Abstract
Solanum nigrum L. is a popular traditional medicine for various inflammatory conditions including rheumatism and joint pain. The current study aimed to evaluate the anti-arthritic mechanism of Solanum nigrum L. Four extracts were prepared using n-hexane, methanol, chloroform, and water. The anti-nociceptive and anti-inflammatory activity was carried out with 100, 200, and 300 mg/kg body wt. PO of each extract by the hot plate and carrageenan-induced paw oedema methods, respectively. The anti-arthritic study was performed with chloroform and aqueous extracts (300 mg/kg) in complete Freund’s adjuvant (CFA)-induced arthritis. Paw size (mm), ankle joint diameter (mm), and latency time (sec) were recorded on day 0 and every 4th day till 28 days. The hematological, inflammatory, and oxidative biomarkers were estimated. Results showed that significant analgesia (p < 0.05) and reduction in paw inflammation were achieved with all extracts. The highest percent inhibition in Carrageenan-induced inflammation was achieved with 300 mg/kg of chloroform (72.19%) and aqueous (71.30%) extracts, respectively. In the CFA model, both extracts showed a significant reduction in paw size and ankle joint diameter (p < 0.05). The RT-qPCR analysis revealed the upregulation of interleukin-4 and interleukin-10, and down-expression of interleukin-1β, interleukin-6, tumor necrosis factor-α, cycloxygenase-2, nuclear factor-κB, prostaglandin E synthase 2, and interferon-γ. A significant increase in superoxide dismutase, catalase, and glutathione levels was observed. Hence, it is concluded that Solanum nigrum L. leaf extracts regulate the expression of inflammatory markers and improve oxidative stress resulting in the attenuation of CFA-induced arthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a systemic autoimmune disease of the chronic form. There exists a variation in severity between different patients and genders; however, females are in general more frequently affected as compared to males (Alam et al. 2017). The characteristic inflammatory changes in RA not only affect synovial tissue of joints but also bone and cartilage. Involvement of extra-articular regions is also reported. Clinically, these changes are manifested as redness, arthralgia, swelling, and limited mobility of symmetrical joints. One of the most distinctive features of RA is synovial hyperplasia which leads to the formation of pannus. A complex involvement of adaptive and innate immune responses to evoke inflammatory responses ensued. Formation of autoantibodies like rheumatoid factors (RF), ACPA, and hyperactive macrophage/ monocyte system in the target tissues give rise to a plethora of clinical and histomorphological features of the disease. Arachidonic acid metabolites and inflammatory cytokines have been identified as causing systemic manifestations of RA. The role of pro-inflammatory cytokines has been well established in causing joint damage during RA development (Liu et al. 2019). The destructive process of active RA is dominated by macrophages and fibroblasts (Scherer et al. 2020). The progression and severity of RA follow multiple interlinked mechanisms of inflammation, oxidative stress, and generation of reactive oxygen species (Shahmohamadnejad et al. 2015). Free radicals lead to molecular damage and are believed to trigger transcription of IL-6, TNF-alpha, and IL-1β associated with NF-κB ultimately resulting in marked synovitis and destruction of cartilage (Quiñonez-Flores et al. 2016).
The main goal of available conventional drug therapy (non-steroidal anti-inflammatory drugs, biological therapies, disease-modifying anti-rheumatic drugs, and glucocorticoids) is to mitigate RA symptoms but due to the possible occurrence of deleterious body system side effects, their use is being limited (Smolen and Aletaha 2015). A need to develop novel remedies with better effectiveness and lesser risk of adverse effects has diverted the current trend of therapy toward the use of herbal alternatives. To limit progression and control the severity of RA, natural plants possessing anti-inflammatory potential have been extensively studied (Zhang et al. 2019). Cinnamomum cassia (Lauraceae), Ligusticum chuanxiong (Umbelliferae), Aconitum kusnezoffii (Ranunculaceae), Tripterygium wilfordii (Celastraceae), and Curcumae Longae (Zingiberaceae) are some well-known plants, that significantly regulate immunological activity and inflammatory signaling pathways showing potential therapeutic potential against RA (Zhao et al. 2021).
Solanum nigrum L. or “Black Nightshade/ Makoi” is an annual/perennial member of the Solanaceae family. It generally grows as a dicot weed in damp environments in a variety of soils ranging from dry or stony to shallow and deep. It is indigenous to Eurasia; the tropical and subtropical regions are ideal for its cultivation during April and May. Therapeutically, it has been employed for the management of several ailments, namely toothache, pneumonia, tonsillitis, stomach pain, inflammation, fever, pain, tumors as an antioxidant, anti-inflammatory, diuretic, antipyretic, and hepatoprotective (Kuete 2014). In traditional Indian practice, infusions are used for dysentery, tuberculosis, stomach complaints, and fever. The juice is effective for skin diseases, ulcers, and whooping cough. The fruits are useful for laxative action, asthma and work well as an appetite stimulant. In oriental medicinal practice, its use as an antioxidant, anti-tumorigenic, hepatoprotective, anti-inflammatory, and diuretic is extensively reported (Goel et al. 2022). Several active phytochemicals like phenols, terpenes, flavonoids, sesquiterpenes, carotenoids, and lactones have been linked to the potential antioxidant and anti-inflammatory activities, making them a suitable treatment approach in RA (Singh et al. 2020).
The anti-arthritic potential of the aqueous methanolic extract of Solanum nigrum L. berries against the complete Freund's adjuvant (CFA) arthritis rat model has been explored (Alamgeer et al. 2019). Ethyl alcohol extract from Solanum nigrum L. leaves (100 and 200 mg/kg) significantly decreased pro-inflammatory cytokines (IL-1, IL-2, IL-6, TNF-α, and PGE2) in CFA-induced arthritis (ur Rasheed 2022). The current study evaluated the in vitro anti-arthritic and in vivo analgesic and anti-inflammatory potential of four different extracts of Solanum nigrum L. leaves in an acute study. To further explore the basis of the molecular mechanism of inflammation underlying rheumatoid arthritis and for appraisal of anti-arthritic action along with oxidative stress modulation, the most active extracts (Chloroform and aqueous) were selected for the sub-acute study using complete Freund/s adjuvant-induced arthritis model.
Materials and methods
Preparation of extracts
Solanum nigrum L. leaves were collected from their natural habitat from the area of District Jhang, South Punjab, and identified by the taxonomist from the Department of Botany, Government College University (GCU)—Lahore, Pakistan. The plant was issued authentication voucher numbers GC. Herb. Bot. 33,358 and deposited in the herbarium for future reference. The sample was well-cleaned, shade-dried, and powdered to a fine size. The n-hexane, methanol, chloroform (Sigma Aldrich), and distilled water were used separately to soak the powder in 1:5 w/v for maceration twice. The semisolid mass of all extracts was formed in a rotary evaporator at a temperature of 40 °C under reduced pressure.
