Abstract
Keratoconus is a bilateral and asymmetric corneal ectasia. Cross-linking uses ultra-violate rays to enhance corneal tissue. The purpose of this study was to use in vivo confocal microscopy to quantitatively analyze microstructural changes over time, after corneal collagen cross-linking (CXL) in keratoconus patients. In this before-and-after study, a total of 45 keratoconic eyes were selected for cross-linking among patients referred to Al-Zahra ophthalmology clinic during 2013–2014. All patients underwent complete ophthalmologic examinations. Keratocytes and the present of activated keratocytes were calculated preoperatively and at 1, 3, 6, and 12 months postoperatively using confocal microscopy. One year after CXL, best corrected and best uncorrected visual acuity was increased significantly (p < 0.001). Spherical equivalent and spherical refractive errors reduced significantly (p < 0.001). The reduction in density of anterior and mid-stromal keratocytes was significant initially (p < 0.001). During follow-up, the density of keratocytes increased significantly in all layers reaching near normal values by 12 months. The percentage of activated keratocytes showed a significant increase 1 month after cross-linking (p < 0.001) albeit this percent reduced as the corneal healing proceeded by month 12. The endothelial cells showed no significant reduction during the follow-up. Collagen cross-linking-induced significant reduction in keratocyte density. The percent of activated keratocytes increased significantly after cross-linking which showed reduction with improvement of corneal healing. After collagen cross-linking, hyper-reflective structures were observed consistent with the stromal collagen structures. Further studies are needed to assess possible changes on corneal biomechanics. The consistency in corneal endothelium numbers proves the safety of this technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keratoconus is a relatively frequent, progressive, noninflammatory, bilateral ectatic corneal disease, in which the cornea assumes a conical shape due to thinning and protrusion [1]. Corneal ectatic disorders may lead to protrusion, astigmatism, loss of visual acuity, and potentially even perforation. In keratoconus, apoptosis of keratocytes or release of degradative enzymes is thought to be the causes of keratocyte loss and consequently loss of corneal stroma and decreased mechanical strength of cornea [2]. A longitudinal 8-year evaluation of keratoconus noted that the mean rate of steepening of the flattest keratometric value was 0.2 ± 0.8 diopters (D) per year [3].
Collagen cross-linking (CXL) with Riboflavin and UVA is a relatively new approach in treating progressive keratoconus directly targeting the stroma. In this technique, riboflavin is used as a photosensitizer in the presence of UVA in an attempt to stiffen the cornea by increasing intra- and inter-fibrillar covalent bands, improve biomechanical strength, induce keratocyte apoptosis, and increase resistance to enzymatic digestion [4–10].
In vivo confocal microscopy (IVCM) is an evolving technique for the in vivo study of the cornea at the cellular level, which provides images comparable to ex vivo histochemical methods, and is especially suitable for cell layer analysis of the cornea [11].
The aim of this study was to evaluate the changes induced in corneal microstructure of keratoconus patients after CXL treatment, and to analyze the quantitative changes over time using IVCM.
Methods
In this prospective study, 45 keratoconic eyes were selected from patients referring to Al-Zahra eye hospital (Zahedan, Iran) for corneal collagen cross-linking. Inclusion criteria included patients older than 14 years of age with confirmed keratoconus defined as KR more than 47.2, a pattern consistent with keratoconus in axial map, more than 100 µm differences between the thinnest point and 7-mm zone, clear cornea with no scarring and other pathologies. Exclusion criteria included KR > 60D, corneal thickness less than 400 µm previous history of refractive surgery, chemical or penetrating trauma, ocular disease (other than keratoconus), pregnancy, breast feeding, and use of contact lenses during the last month.
All patients underwent complete ophthalmologic and optometric examinations including slit lamp biomicroscopy, dilated fundus examination, and IVCM. Best corrected and uncorrected visual acuity were evaluated using the E chart and refraction determined (using autorefraction followed by subjective refraction) then converted to LogMAR using conversion table [12]. Informed consent was obtained from all participants, and the study protocol was approved by the ethics committee of Zahedan university of medical sciences.
