Abstract
Background
This study aimed to explore the correlation of circulating inflammatory cytokines’ levels with treatment response to etanercept (ETN) treatment in psoriasis patients.
Methods
97 moderate-to-severe plaque-psoriasis patients were continuously recruited in this prospective cohort study, and all patients received ETN treatment. Serum samples were collected before and at 6 months (M6) after treatment, and nine inflammatory cytokines expressions were detected by enzyme-linked immuno sorbent assay. Psoriasis Area and Severity Index (PASI) score was evaluated at baseline (M0), 1 month (M1), 3 months (M3) and M6 after treatment, and the corresponding PASI 75/90 responses’ rates were calculated.
Results
Tumor necrosis factor-alpha (TNF-α), interleukin (IL)-1β, IL-6, IL-12, IL-17A, IL-22, IL-23, and IL-32 levels were reduced, while IL-10 level was elevated at M6 after ETN treatment compared to baseline. PASI 75/90 responses’ rates to ETN were 69.1 and 38.1% at M6, respectively. IL-1β and IL-17A levels were elevated in PASI 75-response patients compared to PASI 75 non-response patients, while IL-17A level was also increased in PASI 90-response patients compared to PASI 90 non-response patients. Multivariate logistic regression revealed that IL-1β, IL-17A and combined phototherapy during study predicted higher, while previous systemic biologic treatment predicted lower PASI 75 response to ETN independently. In addition, IL-17A independently predicted higher PASI 90 response to ETN as well.
Conclusions
IL-1β, IL-17A, and combined phototherapy predicts higher while previous systemic biologic treatment predicts lower treatment response to ETN independently in psoriasis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriasis is a chronic autoimmune disease featured by inflammatory disorder of skin (but not restricted to the skin) with thickened, erythematous and scale-coated plaques, which affects around 2.5% population worldwide (Boehncke and Schon 2015). For disease management, various therapies have been applied including systemic biological agents, topical treatment and UV phototherapy (Prinz et al. 2016). As one of the first-line systemic biological agents, etanercept (ETN) has been adopted for the treatment of moderate-to-severe plaque psoriasis, which is characterized by low drug toxicity and flexible dosing, whereas poor treatment efficacy still exists in a number of patients (Drug Bank https://www.drugbank.ca/drugs/DB00005). Therefore, it is essential to discover potential biomarkers which could predict ETN treatment response to improve the prognosis in psoriasis patients.
Inflammatory cytokines are signaling molecules secreted by pro-inflammation cells such as T cells and macrophages, and their levels have been illustrated to be up-regulated in psoriasis (Boehncke and Schon 2015; Senra et al. 2016). According to previous studies, several inflammatory cytokines’ levels including tumor necrosis factor-alpha (TNF-α), interleukin (IL)-23, IL-22 as well as IL-17 are positively associated with disease severity in psoriasis patients and their biological blocking agents are effective on psoriasis treatment (Nakajima et al. 2011; Soderstrom et al. 2017; Wolk et al. 2006). Whereas for the role of inflammatory cytokines in psoriasis patients that underwent systemic biological blockers’ treatment, especially ETN, there is still a lack of information. Thus, this study aimed to explore the correlation of circulating inflammatory cytokines’ levels with treatment response to ETN treatment in psoriasis patients.
Materials and methods
Patients
This prospective cohort study consecutively recruited 97 moderate-to-severe plaque-psoriasis patients who underwent ETN treatment between 1 January 2013 and 31 June 2017 in The People’s Hospital of Shiyan. The inclusion criteria were: diagnosed as plaque psoriasis with moderate-to-severe disease activity, which was defined as psoriasis-affected body surface area (BSA) no less than 10% and Psoriasis Area and Severity Index (PASI) score no less than 8 points; age above 18 years; about to receive ETN treatment; likely to be followed up regularly for 6 months. Patients with the following conditions were excluded: complicated with other active skin diseases apart from psoriasis which interfered the assessment of psoriasis or complicated with moderate-to-severe hepatic, renal or heart dysfunction; received biologics treatment within 6 months or glucocorticoid treatment within 1 month; pregnant or lactating women; had contraindications to ETN treatment. The Ethics Committee of The People’s Hospital of Shiyan approved this study, and this study was executed in line with the Declaration of Helsinki, each patient provided written informed consent before inclusion.