Experimental animals
The approval for the experiment was acquired from the Animal Ethical Committee, Punjab University College of Pharmacy, Lahore vide no. D/ 241/ FIMS dated June 1st, 2022. The animal experiments were conducted in accordance with the guidelines of NIH publication #85–23, revised in 1985. Healthy male Wistar rats with an average weight of 180–200 g were housed under appropriate environmental temperature and humidity conditions (28 ± 2 °C and 55 ± 2%, respectively). Proper access to water and food was made possible throughout the study period.
Qualitative and quantitative phytochemical study
Phytochemical analysis of all four extracts was performed to identify primary and secondary metabolites according to previously reported methods (Aduwamai et al. 2018). Crude extracts were subjected to quantitative analysis of total phenol content (TPC) by the following method with slight modifications (Veerapagu et al. 2018).
Total phenol content
The total phenol content of all extracts was found through Folin–Ciocalteu (FC) method in triplicate. 1 ml of each Solanum nigrum L. leaves extract (1 mg/ml) was mixed with 5 ml of dilute FC reagent and 4 ml of 1 M Na2CO3. For half an hour, the mixture was kept until color developed at standard temperature. The absorbance was recorded in a UV–Vis Spectrophotometer at 765 nm. For the preparation of the standard curve; 10, 20, 30, 40, and 50 µg/ml concentrations of Gallic acid were prepared in methanol, and the absorbance was measured by mixing 1 ml of each concentration (1 mg/ml) as described above.
Total flavonoid content
0.5 ml of each extract (1 mg/ml) was mixed with ethanol 1.5 ml, 10% ALCL3 0.1 ml, 1 M potassium acetate 0.1 ml, and distilled water 2.8 ml to make a reaction mixture. This was incubated at room temperature of 37 °C for 30 min. The absorbance was read at 415 nm using a spectrophotometer. To prepare a standard curve, different concs.50, 100, 150, 200, and 250 mcg/ml of Quercetin stock solution in ethanol (1 mg/ml) were prepared and the absorbance was measured by mixing 0.5 ml of each conc (1 mg/ml) as described with extracts (Nancy and Ashlesha 2015).
High-pressure liquid chromatography analysis (HPLC)
Different phenols and flavonoids in all plant extracts were estimated by performing HPLC analysis. 20 µl of the sample was carefully injected into HPLC (Shimadzu, Japan) provided with a UV–visible detector. Phytochemical detection was performed by Gradient HPLC with Shim-Pack CLC-ODS (C18) column. The mobile phases used were (94:6) aqua-acetic acid and acetonitrile. Both the phenols and flavonoids were analyzed by their peaks and retention times. Their quantities were analyzed by comparing them with standard chromatograms (Saleem et al. 2020).
In vitro anti-arthritic activity
Protein denaturation inhibition assay
Test solution (TS) comprised 0.05 ml of 100, 250, and 500 mcg/ml test concentrations of plant extracts and 0.45 ml Bovine Serum Albumin (BSA). The Test Control (TC) contained 0.05 ml of DW in 0.45 ml of BSA (5% w/v). Likewise, the positive control (PC) consisted of 0.45 ml dist. water with 0.05 ml of extract concentrations. BSA (0.45 mL) and different concentrations of diclofenac sodium (0.05 ml) served as a standard solution. Following incubation for 20 min at 37 °C, the test temperature was raised to 57 °C for 180 secs. Afterward, to all solutions, 2.5 ml of 6.3 pH phosphate buffer was added after cooling. The absorbance of all solutions was recorded at 660 nm wavelength. The assay was completed in triplicate to calculate the percentage of protein inhibition (Bashir and Niazi 2020) as follows:
Analgesic activity
The analgesic activity of all extracts was evaluated using the previously described hot plate method by Khodabakhsh et al. 2015. Fifty-six rats were randomly divided into 14 groups (n = 4 each). Group 1 was kept as control and received only dist. water PO; group 2 served as positive control and was administered diclofenac Na 10 mg/kg b.wt. Treatment groups received 100, 200, and 300 mg/kg b.wt PO of different extracts as follows. Treatment groups 3, 4, and 5 received n-hexane extract of Solanum nigrum L. (HESN). Groups 6, 7, and 8 rats were given methanol extract of Solanum nigrum L. (MESN); Groups 9, 10, and 11 received chloroform extract (CESN) and groups 12, 13, and 14 were treated with aqueous extract (AESN). Test animals were exposed to noxious pain stimuli on a hot plate kept at 55 ± 2 °C. Latency time was recorded in seconds at 0, 15, 30, 45, and 60 min following drug administration as rats jumped or started licking of paws following one or both paws. To avoid tissue damage to the paw, 45-s cut-off time was set.
Acute anti-inflammatory activity
Carrageenan-induced rat paw oedema model was employed to evaluate the acute anti-inflammatory potential of Solanum nigrum L. leaves extracts (Ijaz et al. 2021). A total of 84 rats were assigned different treatments (n = 6 rats in each group). A digital vernier caliper was used to measure the paw size of rats in mm. One h before 0.1 ml injection of 1% carrageenan solution (w/v) in the left hind paw, group 1 rats were given distilled water orally; diclofenac Na (10 mg/kg) b.wt. was administered intraperitoneally to group 2 rats; groups 3, 4, and 5 rats received HESN; groups 6, 7, and 8 rats received MESN; groups 9, 10, and 11 were treated with CESN; and groups 12, 13, and 14 received AESN at 100, 200, and 300 mg/kg b. wt., orally, respectively. The rat paw size was measured at intervals of 0, 1, 2, 3, 4, and 5 h after carrageenan injection. The percentage inhibition in paw oedema was measured according to the following formula:
where Eo is the paw size at 0 h (before carrageenan injection), Et shows the paw size at each corresponding hour, and (Et–Eo) represents the paw oedema.
Sub-acute anti-arthritic activity
The sub-acute study was carried out on chloroform and aqueous extracts (300 mg/kg b.wt) of Solanum nigrum L. leaves in complete Freund's adjuvant-induced arthritis model.
Complete Freund’s adjuvant (CFA)-induced arthritis
CFA prompts an immunopathological condition resembling features of rheumatoid arthritis in humans. Edematous joints with infiltrates of neutrophils and lymphocytes in the synovium, followed by bone destruction and loss of cartilage ending up in dysfunctional joints are all similar characteristics in CFA-induced animal models to human RA (Choudhary et al. 2018).