Protocol of collagen cross-linking
Under topical anesthesia Tetracaine 0.5 % and under sterile conditions of the operating room, patients were prepped and draped. The central 7–8 mm of the cornea was marked using a trephine. The epithelium was loosened with 20 % alcohol for 20 s, while the well was in place to prevent limbal touch. After thorough irrigation, the epithelium was removed using a blunt spatula taking care not to damage the Bowman’s layer. All corneas were treated with isotonic riboflavin solution 0.1 % (10 mg riboflavin-5-phosphate in 10 ml dextran-T0500 solution) every 5 min for 30 min. Then, the cornea was exposed to UVA 365 nm for 30 min at an irradiance of 3mW/cm2 surface (5.4 J/cm2 surface dose after 30 min) (MLase AG, corneal cross-linking system −365). Riboflavin was instilled every 5 min till the end of procedure. After completion of procedure and irrigation of corneal surface with balanced salt solution, a soft bandage contact lens was placed. Patients were treated postoperatively with chloramphenicol 0.05 % and fluorometholone 0.1 % eye drops 4 times daily for 1 week. Bandage contact lens was removed after complete epithelial healing usually between 48 and 72 h postoperatively.
In vivo confocal microscopy
In vivo confocal microscopy (IVCM) using confoscan 3 (Nidek Technologies, Gamagori, Japan) was conducted for all patients before cross-linking and one, three, six, and 12 months after treatment. After the procedure was fully explained and informed consent obtained, each patient was prepared. The cornea was anesthetized using tetracaine 0.5 %; the lens was disinfected, and Viscotears (Carbomer 940, 2 mg/g; CIBA Vision, Castle Hill, NSW, Australia) was placed on the lens objective as the coupling agent. The patient was instructed to fix at a distant target. The device was guided so that the objective lens made contact with the corneal apex perpendicularly. Standard Zeiss 40 × lens with 2-mm working distance coupled with Viscotears was used with a final resolution of 768 × 576 pixel and magnification 500×. The full thickness cornea was scanned with manual mode and passes were made until 350 sequential digital images were obtained. The procedure was completed for each eye in about 5–10 min depending on patient compliance. No corneal complications were encountered as the consequence of examination.
Image analysis
At the end of each examination, 2 of the clearest images of endothelium, posterior, middle, and anterior stroma were chosen using the z-scan diagram. The anterior stroma was defined as the first 10 % of stroma after basal epithelial layer. The middle stromal layer was defined as the middle 33–67 % of stromal depth using the Z-scan diagram. The posterior stroma was defined as the posterior 10 % of stroma anterior to the endothelium. Quantitative analysis was subsequently performed by a single examiner. Endothelium was evaluated using the manual endothelial analysis tool on the NAVIS application on the confoscan 3 (Nidek Technologies, Gamagori, Japan). At least 45 endothelial cells and their surrounding circumference were marked for each count. The stromal keratocytes and activated keratocytes were quantitated by the NAVIS application by choosing a region of interest (ROI) of 500 µm2.
SPSS software (version 20) was used for statistical analysis. All collected data were analyzed using ANOVA statistical test and Bonferroni correction. A 5 % significance level was maintained for all analyzed data.
Results
In this research, 21 right and 24 left eyes from 31 patients (21 males and 10 females) were treated. The mean age of these cases was 22.4 ± 4.9 years.
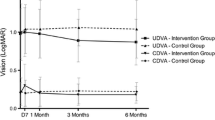
Best corrected (BCVA) and uncorrected visual acuity (BUCVA) is shown in Table 1. Change of BUCVA was not significant at the first 3 months compared to the baseline. But, the mean BUCVA increased significantly at months 6 (0.66 ± 0.34 LogMAR) and 12 (0.59 ± 0.31 LogMAR).
There was a statistically significant change at the first month in BCVA (0.20 ± 0.13) which remained significant until the end of follow-up period. (P = 0.001).
