Abstract
Background
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease characterized by joint swelling, pain, and deformation. RA patients have an increased risk of thyroid dysfunction, and drugs of RA treatment may have potential effects on thyroid function.
Methods
This is a single-center cross-sectional study including 281 inpatients with RA in the First Affiliated Hospital of Guangzhou University of Chinese Medicine. The purpose of this study is to explore the correlation between RA therapeutic drugs and thyroid function. The medical records of 281 inpatients with RA were collected, including general data, laboratory examination, complications, and RA treatment. Spearman correlation analysis was used to explore the association of independent variables with thyroid function and antibodies in RA patients. Multinomial logistics and binary logistic regression were used for multivariate analysis. The statistically significance level was set as P < 0.05. SPSS 22.0 was used for statistical analysis.
Results
Patients taking methotrexate (OR = 0.067, 95%CI: 0.008–0.588, P = 0.015) had lower levels of total thyroxine (TT4) (TT4 < 78.38 nmol/L). There was a negative correlation between glucocorticoids (r = − 0.153, P = 0.010) and total triiodothyronine (TT3) level (TT3 ≥ 1.34 nmol/L), but it was not significant in the multivariate regression model of TT3, although the regression model was statistically significant (P = 0.001).
Conclusion
Methotrexate is associated with decreased TT4 levels in RA patients, and glucocorticoids is associated with decreased TT3 levels. Drugs of RA treatment may affect the thyroid function of patients while treating RA, which may be one of the causes of secondary thyroid diseases in RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease characterized by symmetrical swelling, pain, and stiffness of joints, which can lead to joint deformity and limitation of joint activity, seriously affecting the quality of life of patients (Komatsu and Takayanagi 2022). The typical laboratory manifestations of RA patients were positive for rheumatoid factor (RF) and anti-citrullinated protein antibody (ACPA), and elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) levels (Aletaha et al. 2010). Narrowing of joint space and destruction of joint structure could be observed on imaging. The treatment of RA includes glucocorticoids (GCs), nonsteroidal anti-inflammatory drugs (NSAIDs), and disease-modifying antirheumatic drugs (DMARDs) (Fraenkel et al. 2021).
The thyroid is one of the targets of autoimmune disease. Thyroid dysfunction can not only lead to thyroid lesions, but also related to the increased risk of mortality of diseases such as heart disease (Biondi et al. 2019). Serum thyroid hormones (THs) and thyroid autoantibodies (TAbs) are important indicators for screening early thyroid diseases. THs contain triiodothyronine (T3) and thyroxine (T4). Thyroid-stimulating hormone (TSH) can promote the production of T3 and T4 and regulate growth, development and metabolism with them (Jing and Zhang 2022). The positive results of anti-thyroglobulin antibody (TgAb) and anti-thyroperoxidase antibody (TPOAb) suggest thyroid immune diseases (Dwivedi et al. 2022).
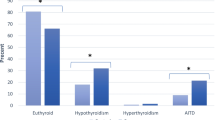
Many studies have shown that there is an association between RA and thyroid diseases. Compared with non-RA patients, RA patients have an increased risk of thyroid dysfunction (Liu et al. 2022). The level of THs in RA patients are related to serum ESR and RF levels (Atzeni et al. 2008). RA patients with positive TAbs had higher disease activity score-28 and more severe joint damage than those with negative TAbs (Chen et al. 2018). However, the effect of RA treatment on thyroid function is often ignored. A Swedish study showed that the prevalence of autoimmune thyroid diseases (AITD) in RA patients increased in the five years before the diagnosis of RA, with a prevalence of 10.3% at the time of diagnosis of RA (Waldenlind et al. 2018). After the diagnosis of RA, the risk of AITD was reduced. This result may indicate the potential impact of drugs of RA treatment on thyroid function.
Therefore, the purpose of this study is to explore the correlation between RA therapeutic drugs and THs and TAbs.
Subjects and methods
Data and sample sources
This is a single-center cross-sectional study. This study does not involve identifiable personal information and meets the criteria of exempting patients’ informed consent from the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (FAHGUCM). The commitment to protect the privacy of subjects has been submitted to the Ethics Committee. This study has been approved by the Ethics Committee of FAHGUCM (NO. JY[2021]063).
