Abstract
The aim of the study is to investigate the applicability of a newly developed corneal topographer in assessing tear film stability in Indian subjects. A prospective comparative study of 25 Indian subjects with dry eyes attending a tertiary eye care clinic in South India and 25 normal control subjects was conducted. The diagnosis of dry eye was made based on ocular surface disease index questionnaire. Non-invasive tear film break-up time (NI-TBUT) was measured using a new method based on a corneal topographer equipped with modified scan software. The correlations between the NI-TBUT and the traditional fluorescein tear film break-up time (F-TBUT), Schirmer I test values were determined. A total of 50 patients (100 eyes) were included. The values of NI-TBUT were significantly lower than the values of F-TBUT in both the cases (NI-TBUT 5.78 ± 0.8 s and F-TBUT 7.56 ± 0.5 s; p < 0.02) and controls (NI-TBUT 11.66 ± 1 s and F-TBUT 12.92 ± 1.2 s; p < 0.01). NI-TBUT values were significantly lower than the corresponding F-TBUT values in the varying grades of dry eyes. The mean NI-TBUT values in mild dry eyes was 6.42 ± 0.2 s, moderate dry eyes was 4.70 ± 0.3 s and in severe dry eyes was 2.32 ± 1.2 s. There was a significant difference in the NI-TBUT values for cases and controls (p < 0.001). There was a good correlation seen between the NI-TBUT values and the F-TBUT values, Schirmer I values and the ODSI scores. NI-TBUT was found to have a sensitivity of 86.1 % and a specificity of 81.1 % when the cut-off value was kept at 6.2 s. We investigated the performance of a non-invasive technique for measuring tear film stability to aid in the diagnosis of dry eye disease. It is a useful non-invasive objective method for the detection of dry eye, and its varying grades and may be useful in monitoring the efficacy of therapies for dry eye.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dry eye is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface [1]. Dry eye evaluation includes tests for assessment of tear production, tear film stability, ocular surface disorder and various laboratory and histological tests. A study by Serin D et al. ranked tear break-up time (93 %), corneal staining (85 %), tear film assessment (76 %), conjunctival staining (74 %) and Schirmer test (54 %) as the most commonly used diagnostic tests for initial assessment of dry eye [2]. Schirmer test is an invasive test to assess tear production. It is done using Whatman filter paper No.41 (5 × 35 mm) [3]. A cut-off of 5.5 mm is considered significant. Schirmer I measures total tear secretion (reflex and basal tears), and Schirmer II utilises anaesthetic to measure basal secretions. An unstable tear film is one of the most common findings in patients with ocular irritation caused either by reduced aqueous tear production or an increase in tear evaporation, as in the case of meibomian gland disease [4]. The method most frequently used to assess tear film stability is to measure the tear break-up time (TBUT), that is, the time interval between a complete blink and the first appearance of a dry spot in the precorneal tear film [5]. The TBUT can be assessed by invasive and non-invasive techniques. The most commonly employed method in routine clinical practice is Fluorescein Tear Film Break-up Time (F-TBUT). It uses a slit lamp with a cobalt blue light source to view the tear film after the instillation of fluorescein. The first appearance of a dark spot marks the tear break-up time. A F-TBUT time of less than 10 s (s) indicates instability [5]. Despite its wide usage in clinical and research practice, F-TBUT has many lacunae like lack of standardised procedure in terms of method (micropipette or fluorescein strip) and volume of fluorescein instilled, large range of normal values, inaccuracy, non-reproducibility and lack of association with subjective symptoms. Mengher et al. have found that the instillation of fluorescein itself, being invasive, shortens the TBUT [6, 7]. In an attempt to overcome the lacunae of F-TBUT estimation, various non-invasive methods have been developed to assess tear film stability. Mengher et al. [8] first described measuring non-invasive TBUT (NI-TBUT) by projecting a rectangular grid pattern onto 70–80 % of the corneal surface which was viewed through a slit-lamp (xeroscope)-modified bowl perimeter. The distortion of the grid pattern marks the TBUT [8, 9]. Many other instruments have then been developed like observing standard keratometer mires, modified keratometer mires with a HIR-CAL grid [10], a hand-held keratoscope with a Loveridge grid [10]. These instruments all project a white grid on a black background. The Keeler Tearscope and Keeler Tearscope Plus (keeler ophthalmic instruments) with a corneal topography grid attachment [13] project a black grid on a white background. Other instruments are the DR-1 (Kowa Co. Ltd, Japan) [11, 12] or other prototypes [14, 15]. Tear film lipid layer interferometry is another method that has been described to measure the superficial lipid layer of the tear film [16, 17]. Corneal topography with its topographic regularity indices have been used to assess tear film stability [18, 19]. Recently, teat stability analysis system (TSAS) software [20–23] was used with the RT-7000 Auto Refractor-Keratometer (Tomey Corporation, Nagoya, Japan) by Gumus K et al. [24] as a non-invasive kinetic evaluation of TBUT. Hong Jiaxu et al. used a keratograph (Oculus, Wetzlar, Germany) equipped with modified TF-scan software for NI-TBUT measurements [25].
