Abstract
The purpose of this study was to investigate the effects of pupil dilation on the parameters of the AL-Scan (Nidek Co., Ltd, Gamagori, Japan). We compared the measurements of axial length (AL), anterior chamber depth (ACD), central corneal keratometry reading, pupil diameter, and intraocular lens (IOL) power of 72 eyes of 72 healthy volunteers and patients scheduled for cataract surgery before and 45 min after instillation of cyclopentolate hydrochloride 1 % using the AL-Scan. Intraobserver repeatability was assessed by taking three consecutive recordings of ACD and AL. Only ACD readings were significantly different between predilation and postdilation (P < 0.001). The difference of the other measurements between two sessions was not statistically significant (P > 0.001). Only two cases in the study demonstrated changes in IOL power higher than 0.5 D. The intraobserver repeatability of both devices was good (CV values for ACD and AL were 0.16 and 0.20 %, respectively). Dilated pupil size did not affect the measurement of IOL power using the A-Scan optical biometer, but increase in ACD after dilation should be taken into account when performing refractive surgeries in which ACD is very important such as phakic anterior chamber IOL implantation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate biometry is of great importance for the calculation of the precise refractive power of the intraocular lens (IOL) power calculation in cataract surgery. IOL Master (Carl Zeiss Meditec AG, Jena, Germany) was the first optical biometry introduced in 1999 using partial coherence interferometry (PCI) [1]. Then, the Lenstar LS 900 biometer (Haag-Streit AG, Koeniz, Switzerland) using optical low-coherence reflectometry (OLCR) was introduced in 2008. Reliable intraobserver and interobserver measurements for both instruments have been reported by several studies [2–4]. Recently, a new biometry device, AL-Scan (Nidek Co., Ltd, Gamagori, Japan), was released in the market. This device uses an 830 nm infrared laser diode for AL measurement with PCI. It also measures keratometry readings (K), anterior chamber depth (ACD), central corneal thickness (CCT), white-to-white distance (WTW), and pupil size (PD).
Some certain types of cataracts may have a potential to create difficulties when performing optical biometry [3, 5]. Dilating the pupil can serve to aid in obtaining biometrical parameters when the surgeon face such a problem. Does dilating the pupil may affect the parameters? This particular question is unique as little is known about this situation. ACD, PD, and CCT are also very important factors for refractive surgeries in which no cataract is seen such as phakic anterior chamber IOL implantation and excimer laser ablation.
In this study, we aimed to investigate the effect of pupil dilation on the biometric parameters of the AL-Scan.
Methods
This prospective cross-sectional study enrolled 72 eyes of 72 healthy volunteers and patients scheduled for cataract surgery. Cases with unhealthy corneas, previous ocular surgery, or chronic eye disease were excluded. The study was approved by the Ethics Committee of Ondokuz Mayıs University, Samsun, Turkey, and written informed consent was obtained from each participant after they were told the purpose of this study. The study followed the tenets of the Declaration of Helsinki.
Measurements of AL, ACD, CCT, K readings, pupil diameters, and IOL power were performed before and 45 min after instillation of two drops of cyclopentolate hydrochloride 1 % using the AL-Scan. SRK/T formula was used to calculate IOL power in all eyes. Drop administration and biometry measurements were performed by the same ophthalmologist. Three consecutive measurements of each undilated eyes were taken by the same operator to determine the intraobserver repeatability.
Statistical analysis was performed with SPSS (SPSS for Windows, version 15.0, SPSS, Chicago). All data were reported as averages ± standard deviations (SD). To compare variables between the pre- and postcycloplegia measurements, paired t test was used. A value of P < 0.05 was considered statistically significant. Bland–Altman method was used to evaluate agreement. The 95 % limits of agreements (LoA) were defined as the mean ± 2 SD of the differences between the two measurements. Repeatability analysis of the study measurements was evaluated with coefficient of variation (CV).