The medical records of 281 inpatients with RA in FAHGUCM from July 2014 to June 2021 were collected, including general data, laboratory examination, complications and RA treatment. The diagnosis was made according to the 2010 American College of Rheumatology (ACR)/European Alliance of Association for Rheumatology RA classification criteria (Aletaha et al. 2010).
Patients under 18 years old, pregnant women, patients with a history of thyroid diseases before the first diagnosis of RA, patients with a history of taking drugs affecting thyroid function, neck surgery, neck regional radiotherapy, tumor, hypothalamus or pituitary diseases were excluded from the study (Fig. 1).
Assessment of thyroid function and thyroid antibodies
Blood samples of patients were obtained from the inpatient department of FAHGUCM. TSH, total triiodothyronine (TT3), total thyroxine (TT4), Free T3 (FT3), and Free T4 (FT4) were detected using microparticle chemiluminescence method with BECKMAN COULTER UniCel DxI 800 Access. TgAb and TPOAb were detected using acridine ester chemiluminescence method with Abbott U.S. ARCHITECT i2000SR.
Thyroid function and thyroid antibodies were treated as outcome variables in this study. Patients were divided into groups according to the distribution of patients and the reference range of laboratory tests. TSH was categorized as < 0.56, 0.56–5.91 and > 5.91 mIU/L. TT3 was categorized as < 1.34 and ≥ 1.34 nmol/L. TT4 was categorized as < 78.38 and ≥ 78.38 nmol/L. FT3 was categorized as < 3.8 and ≥ 3.8 pmol/L. FT4 was categorized as ≤ 12.49 and > 12.49 pmol/L. TgAb was categorized as TgAb (+) and TgAb (−). TPOAb was categorized as TPOAb (+) and TPOAb (−).
Subgroup analysis
Variables that may affect thyroid function and thyroid antibodies in RA patients were included in this study, as detailed in Supplementary information (SI) 1. The detection methods and instruments used for laboratory tests in the variables are shown in SI 2. In the subgroup analysis, patients were grouped according to the reference range of laboratory tests provided by the kit instructions and the distribution of patients (SI 3).
Statistical analysis
SPSS 22.0 was used for statistical analysis. The normality of the quantitative data was evaluated by the Shapiro–Wilk test. The data with abnormal distribution were presented as median (Interquartile range [IQR]), and the data with normal distribution were presented as mean ± standard deviation (SD). Qualitative data were presented as number and percentage. In the subgroup analysis, Spearman correlation analysis was used to explore the association of independent variables with thyroid function and antibodies in RA patients. The significant variables in the Spearman correlation analysis were included in the multivariate analysis, using multinomial logistics regression and enter method in binary logistic regression. The statistically significance level was set as P < 0.05.
Results
Baseline characteristics of participants
A total of 281 participants were enrolled, of whom 78.6% were females and 21.4% were males, with an average age of 56.57 ± 12.52 years and the median RA duration of 72.0 (24.0,144.0) months. The baseline characteristics of RA participants are shown in Table 1.
Subgroup analysis of TSH
Spearman correlation analysis was used to explore the association between variables and TSH in 281 RA patients. The results showed that heart diseases (r = − 0.145, P = 0.015) and glucose (Glu) ≥ 6.1 mmol/L (r = − 0.118, P = 0.049) were negatively correlated with TSH level, while RF ≥ 160 IU/mL (r = 0.147, P = 0.013) and anti-double-stranded DNA (dsDNA) antibody (+) (r = 0.134, P = 0.024) were positively correlated with TSH level. The association between TSH and variables in RA patients is shown in supplemental Table S1.
Heart disease, Glu, RF, and anti-dsDNA antibody (+) were incorporated in the multinomial logistics regression model of TSH (Table 2). The regression model was statistically significant (P = 0.001). Among them, RA patients with heart diseases (P = 0.008, OR = 3.102, 95%CI: 0.990–9.723) had lower TSH levels (TSH < 0.56 mIU/L), and RF ≥ 160 IU/mL (P = 0.029, OR = 2.745, 95%CI: 1.019–7.396) was the high-risk factor for the increased TSH (TSH > 5.91 mIU/L).