Treatment and assessment
Psoriasis patients received 25 mg ETN twice per week by subcutaneous injection for 6 months, while for some patients who achieved PASI 75 response during the study, the dose was reduced to 25 mg once per week by subcutaneous injection. In addition, combinations were documented and categorized into topical therapy, phototherapy, and non-biologic therapy for analysis. PASI 75/90 responses were calculated at 1 month (M1), 3 months (M3) and 6 months (M6) as follows: PASI 75 response was defined as 75% or above reduction in PASI score from baseline to each visit, and PASI 90 response was defined as 90% or above reduction in PASI score from baseline to each visit.
Serum sample collection and enzyme-linked immuno sorbent assay (ELISA)
Peripheral blood was obtained from psoriasis patients before treatment (M0) and at M6 after treatment, followed by isolation of serum by centrifugation at 4000 Revolutions Per Minute (RPM) for 6 min. Serum TNF-α, IL-1β, IL-6, IL-10, IL-12, IL-17A, IL-22, IL-23, and IL-32 expressions were detected by ELISA using commercial ELISA kits (eBioscience, USA).
Statistics
Statistical analysis was performed by SPSS 19.0 Software (IBM, USA) and GraphPad Prism 6.01 Software (GraphPad, USA). Data were displayed as mean ± standard deviation, median (25th–75th quantiles) or count (with or without percentage). Comparison between two groups was analyzed by Wilcoxon rank sum test, the comparison between M0 (before treatment) and M6 (after treatment) was analyzed by Wilcoxon signed-rank sum test, factors affecting PASI 75/90 responses were analyzed by logistic regression analysis. p < 0.05 was considered significant.
Results
Study flow
In this study, 178 psoriasis patients were invited, while 49 patients were excluded (including 31 patients who missed the invitation and 18 patients who declined to attend the pre-screening procedure). 129 patients were subsequently screened for eligibility, whereas 32 patients were ineligible (including 22 patients who did not meet the inclusion criteria and 10 patients who declined to sign the informed consent). After that, 97 eligible patients were recruited in the present study and inflammatory cytokines were assayed at baseline. All patients received ETN treatment for 6 months, and PASI 75/90 responses were evaluated at M1, M3, and M6. During this period, 8 withdrawals occurred (including 5 patients who withdrew due to lost follow-up, 2 patients withdrew due to lack of efficiency and 1 patient withdrew due to an adverse event), and inflammatory cytokines were assayed at M6 or last visit. In this study, intention-to-treat (ITT) analysis was applied and a total of 97 recruited psoriasis patients were included in the final analysis. The detailed study flow is shown in Fig. 1.
Baseline characteristics of psoriasis patients
The mean age of 97 psoriasis patients was 47.1 ± 13.4 years, and there were 61 males and 36 females. The median disease duration, psoriasis-affected BSA and PASI score were 11.0 (4.0–16.0) years, 24.0 (19.5–31.5)%, and 13.4 (9.8–19.9)%, respectively. As to inflammatory cytokines, the median baseline serum levels of TNF-α, IL-1β, IL-6, IL-10, IL-12, IL-17A, IL-22, IL-23, and IL-32 were 37.98 (19.31–57.30) pg/ml, 5.48 (3.27–9.45) pg/ml, 29.89 (17.36–50.01) pg/ml, 23.08 (11.96–42.79) pg/ml, 76.07 (41.21–120.23) pg/ml, 64.17 (33.91–98.96) pg/ml, 55.49 (20.38–86.13) pg/ml, 60.59 (28.37–118.42) pg/ml and 37.94 (18.93–78.11) pg/ml, respectively. Other detailed baseline characteristics are listed in Table 1.
Change of inflammatory cytokines’ levels after ETN treatment
Compared to baseline, serum pro-inflammatory cytokines including TNF-α (Fig. 2a), IL-1β (Fig. 2b), IL-6 (Fig. 2c), IL-12 (Fig. 2e), IL-17A (Fig. 2f), IL-22 (Fig. 2g), IL-23 (Fig. 2h), and IL-32 (Fig. 2i) were decreased (All p < 0.001), while serum anti-inflammatory cytokine IL-10 (Fig. 2d) was elevated (p < 0.001) at M6 after ETN treatment.
