Abstract
Background
Curcuma longa has been well documented for managing joint inflammation and pain. The present study investigated the effect of polar extract of C. longa (NR-INF-02) on cartilage homeostasis in human articular chondrocytes knee (NHAC-kn) cells to understand its plausible mechanism of action.
Methods
Dysregulation of cartilage homeostasis was induced by IL-1β and H2O2. Modulating effects of NR-INF-02 on degradation markers viz., chondrocyte apoptosis, senescence, cytokine, eicosanoids, and cartilage synthesis markers viz., glycosaminoglycans and type II collagen degradation was evaluated in human articular chondrocytes knee (NHAC-kn) cells. Further, the effect of NR-INF-02 on lipopolysaccharide (LPS)-induced expression of NF-kB in RAW264.7 macrophages was investigated.
Results
NR-INF-02 significantly attenuated IL-1β-induced chondrocyte cytotoxicity, apoptosis and release of chondrocyte degradation markers such as IL-6, IL-8, COX-2, PGE2, TNF-α, ICAM-1 in NHAC-kn cells. Also, NR-INF-02 protected IL-1β-induced damage to synthesis markers such as glycosaminoglycans, type II collagen and further attenuated H2O2-induced chondrocyte senescence. In addition NR-INF-02 suppressed LPS-induced NF-kB expression in RAW264.7 cells.
Conclusions
NR-INF-02 protects cartilage homeostasis by maintaining the balance between synthesis and degradation of cartilage matrix.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is a major contributor of physical disability and morbidity in millions of individuals across the world. It is a progressive degenerative condition associated with structural and compositional changes in the articular cartilage. Articular cartilage consists of extra-cellular matrix (ECM) and highly specialized cells chondrocytes. Under normal condition, articular chondrocytes, the sole cellular component of the joint maintains dynamic equilibrium between synthesis (anabolism) and degradation (catabolism) of ECM components (Nakata et al. 1993; Sandell and Aigner 2001; Sophia et al. 2009). However, in OA states, a disruption of ECM equilibrium leads to progressive loss of cartilage tissue, clonal expansion of chondrocytes in the depleted regions, induction of oxidative states and apoptosis of cells (Lane et al. 2011; Bauer et al. 2006). With progression, there is usually an overall shift toward catabolism over anabolism. The principal catabolic mediators that contribute to degradative and nociceptive pathways in OA include pro-inflammatory members from cytokine family viz., IL-1β, IL-17, IL-6, IL-8, IL-18, TNF-α (Sokolove and Lepus 2013), inflammatory mediators like PGE2, COX-2, NO (Wojdasiewicz et al. 2014). These pro-inflammatory and inflammatory mediators in turn cause ROS production. In addition, chondrocyte ageing is characterised by a progressive loss of function integrity resulting in cellular alteration and cell death. The pro-inflammatory, inflammatory mediators, ROS and ageing, contribute to chondrocyte death which result in the failure to maintain structure of articular cartilage led to OA pain, functional disability and reduced quality of life (Hwang and Kim 2015). Hence, therapy aimed at maintaining ECM balance will address the unmet need for preventing OA progression.
In view of the unmet need for preventing OA progression and penchant towards herbal medicines globally (Beg et al. 2011), NR-INF-02 or Turmacin™ was developed and standardized to contain turmerosaccharides (> 10% w/w) with negligible amount of curcuminoids from Curcuma longa (C. longa) (Chandrasekaran et al. 2013). NR-INF-02 has been proven to alleviate joint pain in OA patients. In a randomized, single blind, placebo-controlled trial, NR-INF-02 administered at 1 g/day to patients with primary painful knee OA for 42 days significantly (p < 0.05) decreased VAS, WOMAC and CGIC scores compared to placebo. Further, NR-INF-02 treated group showed a significant (p < 0.01) decrease in use of rescue medication, along with clinical signs improvement compared to placebo (Madhu et al. 2013). In addition, oral administration of turmerosaccharide fraction of NR-INF-02 significantly decreased the OA pain at 1-, 3-, 6-, and 24-h intervals in monosodium iodoacetate (MIA)-induced OA pain model in rats (Bharathi et al. 2017). Further, anti-inflammatory effects were demonstrated in in vitro and in vivo studies. NR-INF-02 exhibited anti-inflammatory activity in both acute (carrageenan and xylene) and chronic (cotton pellet granuloma) animal models of inflammation (Anandakumar et al. 2014). In vitro studies on NR-INF-02 revealed anti-inflammatory activity by inhibiting prostaglandins and interleukins and thus re-enforced the in vivo findings (Chandrasekaran et al. 2013).