Subgroup analysis of TT3
Spearman correlation analysis was used to explore the association between variables and TT3 in 281 RA patients. The results showed that GCs (r = − 0.153, P = 0.010), Glu ≥ 6.1 mmol/L (r = − 0.213, P < 0.001), white blood cell (WBC) ≥ 10 × 109/L (r = − 0.170, P = 0.004), neutrophil (NEU) ≥ 7.5 × 109/L (r = − 0.204, P = 0.001), red blood cell (RBC) < 3.5 × 1012/L (r = − 0.160, P = 0.007), hemoglobin (HGB) < 110 g/L (r = − 0.259, P < 0.001), platelet (PLT) ≥ 300 × 109/L (r = − 0.193, P = 0.001), ESR ≥ 15 mm/h (r = − 0.141, P = 0.018), CRP ≥ 8 mg/L (r = − 0.245, P < 0.001), and complement 4 (C4) < 0.16 g/L (r = − 0.142, P = 0.017) were negatively correlated with TT3 ≥ 1.34 nmol/L. The association between TT3 and variables in RA patients is shown in supplemental Table S2.
GCs, Glu, WBC, NEU, RBC, HGB, PLT, ESR, CRP, and C4 were incorporated in the binary logistic regression model of TT3 (Table 3). The regression model was statistically significant (P < 0.001). Among them, RA patients with Glu ≥ 6.1 mmol/L (OR = 0.234, 95%CI: 0.094–0.582, P = 0.002), HGB < 110 g/L (OR = 0.387, 95%CI: 0.206–0.728, P = 0.003) or C4 < 0.16 g/L (OR = 0.399, 95%CI: 0.177–0.898, P = 0.026) had lower TT3 levels (TT3 < 1.34 nmol/L).
Subgroup analysis of TT4
Spearman correlation analysis was used to explore the association between variables and TT4 in 281 RA patients. The results showed that methotrexate (MTX) (r = − 0.161, P = 0.007) and total cholesterol (T-Chol) ≥ 5.2 mmol/L (r = − 0.125, P = 0.036) were negatively correlated with TT4 ≥ 78.38 nmol/L. The association between TT4 and variables in RA patients is shown in supplemental Table S3.
MTX and T-Chol were incorporated in the binary logistic regression model of TT4 (Table 4). The regression model was statistically significant (P = 0.002). Among them, patients taking MTX (OR = 0.067, 95%CI: 0.008–0.588, P = 0.015) or with T-Chol ≥ 5.2 mmol/L (OR = 0.147, 95%CI: 0.030–0.715, P = 0.018) had lower levels of TT4 (TT4 < 78.38 nmol/L).
Subgroup analysis of FT3
Spearman correlation analysis was used to explore the association between variables and FT3 in 281 RA patients. The results showed that GCs (r = − 0.128, P = 0.032), NEU ≥ 7.5 × 109/L (r = − 0.119, P = 0.047), RBC < 3.5 × 1012/L (r = − 0.199, P = 0.001), HGB < 110 g/L (r = − 0.144, P = 0.015), anti-dsDNA antibody (+) (r = − 0.123, P = 0.039), and complement 3 (C3) < 0.79 g/L (r = − 0.124, P = 0.038) were negatively correlated with FT3 ≥ 3.8 pmol/L. The association between FT3 and variables in RA patients is shown in supplemental Table S4.
GCs, NEU, RBC, HGB, anti-dsDNA antibody, and C3 were incorporated in the binary logistic regression model of FT3 (Table 5). The regression model was statistically significant (P = 0.001). However, there was no statistical difference among the variables.
Subgroup analysis of FT4
Spearman correlation analysis was used to explore the association between variables and FT4 in 281 RA patients. The results showed that gastrointestinal diseases (r = 0.153, P = 0.010), WBC ≥ 10 × 109/L (r = 0.156, P = 0.009), HGB < 110 g/L (r = 0.146, P = 0.014), PLT ≥ 300 × 109/L (r = 0.267, P < 0.001) and CRP ≥ 8 mg/L (r = 0.213, P < 0.001) were positively correlated with FT4 > 12.49 pmol/L. The association between FT4 and variables in RA patients is shown in supplemental Table S5.