Inflammatory cytokines levels before and after ETN treatment. At M6 after ETN treatment, TNF-α (a), IL-1β (b), IL-6 (c), IL-12 (e), IL-17A (f), IL-22 (g), IL-23 (h) and IL-32 (i) levels were decreased, while IL-10 (d) level was increased compared to baseline. Comparison of inflammatory cytokine levels before and after ETN treatment was performed using Wilcoxon signed-rank sum test. p < 0.05 was considered significant. ETN etanercept, TNF-α tumor necrosis factor-alpha, IL interleukin, M month
PASI 75/90 response rates by ETN treatment
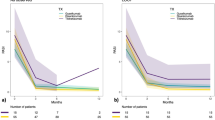
After ETN treatment, PASI 75 response rates were 9.3, 33.0, and 69.1% at M1, M3, and M6, respectively (Fig. 3a), and PASI 90 response rates were 0.0, 17.5, and 38.1% at M1, M3, and M6, respectively (Fig. 3b).
PASI 75 and PASI 90 response rates in psoriasis patients at each visit. PASI 75 response rates (a) at M1, M3 and M6 were 9.3, 33.0 and 69.1%, respectively. The PASI 90 response rates (b) were 0.0, 17.5 and 38.1% at M1, M3, and M6, respectively. PASI psoriasis area and severity index, ETN etanercept, M month
Comparison of inflammatory cytokines’ levels between PASI 75 response and non-response patients
Patients were divided into PASI 75 response cases (N = 67) and non PASI 75 response cases (N = 30) according to whether PASI 75 response was realized at M6, and we observed that serum IL-1β (p = 0.007) (Fig. 4b) and IL-17A (p = 0.002) (Fig. 4f) levels were increased in PASI 75 response patients compared to PASI 75 non-response patients. While no difference of serum TNF-α (p = 0.773) (Fig. 4a), IL-6 (p = 0.553) (Fig. 4c), IL-10 (p = 0.737) (Fig. 4d), IL-12 (p = 0.165) (Fig. 4e), IL-22 (p = 0.904) (Fig. 4g), IL-23 (p = 0.292) (Fig. 4h) or IL-32 (p = 0.685) (Fig. 4i) level between PASI 75 response patients and PASI 75 non-response patients was observed.
Comparing inflammatory cytokines levels in PASI 75 response and non-response groups at M6 after ETN treatment. IL-1β (b) and IL-17A (f) levels were elevated in PASI 75 response group compared to non-response group. There was no difference in the level of TNF-α (a), IL-6 (c), IL-10 (d), IL-12 (e), IL-22 (g), IL-23 (h) or IL-32 (i) between the two groups. Wilcoxon rank sum test was used to determine the difference in inflammatory cytokines levels between two groups. p < 0.05 was considered significant. PASI psoriasis area and severity index, TNF-α tumor necrosis factor-alpha, IL interleukin
Factors affecting PASI 75 (M6) response in psoriasis patients
Univariate logistic regression exhibited that IL-1β (OR = 1.186, p = 0.007), IL-17A (OR = 1.019, p = 0.004) and phototherapy during study (OR = 3.392, p = 0.011) were positively correlated with PASI 75 response, while previous systemic biologic treatment (OR = 0.154, p = 0.011) was negatively correlated with PASI 75 response at M6. All factors were subsequently included in multivariate logistic regression, which revealed that IL-1β (OR = 1.209, p = 0.032), IL-17A (OR = 1.023, p = 0.020) and combined phototherapy (OR = 7.328, p = 0.017) were independent predictive factors for higher PASI 75 response, while previous systemic biologic treatment (OR = 0.063, p = 0.031) independently predicted lower PASI 75 response to ETN treatment at M6 (Table 2).
Comparison of inflammatory cytokines levels in PASI 90 response and non-response patients
Patients were divided into PASI 90 response cases (N = 37) and non PASI 90 response cases (N = 67) according to whether PASI 90 response was realized at M6, and we discovered that only serum IL-17A level was increased (p = 0.038) (Fig. 5f) in PASI 90 response group compared to PASI 90 non-response group, while there was no difference of serum TNF-α (p = 0.959) (Fig. 5a), IL-1β (p = 0.533) (Fig. 5b), IL-6 (p = 0.705) (Fig. 5c), IL-10 (p = 0.721) (Fig. 5d), IL-12 (p = 0.316) (Fig. 5e), IL-22 (p = 0.270) (Fig. 5g), IL-23 (p = 0.572) (Fig. 5h) or IL-32 (p = 0.859) (Fig. 5i) levels between the two groups.
