Abstract
Interleukin 6 (IL-6), a multifunctional cytokine, has been implicated in the pathophysiology of type 2 diabetes (T2D). The elevated circulating level of IL-6 is an independent predictor of T2D and is considered to be involved in the development of inflammation, insulin resistance and β-cell dysfunction. On the other hand, an increasing number of evidence suggests that IL-6 has an anti-inflammatory role and improves glucose metabolism. The complex signal transduction mechanism of IL-6 may help explain the pleiotropic nature of the cytokine. IL-6 acts via two distinct signalling pathways called classic signalling and trans-signalling. While both signalling modes lead to activation of the same receptor subunit, their final biological effects are completely different. The aim of this review is to summarize our current knowledge about the role of IL-6 in the development of T2D. We will also discuss the importance of specific blockade of IL-6 trans-signalling rather than inhibiting both signalling pathways as a therapeutic strategy for the treatment of T2D and its associated macrovascular complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interleukin 6 (IL-6) is a cytokine which was originally identified as a B cell differentiation factor (Hirano et al. 1985). Numerous cell types including immune cells, endothelial cells, skeletal and smooth muscle cells, thyroid cells, fibroblasts, mesangial cells, keratinocytes, microglial cells, astrocytes, certain tumor cells and islet β-cells have been reported to produce IL-6 (Kamimura et al. 2003). In general, IL-6 is involved in inflammatory and immunological processes, hematopoiesis, liver and neuronal regeneration (Rothaug et al. 2016; Scheller et al. 2006). IL-6 synthesis and secretion are induced during inflammatory conditions such as upon stimulation of Toll-like receptor (TLR) by lipopolysaccharide or upon stimulation of cells by interleukin 1 (IL-1) or tumor necrosis factor (TNF). IL-6 influences various cell types and has both pro- and anti-inflammatory characteristics (Hunter and Jones 2015). Dysregulation of IL-6 signalling has been implicated in the pathogenesis of several autoimmune and inflammatory diseases including type 2 diabetes (T2D) (Kamimura et al. 2003). It has been suggested that IL-6 promotes insulin resistance and contributes to the development of T2D. However, due to its different actions in distinct tissues, the role of IL-6 in the development of insulin resistance has been a subject of debate (Pedersen and Febbraio 2007). Here, we provide an overview of IL-6 signalling mechanisms, its controversial role in the pathogenesis of T2D and the rationale for the use of specific inhibitors of IL-6 trans-signalling in treatment of T2D.
IL-6 signalling
On target cells, IL-6 first binds to IL-6 receptor subunit α (IL-6R). The IL-6/IL-6R complex then associates with transmembrane signal transducing IL-6 receptor subunit β (gp130), which in turn induces gp130 dimerization and initiation of IL-6 intracellular signalling. IL-6 signal transduction through gp130 leads to the activation of Janus kinase/signal transducer and activator of transcription (JAK/STAT), mitogen-activated protein kinase (MAPK) and phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K) pathways inside cells (Fig. 1) (Hunter and Jones 2015; Schaper and Rose-John 2015).
IL-6 signalling A fully competent IL-6 receptor complex consists of IL-6, IL-6R and gp130. Formation of the IL-6/IL-6R/gp130 complex induces autophosphorylation and activation of the gp130-associated JAKs. These activated JAKs phosphorylate five tyrosine residues within the cytoplasmic portion of gp130. Phosphorylation of the membrane-proximal tyrosine residue, leads to the recruitment of SHP2, which then stimulates the activation of MAPK and PI3K pathways. Phosphorylation of the other tyrosine residues, in turn, leads to recruitment, phosphorylation, and translocation of STATs to the nucleus. In the nucleus, STATs bind to the DNA and induce the expression of various genes including acute phase proteins and the SOCS3 protein genes. SOCS3 inhibits JAKs, and therefore acts as a negative regulator of the gp130-associated signalling pathways
To mediate its biological effects, IL-6 utilizes two pathways termed classic and trans-signalling (Fig. 2). In classic signalling, IL-6 first binds to the membrane-bound non-signalling IL-6R (mbIL-6R). The IL-6/IL-6R complex associates with gp130 subunit and forms a signal transducing competent structure (Hunter and Jones 2015; Schaper and Rose-John 2015). While almost all cells in the body express gp130, mbIL-6R is only found on monocytes, macrophages, neutrophils, some types of T cells, hepatocytes, some epithelial cells, as well as, α- and β-cells of pancreatic islets (Ellingsgaard et al. 2008; Rose-John 2012; Schaper and Rose-John 2015). Since the receptor subunit gp130 does not have any measurable affinity for IL-6 (Jostock et al. 2001), the majority of cells in the human body, which do not express IL-6R, are completely unresponsive to IL-6 (Fischer et al. 1997). Interestingly, IL-6R also exists in a soluble form (sIL-6R) comprising the extracellular portion of the receptor. In humans, sIL-6R is predominantly made by shedding of mbIL-6R, a process which is mediated by the metalloproteases ADAM10 and ADAM17 (Matthews et al. 2003). Furthermore, sIL-6R, to a lesser extent, can be generated by translation from an alternatively spliced IL-6R mRNA (Lust et al. 1992). SIL-6R can bind to IL-6, with an approximately similar affinity as mbIL-6R, to form an agonistic complex that signals through gp130 (Rose-John and Heinrich 1994). Even in the absence of mbIL-6R, the complex of IL-6 and sIL-6R can stimulate gp130 expressing cells and initiate the subsequent signalling (Taga et al. 1989). This process is called trans-signalling and due to the widespread expression of gp130 on almost every cell type, dramatically expands the spectrum of IL-6 target cells. While it is generally believed that IL-6 classic signalling is involved in the anti-inflammatory and regenerative activities of IL-6, IL-6 trans-signalling is considered to be responsible for the pro-inflammatory responses caused by this cytokine (Rose-John 2012; Schaper and Rose-John 2015).