Gastrointestinal diseases, WBC, HGB, PLT, and CRP were incorporated in the binary logistic regression model of FT4 (Table 6). The regression model was statistically significant (P < 0.001). Among them, patients with gastrointestinal diseases (OR = 2.770, 95%CI: 1.291–5.947, P = 0.009) or PLT ≥ 300 × 109/L (OR = 2.157, 95%CI: 1.232–3.777, P = 0.007) had higher FT4 levels (FT4 > 12.49 pmol/L).
Subgroup analysis of TgAb
Spearman correlation analysis was used to explore the association between variables and TgAb in 281 RA patients. The results showed that autoimmune diseases (r = 0.127, P = 0.033) and anti-dsDNA antibody (+) (r = 0.153, P = 0.010) were positively correlated with TgAb (+), while gastrointestinal diseases (r = − 0.175, P = 0.003) were negatively correlated with TgAb (+). The association between TgAb and variables in RA patients is shown in supplemental Table S6.
Autoimmune diseases, gastrointestinal diseases and anti-dsDNA antibody were incorporated in the binary logistic regression model of TgAb (Table 7). The regression model was statistically significant (P < 0.001). Among them, autoimmune diseases (OR = 1.985, 95%CI: 1.083–3.640, P = 0.027) and anti-dsDNA antibody (+) (OR = 3.250, 95%CI: 1.308–8.074, P = 0.011) were the high-risk factors for TgAb (+). RA patients with gastrointestinal diseases (OR = 0.266, 95%CI: 0.106–0.669, P = 0.005) are less likely to be TgAb positive.
Subgroup analysis of TPOAb
Spearman correlation analysis was used to explore the association between variables and TPOAb in 281 RA patients. The results showed that osteoporosis (r = − 0.123, P = 0.040) was negatively correlated with TPOAb (+). The association between TPOAb and variables in RA patients is shown in supplemental Table S7.
Discussion
In our cross-sectional study of 281 subjects, we observed that RA patients treated with MTX were more likely to have lower TT4 levels than those without MTX. In correlation analysis, RA patients treated with GCs were more likely to have lower TT3 levels, but this result was not significant in regression model, although the regression model was statistically significant. Our results suggest that MTX may be an independent risk factor for TT4 reduction in RA patients.
A study in Sweden showed that young RA patients with AITD had a lower initial response rate to MTX, but this effect was not found in older patients (Waldenlind et al. 2020). Tokumaru reported a RA patient with thyroid lymphoid hyperplasia. The patient’s symptoms were alleviated after discontinuation of MTX (Tokumaru et al. 2021). On the other hand, MTX is considered as a potential effective drug for the treatment of Graves’ ophthalmopathy (Genere and Stan 2019). In a study by Sipkova et al., MTX was shown to reduce disease activity and decrease glucocorticoid usage in patients with active thyroid eye disease, which may be related to the reduction of non-site-specific immune responses by the intervention of cellular immune pathways (Sipkova et al. 2018; Strianese and Rossi 2019). However, the mechanism of MTX on thyroid function remains unclear.
Many studies have shown the correlation between RA and thyroid dysfunction. It is easy to find evidence to support the association between drugs of RA treatment and thyroid without considering the impact of RA. Celecoxib can significantly reduce serum TSH levels in rats (Selmanoğlu et al. 2006). Mild to moderate lymphoid areas and mild glial deformation can be observed in thyroid tissues of rats treated with celecoxib. The increased vacuoles in the colloid indicate that it has more hormone secretion activity. Re et al. found that serum basal TSH level, the production rates of TSH, TSH peak response to thyrotropin-releasing hormone (TRH) and TSH reserve decreased and TSH metabolic clearance rates increased after dexamethasone treatment in 8 normal subjects, while basal prolactin (PRL), peak PRL after TRH and PRL reserve did not change after dexamethasone administration (Re et al. 1976). At the same time, the TT3 and FT3 levels of patients decreased. The patient’s TSH level increased after taking metyrapone to reduce plasma cortisol levels. This may suggest that high-dose dexamethasone can directly inhibit pituitary TSH secretion. In addition, the physiological level of circulating cortisol also has an inhibitory effect on serum TSH. Kasono et al. reported that serum FT3 levels increased in 3 patients after treatment with diclofenac, and decreased to normal levels after discontinuation of diclofenac (Kasono et al. 2001). Diclofenac can promote the release of FT3 or FT4 from thyroid hormone-binding protein, resulting in a decrease in TSH and a slight increase in FT3 and FT4. Also, the cross reaction between diclofenac and FT3 in some kits may lead to false-positive FT3, which can be avoided by improving anti-FT3 antibodies.