Comparing inflammatory cytokines levels in PASI 90 response and non-response groups at M6 after ETN treatment. IL-17A (f) level was increased in PASI 90 response group compared to non-response group. No difference in the level of TNF-α (a), IL-1β (b), IL-6 (c), IL-10 (d), IL-12 (e), IL-22 (g), IL-23 (h) or IL-32 (i) was observed between the two groups. Wilcoxon rank sum test was used to determine the difference in inflammatory cytokine levels between two groups. p < 0.05 was considered significant. PASI psoriasis area and severity index, IL interleukin, TNF-α tumor necrosis factor-alpha
Factors affecting PASI 90 (M6) response in psoriasis patients
Univariate logistic regression displayed that IL-17A (OR = 1.011, p = 0.029) was positively associated with PASI 90 response, and multivariate logistic regression further illustrated that IL-17A (OR = 1.018, p = 0.012) independently predicted higher PASI 90 response to ETN treatment at M6 (Table 3).
Discussion
This present study disclosed that in psoriasis patients who underwent ETN treatment: (1) Circulating pro-inflammatory cytokines levels were reduced while anti-inflammatory cytokine level was raised at M6 compared to baseline. (2) IL-1β, IL-17A and combined phototherapy independently predicted higher PASI 75 response, while previous systemic biologic treatment independently predicted lower PASI 75 response at M6; in addition, IL-17A was also an independent predictive factor for increased PASI 90 response.
Psoriasis is a chronic disease initiated by activation of various immune cells and aggravated by self-sustained inflammation cascade due to the secretion of inflammatory cytokines (e.g. IL-17A, TNF-α, IL-1β, IFN-α, IL-23 and IL-22) by activated T cells, natural killer cells, and local myeloid dendritic cells. Hence, drugs that target the inflammatory mediator pathways emerge as the main systemic treatment agents for psoriasis (Lockshin et al. 2018; Sobhan et al. 2016; Strober et al. 2008; Tan et al. 2007). ETN, acting as a TNF inhibitor, is a dimeric fusion protein produced by linking extracellular ligand-binding portion of TNF receptor to the Fc portion of human immunoglobulin 1, and its efficacy on psoriasis treatment has been identified based on several clinical studies (Kivelevitch et al. 2014; Tan et al. 2007; Tsai and Tsai 2017; Wasilewska et al. 2016). For instance, a previous study in Chinese psoriasis patients reveals that ETN treatment effectively reduces the infected body area and 40.98% patients achieved PASI 75 response at 12 weeks (Xie et al. 2017). In addition, both children and adolescent patients with plaque psoriasis have been reported to achieve 75, 57 and 27% PASI 50, 75 and 90 responses, respectively, by ETN treatment at 12 weeks, which are greatly increased compared with placebo (Di Lernia et al. 2018; Paller et al. 2008). Moreover, a systemic review including 12 randomized control trials reveals that ETN treatment obviously remits pruritus, pain and fatigue in moderate-to-severe plaque-psoriasis patients and improves long-term patients’ satisfaction compared with placebo (Carrascosa et al. 2018). In this present study, we observed that ETN produced a 69.1% PASI 75 response rate and 38.1% PASI 90 response rate at M6, which are numerically higher compared with previous studies, these might result from that (1) the treatment duration was higher in this study (6 months) compared with previous studies (mostly 3 months); (2) most of the patients received combined therapy such as topical therapy, phototherapy and systemic non-biologic treatment during ETN treatment in this study which increased the treatment response.
Several studies have identified that ETN regulates inflammatory cytokines levels in psoriasis. For example, a previous small-sample cohort study shows that TNF-α, IL-1β and IL-6 levels in umbilical fat tissue are all decreased after 24-week ETN treatment (Motolese et al. 2017). While another cohort study reveals that IL-17A, IL-19, IL-20, IL-22, IL-23p19 and IL-24 are all reduced at 4 weeks in psoriasis responding to ETN (Wang et al. 2012). In line with previous studies, our study observed that eight serum pro-inflammatory cytokines levels (TNF-α, IL-1β, IL-6, IL-12, IL-17A, IL-22, IL-23 and IL-32) were dramatically reduced while one serum anti-inflammatory cytokine level (IL-10) was greatly raised at M6 after ETN treatment compared to baseline. This might be explained by that: ETN blocked TNF-induced activation of inflammation, thus decreased secretion of pro-inflammatory cytokines while increased expression of anti-inflammatory cytokine.