Classic and trans-signalling of IL-6 In classic signalling, IL-6 binds to the membrane bound IL-6R. The IL-6/IL-6R complex associates with the signal transducing protein gp130, initiating intracellular signalling. In trans-signalling, a soluble form of IL-6R is proteolytically released by metalloprotease ADAM10/17 or by translation from an alternatively spliced IL-6R mRNA, and can bind IL-6 to form a complex that signals through gp130
Several soluble forms of gp130 (sgp130) are also present in the circulation. These soluble forms of gp130 are generated by translation from an alternatively spliced IL6ST mRNA. Sgp130 functions as a natural negative regulator of IL-6 trans-signalling (Narazaki et al. 1993). While sgp130 does not bind IL-6 or IL-6R alone, it interacts with the IL-6/sIL-6R complex and specifically blocks IL-6 trans-signalling, without affecting classical IL-6 signalling. High circulating levels of sgp130 in complex with IL-6 and sIL-6R are found in the serum of healthy individuals. It appears that sIL-6R and sgp130 constitute a physiological buffer for circulating IL-6, in order to prevent a systemic response to IL-6 trans-signalling. Once IL-6 is released into the circulation, it binds to sIL-6R. The IL-6/sIL-6R complex then associates with sgp130, which results in inhibition of systemic IL-6 trans-signalling. During some inflammatory conditions, however, plasma IL-6 levels exceed the levels of sgp130, thus IL-6 can act systemically via trans-signalling (Rose-John 2012).
IL-6 role in the pathogenesis of T2D
T2D is a metabolic disorder characterized by relative insulin deficiency, hyperglycemia, increased demand for insulin and β-cell dysfunction resulting in insufficient production of insulin (Stumvoll et al. 2005). Obesity, in particular excess visceral adiposity, could lead to the development of chronic low-grade inflammation (Van Greevenbroek et al. 2013). Increasing evidence indicates that a chronic low-grade inflammatory state is associated with the pathogenesis of T2D. This low-grade inflammation represents itself, among other things, by elevated circulating levels of inflammatory cytokines such as IL-6 (Van Greevenbroek et al. 2013). Systemic levels of IL-6 are elevated in T2D patients (Kado et al. 1999) and high concentrations of circulating IL-6 is considered to be an independent predictor of T2D (Spranger et al. 2003). There is also evidence indicating that certain polymorphisms in IL-6 gene have a significant association with the incidence of T2D (Illig et al. 2004). The role of IL-6 in the development of insulin resistance and T2D is not yet clear. Some studies point to the deteriorating effect of IL-6 on insulin action (Klover et al. 2003; Lagathu et al. 2003), while others suggest that IL-6 is probably required to maintain glucose homeostasis (Matthews et al. 2010; Wallenius et al. 2002).
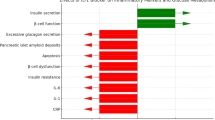
Insulin sensitive tissues and pancreatic islets
Given its well-known pro-inflammatory properties and following the observation that its systemic concentration is elevated in T2D patients, IL-6 was soon implicated in the development of T2D. In the past few years, several studies have provided clear evidence that IL-6, via its effect on insulin sensitive tissues and pancreatic islets, plays a significant role in the regulation of glucose metabolism. However, due to their controversial results, these studies failed to elucidate the exact role of IL-6 in the pathogenesis of T2D.
Adipose tissue
Insulin resistance in adipose tissue is an early and pivotal phenomenon in the development of T2D. Adipocytes and adipose tissue macrophages are the major sources of circulating IL-6 in T2D (Makki et al. 2013). It is of note that T2D patients have more visceral adipose tissue (VAT) than nondiabetics (Gallagher et al. 2009). VAT is characterized by high secretion of inflammatory cytokines such as IL-6 (Van Greevenbroek et al. 2013). These inflammatory cytokines may cause insulin resistance in adipose tissue and may be transported through the circulation, affecting more distant sites including the vessel walls, skeletal and cardiac muscle, kidneys and circulating leukocytes (Donath and Shoelson 2011). Research shows that short- and long-term treatment of adipocytes with IL-6 has different effects on insulin signalling (Table 1). Short-term treatment with IL-6 does not impair the effect of insulin in the adipose tissue of rats (Rotter Sopasakis et al. 2004) and enhances glucose uptake in 3T3-L1 adipocytes (Stouthard et al. 1996). In contrast, chronic treatment with IL-6 induces insulin resistance, suppresses glucose transport and reduces insulin-induced lipogenesis in 3T3-L1 adipocytes (Lagathu et al. 2003; Rotter et al. 2003). Additionally, IL-6 has been shown to interfere with insulin signalling (Rotter et al. 2003) and increase lipolysis (Trujillo et al. 2004) in adipocytes. Several mechanisms have been suggested to be involved in IL-6-induced disruption of insulin signalling in adipocytes. Notably, chronically elevated IL-6 can increase the expression of suppressor of cytokine signalling 3 (SOCS3) (Lagathu et al. 2003). In adipocytes, SOCS3 overexpression is thought to inhibit insulin signalling by reducing the insulin-stimulated phosphorylation of insulin receptor β (IR-β), insulin receptor substrate 1 (IRS-1), protein kinase B (PKB/Akt), extracellular-signal-regulated kinase 1 (ERK1) and extracellular-signal-regulated kinase 2 (ERK2) (Fig. 3) (Lagathu et al. 2003). Moreover, negative effect on the expression of adiponectin, GLUT4, IRS-1, peroxisome proliferator-activated receptor gamma (PPAR-γ) and IR-β are among other potential mechanisms linked with IL-6-induced impairment of insulin actions in fat cells (Fasshauer et al. 2003; Lagathu et al. 2003; Rotter et al. 2003). Furthermore, exposure to TNF-α enhances the transcription of IL-6 gene and thus contributes to the development of insulin resistance in adipocytes (Lagathu et al. 2003). In addition, IL-6 is responsible for macrophage recruitment to adipose tissue in obesity, which subsequently leads to the development of inflammation, insulin resistance and T2D (Fig. 3) (Kraakman et al. 2015).