We performed this study to evaluate the NI-TBUT values in normal and dry eye patients identified using the ocular surface disease index (OSDI) questionnaire using a corneal topographer and to find its correlation with different grades of dry eye severity. The correlation of the NI-TBUT values with subjective symptoms as determined by the OSDI scores was assessed.
Materials and methods
This was a prospective comparative study of 25 Indian subjects with dry eye attending a tertiary eye care clinic in South India and 25 normal control subjects recruited from a population based study. An informed written consent was obtained from all the subjects and the study had the approval of the Scientific and the Ethical committee. All subjects were interviewed regarding their medical history. The diagnosis of dry eye was made based on OSDI questionnaire [26]. It has 12 items; 6 for visual function, 3 for ocular symptoms and 3 for environmental triggers. It gives a score from 0 to 100; 100 = complete disability; 0 = no disability. All patients diagnosed with dry eyes were subjected to NI-TBUT using the Optikon Keratron Scout (Optikon, Italy), a corneal topographer, by studying the irregularities in the mires of the Placido disc that is reflected onto the cornea. The instrument shoots 15 high-speed (one picture per second) photographs of the cornea with a projection of Placido disc on the corneal surface (Figs. 1, 2, 3, 4, 5, 6, 7). These pictures are then analysed for irregularities in the mires. The procedure was carried out in a dark room. Subjects were told to blink 2–3 times and then the photographs were taken for 15 s or till the time the patient blinked. The method adopted to identify the irregularity in the mires was the appearance of discontinuity in the mires of at least 3 spots in the central 6 mm. Presuming that the TBUT is 10 s, any patient showing irregularities in the mires before the tenth picture was considered as dry eyes, and the NI-TBUT was recorded in seconds. This was followed by slit-lamp examination, the traditional F-TBUT measurement (2 µL of a preservative free combination of 1 % fluorescein dye) and fluorescein vital staining of the ocular surface, the same criteria of appearance of first dry spot in the central 6 mm of the cornea was taken as TBUT in seconds. The time interval between instillation of fluorescein and recording of F-TBUT was 10 s. Time interval was kept same in all patients. It was made sure that patient did not blink during the recording as it will give false reading. All these examinations were done by a single examiner and finally, the Schirmer I test was performed. The gap between the tests was more than 15 min. Schirmer’s I test was done to assess tear production. A Whatman filter paper with a scale 0–35 mm was used. Patients were asked to sit in a room devoid of any air conditioning or fan and were asked to blink normally.
Results
A total of 50 eyes of 25 dry eye patients (15 females, 10 males) with a mean age of 42.64 ± 14.12 years and 50 eyes of 25 normal control subjects (15 females, 10 males) with a mean age of 48.32 ± 15.1 years were recruited for the study (Table 1). All subjects were of Indian origin. As per the OSDI questionnaire, the cases were divided into mild (14 eyes), moderate (20 eyes) and severe (16 eyes) dry eyes.
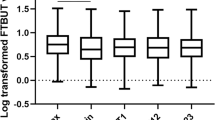
The NI-TBUT values in the cases group were significantly lower (5.78 ± 0.8 s) compared to the control group (11.66 ± 1.0 s, Table 1) There was a significant difference in the NI-TBUT values between the different grades of severity of dry eyes with the severe dry eye group having lowest NI-TBUT values (2.32 ± 1.2 s). The mean NI-TBUT values in moderate dry eyes was 4.70 ± 0.3 s and in the mild dry eyes was 6.42 ± 0.2 s (Table 2) The F-TBUT values were significantly higher than the corresponding NI-TBUT values in all the mild, moderate and severe grades of dry eyes. The F-TBUT values were significantly higher than the NI-TBUT values in both the cases (p < 0.02) and control groups (p < 0.01) (Table 3).