For the correlation of inflammatory cytokines levels with ETN treatment response in chronic inflammatory diseases, several studies have been carried out (Shi et al. 2018; Takahashi et al. 2010). For example, baseline IL-6 level is illustrated to be positively correlated with treatment response, and the combination of IL-6 and survivin could distinguish responders from non-responders to ETN treatment with area under curve of 0.875 (95% CI 0.771–0.976) in patients with established rheumatoid arthritis (Shi et al. 2018). While only a few studies investigate the correlation of inflammation markers (including cytokines) levels with ETN treatment response in psoriasis patients. A previous cohort study presents that an increase in hs-CRP and ESR difference (from week 12 to 0) correlates with higher PASI 75 response (Kanelleas et al. 2011). Another cohort study illustrates that a decrease of IL-17A during 12-week ETN treatment associates with increased PASI 75 response in psoriasis patients (Fitz et al. 2018). However, no study has explored the predictive value of comprehensive inflammatory cytokines levels for treatment response to ETN in psoriasis patients until now. In the current study, we measured 9 serum inflammatory cytokines levels, and we found that IL-1β and IL-17A independently predicted higher PASI 75 response, and IL-17A independently predicted raised PASI 90 response as well at M6 in psoriasis patients after ETN treatment. These might be due to that: (1) As one of the main inflammatory gene products induced by the activation of TNF-α related inflammatory cascade, IL-1β was more effectively downregulated by ETN (the TNF inhibitor) treatment, which reduced the inflammation in skin, thereby leading to decreased PASI score and achievement of PASI 75/90 (Tan et al. 2007); (2) IL-17A might increase immune cells sensitivity to ETN antagonization, thereby improving the ETN treatment efficacy, decreasing inflammatory skin lesion, and leading to PASI 75/90 response in psoriasis patients.
In addition, we also observed that combined phototherapy independently predicted higher while previous systemic biologic treatment independently predicted lower PASI 75 response to ETN treatment in psoriasis patients, the possible explanations were as follows: (1) Phototherapy directly reduced target skin lesions thus its combination improved treatment response; (2) Previous systemic biologic treatment might increase concentration of antibodies to TNF-α antibody, and decreased sensitivity of TNF-α inhibitors, resulting in lower treatment response.
There were several limitations in this study, including: (1) the follow-up period was 6 months, thus, the correlation of inflammatory cytokines with long-term efficacy of ETN was not investigated; (2) the sample size was relatively small with 97 patients eligible for analysis, which might reduce the statistical power; (3) this study only enrolled ETN-treated psoriasis patients, while other TNF inhibitors (such as infliximab and adalimumab) treated psoriasis patients were not included, thus the predictive value of comprehensive inflammatory cytokines levels with treatment response to other TNF inhibitors was not explored.
In conclusion, IL-1β, IL-17A, combined phototherapy predicts higher while previous systemic biologic treatment predicts lower treatment response to ETN independently in psoriasis patients.
References
Boehncke WH, Schon MP (2015) Psoriasis. Lancet 386:983–994. https://doi.org/10.1016/S0140-6736(14)61909-7
Carrascosa JM, Rebollo F, Gomez S, De-la-Cueva P (2018) Effects of etanercept on the patient-perceived results (PROs) in patients with moderate-to-severe plaque psoriasis: systematic review of the literature and meta-analysis. J Dermatol Treat. https://doi.org/10.1080/09546634.2018.1467536
Di Lernia V et al (2018) Effectiveness of etanercept in children with plaque psoriasis in real practice: a one-year multicenter retrospective study. J Dermatol Treat 29:217–219. https://doi.org/10.1080/09546634.2017.1364692
Fitz L et al (2018) Association between serum interleukin-17A and clinical response to tofacitinib and etanercept in moderate to severe psoriasis. Clin Exp Dermatol. https://doi.org/10.1111/ced.13561
Kanelleas A et al (2011) The role of inflammatory markers in assessing disease severity and response to treatment in patients with psoriasis treated with etanercept. Clin Exp Dermatol 36:845–850. https://doi.org/10.1111/j.1365-2230.2011.04131.x
