traction that applies to the macula may also explain the delayed occurrence of the eccentric hole in this case. However, not all the holes in our cases developed epimacular proliferation in the area of peeled ILM. In four cases (cases 1, 2, 3, and 5), the eccentric macular holes occurred adjacent to the residual ILM, based on the review of surgical video records. These observations suggest that tangential traction to the macula either by a secondary epimacular membrane or a residual ILM may plays an important role in the postoperative macular hole pathogenesis.
Steven et al. [2] proposed that preoperative cystoid macular edema may account for the formation of postoperative macular holes by the formation of an opening of intraretinal cysts after ILM removal. In our study, three cases (cases 1, 3, and 4) out of five with postoperative macular holes presented with preoperative intraretinal cysts, suggesting that cystoid macular edema alone cannot be responsible for the formation of all types of macular holes.
A limitation of our study constitutes the selection and information bias, due to the retrospective nature of the study. Nevertheless, the variability in number, size and time of appearance of the uncommon complication of eccentric macular holes following vitrectomy and ILM peeling is highlighted. Moreover, the late onset of hole formation (approximately 3 years) in one of our cases has never been reported up to now. Our study also adds five new cases to a very small number of published cases with postoperative eccentric macular holes and demonstrates via OCT the contraction of the secondary epimacular proliferation as a possible mechanism for the hole formation.
In conclusion, the postoperative macular holes occurring in our patients were variable in number, size, and time of appearance but remained stable and were not associated with any complications. The pathogenesis of macular holes in our study is most consistent with contraction of the residual ILM or secondary epimacular proliferation, stimulated by ILM peeling. However, we cannot exclude the possibility of other mechanisms contributing to the etiology of holes, such as ILM peeling itself or cystoid macular edema.
References
Rubinstein A, Bates R, Benjamin L, Shaikh A (2005) Iatrogenic eccentric full thickness macular holes following vitrectomy with ILM peeling for idiopathic macular holes. Eye 19:1333–1335
Steven P, Laqua H, Wong D, Hoerauf H (2006) Secondary paracentral retinal holes following internal limiting membrane removal. Br J Ophthalmol 90:293–295
Mason JO III, Feist RM, Albert MA Jr (2007) Eccentric macular holes after vitrectomy with peeling of epimacular proliferation. Retina 27:45–48
Sandali O, El Sanharawi M, Basli E et al (2012) Paracentral retinal holes occurring after macular surgery: incidence, clinical features, and evolution. Graefes Arch Clin Exp Ophthalmol 250:1137–1142
Rush RB, Simunovic MP, Aragon AV II, Ysasaga JE (2014) Postoperative macular hole formation after vitrectomy with internal limiting membrane peeling for the treatment of epiretinal membrane. Retina 34:890–896
Yeh S, Bourgeois KA, Benz MS (2007) Full-thickness eccentric macular hole following vitrectomy with internal limiting membrane peeling. Ophthalmic Surg Lasers Imaging 38:59–60
Kozak I, Freeman WR (2006) Nonprogressive extrafoveal retinal hole after foveal epiretinal membrane removal. Am J Ophthalmol 141:769–771
Wolf S, Schnurbusch U, Wiedemann P et al (2004) Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology 111:238–243
Querques G, Prascina F, Iaculli C, Noci ND (2008) Retinal toxicity of indocyanine green. Int Ophthalmol 28:115–118
Karayanan R, Kenney MC, Kamjoo S et al (2005) Toxicity of indocyanine green (ICG) in combination with light on retinal pigment epithelial cells and neurosensory retinal cells. Curr Eye Res 30:471–478
Uemoto R, Yamamoto S, Takeuchi S (2004) Epimacular proliferative response following internal limiting membrane peeling for idiopathic macular holes. Graefes Arch Clin Exp Ophthalmol 242:177–180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol followed the principles in the Declaration of Helsinki. Informed consent was obtained from all patients, and the present study was approved by the institutional review board of “G. Gennimatas” General Hospital, Athens, Greece.
Rights and permissions
About this article
Cite this article
Brouzas, D., Dettoraki, M., Lavaris, A. et al. Postoperative eccentric macular holes after vitrectomy and internal limiting membrane peeling. Int Ophthalmol 37, 643–648 (2017). https://doi.org/10.1007/s10792-016-0320-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0320-6