Results
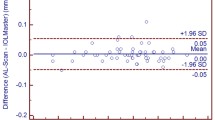
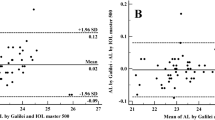
The mean ages of the cases (54.5 % men and 45.5 % women) were 33.12 years ± 9.2 (range 22–50 years). Figure 1 represents PD changes before and after cycloplegia. Table 1 shows the mean AL-Scan readings before and after cycloplegia. Only ACD readings were significantly different between predilation and postdilation (P < 0.001). The median Ksteep measurements of predilated and postdilated pupils were 43.9 D (40.96–46.62) and 43.96 D (41.01–46.62), respectively. The mean ACD values of predilated and postdilated pupils were 3.36 mm (2.66–5.74) and 3.45 mm (2.72–5.70), respectively. The mean CCT measurements of predilated and postdilated corneas were 561.45 mm (494–628) and 559.74 (502–623) mm, respectively. Bland–Altman plots of IOL power and AL measurements showed that the difference between IOL powers and AL measurements was not statistically significant in predilation and postdilation measurements. Only two cases in the study demonstrated changes in IOL power higher than 0.5 D. The intraobserver repeatability of both devices was good which yielded CV values of ACD and AL as 0.16 and 0.20 %, respectively Figs. 2 and 3.
Discussion
It has been reported that when performing biometry with both the IOL Master and the Lenstar, the measurement of AL can be challenging in patients with posterior subcapsular and dense nuclear cataracts [6]. Although dilating the pupil is a choice to control this problem, we cannot state with certainty that dilated pupil has an effect on biometric parameters. Besides AL, anterior segment parameters, particularly ACD and CCT are the important factors for other refractive surgeries. Dilated pupil would have significant effect on anterior segment parameters when these surgeries are considered. In a study performed with applanation biometer, dilating the pupil did not affect the AL measurements [7]. In another study evaluating the effect of pupil dilation on the biometric parameters of the Lenstar LS 900 (Haag-Streit AG, Koeniz, Switzerland), it has been shown that dilated and undilated PD did not affect the measurement of IOL [8]. So, we decided to investigate the effect of dilating the pupil on biometric and anterior segment parameters performed with the LTCI.
AL-Scan, a LTCI optical biometer, is a new generation optical biometer based on LTCI. Using auto-alignment function, the instrument can measure 6 values (AL, K readings, ACD, CCT, WTW distance and PS) within 10 s. Keeping the patient fixated to a red led (700 nm) beam, the eyes become in focus when the patient’s head is approximately 4.5 cm away from the instrument. AL is measured with LTCI using the 830 nm superluminescent diode. CCT and ACD of the patient’s eye are measured with the scheimpflug principle. Keratometry readings are measured using 6 spots of light projected onto the cornea at the central 2.5 mm zone.
Studies have shown that forward movement and thickening of the lens in accommodation and the thinning and backwards movement in relaxation cause several changes in the dimensions of ACD [9, 10]. Application of cyclopentolate causes the lens thickness to be decreased and the lens moves backwards, resulting in an increase in ACD.
Our results are consistent with those of Bakbak et al., Palamar et al., and Arriola-Villalobos et al. who reported a statistically significant change in ACD values but no significant change in AL or IOL power between undilated and dilated pupil biometry readings [8, 11, 12]. In their study, Palamar et al. investigated the effects of cyclopentolate on the main numerical parameters of anterior segment with Pentacam rotating scheimpflug camera in children and found that ACD was significantly different before and after instillation of cyclopentolate. Arriola-Villalobos investigated the influence of pupil dilation on IOL power predictions with OLCR optical biometer and found that only ACD varied significantly according to pupil dilation. An error of 0.1 mm in ACD may result in a 0.1 D error in post-operative refraction [13, 14]. Measuring of the ACD is important for exact biometry. Biometric formulas such as Haigis, Holladay 2, and Olsen use preoperatively measured ACD to predict effective lens position. According to our study, measuring the ACD after instillation of cyclopentolate may result with an error of approximately 0.09 D and this error is not clinically significant.