Role of IL-6 in regulation of insulin signalling in adipocytes In adipocytes, elevated levels of IL-6 increase SOCS3 expression. SOCS3 negatively regulates insulin signalling by reducing the insulin-stimulated phosphorylation of IR-β, IRS-1, and PKB. Moreover, IL-6 impairs insulin action in adipocytes by decreasing the expression of insulin signalling components (IR-β, IRS-1, and GLUT4) and insulin-sensitizing factors (PPAR-γ and adiponectin). IL-6 can also induce macrophage recruitment to adipose tissue, which leads to the development of inflammation and subsequent disruption of insulin signalling
Liver
In hepatocytes, the ability of IL-6 to modulate insulin signalling has been investigated by a number of independent studies (Table 2). In vitro studies demonstrated that acute treatment of human hepatocarcinoma cells and mouse hepatocytes with IL-6 inhibits insulin-stimulated tyrosine phosphorylation of IRS-1 and thus leads to the impairment of insulin signalling (Senn et al. 2002). These findings were further supported by in vivo experiments in which both acute and chronic exposure to IL-6 caused insulin resistance in mouse hepatocytes by reducing tyrosine phosphorylation of IRS-1 and IRS-2 (Kim et al. 2004; Klover et al. 2003). In line with these studies, Cai et al. found that injection of IL-6-neutralizing antibodies improves hepatic insulin sensitivity in mice (Cai et al. 2005). It has been suggested that mammalian target of rapamycin (mTOR), via regulation of STAT3 activation, could play a key role in IL-6-induced hepatic insulin resistance. Upon stimulation with IL-6, mTOR enhances STAT3 activation, which results in SOCS3 overexpression and subsequent inhibition of insulin signalling in liver cells (Fig. 4) (Kim et al. 2008). In contrast to the aforementioned data which point to IL-6 as a negative regulator of insulin action in the liver, results from several studies using transgenic strategies suggest a beneficial role of IL-6 in hepatic insulin action. For example, studies of IL-6-deficient mice (IL-6−/−) showed that the absence of IL-6 leads to the development of inflammation and insulin resistance in the liver (Matthews et al. 2010). In addition, mice with hepatocyte-specific IL-6R deficiency displayed enhanced secretion of inflammatory cytokines by Kupffer cells, which led to the development of systemic inflammation and insulin resistance in the liver, skeletal muscle and white adipose tissue, suggesting that hepatic IL-6 signalling limits the expression of inflammatory cytokines in the liver and contributes to the improvement of both local and systemic insulin sensitivity (Wunderlich et al. 2010).
Role of IL-6 in regulation of hepatic insulin signalling In hepatocytes, mTOR upon IL-6 stimulation, enhances the activity of STAT and increases SOCS3 expression. SOCS3 negatively regulates insulin signalling which leads to the development of insulin resistance in the liver. Note that in cells such as hepatocytes, which express IL-6R, IL-6 could act via both classic and trans-signalling
Skeletal muscle
It is now well-known that exercise can significantly induce the production and release of IL-6 into the circulation by skeletal muscles (Steensberg et al. 2000). The acute elevation of plasma IL-6 is followed by increased plasma levels of anti-inflammatory interleukin 10 (IL-10) and interleukin-1 receptor antagonist (IL-1ra). IL-10 and IL-1ra are known to have inhibitory effects on the production of pro-inflammatory cytokines TNF-α and IL-1, respectively (Pedersen and Febbraio 2008). Therefore, it appears that exercise-induced release of IL-6 into the circulation, through promoting an anti-inflammatory environment, plays a protective role against systemic inflammation and leads to the improvement of global insulin sensitivity. Regarding the effects of IL-6 on skeletal muscles, IL-6 treatment has been shown to increase the translocation of GLUT4 to plasma membrane and promote insulin-stimulated glucose uptake in rat myotubes (Carey et al. 2006). As this effect of IL-6 was abolished in AMP-activated protein kinase (AMPK) dominant-negative-infected cells, IL-6 action on glucose metabolism of skeletal muscles was suggested to be mediated by AMPK (Carey et al. 2006). Moreover, both acute and chronic exposure to IL-6 resulted in increased glucose uptake in human skeletal muscle cells (Al-Khalili et al. 2006; Glund et al. 2007). Another study conducted by Weigert et al. showed that short-term exposure to IL-6, by inducing a rapid recruitment of IRS-1 to the IL-6 receptor complex and activation of IRS-1/Akt signalling, results in the improvement of insulin action in mouse skeletal muscle (Weigert et al. 2006). The same study reported that induction of SOCS3 expression by IL-6, which is thought to be an important mechanism for IL-6-mediated reduction of insulin action in both adipocytes and hepatocytes, does not occur in skeletal muscle cells (Weigert et al. 2006). In contrast to these findings, Kim et al. demonstrated that IL-6 infusion in mice inhibits insulin-stimulated IRS-1-associated PI3K activity, and therefore reduces insulin-stimulated glucose uptake in skeletal muscle (Kim et al. 2004). Moreover, chronically elevated levels of IL-6, by activation of c-Jun N-terminal kinase (JNK), accumulation of SOCS3 and protein tyrosine phosphatase1B (PTP1B) activity increase results in decreased insulin-stimulated glucose uptake in murine skeletal muscle cells (Table 3) (Fig. 5) (Nieto-Vazquez et al. 2008).