Rats were randomly divided into five groups (n = 5). Arthritis in all experimental rats (except the control group) was induced by inoculation of 0.1 mL of CFA comprising of heat-killed M. tuberculosis (10 mg/mL) into the sub-plantar area of the left hind paw. The administration of standard and extracts started from the 12th day and continued till 28 days. (1) Control group: received distilled water PO along with standard pellet food. (2) Disease control group: arthritis-induced rats. (3) Drug control group: given diclofenac sodium (5 mg/ kg) PO. (4) Chloroform extract of Solanum nigrum L. (CESN)-treated group: 300 mg/ kg of CESN was given PO. (5) Aqueous extract of Solanum nigrum L. (AESN)-treated group: 300 mg/ kg of AESN (PO).
Macroscopic arthritic changes induced by CFA
Paw size and ankle joint diameter (mm) in CFA-induced arthritic rats were determined with the help of a digital vernier caliper on day 0 and then after every 4th day up to the 28th day (Gul et al. 2023).
Assessment of pain response in the CFA model of arthritis
Pain response was assessed in terms of latency time in seconds by the hotplate method. Using a cut-off time of 45 secs, the temperature was kept at 53 ± 2 °C, and the time to withdraw paw or jump was recorded (Mahdi et al. 2018).
Quantitative real-time polymerase chain reaction (qRT-PCR)
Real-time polymerase chain reaction was performed to quantify pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, and IFN-γ), anti-inflammatory cytokines (IL-4 and IL-10), and other important mediators of inflammation (NF-ĸB, COX-2, and PGES-2). On the last day of the experiment, the rat blood samples were collected from anesthetized rats in EDTA tubes. RNA extraction was performed using Pure-Link RNA Mini Kit by Invitrogen (Catalogue No. 12183018A). RNA samples were measured and equalized by Nanodrop Quantification by testing samples in replicas. RNA samples were reverse transcribed into cDNA using RevertAid First-Strand cDNA Synthesis Kit (Catalogue No. K1622) by ThermoFisher Scientific using a minimum input of 10 ng/µL of RNA. The expression of targeted genes was performed using SYBR Select Master Mix (Catalogue No. 4472903) by having cDNA as the template with appropriate primers in duplicates. The relevant CTs of samples were compared with controls and control samples having housekeeping genes (GAPDH). Concisely, a reaction mixture of 0.02 mL composed of master mix (0.01 mL), forward and reverse primers (150–400 nM), complementary DNA template + RNase-free H2O was added to a microplate and placed in qPCR instrument (Thermo Fisher Scientific®, USA). The specifications for the thermal cycler were kept as: 40 circles of 2 min of denaturation at 90 °C, annealing at 60 °C (15 secs), and extension at 72 °C (1 min). Finally, the threshold cycles (CT) and relative quantification (ΔΔCT) were computed (Saleem et al. 2020). The primers used in the study are presented in Table 1
Biochemical and hematological analysis
Using mild ether anesthesia, rat blood was obtained by cardiac puncture and collected in ethylenediaminetetraacetic acid (EDTA) tubes on the 28th day of the study. Serum samples were prepared to analyze antioxidant enzymes superoxide dismutase (SOD), reduced glutathione (GSH), and catalase (CAT) using mouse super oxidase dismutase (SOD), mouse reduced glutathione (GSH), and mouse catalase (CAT) ELISA Kits by following instructions of the manufacturer (Zokeyo, China). An advanced immune analyzer, ichromα reader (KR) was used to determine C-reactive protein (CRP) conc. Hematological parameters were analyzed on a Sysmex XP- 300 Hematology analyzer.
GC–MS analysis
The specifications of GC–MS (Shimadzu®, Japan, model: QP 2010 plus) for the plant extracts analysis were: use of capillary column, DB-5 MS (film thickness of 30 m × 0.25 mm × 0.25 µm) as stationary phase; helium (99.9%) with a flow rate of 1 ml/min as a carrier gas; a split-less injection method and temperature of 80 °C later increased to 220 °C for 5 min. The temperature of MS was kept at 280 °C. The total run time of the sample was 30 min (Uroos et al. 2017).
Radiographical analysis
On the 28th day, radiographs of the hind paws of rats were taken. The X-ray films were obtained and observed for swelling of tissue joints, narrowing among joint spaces, and bony erosions (Ijaz et al. 2021).
Statistics
Results are presented as Mean ± SEM. Unpaired t-test (where relevant) and one-way ANOVA followed by Dunnett's test were used for the assessment of all numerical variables and a p-value < 0.05 was considered statistically significant.
Results
The percentage yield of n-hexane, methanol, chloroform, and aqueous Solanum nigrum L. extracts was found to be 1.74, 12.7, 4.65, and 15%, respectively.
Qualitative phytochemical analysis
The qualitative analysis for the identification of various primary and secondary plant metabolites showed that n-hexane extract contained phenols, flavonoids, protein, and sterols. In methanol, chloroform, and aqueous extracts, the presence of alkaloids, terpenoids, flavonoids, phenols, and proteins was noticed. Results are given in Table 2.
Quantitative phytochemical analysis
Total flavonoid content
The total flavonoid content of all extracts is presented in Table 3. It is expressed as mg quercetin equivalents/g using the calibration curve y = 0.0012x + 0.7994, R2 = 0.9896, where x represents the absorbance and y is the quercetin equivalent. The maximum total flavonoid content was found in CESN (109.6 ± 0.38 mg QE /g) and aqueous (75.81 ± 0.52 mg QE /g) extract.
Total phenolic content
Table 3 represents the total phenolic contents of all extracts. The maximum total phenolics were present in CESN (64.36 ± 0.50 mg GA/g) and AESN (81.29 ± 0.55 mg GA/g). It was calculated using the calibration curve: Y = 0.0009x + 0.052, R2 = 0.9837, where x is the absorbance and y represents the gallic acid equivalent.
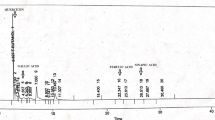
HPLC analysis
The HPLC quantitative estimation of Solanum nigrum L. leaves extracts revealed that in all extracts, quercetin was present. The maximum conc. of quercetin was found in an aqueous extract of Solanum nigrum L. leaves (13.90 mcg/g). Higher amounts of phenolic and flavonoids were present in chloroform and aqueous extracts as compared to methanol and n-hexane extracts. Different quantities of phytochemicals detected in various Solanum nigrum L. extracts are displayed in Table 4, Figs. (1, 2, 3, 4).
Effect of Solanum nigrum L. on protein denaturation inhibition
Chloroform and aqueous extracts of Solanum nigrum L. showed maximum inhibition of protein denaturation (87.93% and 82.44%) followed by n-hexane (80.68%) and methanol extracts (74.44%) as compared to the standard diclofenac sodium (83.97%) as shown in Table 5
Effect of Solanum nigrum L. on pain response in hot plate test
A significant increase in latency time (p < 0.05) was observed with AESN at all dose levels. However, the variable response was observed in HESN, MESN, and CESN 100 mg/kg, 200 mg/kg, and 300 mg/kg treated rats. HESN at 200 mg/kg dose showed a significant increase in LT up to one hour; MESN 200 and 300 mg/kg showed a significant increase after 30 min. CESN 300 mg/kg significantly increased latency time from 30 to 60 min compared to normal control as shown in Table 6.