The present study was planned to explore the effects of NR-INF-02 on biomarkers for cartilage homeostasis in the joint and to acquire insights on the possible mechanisms of action. Specifically, the effect of NR-INF-02 on IL-1β-induced chondrocyte death, apoptosis, catabolic factors (IL-6, IL-8, TNF-α and PGE2, ICAM-1, COX-2) in human articular chondrocytes and expression of NF-kB in RAW264.7 cells was investigated. Further protective effect of NRINF-02 on IL-1β-induced glycosaminoglycan and collagen degradation; H2O2-induced chondrocyte senescence was also studied.
Materials and methods
Plant material and preparation of NR-INF-02
The rhizomes of C. longa Linn. were collected from different parts of Tamil Nadu State, India and authenticated at National Institute of Science Communication and Information Resources. A voucher specimen (No. 653) was deposited in our herbarium. Preparation of NR-INF-02 and characterization of polysaccharides has been described in our earlier report. In brief, coarsely powdered C. longa rhizomes were subjected to steam distillation to remove the turmeric oil and further extracted by refluxing with water. The extract was then concentrated and spray dried to obtain a free coarse powder. NR-INF-02 was prepared by blending the spray dried water extract and the turmeric oil at a ratio of 99:1 (w/w) followed by sieving. As reported previously, the extract is found to contain polysaccharide determined by HPLC (> 10% w/w) with negligible amount of curcuminoids (Chandrasekaran et al. 2013). NR-INF-02 was developed and registered as Turmacin™ by Natural Remedies Pvt. Ltd, Bangalore, India.
Cell cultures
Human primary knee articular chondrocytes [NHAC-kn (CC-2550)] were purchased from Lonza (Basel, Switzerland). Chondrocytes were cultured and re-differentiated to express their marker profile according to the manufacturer’s protocol.
Human articular chondrocyte derived from the knee (NHAC-kn) were maintained in a special chondrocyte basal medium mixed with 5% fetal bovine serum, growth factors and supplements (0.2% R3-IGF-1, 0.5% bFGF, 0.1% transferrin, 0.2% insulin, 0.1% GA-1000). The cells were grown in a monolayer culture and the growth medium was changed every 2–3 days. Cells of passage number less than 5 were used throughout the study.
RAW264.7 macrophages obtained from American Type Culture Collection were cultured in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% FBS at 37 °C, 5% CO2.
Materials
MTT, LPS, H2O2 (Sigma-Aldrich, Inc, USA), IL-1β, > 98% (BioVision, USA), DMEM (Gibco Life Technologies, USA), Chondrocyte growth medium (Lonza, Switzerland) were procured and utilized for the in vitro experiments.
Chondrocyte viability assay
Cell viability was quantified by MTT uptake method. Briefly 104 NHAC-kn chondrocytes per well were cultured for 16 h in a 48-well plate and then treated with NR-INF-02 (31.25–500 µg/mL) or NR-INF-02 and IL-1β for 3, 6 and 9 days at 37 °C. Cell supernatant was removed and 100 μL fresh medium and 10 μL MTT solution (5 mg/mL) were added to each well and incubated for 4 h at 37 °C, 5% CO2. Subsequent to the removal of supernatant, 200 μL of DMSO was added to dissolve the formazan crystals (Terry et al. 2007). Cell viability was calculated by reading the absorbance of each well at 570 nm (Molecular Devices, USA).
Detection of apoptosis
NHAC-kn cells were seeded in 96-well plates at a density of 2 × 104 cells/well. At 24 h of plating, cell supernatant was removed from each well and replenished with fresh medium containing NR-INF-02 concentrations ranging from 31.25 to 500 µg/mL with IL-1β (10 ng/mL) and incubated at 37 °C for 48 h. Following 48 h of treatment (Cheng et al. 2013), apoptosis was measured using the Cell Death Detection ELISA kit (Roche Diagnostics GmbH, Germany) that quantified histone-associated DNA fragments (mono and oligonucleosomes). The procedure was performed according to the manufacturer’s protocol. Briefly, cell lysates were prepared and incubated in the microtiter plate coated with anti-histone antibody. Subsequent to substrate addition, color development was measured spectrophotometrically using microplate reader at 405 nm.