Our results of CCT measurements are not consistent with those of Palamar et al. [11]. They found a significant change in measurements of CCT and assumed that topical cyclopentolate, which is an atropine-like muscarinic receptor antagonist, probably decreases the tear film thickness and causes decreased CCT measurements as systemic atropine does [11, 15]. However, further investigations are needed to demonstrate the effect of cyclopentolate hydrochloride on CCT.
It might seem a limitation that our study includes both healthy and cataractous eyes rather than cataractous eyes only. Considering the fact that precise measurement of anterior segment parameters of the eye (particularly ACD, PD, and CCT) is a very important factor for refractive surgeries in which no cataract is seen such as phakic anterior chamber IOL implantation and excimer laser ablation, we thought that evaluating the effect of pupil dilation in healthy eyes would be a beneficial step. Even so, further studies with the eyes having different types of cataract are needed to evaluate the effect of pupil dilation and measurement capability of the AL-Scan optical biometer for cataract surgeries.
In conclusion, cyclopentolate instillation causes statistically significant increase in ACD compared with precycloplegia measurements. Although this increase did not affect the measurement of IOL power or excimer laser procedures, it should be taken into account when performing refractive surgeries in which ACD is very important such as phakic anterior chamber IOL implantation.
References
Haigis W, Lege B, Miller N, Schneider B (2000) Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 238:765–773
Gallinaro C, Toulemont PJ, Cochener B (1996) Excimer laser photorefractive keratectomy to correct astigmatism. J Cataract Refract Surg 22:557–563
Buckhurst PJ, Wolffsohn JS, Shah S (2009) A new optical low coherence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol 93:949–953
Holzer MP, Mamusa M, Auffarth GU (2009) Accuracy of a new partial coherence interferometry analyser for biometric measurements. Br J Ophthalmol 93:807–810
Tehrani M, Krummenauer F, Blom E (2003) Evaluation of the practicality of optical biometry and applanation ultrasound in 253 eyes. J Cataract Refract Surg 29:741–746
Drexler W, Findl O, Menapace R (1998) Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol 126:524–534
Sadiq SA, McElvanney AM (1996) Pupillary dilation and axial length measurement for preoperative assessment of intraocular lens power. Eur J Ophthalmol 6:147–149
Bakbak B, Koktekir BE, Gedik S (2013) The effect of pupil dilation on biometric parameters of the Lenstar 900. Cornea 32(4):e21–e24
Wendt M, Croft MA, McDonald J (2008) Lens diameter and thickness as a function of age and pharmacologically stimulated accommodation in rhesus monkeys. Exp Eye Res 86:746–752
Ostrin LA, Glasser A (2010) Autonomic drugs and the accommodative system in rhesus monkeys. Exp Eye Res 90:104–112
Palamar M, Egrilmez S, Uretmen O (2011) Influences of cyclopentolate hydrochloride on anterior segment parameters with Pentacam in children. Acta Ophthalmol 89:e461–e465
Arriola-Villalobos P, Diaz-Valle D (2014) Effect of pharmacologic pupil dilation on OLCR optical biometry measurements for IOL predictions. Eur J Ophthalmol 24:53–57
Holladay JT (1997) Standardizing constants for ultrasonic biometry, keratometry, and intraocular lens power calculations. J Cataract Refract Surg 23:1356–1370
Olsen T, Corydon L, Gimbel H (1995) Intraocular lens power calculation with an improved anterior chamber depth prediction algorithm. J Cataract Refract Surg 21:313–319
Norn M (1985) The effects of drugs on tear flow. Trans Ophthalmol Soc UK 104(Pt 4):410–414
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Funding
No financial support was received for this submission.
Rights and permissions
About this article
Cite this article
Can, E., Duran, M., Çetinkaya, T. et al. The effect of pupil dilation on AL-Scan biometric parameters. Int Ophthalmol 36, 179–183 (2016). https://doi.org/10.1007/s10792-015-0097-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-015-0097-z