Spearman correlation analysis showed that the values of NI-TBUT in the cases group correlated well with OSDI score (ρ = −0.85; p < 0.001), Schirmer I values (ρ = 0.834; p < 0.001) and F-TBUT values (ρ = 0.919; p < 0.001) (Graphs 1, 2). Similarly, the NI-TBUT values in the control group showed correlation with F-TBUT values (ρ = 0.783; p < 0.001). But there was no significant correlation between NI-TBUT values and OSDI score in controls. NI-TBUT was found to have a sensitivity of 86.1 % and a specificity of 81.1 % when the cut-off value was kept at 6.2 s (Table 4; Graph 3). In comparison, F-TBUT was found to have a sensitivity as well as specificity of 92 % when the cut-off was kept at 10 s.
Discussion
The diagnosis and management of dry eye disease is a challenge in the modern ophthalmologic clinical practice. In today’s world, due to increasing pollution and computer usage, a large number of patients in the younger age group present with dry eye symptoms and require a high standard of care. It is not always easy to objectively quantify dry eye disease [27]. The ophthalmologist is equipped with an arsenal of tests and questionnaires that are substantially subjective and are not necessarily reproducible nor definitive [28]. The OSDI questionnaire provides a subjective grading of dry eye [26]. Of the numerous variables which determine the tear film quantity and quality, the TBUT assesses both by determining the tear film stability [29]. The traditional F-TBUT values are not reproducible and are largely subjective and operator dependent.
The NI-TBUT quantifies both anatomical and physiological function as the deterioration of the mires quality directly affects the visual function by reduction in the quality of image formed at macula [30, 31]. We recommend using non-invasive technique of measuring tear film break-up time with Optikon keratron scout topographer as a reliable objective tool to identify dry eye disease. Using this system, we found that the values of NI-TBUT were significantly lower than those of F-TBUT (p < 0.001) in all the subjects tested. Values of NI-TBUT correlated well with the F-TBUT values as well as with the Schirmer I test values. The values of NI-TBUT progressively decreased with increasing severity of dry eye and correlated well with the OSDI dry eye grading scores. Gumus K et al. [24] measured the NI-TBUT values using the TSAS software for the RT-7000 Auto Refractor-Keratometer. They found the NI-TBUT values well correlating with the severity of dysfunctional tear syndrome (DTS) criteria modified from the dry eye workshop (DEWS) based on the symptom severity scores. They found a cut-off point for ring break-up time (RBUT) of 3.0 s to have optimum sensitivity and specificity of 82.2 % and 88.0 %, respectively.
Hong J. et al. [25] evaluated the efficacy of NI-TBUT values measured using the keratograph (Oculus, Wetzlar, Germany) equipped with modified tear film scan software in Chinese subjects. They found the NI-TBUT values measured with the software to be well correlating with the F-TBUT values. However, their study did not consider clinical dry eye grading and included moderate to severe dry eye subjects. They found a cut-off point of 2.65 s for the NI-TBUT to have the greatest sensitivity (84.1 %) and specificity (75.6 %).
Mengher et al. [6] proposed that NI-TBUT may be longer than F-TBUT as fluorescein instillation may reduce the tear film stability [7]. Kojima et al. used change in corneal power of more than 0.5 diopter to determine areas of tear film instability using the TSAS software for the TMS-2 N [23].
Notably, our study found that the NI-TBUT measured by this newly developed technique showed good correlation with the F-TBUT. Cho P et al. did not find good agreement between F-TBUT and NI-TBUT [32, 33]. Our study had the advantage that it also considered clinical dry eye grading as compared to previous studies. Moreover, this study recruited patients from the entire spectrum of dry eye disease, from mild to severe dry eye. The study shows significant correlation between the clinically obtained subjective OSDI questionnaire score and objective testing by NI-TBUT in cases of dry eye.