Dual role of IL-6 in regulation of insulin signalling and glucose metabolism in skeletal muscle In skeletal muscle, IL-6 enhances glucose uptake via stimulating the activity of AMPK and PI3K. IL-6 could also negatively affect insulin action in a JNK-dependent manner. Serine phosphorylation of IRS-1 by JNK impairs insulin signalling. Moreover, JNK increases PTP1B activity and SOCS3 expression. Tyrosine dephosphorylation of IRS-1 by PTP1B and impairment of tyrosine phosphorylation of IRS-1 by SOCS3 lead to decreased insulin-stimulated glucose uptake in skeletal muscle
Pancreatic islets
The progression from insulin resistance to T2D implicates a failure of pancreatic β-cells to compensate for the increased insulin demand. Under conditions of metabolic stress (elevated glucose and/or palmitate) and T2D, IL-6 levels are increased in human and mouse islets (Böni-Schnetzler et al. 2009; Ehses et al. 2007). This indicates that in addition to systemic increase of IL-6, local islet IL-6 levels are also elevated in T2D, suggesting a potential role of IL-6 in pancreatic islets under this condition. Long-term treatment of rodent islets with IL-6 impairs glucose-stimulated insulin secretion (Ellingsgaard et al. 2008). Moreover, IL-6 regulates the proliferation and apoptosis of pancreatic α- and β-cells. IL-6 induces the proliferation of both α- and β-cells. However, this cytokine exerts distinct effects on α- and β-cell apoptosis. In islet cells treated with high levels of glucose and palmitate, the presence of IL-6 protects α-cells from apoptosis, whereas β-cell apoptosis is exaggerated in the presence of IL-6 (Ellingsgaard et al. 2008). Furthermore, elevation of plasma IL-6 was recently found to stimulate pancreatic α-cells to secrete glucagon-like peptide-1 (GLP-1). GLP-1 is a hormone which induces insulin secretion by β-cells and thus results in improved glycemic parameters (Table 4) (Ellingsgaard et al. 2011). Interestingly, following high fat diet (HFD) feeding, IL-6 knockout mice are unable to expand their α-cell mass and show increased glycemia caused by impaired insulin secretion. These results suggest that systemically elevated levels of IL-6 in response to HFD, which leads to an α-cell expansion and subsequent increase in GLP-1 production, may be an adaptive response to maintain proper insulin secretion by β-cells (Fig. 6a) (Ellingsgaard et al. 2008, 2011). Overall, although the deleterious effect of elevated IL-6 on glucose homeostasis in pancreatic islets cannot be ignored, it appears that the role of IL-6 in the regulation of α-cells may compensate for the impaired β-cells function in T2D and contributes to limit hyperglycemia.
Metabolic effect of IL-6 on pancreatic islets and its role in the development of macrovascular complications a Elevated IL-6 concentrations stimulate GLP-1 secretion from pancreatic α-cells, improving insulin secretion and glycemia; a mechanism which may be involved in β-cell compensation for insulin resistance in T2D patients. b The effect of IL-6 on vascular smooth muscle cells and endothelial cells via trans-signalling leads to atherosclerosis and various macrovascular complications in diabetic patients
In summary, the above-mentioned data are suggestive of a tissue-specific and context-dependent effect of IL-6 on the regulation of glucose homeostasis. The final effect of IL-6 on insulin sensitive tissues seems to be dependent on several factors such as its concentration (high or low), kinetics (acute or chronic) and source. In addition, certain metabolic stressors (e.g. glucose and free fatty acids) and inflammatory mediators (e.g. cytokines and chemokines) can regulate IL-6 signalling and thus affect how IL-6 acts in different conditions. Furthermore, given the anti-inflammatory and insulin-sensitizing effects of IL-6, it is possible that elevated levels of IL-6 in T2D patients represent a compensatory mechanism in order to reduce inflammation and maintain proper glucose homeostasis. The latter view is further supported by studies using transgenic mice, which suggest that IL-6 is needed to counteract the increased inflammation and the absence of IL-6 could impair insulin signalling. Finally, as mentioned previously, the physiological responses to classic and trans-signalling of IL-6 are completely different from each other. Therefore, presence or lack of mbIL-6R on target cells, as well as, relative levels of sIL-6R and sgp130 could also influence the biological outcomes of exposure to IL-6.
Immune cells
Immune cells are considered as both sources and targets of IL-6 (Table 5). Studies have shown that interactions between IL-6 and the components of innate and adaptive immune systems play a major role in the development of low-grade chronic inflammation in T2D.
Innate immune cells
Macrophages are central mediators of inflammation in T2D. These cells are generally classified into two distinct subtypes: the classically activated macrophages termed M1, which mainly secrete pro-inflammatory cytokines including IL-6 and the alternatively activated macrophages termed M2, which produce anti-inflammatory cytokines (Chawla et al. 2011). In T2D, macrophage infiltration into insulin sensitive tissues and pancreatic islets, as well as, macrophage polarization toward the M1 phenotype in these tissues increase and contribute to the development of an inflammatory state (Esser et al. 2014). In addition to macrophages, the number of mast cells also increases in adipose tissue of obese humans and mice. These cells exacerbate insulin resistance and promote glucose intolerance by producing IL-6 and interferon-γ (Liu et al. 2009). Furthermore, neutrophils play an important part in the regulation of IL-6 signalling during inflammatory states. Neutrophils are among the first cells to accumulate at the sites of inflammation. These cells have a short life-span and die rapidly via apoptosis. In inflammatory conditions, apoptosis induces shedding of IL-6R from neutrophils. This process facilitates the formation of IL-6/sIL-6R complex and promotes IL-6 trans-signalling in smooth muscle cells, endothelial cells, mesothelial cells, epithelial cells and fibroblasts (Hunter and Jones 2015; Rose-John et al. 2017).