Confocal findings
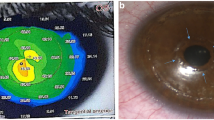
At anterior stromal layer, total absence of keratocytes was seen in 46 % of cases 1 month after operation. Honeycomb hyper-reflective structures and anterior stromal edema were observed during the first 3 months postoperatively (Fig. 1). These changes diminished gradually and keratocytes were apparent at 6 and 12 months. In 54 % of cases, scarcely scattered keratocytes were detected at the first month which increased during 3, 6, and 12 months after cross-linking, (Fig. 2; Table 2). Gradual increase of middle and posterior stromal keratocytes was detected, respectively. The repopulated keratocytes were thought to form new, well-structured collagen, and more compact lamellar interconnections, resulting in improved structural integrity.
Statistical analyzes confirmed that anterior and mid-stromal keratocytes were significantly decreased at 1, 3, 6, and 12 months. Posterior keratocytes decreased significantly during the first 3 months, but the density was not significantly decreased 6 and 12 months postoperatively (Table 2). Hyper-reflective and needle-like structures were observed at mid-stromal layer 1 month after cross-linking which was replaced by keratocytes 6 and 12 months postoperatively (Fig. 3). No decline in endothelial cells was detected during follow-up period.
In addition, we calculated the ratio of active keratocyte to total keratocyte density in anterior and mid-stromal layers (Fig. 4). This ratio was 0.95 ± 1.28 percent preoperatively. In the mid- and anterior stroma, there was increased density of active keratocyte nuclei percentage at the first month which was gradually decreased at 3, 6, and 12 months after surgery. In all follow-up steps, active keratocyte density was significantly different to the preoperative reference values (Table 3).
Discussion
Use of riboflavin and UVA irradiation to achieve CXL of corneal collagen was first described by Sporel and associates (1998) who showed that corneal CXL increased the rigidity of human corneal tissue [13]. CXL is known as the only “pathogenetic approach” to progressive keratoconus that can delay or block its progression, reducing demand for donor keratoplasty [14].
In this study, we focused on quantifying the microstructural changes occurring in the cornea over time after collagen cross-linking.
In theory, insufficient ultraviolet energy and oxygen radicals present at the depth beyond 300 µm in CXL insures minimal toxic effects on the corneal endothelium [15]. This hypothesis was consistent with our results, as no significant decline in endothelial cell counts was encountered in our patients from the first till the 12th month of follow-up (Table 2). Ramirez et al. [16] and Jordan et al. [5] also reported similar results.
As mentioned before one month after CXL, 46 % of corneas were devoid of keratocytes in the anterior lamella. Instead, areas of hyper-reflective honeycomb bands were observed with interweaving hypo-reflective stoma. These bands were present in mid-stromal cornea with a broad, long, and straight configuration, but less density. Previous in vivo and ex vivo IVCM studies have also reported keratocyte apoptosis along with honeycomb-like structures mostly in anterior stroma (270-350 µm) which is consistent with our results [15, 17, 18]. These structures are believed to be stromal edema. Other surgical insults such as PRK or epithelial debridement can also lead to keratocyte apoptosis but this is usually confined to the more superficial layers (50–75 µm) [19]. Therefore, although some of these changes could be attributed to the epithelial injury but recent ex vivo studies have demonstrated higher rates of keratocyte apoptosis in standard CXL (with epithelial removal) than corneal epithelial removal with either UVA or riboflavin alone [20]. These reports are consistent with our results indicating that CXL has indeed significant impact on corneal stroma and keratocyte apoptosis helping to remodel a firmer microstructure. Other studies on the other hand question this effect. Mastropasqua and colleagues compared changes in corneal microstructure in patients with trans epithelial and standard CXL using ICVM. They concluded that microstructural changes visible after CXL are more likely consequence of an inflammatory reaction induced by epithelial injury and the low resolution of in vivo imaging techniques limit the detection of collagen modification induced by CXL treatments [21].