The originally used Tearscope for NI-TBUT measurement uses a cold cathode light source which is designed to be as far away from the eye as possible, combined with a heat sink which draws the heat away from the light via the handle. This design reduces any heat related drying effect. The Tearscope can be used with or without a slit lamp; slit-lamp observation allows higher magnification and a more sensitive assessment of the tear film [13]. The placido-based topographers describe the anterior surface fluid shape which is used to predict the actual underlying corneal shape. The live video assessment of the placido reflection defines when tear instability is present, but it does not measure or quantify the degree of tear film instability. Numerous topographer manufacturers have therefore begun to implement algorithms to gauge tear film quality [34]. The automated break-up time measurements with the keratograph (Oculus, Wezlar, Germany) have been shown to be significantly shorter than those measured subjectively with the Keeler Tearscope [35]. Weideman D et al. [36] assessed non-invasive tear film assessment techniques results using a corneal topographer (OCULUS Keratograph) and its newly developed measuring software (TF-Scan) and found that it supplies good classification results. Sofie MJ et al. [37] evaluated NI-TBUT in normal children and demonstrated that NI-TBUT is greater in children in comparison to adults. In their study, NI-TBUT and lipid layer interferometry were performed using a Keeler Tearscope mounted on a slit lamp. Amaechi et al. [38] studied the NI-TBUT using Bausch and Lomb Keratometer with CAT. N0.71-21-35 and serial No.10115YY manufactured in USA in Nigerian adults and found that F-TBUT values were comparable to NI-TBUT values. They concluded that as such either of the two techniques can assuredly be used to assess the tear film stability. The status of the tear stability would help in selecting suitable candidates for contact lens wear.
The Optikon Keratron Scout topographer used in our study is a portable corneal topographer. Besides its wide applications in assessing the corneal topography, it can be used to assess the NI-TBUT by the method mentioned in our study.
We found that due to good correlation of the NI-TBUT values obtained in our study with the clinical OSDI scores, the NI-TBUT values can be used to objectively grade the severity of dry eye disease in addition to objectively identify potential dry eye population from the routine subjects. The NI-TBUT values obtained by this method in addition to judging the severity of dry eye disease can help in the appropriate management of such patients. We found a cut-off value of 6.2 s to give a sensitivity of 86.1 % with a specificity of 81.1 %.
We investigated the performance of a non-invasive technique for measuring tear film stability to aid in the diagnosis of dry eye disease in the Indian population. Thus, NI-TBUT can be a valuable tool in diagnosis of dry eye and its severity, as a quick, non-invasive, reliable and patient-friendly test. It is a useful non-invasive objective method for the detection of dry eye and may be useful in monitoring the efficacy of therapies for dry eye. More studies are required to validate our findings.
References
Lemp MA (2007) The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul Surf 5:75–135
Serin D, Karsloglu S, Kyan A, Alagöz G (2007) A simple approach to the repeatability of the Schirmer test without anesthesia: eyes open or closed. Cornea 26:903–906
Clinch TE, Benedetto DA, Felberg NT et al (1983) Schirmer’s test. A closer look. Arch Ophthalmol 101:1383–1386
Lemp MA, Hamill JR Jr (1973) Factors affecting tear film breakup in normal eyes. Arch Ophthalmol 89:103–105
Lee JH, Kee CW (1988) The significance of tear film break-up time in the diagnosis of dry eye syndrome. Korean J Ophthalmol 2:69–71
Mengher LS, Bron AJ, Tonge SR, Gilbert DJ (1985) Effect of fluorescein instillation on the pre-corneal tear film stability. Curr Eye Res 4:9–12
Cho P, Brown B, Lau C (1996) Effect of fluorescein on the tear stability of Hong Kong-Chinese. Optom Vis Sci 73:1–7
Mengher LS, Bron AJ, Tonge SR, Gilbert DJ (1985) A non-invasive instrument for clinical assessment of the pre-corneal tear film stability. Curr Eye Res 4:1–7
Mengher LS, Pandher KS, Bron AJ (1986) Non-invasive tear film break-up time: sensitivity and specificity. Acta Ophthalmol (Copenh) 64:441–444
Hirji N, Patel S, Callander M (1989) Human tear film pre rupture phase time (TP RPT) a non invasive technique for evaluating the pre corneal tear film using a novel keratometer mire. Ophthal Physiol Opt 9:139–142