Assays for cytokine, PGE2 and COX-2
NHAC-kn cells were cultured in 48-well plates at a density of 5 × 105 cells/mL. At 24 h of plating, cell supernatant was removed from each well and replenished with fresh medium containing NR-INF-02 concentrations ranging from 31.25 to 500 µg/mL with IL-1β (10 ng/mL) and incubated for 48 h (Pulai et al. 2005; Haseeb et al. 2013). Following incubation for 48 h, the cell supernatant was collected for estimation of TNF-α, IL-6, IL-8, PGE2 and cell lysate for determination of COX-2 levels. The quantification of TNF-α, IL-6, IL-8, PGE2 and COX-2 was be performed by ELISA according to the manufacturer’s guidelines (Cloud-Clone Corp, USA).
Assay for NF-κB expression in LPS-induced RAW264.7 cells
Murine monocytic macrophages cell line (RAW264.7) were adjusted to be 105 cells/mL in DMEM supplemented with 10% FBS. 200 μL of the cell suspension was plated into 96-well culture plate and incubated at 37 °C, 5% CO2 for 16 h. Following incubation the cells were rinsed three times with phosphate buffered saline (PBS). The cells were treated with NR-INF-02 (31.25–500 µg/mL) for 1 h and then incubated with LPS (1 µg/mL) for 24 h (Wu et al. 2015). NF-kB expression was measured using NF-kB p65 Cell based ELISA kit (R&D systems, Minneapolis, USA). Briefly after LPS treatment, the cells were rinsed multiple times and subsequently incubated with primary antibody mixture against NF-kB for 16 h at 4 °C. The cells were incubated with horseradish peroxidase-conjugated secondary antibody for 2 h at room temperature. Further, NF-kB expression was quantified by the addition of substrate and the fluorescence measured at 540 nm excitation, 600 nm emission and then at 360 nm excitation and 450 nm emission using a fluorescence plate reader (FLUOstar Optima, BMG Labtech, Germany).
Assay for ICAM—1 expression
NHAC-kn cells were seeded at a density of 2 × 104 cells/well in 96-well plates. At 24 h of plating, cell supernatant was removed and replenished with fresh medium containing NR-INF-02 concentrations ranging from 31.25 to 500 µg/mL with IL-1β (10 ng/mL) and further incubated at 37 °C for 24 h (Kienzle and Kempis 1998). Post incubation, the ICAM-1 expression was measured using colorimetric cell based ELISA kit (Assay Biotech, CA, USA). Post incubation, the cells were rinsed and subsequently incubated with primary antibody against ICAM-1 for 16 h at 4 °C. Further, cells were incubated with horseradish peroxidase-conjugated secondary antibody for 1.5 h at room temperature. The cell surface protein expression of ICAM-1 was quantified by the addition of substrate followed by reading the absorbance at 450 nm using a microplate reader (Molecular Devices, USA).
Glycosaminoglycan assay
NHAC-kn cells were adjusted to be 2 ×105 cells/mL in Chondrocyte Basal Medium (CBM) supplemented with R3-IGF-1 0.2%, bFGF 0.5%, transferrin 0.5%, insulin 0.2%, FBS 5%, GA-1000 0.1%. 500 μL of the cell suspension was plated into each well of 48-well culture plate and incubated for 24 h at 37 °C, 5% CO2. At 24 h of plating, cell supernatant was removed from each well and replenished with fresh medium containing NR-INF-02 concentraions ranging from 31.25 to 500 µg/mL. The cells were treated with NR-INF-02 for 1 h and then incubated with IL-1β (10 ng/mL) for 72 h. Post treatment period, the cell supernatant was discarded and intra-cellular glycosaminoglycan content was determined. In brief, cells attached to the culture plate were rinsed twice with PBS and then intra-cellular glycosaminoglycan was digested using papain extraction reagent (Choi et al. 2014). Cell lysate was sonicated and centrifuged at 10,000g for 10 min, About 100 μL of supernatant was mixed with 1 mL of Blyscan dye reagent and incubated in a shaker for 30 min and subsequently 0.5 mL of dissociation reagent was added. The glycosaminoglycan content was determined by DNB (dimethyl methylene blue) dye binding method using assay kit as per manufacturer’s guidelines (Biocolor; Blyscan, Sulfated Glycosaminoglycan assay kit, UK).