Although these drugs may affect THs or TAbs, they are still widely used in the treatment of RA. According to common sense, these drugs are undoubtedly an important factor leading to thyroid dysfunction in RA patients. However, when the drugs are mixed with various factors to calculate their effects on thyroid function in RA patients, we find that the effects of drugs are not as much as speculated. In this study, NSAIDs, LEF, IGU, HCQ, tofacitinib, and etanercept did not show correlation with THs and TAbs in RA patients. RA patients treated with GCs showed lower TT3 levels, but there was no significant difference in regression analysis, which may be related to the small number of samples included. In addition, the confounding factors of multivariate analysis may also interfere with the statistical results. It is worth noting that some drugs of RA treatment have therapeutic effects on thyroid diseases. LEF can down-regulate the neuroendocrine markers ASCL1 and chromaffin A, and inhibit the proliferation of human medullary thyroid cancer cells in a dose-dependent manner (Alhefdhi et al. 2013). Bliddal et al. showed that biological DMARDs did not induce or aggravate autoimmune thyroid diseases, but had a tendency to reduce TPOAb and TgAb concentrations and reduce TSH levels in patients with hypothyroidism (Bliddal et al. 2017). Rituximab is a commonly used drug for the treatment of RA. Studies have found that it can be used to treat Graves’ disease and Graves’ orbitopathy. Compared with Graves’ disease patients treated with antithyroid drugs alone, patients treated with rituximab combined with antithyroid drugs had higher remission rate and lower recurrence rate, which may be related to B cell depletion caused by rituximab and its reduction of TRAb titer (Supronik et al. 2022). The improvement of thyroid function was observed in patients with hypothyroidism or TPOAb positive patients treated with adalimumab for 6 months, including the decrease of TSH level and TPOAb titer (Raterman et al. 2011). However, some studies show the opposite results. Cañas CA reported a 32-year-old man who developed fever and thyroid pain after 8 months of etanercept treatment for RA (Cañas et al. 2009). Thyroid biopsy showed granulomatous thyroiditis. After ceasing etanercept treatment and administering steroid therapy, the patient’s clinical and laboratory results improved. Another study showed that etanercept may cause subacute thyroiditis in RA patients (Hella et al. 2017).
In addition to drugs, we found that other factors in RA may be related to thyroid function in RA patients. In our study, we found that the higher level of RF is associated with the increase of TSH. However, this may be related to the fact that RF can interfere with the TSH results detected by chemiluminescent and IRMA assays, resulting in a false increase in TSH (Georges et al. 2011). We also found that RA patients with low C4 have lower TT3 levels, and patients with other autoimmune diseases or anti-dsDNA antibody positive are more likely to develop TgAb (+). Anti-dsDNA antibody was positive in some RA patients, and cytoplasmic dsDNA was involved in the pathological process of RA synovitis (Wang et al. 2019). Studies by SiriwardhaneT et al. showed that 26.9% of TgAb-positive patients were positive for anti-dsDNA or autoantibodies to extractable nuclear antigens, which was associated with autoimmune diseases (Siriwardhane et al. 2018).
In addition to that, several factors such as comorbid heart disease in RA patients, as well as Glu, T-Chol and HGB levels, were also found to be associated with thyroid function in this study. These factors and thyroid function are mutually causal, and their correlation seems to be more due to thyroid diseases rather than RA, which needs to be further clarified by more studies (Liu et al. 2022; Wang et al. 2023; Kjaergaard et al. 2022).