Adaptive immune cells
Cells of the adaptive immune system are also involved in adipose tissue inflammation and insulin resistance. Several studies have demonstrated a role for T cell subset imbalance in tissue inflammation. In general, it appears that the number of CD8+ T cells and CD4+ T helper 1 (TH1) cells increase in obese adipose tissue. The expansion of CD8+ T cells and TH1 cells stimulate the M1 polarization of macrophages. As discussed earlier, M1 macrophages secrete pro-inflammatory cytokines such as IL-6 and further contribute to the progression of inflammation and insulin resistance (Feuerer et al. 2009; Nishimura et al. 2009; Winer et al. 2009). In addition to pro-inflammatory T cells, the number of B cells also increases in visceral adipose tissue of obese mice (Winer et al. 2011). B cells from obese mice secrete high amounts of pro-inflammatory cytokines such as IL-6 (DeFuria et al. 2013). As a result, B cells enhance the activation and differentiation of adipose tissue pro-inflammatory T cells, which in turn leads to M1 macrophage polarization and insulin resistance. In addition, it is also possible that B cell-produced antibodies and cytokines directly affect insulin sensitivity in adipocytes (Winer et al. 2011).
Circulating leukocytes
While IL-6 mRNA expression is increased in peripheral blood mononuclear cells (PBMCs) of hypertensive T2D patients (Navarro-Gonzalez et al. 2010) and type 2 diabetic women (Tsiotra et al. 2008), induced hyperglycemia has been shown to decrease IL-6 gene transcription (Spindler et al. 2016). Moreover, a study conducted by Pickup et al. demonstrates that, despite the elevated levels of plasma IL-6, the production of this cytokine by blood cells of T2D patients is lower than nondiabetics (Pickup et al. 2000).
IL-6 signalling as a therapeutic target for treatment of T2D
Data from several studies suggest that IL-6 contributes to the onset and progression of chronic inflammation and autoimmunity (Tanaka et al. 2014). The pathological role of IL-6 is further supported by experiments whereby IL-6 blockade (using anti-IL-6 or anti-IL-6R antibodies, or IL-6−/− mice) demonstrated preventive and suppressive effects on the development of various immune-related disorders. Notably, the humanized anti-IL-6R antibody tocilizumab has been approved for the treatment of Rheumatoid Arthritis (RA) in more than 100 countries. Tocilizumab inhibits the binding of IL-6 to both mbIL-6R and sIL-6R and thereby results in complete blockade of IL-6 signalling (Tanaka et al. 2012, 2014). In addition to RA, tocilizumab and other anti-IL-6R antibodies have shown promising results in the treatment of several immune-related disorders (Tanaka et al. 2014; Waetzig and Rose-John 2012). For example, tocilizumab has been reported to improve insulin sensitivity and decrease glycated hemoglobin (HbA1c) levels in humans (Ogata et al. 2010; Schultz et al. 2010). Taken together, these findings support the idea that IL-6 signalling is a potential therapeutic target for the treatment of inflammatory-associated disorders including T2D.
However, as mentioned earlier, IL-6 is a truly multifunctional cytokine. Despite its role in the development of inflammation and insulin resistance, IL-6 is also involved in the improvement of insulin sensitivity, insulin secretion, glucose homeostasis and suppression of inflammatory processes in obesity and/or T2D. This pleiotropic behavior is closely related to whether IL-6 acts via its classic or trans-signalling mechanism. The effect of IL-6 on pancreatic islets, which in turn leads to increased insulin secretion by β-cells and improvement in glycemia is mediated through classic signalling (Ellingsgaard et al. 2008, 2011). Moreover, given the presence of mbIL-6R in hepatocytes, the beneficial effect of IL-6 on insulin sensitivity, glucose tolerance and inflammatory processes in the liver is most likely mediated by classic rather than trans-signalling of IL-6. On the other hand, IL-6 trans-signalling is involved in the infiltration of macrophages into expanding adipose tissue, resulting in the establishment of a chronic inflammatory state and insulin resistance in obese individuals (Kraakman et al. 2015). In addition, the lack of mbIL-6R on endothelial cells and vascular smooth muscle cells points to trans-signalling as the main mechanism involved in the deleterious effect of IL-6 on vasculature, which in turn could lead to atherosclerosis and various macrovascular complications in diabetics. IL-6 impairs the vasodilator effects of insulin in endothelial cells (Andreozzi et al. 2007). Additionally, IL-6, via trans-signalling, promotes the secretion of various chemokines and adhesion molecules in both endothelial and vascular smooth muscle cells, leading to the attraction of circulating leukocytes and consequent resolution of inflammatory reactions (Fig. 6b) (Klouche et al. 1999; Romano et al. 1997).
From these data it can be concluded that IL-6 trans-signalling through sIL-6R is mainly associated with pro-inflammatory and harmful actions of the cytokine in the pathogenesis of T2D. Conversely, classic signalling via mbIL-6R is mostly linked with anti-inflammatory and regenerative activities of IL-6 and probably has a beneficial effect on glucose metabolism. Tocilizumab and many other IL-6R antibodies block both classic and trans-signalling of IL-6. This global inhibition of IL-6 signalling pathways, disrupts both pro- and anti-inflammatory activities of the cytokine and may result in various physiological dysfunctions. Moreover, global IL-6 blockade has been associated with increased risk of bacterial infections, liver malfunction, elevation of cholesterol and weight gain (Tanaka et al. 2012; Waetzig and Rose-John 2012). These findings have led to the suggestion that specific inhibition of trans-signalling, as compared to the global inhibition of IL-6, may result in better therapeutic outcomes with fewer undesired side effects.