Type II collagen assay
NHAC-kn cells were adjusted to be 5 × 105 cells/mL in Chondrocyte Growth Medium (CGM). 500 μL of the cell suspension per well was plated into 48-well culture plate and incubated for 24 h at 37 °C, 5% CO2. Post incubation, cell supernatant was removed from each well and replenished with fresh medium (500 µL CGM) containing NR-INF-02 concentrations ranging from 31.25 to 500 µg/mL with IL-1β (10 ng/mL) for 72 h (Liu et al. 2015). Post incubation, the cell lysate was estimated for type II collagen using collagen detection kit (Chondrex, Inc, WA, USA). In brief, cells attached to the culture plate were rinsed twice with PBS and then intra-cellular collagen was digested using pepsin (Choi et al. 2014). Cell lysate was sonicated and centrifuged at 10,000g for 3 min. Cell supernatant was added to pre-coated ELISA plates and incubated for 2 h at room temperature. Plates were rinsed thrice and incubated with detection antibody. Type II collagen content was quantified by addition of O-phenylenediamine dihydrochloride and reading the absorbance at 490 nm.
Detection of cell senescence
NHAC-kn cells were adjusted to be 2 × 105 cells/mL in CGM. 500 μL of the cell suspension per well was plated into 24-well culture plate and incubated for 24 h at 37 °C, 5% CO2. Post incubation, the adherent cells were rinsed and stressed with H2O2 (100 µM) for 2 h. The cell supernatant was removed and replenished with fresh growth medium containing NR-INF-02 concentrations ranging from 31.25 to 500 µg/mL and further incubated for 24 h (Dai et al. 2006). Post incubation, the cell lysates were estimated for senescence-associated β-galactosidase (SA-β-gal) activity using cellular senescence assay kit (Cell Biolabs, Inc.CA, USA). Briefly, 50 µL of cell lysate was transferred into 96-well plate and incubated with 2X reaction buffer for 2 h. After 2 h, 50 µL of reaction mixture was transferred into new 96 well plate and 200 µL of stop solution was added. SA-β-gal activity was measured by reading the fluorescence of each well at 360 nm (Excitation)/465 nm (Emission).
Statistical analysis
The results were expressed as mean ± standard error of the mean. Statistical analysis was performed using one-way analysis of variance, followed by post hoc Dunnett’s test (GraphPad Prism 5.1). Values are presented as mean ± standard error. p value < 0.05 was considered as statistically significant.
Results
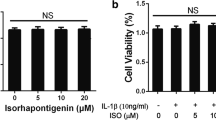
Effect of NR-INF-02 on chondrocyte viability
NR-INF-02 at concentrations ranging from 31.25 to 500 µg/mL for 3, 6 and 9 days neither increased nor decreased the viability of chondrocytes (Fig. 1).
The effects of NR-INF-02 (31.25–500 µg/mL) on chondrocyte viability in the presence of IL-1β were also examined. IL-1β at 10 ng/mL significantly reduced chondrocytes viability when compared to cell control. Treatment with NR-INF-02 at 125, 250 and 500 µg/mL significantly protected articular chondrocytes from IL-1β-induced cell death (Fig. 2).
Effect of NR-INF-02 on cell viability in IL-1β-stimulated NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently IL-1β (10 ng/mL) was added and incubated for 72 h. Cells viability was measured by MTT assay. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control
Effect of NR-INF-02 on IL-1β-stimulated apoptosis in NHAC-kn cells
IL-1β (10 ng/mL) treatment caused significant increase of apoptotic NHAC-kn cells in comparison to control. NR-INF-02 at concentration ranging from 62.5 to 500 µg/mL significantly protected chondrocytes from IL-1β-induced apoptosis in a concentration dependent manner (Fig. 3).