Kivelevitch D, Mansouri B, Menter A (2014) Long term efficacy and safety of etanercept in the treatment of psoriasis and psoriatic arthritis. Biologics 8:169–182. https://doi.org/10.2147/BTT.S41481
Lockshin B, Balagula Y, Merola JF (2018) Interleukin 17, inflammation, and cardiovascular risk in patients with psoriasis. J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2018.02.040
Motolese A, Chiaravalloti V, Cerati M, Oldrini R, Mola F, Passi A (2017) Interleukin levels and macrophagic density in periumbilical fat tissue in patients affected by moderate-to-severe psoriasis with metabolic syndrome, before and after etanercept treatment. G Ital Dermatol Venereol 152:342–347. https://doi.org/10.23736/S0392-0488.16.05235-4
Nakajima H, Nakajima K, Tarutani M, Morishige R, Sano S (2011) Kinetics of circulating Th17 cytokines and adipokines in psoriasis patients. Arch Dermatol Res 303:451–455. https://doi.org/10.1007/s00403-011-1159-3
Paller AS et al (2008) Etanercept treatment for children and adolescents with plaque psoriasis. N Engl J Med 358:241–251. https://doi.org/10.1056/NEJMoa066886
Prinz JC, Puig L, Girolomoni G (2016) Treatment of psoriasis with etanercept: the typical patient profile. J Eur Acad Dermatol Venereol JEADV 30:1092–1099. https://doi.org/10.1111/jdv.13662
Senra L, Stalder R, Alvarez Martinez D, Chizzolini C, Boehncke WH, Brembilla NC (2016) Keratinocyte-derived IL-17E contributes to inflammation in psoriasis. J Invest Dermatol 136:1970–1980. https://doi.org/10.1016/j.jid.2016.06.009
Shi R, Chen M, Litifu B (2018) Serum interleukin-6 and survivin levels predict clinical response to etanercept treatment in patients with established rheumatoid arthritis. Mod Rheumatol 28:126–132. https://doi.org/10.1080/14397595.2017.1317384
Sobhan MR, Farshchian M, Hoseinzadeh A, Ghasemibasir HR, Solgi G (2016) Serum levels of IL-10 and IL-22 cytokines in patients with psoriasis. Iran J Immunol 13(3):317–323
Soderstrom C, Berstein G, Zhang W, Valdez H, Fitz L, Kuhn M, Fraser S (2017) Ultra-sensitive measurement of IL-17A and IL-17F in psoriasis patient serum and skin. AAPS J 19:1218–1222. https://doi.org/10.1208/s12248-017-0094-4
Strober B, Teller C, Yamauchi P, Miller JL, Hooper M, Yang YC, Dann F (2008) Effects of etanercept on C-reactive protein levels in psoriasis and psoriatic arthritis. Br J Dermatol 159:322–330. https://doi.org/10.1111/j.1365-2133.2008.08628.x
Takahashi H, Tsuji H, Hashimoto Y, Ishida-Yamamoto A, Iizuka H (2010) Serum cytokines and growth factor levels in Japanese patients with psoriasis. Clin Exp Dermatol 35:645–649. https://doi.org/10.1111/j.1365-2230.2009.03704.x
Tan JK, Aphale A, Malaviya R, Sun Y, Gottlieb AB (2007) Mechanisms of action of etanercept in psoriasis. J Investig Dermatol Symp Proc 12:38–45. https://doi.org/10.1038/sj.jidsymp.5650037
Tsai YC, Tsai TF (2017) Anti-interleukin and interleukin therapies for psoriasis: current evidence and clinical usefulness. Ther Adv Musculoskelet Dis 9:277–294. https://doi.org/10.1177/1759720X17735756
Wang F et al (2012) Etanercept suppresses regenerative hyperplasia in psoriasis by acutely downregulating epidermal expression of interleukin (IL)-19, IL-20 and IL-24. Br J Dermatol 167:92–102. https://doi.org/10.1111/j.1365-2133.2012.10961.x
Wasilewska A, Winiarska M, Olszewska M, Rudnicka L (2016) Interleukin-17 inhibitors. A new era in treatment of psoriasis and other skin diseases. Postepy Dermatol Alergol 33:247–252. https://doi.org/10.5114/ada.2016.61599
Wolk K et al (2006) IL-22 regulates the expression of genes responsible for antimicrobial defense, cellular differentiation, and mobility in keratinocytes: a potential role in psoriasis. Eur J Immunol 36:1309–1323. https://doi.org/10.1002/eji.200535503
Xie F et al (2017) Safety and efficacy of etanercept monotherapy for moderate-to-severe plaque psoriasis: A prospective 12-week follow-up study. J Huazhong Univ Sci Technol Med Sci = Hua zhong ke ji da xue xue bao Yi xue Ying De wen ban = Huazhong keji daxue xuebao Yixue Yingdewen ban 37:943–947. https://doi.org/10.1007/s11596-017-1832-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, Y., Qin, G., Meng, Z. et al. IL-1β, IL-17A and combined phototherapy predicts higher while previous systemic biologic treatment predicts lower treatment response to etanercept in psoriasis patients. Inflammopharmacol 27, 57–66 (2019). https://doi.org/10.1007/s10787-018-0530-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-018-0530-9