The sgp130Fc protein is a recombinant version of sgp130, which consists of the extracellular portion of gp130 fused to the Fc region of a human immunoglobulin G1 (IgG1) antibody. Sgp130Fc specifically blocks IL-6 trans-signalling, without affecting classical IL-6 signalling. Therefore, sgp130 inhibits the pro-inflammatory actions of IL-6, while leaving its anti-inflammatory and protective activities intact. Sgp130Fc has demonstrated robust efficacy in the treatment of many autoimmune and inflammatory diseases, with better side effect profile than global blockers of IL-6 signalling (Rose-John 2012; Waetzig and Rose-John 2012). Sgp130Fc selectively blocks the chemotactic signalling mediated by sIL-6R, therefore prevents HFD induced-macrophage infiltration into obese adipose tissue (Kraakman et al. 2015). In addition, treatment with sgp130Fc significantly reduces atherosclerosis, decreases expression of endothelial adhesion molecules and intimal smooth muscle cell infiltration, thus reduces monocyte recruitment and the subsequent progression of atherosclerotic plaques (Schuett et al. 2012). Moreover, none of the adverse effects of complete IL-6 blockade was demonstrated with sgp130Fc (Kraakman et al. 2015; Rose-John 2012; Schuett et al. 2012).
The above-mentioned data clearly highlight the therapeutic potential of selective inhibition of IL-6 trans-signalling for treatment of T2D and its vascular complications. Furthermore, given the specificity of sgp130Fc to inhibit trans-signalling, this protein can be used as a molecular tool to identify whether a certain effect of IL-6 (e.g. effect of IL-6 on glucose metabolism) is mediated via classic or trans-signalling (Rose-John 2012). This approach could be particularly useful to study the signalling pathways of IL-6 in mb-IL-6R expressing cells (e.g. hepatocytes and pancreatic islet cells), which can be stimulated by both the classic and trans-signalling pathways. Therefore, in addition to its therapeutic properties, the sgp130Fc protein allows us to discriminate between different IL-6 signalling pathways and thus advance our knowledge on the pathophysiological role of IL-6 signalling in the development of T2D.
Conclusion
Dysregulation of IL-6 production is associated with the pathogenesis of T2D. However, the effects of IL-6 on insulin sensitivity and glucose metabolism are markedly divergent in different tissues and contexts. This pleiotropic nature is at least in part dependent on the signalling pathway which is activated by IL-6. Increasing evidence from clinical and animal studies suggest that, in many inflammatory conditions, selective blockade of trans-signalling is therapeutically more effective and safer than global inhibition of IL-6, supporting the concept that pro-inflammatory and harmful activities of the cytokine are mainly mediated via trans-signalling. Of particular note, the sgp130Fc protein, which is a specific inhibitor of IL-6 trans-signalling, has been shown to completely prevent macrophage infiltration into obese adipose tissue and significantly reduce the extent of atherosclerosis. These results indicate that specific blockade of IL-6 trans-signalling with sgp130Fc could be considered as a potential therapeutic strategy for treatment of T2D and its macrovascular complications. In summary, although further investigations are needed to improve our knowledge about the complex molecular mechanisms of IL-6 signalling and its role in the development of T2D, inhibiting pro-inflammatory and deleterious effects of IL-6, without affecting its beneficial metabolic functions appears to be a tempting approach to deal with IL-6-associated disorders. Using sgp130Fc, which is the only available therapeutic agent for specific blockade of IL-6 trans-signalling, in combination with other anti-inflammatory treatments, such as anti-IL-1β agents, could lead to the development of more efficacious strategies for treatment of T2D.
References
Acosta-Rodriguez EV, Napolitani G, Lanzavecchia A, Sallusto F (2007) Interleukins 1β and 6 but not transforming growth factor-β are essential for the differentiation of interleukin 17–producing human T helper cells. Nat Immunol 8:942–949
Afford SC, Pongracz J, Stockley RA, Crocker J, Burnett D (1992) The induction by human interleukin-6 of apoptosis in the promonocytic cell line U937 and human neutrophils. J Biol Chem 267:21612–21616
Al-Khalili L, Bouzakri K, Glund S, Lönnqvist F, Koistinen HA, Krook A (2006) Signaling specificity of interleukin-6 action on glucose and lipid metabolism in skeletal muscle. Mol Endocrinol 20:3364–3375
Andreozzi F et al (2007) Interleukin-6 impairs the insulin signaling pathway, promoting production of nitric oxide in human umbilical vein endothelial cells. Mol Cell Biol 27:2372–2383
Biffl WL, Moore EE, Moore FA, Barnett CC (1995) Interleukin-6 suppression of neutrophil apoptosis is neutrophil concentration dependent. J Leukoc Biol 58:582–584
Böni-Schnetzler M et al (2009) Free fatty acids induce a proinflammatory response in islets via the abundantly expressed interleukin-1 receptor I. Endocrinology 150:5218–5229
Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J, Shoelson SE (2005) Local and systemic insulin resistance resulting from hepatic activation of IKK-β and NF-κB. Nat Med 11:183–190
Carey AL et al (2006) Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes 55:2688–2697
Chawla A, Nguyen KD, Goh YS (2011) Macrophage-mediated inflammation in metabolic disease. Nat Rev Immunol 11:738–749
Chomarat P, Banchereau J, Davoust J, Palucka AK (2000) IL-6 switches the differentiation of monocytes from dendritic cells to macrophages. Nat Immunol 1:510–514