Effect of Solanum nigrum L. in Carrageenan-induced paw oedema
Significant reduction in rat paw size (p < 0.05) was shown by all the extracts at different dose levels as shown in Table 7. However, maximum percentage inhibition in paw oedema occurred with AESN and CESN as compared to HESN and MESN (Fig. 5).
Effect of n-hexane, methanol, chloroform, and aqueous extracts (100, 200, and 300 mg/kg) of Solanum nigrum L. leaves on % inhibition in paw oedema. HESN: Hexane extract of Solanum nigrum L., MESN Methanol extract of Solanum nigrum L., CESN Chloroform extract of Solanum nigrum L., and AESN Aqueous extract of Solanum nigrum L
Effect of Solanum nigrum L. on paw oedema in CFA-induced arthritic rats
A significant increase (p < 0.0001) in paw size was observed after sub-plantar inoculation of CFA in the disease control group rats with respect to the control group throughout the study duration. Moreover, on the 20th day post initiation of treatment with plant extracts and drug control on day 12, a significant reduction (P < 0.05) in paw size was achieved with AESN at 300 mg/kg dose. Likewise, the subsequent reduction in paw size on day 24 and day 28 was also statistically significant (Fig. 6).
Effect of Solanum nigrum L. on ankle joint diameter in CFA-induced arthritic rats
At day 16, a significant reduction (P < 0.01) in joint diameter was achieved with AESN at 300 mg/kg dose which was retained till the 28th day (5.83 ± 0.16 mm). Similarly, CESN also showed a significant decrease (P < 0.01) in joint diameter (6.73 ± 0.10 mm) as compared to disease control (7.52 ± 0.34 mm) after 1 week post-treatment at day 20 till day 28 (Fig. 7).
Effect of chloroform and aqueous extracts of Solanum nigrum L. leaves on joint diameter (mm). Values are expressed as Mean ± SEM (n = 5). *p < 0.05, **p < 0.01, ***p < 0.001 and ****p < 0.0001 symbolize a significant decrease in the paw size as compared to the disease control after the start of treatment at day 12
Effect of Solanum nigrum L. on pain response in CFA-induced arthritic rats in hot plate test
The latency time to pain response is significantly increased (6.95 ± 0.58 and 6.92 ± 0.42 s) in rats treated with both chloroform and aqueous extracts of Solanum nigrum L. leaves compared to disease control group 2.85 ± 0.36 s (Fig. 8).
Effect of chloroform and aqueous extracts of Solanum nigrum L. leaves on latency time (Secs). Values are expressed as Mean ± SEM (n = 5). *p < 0.05, **p < 0.01, and ***p < 0.001 symbolize a significant decrease in the paw size as compared to the CFA-induced arthritic control after the start of treatment at day 12
Effect of Solanum nigrum L. on mRNA Expression of Inflammatory Cytokines in arthritic rats
Quantitative real-time polymerase chain reaction (qRT- PCR) was used to determine the effect of chloroform and aqueous extracts of Solanum nigrum L. on mRNA expression of various pro-inflammatory and anti-inflammatory biomarkers (Fig. 9). Treatment with both extracts resulted in a significant decrease (P < 0.001) in IL-1β levels 4.61 ± 0.45 and 6.791 ± 0.15 as compared to disease control 12.87 ± 0.96. Following CFA induction, IL-6 levels increased significantly. However, treatment with both extracts resulted in a marked decline (0.34 ± 0.07 and 0.93 ± 0.01) when compared to disease control rats 1.64 ± 0.24. Both TNF-alpha and NF-kB genes were upregulated (1.48 ± 0.01 and 2.29 ± 0.21) as a result of adjuvant induction but post-treatment with 300 mg/kg of CESN and AESN significantly downregulated (P < 0.0001) the levels of these pro-inflammatory biomarkers as shown in Fig. 9.
Effect of chloroform and aqueous extracts of Solanum nigrum L. leaves on mRNA expression of inflammatory cytokines IL-1β: Interleukin-1 beta; IL-6: Interleukin-6; TNF-α: Tumor Necrosis Factor; NF-κB: nuclear-factor-kappa B; COX-2: Cyclo-Oxygenase-2; IFN-γ: Interferon Gamma; PGES-2: Prostaglandin E Synthase 2; IL-4: Interleukin-4 and IL-10: Interleukin-10. Results are presented as Mean ± SEM (n = 5). *p < 0.05, **p < 0.01, ***p < 0.001 and ****p < 0.0001 indicate differences in treatment groups (CESN and AESN vs. disease control)
The mRNA expression of COX-2 was also significantly downregulated (P < 0.001) after treatment with both extracts (0.56 ± 0.09 and 0.64 ± 0.07) in relation to disease control (4.72 ± 0.44). Increased levels of IFN- γ after CFA induction (5.98 ± 0.02) were significantly restored to normal following treatment with both chloroform and aqueous extracts (3.36 ± 0.10 and 3.72 ± 0.32). A similar decrease in PGES-2 expression with both extracts was determined which was significantly lower (P < 0.0001) than the disease control group.
An increase in IL-4 levels post-treatment with both extracts occurred (1.26 ± 0.35 and 1.36 ± 0.20) in comparison to the CFA control (0.05 ± 0.03). Similarly, significant amplification in IL-10 was observed in CESN and AESN treated groups (0.55 ± 0.05 and 0.57 ± 0.12).
Effect of Solanum nigrum L. on hematological parameters in CFA-induced arthritis
Both CESN and AESN treatments resulted in significant improvement in hematological parameters in arthritic rats (Table 8). CRP showed an increase in conc. in the disease control group compared to normal control. However, treatment with both extracts significantly lowered CRP levels (3.28 ± 0.20 and 2.85 ± 0.10) mg/ L when compared with the disease control group as shown in Table 8. Likewise, restoration of ESR to normal values (23.00 ± 1.73 and 28.67 ± 0.88) mm/ 1st h occurred post-treatment with both extracts relative to arthritic rats.
Hemoglobin levels also decreased in the disease control group (9.90 ± 0.15) g/dL and augmented as a result of treatment with both CESN and AESN 300 mg/kg (12.43 ± 0.27 and 12.70 ± 0.05) g/dL as presented in Table 8. Significant alterations in blood cell counts as depicted by decreased RBC count and increased WBCs and platelet count were recorded in arthritic rats. Both the extracts improved RBCs count (5.90 ± 0.11 and 6.20 ± 0.20) 106/µL, reduced the elevated levels of WBCs (6.08 ± 0.06 and 6.63 ± 0.05) 103/µL, and platelets (693.7 ± 1.85 and 740 ± 1.15) 103/µL.