In the remaining 54 % of corneas, keratocyte nuclei were observed sparsely (only 3 % of the keratocyte density measured preoperatively) between the hyper-reflective structures. These keratocyte nuclei showed increased hyper-reflectivity in comparison with preoperative nuclei indicating activated function. Activated keratocyte nuclei constituted 97.92 ± 8.25 % of total nuclei present in the anterior stroma in the first month postoperatively. During 3, 6, and 12 months follow-up after cross-linking, the number of keratocytes increased and the posterior corneal keratocytes reached their preoperative levels by month 6. In the anterior and mid-stroma, this increase was continued until the end of follow-up in month 12 but preoperative levels were not reached. The hyper-reflective bands and networks also started to disappear as part of corneal remodeling post-healing by the end of the 6th month post-CXL. Previous studies have demonstrated the healing of corneal keratocytes starting from the 2nd to 3rd months after cross-linking and reaching preoperative levels by month 6 [14, 17, 22, 23]. Similar to our findings, Knappe and colleagues also reported significant hypocellularity in corneal anterior stroma 12 months after CXL [22]. The delay in our cases could be due to different racial and environmental factors contributing to this healing phenomenon, especially the hot and dry climate which in turn increases the prevalence of ocular surface disease in this state.
Other studies have also reported elongated needle-like structures and hyper-reflective bands in the transitional zone, as mentioned earlier in our results. It has been postulated that these structures represent new synthesized collagens possibly the product of activated keratocytes [17, 22, 24, 25]. Gradual posterior to anterior relocation of these structures has been reported by Kymionis et al. during sequential examinations [26]. Recent pathological studies suggested these particles related to transient fibroblast generation as opposed to myofibroblasts [5]. As the numbers of keratocytes increased during the follow-ups, the percentage of activated keratocytes decreased, tailoring with the healing of the cornea (Table 3). These changes could indicate the role of activated keratocytes in rearrangement of corneal microstructure. More histopathologic or even histochemical studies are needed to point the difference in these activated keratocytes in the molecular level possibly introducing them as the new targets of treatment in keratoconus patients.
In conclusion, in this study, we observed complete keratocyte apoptosis and edema in anterior stroma early post-CXL. Mid-stroma also showed keratocyte apoptosis but to a lower degree compared to anterior stroma. Repeated examination showed increase in cell regeneration from 3rd month post-CXL reaching near normal levels after 12 months. Hyper-reflective bands and elongated needle-like structures were also visible at the boarder of treated and untreated cornea. Corneal endothelium remained unchanged throughout the study.
References
Rabinowitz YS (1998) Keratoconus. Surv Ophthalmol 42:297–319
Dhaliwal JS, Kaufman SC (2009) Corneal collagen cross-linking: a confocal, electron, and light microscopy study of eye bank corneas. Cornea 28:62–67
Wagner H, Barr JT, Zadnik K (2007) Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Contact Lens Anterior Eye 30:223–232
Jankov MR II, Jovanovic V, Nikolic L, Lake JC, Kymionis G, Koskunseven E (2010) Corneal collagen cross-linking. Mid East Afr J Ophthalmol 17(1):21–27
Jordan C, Patel DV, Abeysekera N, McGhee CN (2014) In vivo confocal microscopy analyses of corneal microstructural changes in a prospective study of collagen cross-linking in keratoconus. Ophthalmology 121(2):469–474
Wollensak G, Spoerl E, Seiler T (2003) Riboflavin/ultraviolet A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 135:620–627