Cho P, Ho KY, Huang YC, Chui HY, Kwan MC (2004) Comparison of noninvasive tear break-up time measurements from black and white background instruments. Optom Vis Sci 81:436–441
Yokoi N, Komuro A (2004) Non-invasive methods of assessing the tear film. Exp Eye Res 78:399–407
Guillon JP (1998) Non-invasive tearscope plus routine for contact lens fitting. Cont Lens Ant Eye 21:S31–S40
Nichols JJ, Nichols KK, Puent B et al (2002) Evaluation of tear film interference patterns and measures of tear break-up time. Optom Vis Sci 79:363–369
Wang J, Fonn D, Simpson TL, Jones L (2003) Precorneal and pre-and post lens tear film thickness measured indirectly with optical coherence tomography. Invest Ophthalmol Vis Sci 44(6):2524–2528
Goto E, Tseng SC (2003) Kinetic analysis of tear interference images in aqueous tear deficiency dry eye before and after punctal occlusion. Invest Ophthalmol Vis Sci 44:1897–1905
Goto E, Tseng SC (2003) Differentiation of lipid tear deficiency dry eye by kinetic analysis of tear interference images. Arch Ophthalmol 121:173–180
Paiva CS, Lindsey J, Pflugfelder SC (2003) Assessing the severity of keratitis sicca with videokeratoscopic indices. Ophthalmology 110:1102–1109
Liu Z, Pflugfelder SC (1999) Corneal surface regularity and the effect of artificial tears in aqueous tear deficiency. Ophthalmology 106:939–943
Wilson SE, Klyce SD (1991) Advances in the analysis of corneal topography. Surv Ophthalmol 35:269–277
Goto T, Zheng X, Klyce SD et al (2003) A new method for tear film stability analysis using videokeratography. Am J Ophthalmol 135:607–612
Goto T, Zheng Z, Okamoto S, Ohashi Y (2004) Tear film stability analysis system: introducing a new application for videokeratography. Cornea 23:65–70
Kojima T, Ishida R, Dogru M et al (2004) A new noninvasive tear stability analysis system for the assessment of dry eyes. Invest Ophthalmol Vis Sci 45:1369–1374
Gumus K, Crockett CH, Rao K, Yeu E, Weikert MP, Shirayama M, Pflugfelder S (2011) Noninvasive assessment of tear stability with the tear stability analysis system in tear dysfunction patients. Invest Ophthal V Sci 52(1):456–461
Hong J, Sun X, Wei A, Cui X, Li Y, Qian T (2013) Assessment of tear film stability in dry eye with a newly developed keratograph. Cornea 32(5):716–721
Schiffman RM, Dale Christianson M, Jacobse G et al (2000) Reliability and validity of the ocular surface disease index. Arch Ophthalmol 118:615–621
Nichols KK, Nichols JJ, Mitchell GL (2004) The lack of association between signs and symptoms in patients with dry eye disease. Cornea 23:762–770
Nichols KK, Mitchell GL, Zadnik K (2004) The repeatability of clinical measurements of dry eye. Cornea 23:272–285
Sweeney DF, Millar TJ, Raju SR (2013) Tear film stability: a review. Exp Eye Res 117:28–38
Goto E, Ishida R, Kaido M et al (2006) Optical aberrations and visual disturbances associated with dry eye. Ocul Surf 4:207–213
Lin YY, Carrel H, Wang IJ et al (2005) Effect of tear film break-up on higher order aberrations of the anterior cornea in normal, dry, and post-LASIK eyes. J Refract Surg 21:S525–S529
Cho P, Douthwaite W (1995) The relation between invasive and noninvasive tear break-up time. Optom Vis Sci 72:17–22
Cho, P (1993) Reliability of a portable noninvasive tear break-up time test on Hong Kong-Chinese. Optom Vis Sci 70(12):1049–1054
Szczesna-Iskander DH, Iskander DR (2012) Future directions in non-invasive measurements of tear film surface kinetics. Optom Vis Sci 89(5):749–759
Best N, Drury L, Wolffsohn JS (2012) Clinical evaluation of the Oculus Keratograph. Cont Lens Anter Eye 35:171–174
Wiedemann D Development and realization of a new non-invasive method for tear film assessment using a corneal topographer. Available at: http://www.oculus.de/en/downloads/dyn/sonstige/sonstige/oculus_keratograph_ sonderdruck_kontaktlinse_en.pdf. Accessed November 17, 2011
Jones SM, Nischal KK (2013) The non-invasive tear film break-up time in normal children. Br J Ophthalmol bjophthalmol
Amaechi OU, Osunwoke CM (2004) The relation between invasive and non-invasive tear break-up time in young adults. J Nigerian Optom Assoc 11(1)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhandari, V., Reddy, J.K., Relekar, K. et al. Non-invasive assessment of tear film stability with a novel corneal topographer in Indian subjects. Int Ophthalmol 36, 781–790 (2016). https://doi.org/10.1007/s10792-016-0186-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0186-7