Effect of Solanum nigrum L. on oxidative stress in CFA-induced arthritis
Serum levels of catalase, SOD, and GSH declined significantly (P < 0.0001) as a result of CFA induction (Table 9). However, CESN and AESN treated rats showed a marked reduction in oxidative stress with a significant increase in levels of catalase, SOD, and GSH.
GC–MS analysis
Phytochemicals identified in the Chloroform and aqueous extracts included various esters, alcohols, fatty acids, ketones, and hydrocarbons (Fig. 10 and 11). The maximum conc. (%) in GC–MS spectrum was found to be of docosanoic acid—methyl ester, hexadecanoic acid, tetradecanoic acid, and hexanedioic acid, bis (2-ethylhexyl) ester. The phytochemicals detected by the GC–MS spectrum are listed in Tables 10 and 11.
Radiographic analysis
The disease control rats showed noticeable swelling of paw tissues representing inflammation. Also, narrowed joint spaces accompanying periarticular bone resorption were evident in radiological findings. On the other hand, rats treated with diclofenac Na, CESN, and AESN showed comparatively no remarkable changes (Fig. 12).
Discussion
Solanum nigrum L. has been extensively used in traditional medical practice for the treatment of various inflammatory conditions, rheumatism, and joint pain. Plant-derived constituents show good medicinal properties when extracted using organic solvents (Madane et al. 2013) which formed the basis of using four different organic solvents for extraction. The current study aimed to investigate the effect of Solanum nigrum L. in regulating the expression of inflammatory cytokines and the modulation of oxidative stress biomarkers in acute and sub-acute arthritis models. The in vitro anti-arthritic, anti-nociceptive, and in vivo acute anti-inflammatory potential of different extracts of Solanum nigrum L. leaves was determined. Two extracts (chloroform and aqueous) were further evaluated for sub-acute anti-arthritic activity in CFA-induced arthritis rat model as depicted by the dose–response data.
A plethora of powerful phytoconstituents especially flavonoids is believed to not only possess antioxidant capability but also cause significant inhibition of cyclooxygenases, phospholipase A2, and protein tyrosine kinase and therefore have great biological importance. Phenolic compounds moreover, by reduction of ROS expression pathways, are important anti-inflammatory constituents (Owolabi et al. 2018). The qualitative and quantitative analysis of all Solanum nigrum L. leaves extracts showed the presence of bioactive phytochemicals responsible for analgesic, anti-inflammatory, and anti-arthritic effects.
The HPLC analysis of all Solanum nigrum L. leaves extracts showed the presence of different bioactive phytoconstituents including: quercetin, ferulic acid, chlorogenic acid, gallic acid, syringic acid, sinapic acid, caffeic acid, p- and m-coumaric acid, cinnamic acid, and vanillic acid having significant anti-inflammatory properties; quercetin is believed to decrease the level of potent inflammatory mediators like prostaglandins and leukotrienes (David et al. 2016). The highest conc. of quercetin determined in the aqueous extract of Solanum nigrum L. was 13.90 µg/g. Another phytoconstituent present in AESN was the ferulic acid (39.74 µg/g) which has been found to remarkably inhibit IL-17-mediated RA severity and bone erosions (Ganesan and Rasool 2019). An important polyphenol identified in different extracts is the chlorogenic acid that defends against inflammatory conditions brought on by oxidative stress and has anti-edematous properties (Han et al. 2019). Numerous investigations have shown that the anti-inflammatory effects of gallic acid occur by inhibiting the release of myeloperoxidase and the activities of polymorphonuclear leukocytes (PMNs) (Karimi-Khouzani et al. 2017). Syringic acid has an anti-inflammatory effect via the regulation of different genes involved in inflammation (Ham et al. 2016). Chemically, sinapic acid is a derivative of cinnamic acid. It mediates anti-inflammatory action by decreasing the expression of iNOS and COX-2 (Yun et al. 2008). Cinnamic acid, however, is itself a derivative of phenolic acid causes cyclooxygenases and lipoxygenases to be inhibited (Hadjipavlou-Litina and Pontiki 2015). Caffeic acid and its derivatives have been found to have both antioxidant and pro-oxidant effects. These effects have been attributed to a combination of mechanisms, including radical scavenging action, prevention of lipid peroxidation, and protection against LDL oxidation (Khan et al. 2016). It is known that p-coumaric acid has anti-inflammatory properties by reducing the production of inflammatory mediators and circulating immune complexes (Zhu et al. 2018). Moreover, It is reported that tumor necrosis factor (TNF) and interleukin (IL-6) production is inhibited by vanillic acid, which increases lipopolysaccharide levels (Kim et al. 2011).
Since protein denaturation has been reported as the leading cause of RA (Qasim et al. 2021) for investigation of in vitro anti-arthritic effect, its inhibition using BSA was determined. All the extracts decreased BSA denaturation in vitro. However, the chloroform and aqueous extracts showed maximum inhibition in % protein denaturation. This ability of Solanum nigrum L. to stabilize protein denaturation is suggestive of its potential as an anti-arthritic agent.
Different physiological mediators like prostaglandins, bradykinins, and substance-P play a crucial role in mediating the complex pain response (Nguyen et al. 2020). Debilitating pain in joints due to arthritis is one of the leading symptoms. The analgesic activity of Solanum nigrum L. leaves extracts was determined using the hot plate method. Significant analgesia was reported with aqueous extract of Solanum nigrum L. at all doses 100, 200, and 300 mg/kg as compared to n-hexane, methanol, and chloroform extracts.
The biphasic inflammation process induced by carrageenan is one of the most widely studied models of acute inflammation. Varieties of inflammatory mediators like histamine, bradykinin, 5-hydroxytryptamine, prostaglandins, cyclooxygenases, etc. are released during this process (Fatima et al. 2021). All the plants' extracts showed significant anti-inflammatory potential against carrageenan-induced rat paw oedema. Maximum inhibition in paw oedema was observed with chloroform and aqueous extracts of 300 mg/kg each.
The most extensively used animal model to study clinical and histopathological changes associated with human RA is CFA-induced polyarthritis. In the CFA model, the chronic inflammation is exhibited as an increase in the paw size after induction of adjuvant and this occurs in two phases. The initial irritant reaction of adjuvant is causative of oedema formation followed by a late-phase secondary reaction leading to an immunologic response (Ijaz et al. 2021). The chloroform and aqueous extracts of Solanum nigrum L. (300 mg/kg) leave significantly decreased the size of injected paws and ankle joint diameter recorded with the help of a digital vernier caliper.