Henriquez MA, Izquierdo L Jr, Bernilla C, Zakrzewski PA, Mannis M (2011) Riboflavin/ultraviolet a corneal collagen cross-linking for the treatment of keratoconus: visual outcomes and Scheimpflug analysis. Cornea 30:281–286
Kohlhaas M, Spoerl E, Schilde T, Unger G, Wittig C, Pillunat LE (2006) Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin and ultraviolet A light. J Cataract Refract Surg 32:279–283
Abdelghaffar W, Hantera M, Elsabagh H (2010) Corneal collagen cross-linking: promises and problems. Br J Ophthalmol 94:1559–1560
Koller T, Iseli HP, Hafezi F, Vinciguerra P, Seiler T (2009) Scheimpflug imaging of corneas after collagen cross-linking. Cornea 28:510–515
Chaidaroon W (2007) Confocal microscopy of the human cornea. Chiang Mai Med J 46(2):83–91
Holladay JT (2004) Visual acuity measurements. J Cataract Refract Surg 30:287–290
Spoerl E, Huhle M, Seiler T (1998) Induction of cross-links in corneal tissue. Exp Eye Res 66(1):97–103
Mazzotta C, Traversi C, Baiocchi S, Caporossi O, Bovone C, Sparano MC et al (2008) Corneal healing after riboflavin ultraviolet-A collagen cross-linking determined by confocal laser scanning microscopy in vivo: early and late modifications. Am J Opthalmol 146:527–533
Wollensak G, Spoerl E, Wilsch M, Seiler T (2004) Keratocyte apoptosis after corneal collagen cross-linking using riboflavin/UVA treatment. Cornea 23(1):43–49
Ramírez M, Hernández-Quintela E, Naranjo-Tackman R (2013) Early confocal microscopy findings after cross-linking treatment. Arch Soc Esp Oftalmol 88(5):179–183
Mazzotta C, Balestrazzi A, Traversi C, Baiocchi S, Caporossi T, Tommasi C et al (2007) Treatment of progressive keratoconus by riboflavin-UVA-induced crosslinking of corneal collagen: ultrastructural analysis by Heidelberg Retinal Tomograph II in vivo confocal microscopy in humans. Cornea 26:390–397
Kaya V, Utine CA, Yilmaz OF (2011) Efficacy of corneal collagen cross-linking using a custom epithelial debridement technique in thin corneas: a confocal microscopy study. J Refract Surg 27:444–450
Helena MC, Baerveldt F, Kim WJ, Wilson SE (1998) Keratocyte apoptosis after corneal surgery. Investig Ophthalmol Vis Sci 39:276–283
Salomão MQ, Chaurasia SS, Sinha-Roy A, Ambrósio R Jr, Esposito A, Sepulveda R et al (2011) Corneal wound healing after ultraviolet-A/riboflavin collagen crosslinking: a rabbit study. J Refract Surg 27:401–407
Mastropasqua L, Nubile M, Lanzini M, Calienno R, Mastropasqua R, Agnifili L et al (2013) Morphological modification of the cornea after standard and transepithelial corneal cross-linking as imaged by anterior segment optical coherence tomography and laser scanning in vivo confocal microscopy. Cornea 32(6):855–861
Knappe S, Stachs O, Zhivov A, Hovakimyan M, Guthoff R (2011) Results of confocal microscopy examinations after collagen cross-linking with riboflavin and UVA light in patients with progressive keratoconus. Ophthalmologica 225:95–104
Touboul D, Efron N, Smadja D, Praud D, Malet F, Colin J (2012) Corneal confocal microscopy following conventional, transepithelial, and accelerated corneal collagen cross-linking procedures for keratoconus. J Refract Surg 28:769–776
Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR (2008) A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg 24:S720–S725
Croxatto JO, Tytiun AE, Argento CJ (2010) Sequential in vivo confocal microscopy study of corneal wound healing after cross-linking in patients with keratoconus. J Refract Surg 26:638–645
Kymionis GD, Portaliou DM, Diakonis VF, Kontadakis GA, Krasia MS, Papadiamantis AG et al (2010) Posterior linear stromal haze formation after simultaneous photorefractive keratectomy followed by corneal collagen crosslinking. Investig Ophthalmol Vis Sci 51:5030–5033
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aminifard, MN., Khallaghi, H., Mohammadi, M. et al. Comparison of corneal keratocytes before and after corneal collagen cross-linking in keratoconus patients. Int Ophthalmol 35, 785–792 (2015). https://doi.org/10.1007/s10792-015-0041-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-015-0041-2