Conclusion
Our study shows that MTX is associated with decreased TT4 levels in RA patients, and GCs is associated with decreased TT3 levels. Drugs of RA treatment may affect the thyroid function of patients while treating RA, which may be one of the causes of secondary thyroid diseases in RA patients. However, the mechanism of RA therapeutic drugs on thyroid needs to be further clarified.
Availability of data and materials
All data are available for publication.
References
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62(9):2569–2581. https://doi.org/10.1002/art.27584
Alhefdhi A, Burke JF, Redlich A et al (2013) Leflunomide suppresses growth in human medullary thyroid cancer cells. J Surg Res 185(1):212–216. https://doi.org/10.1016/j.jss.2013.05.089
Atzeni F, Doria A, Ghirardello A et al (2008) Anti-thyroid antibodies and thyroid dysfunction in rheumatoid arthritis: prevalence and clinical value. Autoimmunity 41(1):111–115. https://doi.org/10.1080/08916930701620100
Biondi B, Cappola AR, Cooper DS (2019) Subclinical hypothyroidism: a review. JAMA 322(2):153–160. https://doi.org/10.1001/jama.2019.9052
Bliddal S, Borresen SW, Feldt-Rasmussen U (2017) Thyroid autoimmunity and function after treatment with biological antirheumatic agents in rheumatoid arthritis. Front Endocrinol (Lausanne) 8:179. https://doi.org/10.3389/fendo.2017.00179
Cañas CA, Tobón GJ, Arango LG et al (2009) Developing of granulomatous thyroiditis during etanercept therapy. Clin Rheumatol 28(Suppl 1):S17–S19. https://doi.org/10.1007/s10067-008-1046-2
Chen YL, Lin JZ, Mo YQ et al (2018) Joint damage is amplified in rheumatoid arthritis patients with positive thyroid autoantibodies. PeerJ 6:e4216. https://doi.org/10.7717/peerj.4216
Dwivedi SN, Kalaria T, Buch H (2022) Thyroid autoantibodies. J Clin Pathol. https://doi.org/10.1136/jcp-2022-208290
Fraenkel L, Bathon JM, England BR et al (2021) 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol 73(7):1108–1123. https://doi.org/10.1002/art.41752
Genere N, Stan MN (2019) Current and emerging treatment strategies for Graves’ orbitopathy. Drugs 79(2):109–124. https://doi.org/10.1007/s40265-018-1045-9
Georges A, Charrié A, Raynaud S et al (2011) Thyroxin overdose due to rheumatoid factor interferences in thyroid-stimulating hormone assays. Clin Chem Lab Med 49(5):873–875. https://doi.org/10.1515/CCLM.2011.144
Hella Z, Hodinka L, Turbucz P et al (2017) Etanercept-induced subacute thyroiditis. Case report and literature review. Orv Hetil 158(39):1550–1554. https://doi.org/10.1556/650.2017.30796
Jing L, Zhang Q (2022) Intrathyroidal feedforward and feedback network regulating thyroid hormone synthesis and secretion. Front Endocrinol (Lausanne) 13:992883. https://doi.org/10.3389/fendo.2022.992883
Kasono K, Hikino H, Fujino S et al (2001) Cross-reactive mechanism for the false elevation of free triiodothyronine in the patients treated with diclofenac. Endocr J 48(6):717–722. https://doi.org/10.1507/endocrj.48.717
Kjaergaard AD, Teumer A, Marouli E et al (2022) Thyroid function, pernicious anemia and erythropoiesis: a two-sample Mendelian randomization study. Hum Mol Genet 31(15):2548–2559. https://doi.org/10.1093/hmg/ddac052
Komatsu N, Takayanagi H (2022) Mechanisms of joint destruction in rheumatoid arthritis - immune cell-fibroblast-bone interactions. Nat Rev Rheumatol 18(7):415–429. https://doi.org/10.1038/s41584-022-00793-5
Liu YJ, Miao HB, Lin S et al (2022) Association between rheumatoid arthritis and thyroid dysfunction: a meta-analysis and systematic review. Front Endocrinol (Lausanne) 13:1015516. https://doi.org/10.3389/fendo.2022.1015516
Liu Y, Li Z, Yang T et al (2022) Impaired sensitivity to thyroid hormones and carotid plaque in patients with coronary heart disease: a RCSCD-TCM study in China. Front Endocrinol (Lausanne) 13:940633. https://doi.org/10.3389/fendo.2022.940633