Since heat is responsible for causing local tissue damage and further inducing the release of inflammatory mediators, along with nociceptors sensitization. It ends up in pain as a cumulative response (Angst and Clark 2006). The analgesic effect of both extracts owes to the modulation of pain response as well as the down-regulation of inflammatory mediators.
The pathogenesis of RA has been linked with an augmentation in levels of pro-inflammatory mediators namely TNFα, IL-6, and IL-1β along with increased cyclooxygenase and nuclear factor ĸB levels (Kim et al. 2016). The above mediators have a key role in an adjuvant-induced arthritis model (Choudhary et al. 2018). Not only the tissue regeneration reduced by IL-1 and IL-6, the IL-1 also stimulates numerous inflammatory genes both locally and systemically. Hence, a decrease in the cytokine IL-1 plays an essential part in improving inflammation (Etemadi et al. 2022). A similar effect was observed in both treated groups administered with Chloroform and aqueous extracts of Solanum nigrum L. leaves extracts.
One of the prominent transcription factors in inflammatory response regulation is nuclear factor-kappa B, causing an upregulation of receptors necessary in immune cell functioning, as well as inducing transcription of various inflammatory cytokines like TNF-α, IL-6, IL-1β, and enzymes like COX-2 (Peng et al. 2012). The increased expression of TNF- alpha, IL-1, Il-6, and COX-2 results due to increased production of NF-κB leading to the development of polyarthritis. This role of NF- κB has also been established in the current study as well, shown by the upregulation of TNF-alpha, IL-6, and IL-1 in the diseased group. Pro-inflammatory cytokines-mediated upregulation of COX-2 leads to an indirect rise in PGE2 in an active RA disease (Fattahi and Mirshafiey 2012). PGES-2, a glutathione-independent microsomal subtype of PGE2, is remarkable in constitutively expressing and coupling with cyclooxygenases 1 and 2 to produce PGE2. The plant extracts downregulated levels of both COX-2 and PGES-2.
Another cytokine playing an important role in both innate and adaptive immune responses is interferon-gamma. Based upon its diverse role in physiological immunity, it has been hypothesized that IFN-gamma contributes to the development of RA. The current study also shows a linkage of increased IFN-gamma levels to the establishment of RA in CFA-induced animals, which were significantly improved after treatment with both extracts (Okada et al. 2014).
Interleukin-4 is a major anti-inflammatory cytokine and it impedes the formation of some very important pro-inflammatory cytokines like TNFα, IL-1β, and IL-6 by peripheral blood mononuclear cells, synovial tissue, and rheumatoid SF. Another anti-inflammatory cytokine named human cytokine synthesis inhibitory factor or interleukin-10 also decreases the formation of TNFα, IL-(1α, 1β, 6, 8, and 12), and GM-CSF (Mateen et al. 2016). Both of these anti-inflammatory cytokines were upregulated as a result of treatment with chloroform and aqueous extracts of Solanum nigrum L. leaves in CFA-induced arthritic rats.
The active inflammation in arthritis is evaluated by a convenient serum marker CRP which is an acute phase systemic reactant (Pepys 2003). CRP levels were increased in rats induced with CFA and subsequently decreased as a result of treatment with chloroform and aqueous extracts of Solanum nigrum L. leaves. Aggravated response to pathogenic stimuli results in a rise in WBCs and platelet count in CFA-induced arthritic rats (Perumal et al. 2017). Both plant extracts by modulation in immune response caused improvement in WBCs and platelet count. Low RBC count and resultant anemia have been previously reported widely in RA patients. Significant improvement in RBC count and hemoglobin conc. occurred after treatment with both extracts of Solanum nigrum L. leaves.
SOD, catalase, and GSH were estimated for oxidative stress in rat serum. Both extracts also exhibited antioxidant activities as apparent from the improvement of oxidative stress biomarkers. TNF-alpha is also one of the major cytokines and a strong inducer of pro-inflammatory cytokines causing a disturbance in the standard physiological equilibrium among pro- and anti-inflammatory mediators. Interleukin-6 carries out acute phase responses such as anemia, lipid-metabolism deregulation, and cognitive dysfunction through leukocyte activation and autoantibody production (Alam et al. 2017).
The GCMS analysis of chloroform extract showed the presence of 22 compounds and 18 compounds were determined in the aqueous extract. Docosanoic acid found in aqueous extract possesses high antioxidant activity as previously reported (Olukanni 2020). Hexadecanoic acid methyl ester possesses anti-arthritic effects as suggested by literature showing the potential of aqueous extract as an anti-inflammatory and anti-arthritic (Nabi et al. 2022). Tetradecanoic acid (lauric acid) presence in chloroform extract validates its antioxidant role since it has been reported to act as a lipid anchor in biological membranes (Obasi and Ogugua 2021).
Conclusion
The present results conclude that Solanum nigrum L. possesses analgesic, anti-inflammatory, and anti-arthritic potential. The chloroform and aqueous extracts have more marked anti-inflammatory and anti-arthritic activities as compared to n-hexane and methanol extracts. This owes to the presence of potent phenolics and flavonoids in Solanum nigrum L. that provide the basis for their use in RA. The chloroform and aqueous extracts of Solanum nigrum L. leaves showed promising anti-arthritic activity by regulating gene expression of different pro-inflammatory and anti-inflammatory cytokines namely, IL-1β, IL-6, NF-ĸB, IFN-γ, IL-4, and IL-10. Moreover, the modulation of biomarkers related to oxidative stress also shows the convincing role of both extracts in regulating the inflammatory process. The bioactive phytoconstituents, as revealed in GCMS analysis also validate its anti-arthritic potential making it a suitable choice as a rheumatoid arthritis remedy. Further experiments for the standardization of extracts and formulation of their safety profile are required.
Data availability statement
The datasets analyzed during the current study are not publicly available due to the confidentiality of Ph.D. research data but are available from the corresponding author on reasonable request.