DeFuria J et al (2013) B cells promote inflammation in obesity and type 2 diabetes through regulation of T-cell function and an inflammatory cytokine profile. Proc Natl Acad Sci 110:5133–5138
Donath MY, Shoelson SE (2011) Type 2 diabetes as an inflammatory disease. Nat Rev Immunol 11:98–107
Ehses JA et al (2007) Increased number of islet-associated macrophages in type 2 diabetes. Diabetes 56:2356–2370
Ellingsgaard H et al (2008) Interleukin-6 regulates pancreatic α-cell mass expansion. Proc Natl Acad Sci 105:13163–13168
Ellingsgaard H et al (2011) Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat Med 17:1481–1489
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N (2014) Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 105:141–150
Fasshauer M, Kralisch S, Klier M, Lossner U, Bluher M, Klein J, Paschke R (2003) Adiponectin gene expression and secretion is inhibited by interleukin-6 in 3T3-L1 adipocytes. Biochem Biophys Res Commun 301:1045–1050
Feuerer M et al (2009) Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters. Nat Med 15:930–939
Fielding CA et al (2014) Interleukin-6 signaling drives fibrosis in unresolved inflammation. Immunity 40:40–50
Fischer M et al (1997) A bioactive designer cytokine for human hematopoietic progenitor cell expansion. Nat Biotechnol 15:142–145
Gallagher D et al (2009) Adipose tissue distribution is different in type 2 diabetes. Am J Clin Nutr 89:807–814
Glund S et al (2007) Interleukin-6 directly increases glucose metabolism in resting human skeletal muscle. Diabetes 56:1630–1637
Hegde S, Pahne J, Smola-Hess S (2004) Novel immunosuppressive properties of interleukin-6 in dendritic cells: inhibition of NF-κB binding activity and CCR7 expression. FASEB J 18:1439–1441
Hirano T et al (1985) Purification to homogeneity and characterization of human B-cell differentiation factor (BCDF or BSFp-2). Proc Natl Acad Sci USA 82(16):5490–5494
Hunter CA, Jones SA (2015) IL-6 as a keystone cytokine in health and disease. Nat Immunol 16:448–457
Illig T et al (2004) Significant association of the interleukin-6 gene polymorphisms C-174G and A-598G with type 2 diabetes. J Clin Endocrinol Metab 89:5053–5058
Jostock T et al (2001) Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur J Biochem 268:160–167
Kado S, Nagase T, Nagata N (1999) Circulating levels of interleukin-6, its soluble receptor and interleukin-6/interleukin-6 receptor complexes in patients with type 2 diabetes mellitus. Acta Diabetol 36:67–72
Kamimura D, Ishihara K, Hirano T (2003) IL-6 signal transduction and its physiological roles: the signal orchestration model. Rev Physiol Biochem Pharmacol 149:1–38
Kim H-J et al (2004) Differential effects of interleukin-6 and -10 on skeletal muscle and liver insulin action in vivo. Diabetes 53:1060–1067
Kim J-H, Kim JE, Liu H-Y, Cao W, Chen J (2008) Regulation of interleukin-6-induced hepatic insulin resistance by mammalian target of rapamycin through the STAT3-SOCS3 pathway. J Biol Chem 283:708–715
Klouche M, Bhakdi S, Hemmes M, Rose-John S (1999) Novel path to activation of vascular smooth muscle cells: up-regulation of gp130 creates an autocrine activation loop by IL-6 and its soluble receptor. J Immunol 163:4583–4589
Klover PJ, Zimmers TA, Koniaris LG, Mooney RA (2003) Chronic exposure to interleukin-6 causes hepatic insulin resistance in mice. Diabetes 52:2784–2789
Kraakman MJ et al (2015) Blocking IL-6 trans-signaling prevents high-fat diet-induced adipose tissue macrophage recruitment but does not improve insulin resistance. Cell Metab 21:403–416
Lagathu C, Bastard J-P, Auclair M, Maachi M, Capeau J, Caron M (2003) Chronic interleukin-6 (IL-6) treatment increased IL-6 secretion and induced insulin resistance in adipocyte: prevention by rosiglitazone. Biochem Biophys Res Commun 311:372–379
Liu J et al (2009) Genetic deficiency and pharmacological stabilization of mast cells reduce diet-induced obesity and diabetes in mice. Nat Med 15:940–945
Lust JA, Donovan KA, Kline MP, Greipp PR, Kyle RA, Maihle NJ (1992) Isolation of an mRNA encoding a soluble form of the human interleukin-6 receptor. Cytokine 4:96–100
Makki K, Froguel P, Wolowczuk I (2013) Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflamm 2013:139239. https://doi.org/10.1155/2013/139239
Matthews V et al (2003) Cellular cholesterol depletion triggers shedding of the human interleukin-6 receptor by ADAM10 and ADAM17 (TACE). J Biol Chem 278:38829–38839
Matthews V et al (2010) Interleukin-6-deficient mice develop hepatic inflammation and systemic insulin resistance. Diabetologia 53:2431–2441
Mauer J et al (2014) Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol 15:423–430
Narazaki M et al (1993) Soluble forms of the interleukin-6 signal-transducing receptor component gp130 in human serum possessing a potential to inhibit signals through membrane-anchored gp130. Blood 82:1120–1126
Navarro-Gonzalez J, Mora-Fernandez C, Gomez-Chinchon M, Muros M, Herrera H, Garcia J (2010) Serum and gene expression profile of tumor necrosis factor-α and interleukin-6 in hypertensive diabetic patients: effect of amlodipine administration. Int J Immunopathol Pharmacol 23:51–59
Nieto-Vazquez I, Fernández-Veledo S, de Alvaro C, Lorenzo M (2008) Dual role of interleukin-6 in regulating insulin sensitivity in murine skeletal muscle. Diabetes 57:3211–3221
Nishimura S et al (2009) CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat Med 15:914–920
Ogata A et al (2010) Improvement of HbA1c during treatment with humanised anti-interleukin 6 receptor antibody, tocilizumab. Ann Rheum Dis 70(6):1164–1165