Raterman HG, Jamnitski A, Lems WF et al (2011) Improvement of thyroid function in hypothyroid patients with rheumatoid arthritis after 6 months of adalimumab treatment: a pilot study. J Rheumatol 38(2):247–251. https://doi.org/10.3899/jrheum.100488
Re RN, Kourides IA, Ridgway EC et al (1976) The effect of glucocorticoid administration on human pituitary secretion of thyrotropin and prolactin. J Clin Endocrinol Metab 43(2):338–346. https://doi.org/10.1210/jcem-43-2-338
Selmanoğlu G, Koçkaya EA, Akay MT et al (2006) Subacute toxicity of celecoxib on thyroid and testis of rats: hormonal and histopathological changes. Environ Toxicol Pharmacol 22(1):85–89. https://doi.org/10.1016/j.etap.2005.12.004
Sipkova Z, Insull EA, David J et al (2018) Early use of steroid-sparing agents in the inactivation of moderate-to-severe active thyroid eye disease: a step-down approach. Clin Endocrinol (Oxf) 89(6):834–839. https://doi.org/10.1111/cen.13834
Siriwardhane T, Krishna K, Ranganathan V et al (2018) Exploring systemic autoimmunity in thyroid disease subjects. J Immunol Res 2018:6895146. https://doi.org/10.1155/2018/6895146
Strianese D, Rossi F (2019) Interruption of autoimmunity for thyroid eye disease: B-cell and T-cell strategy. Eye (Lond) 33(2):191–199. https://doi.org/10.1038/s41433-018-0315-9
Supronik J, Szelachowska M, Kretowski A et al (2022) Rituximab in the treatment of Graves’ orbitopathy: latest updates and perspectives. Endocr Connect 11(12):e220303. https://doi.org/10.1530/EC-22-0303
Tokumaru M, Ohba K, Kakudo K et al (2021) Importance of imaging procedures in the evaluation of methotrexate-associated lymphoproliferative disorder of the thyroid gland: a case study. Eur Thyroid J 10(5):434–436. https://doi.org/10.1159/000507826
Waldenlind K, Saevarsdottir S, Bengtsson C et al (2018) Risk of thyroxine-treated autoimmune thyroid disease associated with disease onset in patients with rheumatoid arthritis. JAMA Netw Open 1(6):e183567. https://doi.org/10.1001/jamanetworkopen.2018.3567
Waldenlind K, Delcoigne B, Saevarsdottir S et al (2020) Does autoimmune thyroid disease affect rheumatoid arthritis disease activity or response to methotrexate? RMD Open 6(2):e001282. https://doi.org/10.1136/rmdopen-2020-001282
Wang J, Li R, Lin H et al (2019) Accumulation of cytosolic dsDNA contributes to fibroblast-like synoviocytes-mediated rheumatoid arthritis synovial inflammation. Int Immunopharmacol. 76:105791. https://doi.org/10.1016/j.intimp.2019.105791
Wang Q, Xu X, Ren H et al (2023) Prevalence and risk factors of thyroid dysfunction in outpatients with overweight or obese first-episode and drug-naïve major depressive disorder. J Affect Disord 328:135–140. https://doi.org/10.1016/j.jad.2023.02.068
Funding
There was no funding for the study.
Author information
Authors and Affiliations
Contributions
SL-C conceived the study, collected the data, and drafted the manuscript. QX participated in designing and writing this manuscript. CS-L reviewed and revised this manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical statement
This study does not involve identifiable personal information and meets the criteria of exempting patients’ informed consent from the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (FAHGUCM). The commitment to protect the privacy of subjects has been submitted to the Ethics Committee. This study has been approved by the Ethics Committee of FAHGUCM (NO. JY [2021]063).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, SL., Xu, Q. & Lin, CS. Methotrexate is associated with decreased total thyroxine in patients with rheumatoid arthritis. Inflammopharmacol 31, 2383–2392 (2023). https://doi.org/10.1007/s10787-023-01299-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01299-6