Abbreviations
- RA:
-
Rheumatoid arthritis
- CFA:
-
Complete Freund’s adjuvant
- IL-1β:
-
Interleukin- 1Beta
- IL-4:
-
Interleukin-4
- IL-6:
-
Interleukin-6
- IL-10:
-
Interleukin- 10
- TNF-α:
-
Tumor necrosis factor-alpha
- COX-2:
-
Cycloxegenase-2
- NF-κB:
-
Nuclear factor-kappa B
- PGES-2:
-
Prostaglandin E synthase 2
- IFN-γ:
-
Interferon gamma
- CRP:
-
C-reactive protein
- PCR:
-
Polymerase chain reaction
- SOD:
-
Superoxide dismutase
- GSH:
-
Glutathione
- ACPA:
-
Anti-citrullinated protein/peptide antibody
- APC:
-
Antigen-presenting cells
- ELISA:
-
Enzyme-linked immunosorbent assay
References
Aduwamai UH, Abimbola MM, Ahmed ZH (2018) Effect of Solanum nigrum methanol leaf extract on phenylhydrazine induced anemia in rats. Jordan J Biol Sci 11(1):65–71
Alam J, Jantan I, Bukhari SNA (2017) Rheumatoid arthritis: recent advances on its etiology, role of cytokines and pharmacotherapy. Biomed Pharmacother 92:615–633
Alamgeer SA, Uttra AM, Hasan UH (2019) Alkaloids, flavonoids, polyphenols might be responsible for potent antiarthritic effect of Solanum nigrum. J Tradit Chin Med 39(5):632–641
Angst MS, Clark JD (2006) Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology 104(3):570–587
Bashir S, Niazi ZR (2020) Appraisal of in vitro, in vivo and multi-targeted molecular docking analysis of atorvastatin to elucidate its anti-arthritic potential. Pak J Pharm Sci 33(3):1183–1190
Choudhary N, Bhatt LK, Prabhavalkar KS (2018) Experimental animal models for rheumatoid arthritis. Immunopharmacol Immunotoxicol 40:193–200
David AVA, Arulmoli R, Parasuraman S (2016) Overviews of biological importance of quercetin: a bioactive flavonoid. Phcog Rev 10(20):84
Etemadi S, Abtahi Froushani SM, Hashemi Asl SM, Mahmoudian A (2022) Combined atorvastatin and pentoxifylline in ameliorating inflammation induced by complete Freund’s adjuvant. Inflammopharmacology 30:935–944
Fatima H, Shahid M, Jamil A, Naveed M (2021) Therapeutic potential of selected medicinal plants against carrageenan induced inflammation in rats. Dose-Response 19(4):15593258211058028
Fattahi MJ, Mirshafiey A (2012) Prostaglandins and rheumatoid arthritis. Arthritis. https://doi.org/10.1155/2012/239310
Fiume MM, Bergfeld WF, Belsito DV (2012) Safety assessment of stearylheptanoate and related stearylalkanoates as used in cosmetics. Int J Toxicol 31(suppl 2):141S-146S
Ganesan R, Rasool M (2019) Ferulic acid inhibits interleukin 17-dependent expression of nodal pathogenic mediators in fibroblast-like synoviocytes of rheumatoid arthritis. J Cell Biochem 120(2):1878–1893
Goel K, Ahmed MS, Singh R, Saini V, Bansal S (2022) A Sneak peek (1970–2021) into phytochemistry and ethnomedical properties of Solanum Nigrum Linn (Makoi). J Pharm Negat 22:576–594
Gul B, Anwar R, Saleem M, Noor A, Ullah MI (2023) Cassia absus-mediated upregulation of IL-4, IL-10 and downregulation of IL-1β, IL-6, TNF-α, NF-κB IFN-γ in CFA-Induced Arthritis Model. Inflammopharmacology 31(3):1241–1256
Hadjipavlou-Litina D, Pontiki E (2015) Aryl-acetic and cinnamic acids as lipoxygenase inhibitors with antioxidant, anti-inflammatory, and anticancer activity. In: Armstrong D (ed) Advanced protocols in oxidative stress. Springer, New York, NY, pp 361–377
Ham JR, Lee HI, Choi RY, Sim MO, Seo KI, Lee MK (2016) Anti-steatotic and anti-inflammatory roles of syringic acid in high-fat diet-induced obese mice. Food Funct 7(2):689–697
Han D, Gu X, Gao J, Wang Z, Liu G, Barkema HW, Han B (2019) Chlorogenic acid promotes the Nrf2/HO-1 anti-oxidative pathway by activating p21Waf1/Cip1 to resist dexamethasone induced apoptosis in osteoblastic cells. Free Radic Biol Med 137:1–12
Ijaz M, Fatima M, Anwar R, Uroos M (2021) Green synthesis of gold nanoparticles from Manilkara zapota L. extract and the evaluation of its intrinsic in vivo antiarthritic potential. RSC Adv 11(44):27092–27106
Karimi-Khouzani O, Heidarian E, Amini SA (2017) Anti-inflammatory and ameliorative effects of gallic acid on fluoxetine-induced oxidative stress and liver damage in rats. Pharmacol Rep 69:830
Khan FA, Maalik A, Murtaza G (2016) Inhibitory mechanism against oxidative stress of caffeic acid. J Food Drug Anal 24(4):695–702
Khodabakhsh P, Shafaroodi H, Asgarpanah J (2015) Analgesic and anti-inflammatory activities of Citrus aurantium L. blossoms essential oil (neroli): involvement of the nitric oxide/cyclic-guanosine monophosphate pathway. J Nat Med 69:324–331
Kim MC, Kim SJ, Kim DS, Jeon YD, Park SJ, Lee HS, Um Y, Hong SH (2011) Vanillic acid inhibits inflammatory mediators by suppressing NF-κB in lipopolysaccharide stimulated mouse peritoneal macrophages. Immunopharmacol Immunotoxicol 33:525–532
Kim W, Park S, Choi C, Kim YR, Park I, Seo C, Youn D, Shin W, Lee Y, Choi D (2016) Evaluation of anti-inflammatory potential of the new ganghwaljetongyeum on adjuvant-induced inflammatory arthritis in rats. Evid Based Complement Alternat Med 2016:1230294–1230304
Kuete V (2014) Physical, hematological and histopathological signs of toxicity induced by African medicinal plants. Toxicological survey of African medicinal plants pp. 635–657
Liu Y, Zhang Z, Jin Q, Liu Y, Kang Z, Huo Y, He Z, Feng X, Yin J, Wu X, Wang H (2019) Hyperprolactinemia is associated with a high prevalence of serum autoantibodies, high levels of inflammatory cytokines and an abnormal distribution of peripheral B-cell subsets. Endocrine 64:648–656
Madane AN, Kamble SK, Patil BJ, Aparadh VT (2013) Assessment of solvent solubility by using phytochemical screen tests of some Euphorbiaceae members. Asian J Pharm Res 3:53–55
Mahdi HJ, Khan NAK, Asmawi MZB, Mahmud R, Vikneswaran A, Murugaiyah L (2018) In vivo anti-arthritic and anti-nociceptive effects of ethanol extract of Moringa oleifera leaves on complete Freund’s adjuvant (CFA)-induced arthritis in rats. Integr Med Res 7(1):85–94