Pedersen BK, Febbraio MA (2007) Interleukin-6 does/does not have a beneficial role in insulin sensitivity and glucose homeostasis. J Appl Physiol 102:814–816
Pedersen BK, Febbraio MA (2008) Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev 88(4):1379–1406
Pickup JC, Chusney GD, Thomas SM, Burt D (2000) Plasma interleukin-6, tumour necrosis factor α and blood cytokine production in type 2 diabetes. Life Sci 67:291–300
Romano M et al (1997) Role of IL-6 and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity 6:315–325
Rose-John S (2012) IL-6 trans-signaling via the soluble IL-6 receptor: importance for the pro-inflammatory activities of IL-6. Int J Biol Sci 8(9):1237–1247
Rose-John S, Heinrich PC (1994) Soluble receptors for cytokines and growth factors: generation and biological function. Biochem J 300:281–290
Rose-John S, Winthrop K, Calabrese L (2017) The role of IL-6 in host defence against infections: immunobiology and clinical implications. Nat Rev Rheumatol 13(7):399–409
Rothaug M, Becker-Pauly C, Rose-John S (2016) The role of interleukin-6 signaling in nervous tissue. Biochim Biophys Acta 1863:1218–1227
Rotter Sopasakis V, Larsson B-M, Johansson A, Holmäng A, Smith U (2004) Short-term infusion of interleukin-6 does not induce insulin resistance in vivo or impair insulin signalling in rats. Diabetologia 47:1879–1887
Rotter V, Nagaev I, Smith U (2003) Interleukin-6 (IL-6) induces insulin resistance in 3T3-L1 adipocytes and is, like IL-8 and tumor necrosis factor-α, overexpressed in human fat cells from insulin-resistant subjects. J Biol Chem 278:45777–45784
Schaper F, Rose-John S (2015) Interleukin-6: biology, signaling and strategies of blockade. Cytokine Growth Factor Rev 26:475–487
Scheller J, Grotzinger J, Rose-John S (2006) Updating interleukin-6 classic-and trans-signaling. Signal Transduct 6:240–259
Schuett H et al (2012) Transsignaling of interleukin-6 crucially contributes to atherosclerosis in mice. Arterioscler Thromb Vasc Biol 32:281–290
Schultz O, Oberhauser F, Saech J, Rubbert-Roth A, Hahn M, Krone W, Laudes M (2010) Effects of inhibition of interleukin-6 signalling on insulin sensitivity and lipoprotein (a) levels in human subjects with rheumatoid diseases. PLoS ONE 5:e14328
Senn JJ, Klover PJ, Nowak IA, Mooney RA (2002) Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes 51:3391–3399
Spindler MP et al (2016) Acute hyperglycemia impairs IL-6 expression in humans. Immun Inflamm Dis 4:91–97
Spranger J et al (2003) Inflammatory cytokines and the risk to develop type 2 diabetes. Diabetes 52:812–817
Steensberg A, Hall G, Osada T, Sacchetti M, Saltin B, Pedersen BK (2000) Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6. J Physiol 529:237–242
Stouthard J, Elferink RO, Sauerwein H (1996) Interleukin-6 enhances glucose transport in 3T3-L1 adipocytes. Biochem Biophys Res Commun 220:241–245
Stumvoll M, Goldstein BJ, van Haeften TW (2005) Type 2 diabetes: principles of pathogenesis and therapy. Lancet 365:1333–1346
Taga T et al (1989) Interleukin-6 triggers the association of its receptor with a possible signal transducer, gp130. Cell 58:573–581
Takai Y, Wong G, Clark S, Burakoff S, Herrmann S (1988) B cell stimulatory factor-2 is involved in the differentiation of cytotoxic T lymphocytes. J Immunol 140:508–512
Tanaka T, Narazaki M, Kishimoto T (2012) Therapeutic targeting of the interleukin-6 receptor. Annu Rev Pharmacol Toxicol 52:199–219
Tanaka T, Narazaki M, Ogata A, Kishimoto T (2014) A new era for the treatment of inflammatory autoimmune diseases by interleukin-6 blockade strategy. Semin Immunol 26(1):88–96
Trujillo ME, Sullivan S, Harten I, Schneider SH, Greenberg AS, Fried SK (2004) Interleukin-6 regulates human adipose tissue lipid metabolism and leptin production in vitro. J Clin Endocrinol Metab 89:5577–5582
Tsiotra PC et al (2008) Peripheral mononuclear cell resistin mRNA expression is increased in type 2 diabetic women. Mediat Inflamm 2008:892864
Van Greevenbroek M, Schalkwijk C, Stehouwer C (2013) Obesity-associated low-grade inflammation in type 2 diabetes mellitus: causes and consequences. Neth J Med 71:174–187
Waetzig GH, Rose-John S (2012) Hitting a complex target: an update on interleukin-6 trans-signalling. Expert Opin Ther Targets 16:225–236
Wallenius V et al (2002) Interleukin-6-deficient mice develop mature-onset obesity. Nat Med 8:75–79
Weigert C et al (2006) Direct cross-talk of interleukin-6 and insulin signal transduction via insulin receptor substrate-1 in skeletal muscle cells. J Biol Chem 281:7060–7067
Winer S et al (2009) Normalization of obesity-associated insulin resistance through immunotherapy. Nat Med 15:921–929
Winer DA et al (2011) B cells promote insulin resistance through modulation of T cells and production of pathogenic IgG antibodies. Nat Med 17:610–617
Wright HL, Cross AL, Edwards SW, Moots RJ (2014) Effects of IL-6 and IL-6 blockade on neutrophil function in vitro and in vivo. Rheumatology 53:1321–1331
Wunderlich FT et al (2010) Interleukin-6 signaling in liver-parenchymal cells suppresses hepatic inflammation and improves systemic insulin action. Cell Metab 12:237–249
Acknowledgements
This work was supported by the Iran National Science Foundation with the Award Number 94000647.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbari, M., Hassan-Zadeh, V. IL-6 signalling pathways and the development of type 2 diabetes. Inflammopharmacol 26, 685–698 (2018). https://doi.org/10.1007/s10787-018-0458-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-018-0458-0