Mateen S, Zafar A, Moin S, Khan AQ, Zubair S (2016) Understanding the role of cytokines in the pathogenesis of rheumatoid arthritis. Clin Chim Acta 455:161–171
Nabi M, Zargar MI, Tabassum N, Ganai BA, Wani SUD, Alshehri S, Alam P, Shakeel F (2022) Phytochemical profiling and antibacterial activity of methanol leaf extract of Skimmia anquetilia. Plants 11(13):1667
Nancy P, Ashlesha V (2015) Pharmacognostic and phytochemical studies of Cassia absus seeds extract. Int J Pharm Pharm Sci 8:325–332
Nguyen T, Chen X, Chai J, Li R, Han X, Chen X, Liu S, Chen M, Xu X (2020) Antipyretic, anti-inflammatory and analgesic activities of Periplaneta americana extract and underlying mechanisms. Biomed Pharmacother 123:109753
Obasi DC, Ogugua VN (2021) GC-MS analysis, pH and antioxidant effect of Ruzu herbal bitters on alloxan-induced diabetic rats. Biochem Biophys Rep 27:101057
Okada Y, Wu D, Trynka G, Raj T, Terao C, Ikari K, Kochi Y, Ohmura K, Suzuki A, Yoshida S, Graham RR (2014) Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506(7488):376–381
Olukanni A (2020) Antioxidant and in vitro anti-inflammatory activities of Albizia zygia (DC) JF mebr and the evaluation of its phytochemical constituents. J Med Plants Stud 8(4):317–323
Owolabi OO, James DB, Sani I, Andongma BT, Fasanya OO, Kure B (2018) Phytochemical analysis, antioxidant and anti-inflammatory potential of Feretia apodanthera root bark extracts. BMC Complement Altern Med 18(1):1–9
Peng M, Wang YL, Wang FF, Chen C, Wang CY (2012) The cyclooxygenase-2 inhibitor parecoxib inhibits surgery-induced pro inflammatory cytokine expression in the hippocampus in aged rats. J Surg Res 178(1):e1–e8
Pepys MB, Hirchfield GM (2003) C-reactive protein: a critical update. J Clin Invest 111(12):1805–1812
Perumal SS, Ekambaram SP, Dhanam T (2017) In vivo antiarthritic activity of the ethanol extracts of stem bark and seeds of Calophyllum inophyllum in Freund’s complete adjuvant induced arthritis. Pharm Boil 55(1):1330–1336
Qasim S, Alamgeer SM, Alotaibi NH, Bukhari SN, Alharbi KS, Irfan HM, Anwar R (2021) Appraisal of the antiarthritic potential of prazosin via inhibition of proinflammatory cytokine TNF-α: a key player in rheumatoid arthritis. ACS Omega 6(3):2379–2388
Quiñonez-Flores CM, González-Chávez SA, Del Rio ND, Pacheco-Tena C (2016) Oxidative stress relevance in the pathogenesis of the rheumatoid arthritis: a systematic review. BioMed Res Int 2016:6097417–6097431
Rasheed UR (2022) Antiarthritic and anti-inflammatory activity of Solanum nigrum leaves extract on CFA-induced arthritic rat model. Journal of xi’an Shiyou University. Nat 18(11):840–853
Saleem A, Saleem M, Akhtar MF, Shahzad M, Jahan S (2020) Moringa rivae leaf extracts attenuate Complete Freund’s adjuvant induced arthritis in Wistar rats via modulation of inflammatory and oxidative stress biomarkers. Inflammopharmacology 28:139–151
Scherer HU, Häupl T, Burmester GR (2020) The etiology of rheumatoid arthritis. J Autoimmune 110:102400
Shahmohamadnejad S, Vaisi-Raygani A, Shakiba Y, Kiani A, Rahimi Z, Bahrehmand SE (2015) Association between butyrylcholinesterase activity and phenotypes, paraoxonase192 rs662 gene polymorphism and their enzymatic activity with severity of rheumatoid arthritis: correlation with systemic inflammatory markers and oxidative stress, preliminary report. Clin Biochem 48(1–2):63–69
Singh S, Singh TG, Mahajan K, Dhiman S (2020) Medicinal plants used against various inflammatory biomarkers for the management of rheumatoid arthritis. J Pharm Pharmacol 72:1306–1327
Smolen JS, Aletaha D (2015) Rheumatoid arthritis therapy reappraisal: strategies, opportunities and challenges. Nat Rev Rheumatol 11(5):276–289
Uroos M, Abbas Z, Sattar S, Umer N, Shabbir A, Sharif A (2017) Nyctanthes arbor-tristis ameliorated FCA-induced experimental arthritis: a comparative study among different extracts. Evid Based Complement Altern Med 2017:1–5
Veerapagu M, Jeya KR, Sankaranarayanan A, Rathika A (2018) In vitro antioxidant properties of methanolic extract of Solanum nigrum L. fruit. Pharma Innov 7(5):371
Yun KJ, Koh DJ, Kim SH, Park SJ, Ryu JH, Kim DG, Lee JY, Lee KT (2008) Anti-inflammatory effects of sinapic acid through the suppression of inducible nitric oxide synthase, cyclooxygase-2, and proinflammatory cytokines expressions via nuclear factor kappaB inactivation. J Agric Food Chem 56(21):10265–10272
Zhang QR, Zhong ZF, Sang W, Xiong W, Tao HX, Zhao GD, Li ZX, Ma QS, Tse AKW, Hu YJ, Yu H (2019) Comparative comprehension on the anti-rheumatic Chinese herbal medicine Siegesbeckiae Herba: combined computational predictions and experimental investigations. J Ethnopharmacol 228:200–209
Zhao X, Kim YR, Min Y, Zhao Y, Do K, Son YO (2021) Natural plant extracts and compounds for rheumatoid arthritis therapy. Medicina 57(3):266
Zhu H, Liang QH, Xiong XG, Wang Y, Zhang ZH, Sun MJ, Lu X, Wu D (2018) Anti-inflammatory effects of p-coumaric acid, a natural compound of Oldenlandia difusa, on arthritis model rats. Evid Based Complement Altern Med 2018:5198594–5198603
Acknowledgements
The authors express their gratitude to Punjab University College of Pharmacy (PUCP), University of the Punjab Lahore, Pakistan for providing facilities for the conduct of this Ph.D. project of 01-P-PCOL/15a.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
The study was designed and supervised by RA and MS. Material preparation, data collection, and experiments were performed by BG. HPLC GC–MS data interpreted by SK. The data analysis was done by BG and MA. Manuscript writing was done by BG, MIU, and SK. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gul, B., Anwar, R., Saleem, M. et al. Attenuation of CFA-induced arthritis through regulation of inflammatory cytokines and antioxidant mechanisms by Solanum nigrum L. leaves extracts. Inflammopharmacol 31, 3281–3301 (2023). https://doi.org/10.1007/s10787-023-01357-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01357-z