Effect of NR-INF-02 on IL-1β-induced apoptosis in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently IL-1β (10 ng/mL) was added and incubated for 48 h. NHAC-kn cells were lysed and apoptosis was measured. Values are presented as mean ± standard error of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control
Effect of NR-INF-02 on cytokines and eicosanoid release in IL-1β-stimulated NHAC-kn cells
The effects of NR-INF-02 (31.25–500 µg/mL) on IL-1β-induced cytokine and eicosanoid release in NHAC-kn were examined. IL-1β at 10 ng/mL induced significant increase of IL-6, IL-8, COX-2, PGE2 and TNF-α from NHAC-kn cells in comparison to control. Treatment to NHAC-kn cells with NR-INF-02 concentration range of 31.25–500 µg/mL significantly attenuated IL-6 and IL-8 release induced by IL-1β in a concentration-dependent manner (Fig. 4a). Similarly, NR-INF-02 treatment at 125, 250 and 500 µg/mL significantly attenuated COX-2 and TNF-α release. Also, NR-INF-02 significantly reduced IL-1β-induced PGE2 levels at 250 and 500 µg/mL in a concentration-dependent manner (Fig. 4b).
a Effect of NR-INF-02 on IL-1β-induced IL-6 and IL-8 release in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently IL-1β (10 ng/mL) was added and incubated for 48 h. IL-6 and IL-8 released were estimated. Values are presented as mean ± standard error of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control. b Effect of NR-INF-02 on IL-1β-induced PGE2, TNF-α, COX-2 levels in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently IL-1β (10 ng/mL) was added and incubated for 48 h. PGE2, TNF-α and COX-2 levels were estimated. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control
Effect of NR-INF-02 on NF-κB expression in LPS-induced RAW264.7 cells
LPS treatment at 1 µg/mL significantly increased NF-κB expression in RAW264.7 cells. NR-INF-02 at concentrations (31.25–500 µg/mL) significantly attenuated LPS-induced NF-kB expression (Fig. 5).
Effect of NR-INF-02 on LPS-induced NF-κB expression in RAW264.7 cells. RAW264.7 cells were treated with indicated concentrations of NR-INF-02 for 1 h. Subsequently incubated with LPS (1 µg/mL) for 24 h and NF-kB expression was measured. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from LPS control
Effect of NR-INF-02 on IL-1β-stimulated ICAM-1 expression in NHAC-kn cells
IL-1β treatment at 10 ng/mL induced significant increase of ICAM-1 expression in NHAC-kn cells. NR-INF-02 at 125, 250 and 500 µg/mL significantly inhibited IL-1β-induced ICAM-1 expression (Fig. 6).
Effect of NR-INF-02 on IL-1β-induced ICAM-1 expression in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently incubated with IL-1β (10 ng/mL) for 24 h. ICAM-1 expression was measured. Values are presented as mean ± standard error of the mean three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control
Effect of NR-INF-02 on GAG and type II collagen synthesis in IL-1β stimulated NHAC-kn cells
IL-1β at 10 ng/mL induced significant degradation of intracellular glycosaminoglycan content of chondrocytes. NR-INF-02 at 500 µg/mL significantly protected IL-1β-induced degradation of GAG (Fig. 7a). IL-1β at 10 ng/mL induced significant degradation of intracellular type II collagen content. NR-INF-02 treatment at 125, 250 and 500 µg/mL protected IL-1β-induced degradation of type II collagen content (Fig. 7b).
a Effect of NR-INF-02 on IL-1β-induced glycosaminoglycan degradation in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently incubated with IL-1β (10 ng/mL) for 72 h. NHAC-kn cells were lysed and glycosaminoglycan content was estimated. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control. b Effect of NR-INF-02 on IL-1β-induced type II collagen degeneration in NHAC-kn cells. NHAC-kn cells were treated with indicated concentrations of NR-INF-02 and subsequently incubated with IL-1β (10 ng/mL) for 72 h. NHAC-kn cells were lysed and type II collagen content was estimated. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from IL-1β control
Effect of NR-INF-02 on H2O2-induced cell senescence
Hydrogen peroxide treatment induced premature senescence to NHAC-kn cells. NR-INF-02 at concentration range of 125–500 µg/mL significantly protected H2O2 mediated cell senescence in a concentration dependent manner (Fig. 8).
Effect of NR-INF-02 on H2O2-induced cell senescence in NHAC-kn cells. NHAC-kn cells were incubated with H2O2 for 2 h and treated with indicated concentrations of NR-INF-02 for 24 h. NHAC-kn cells were lysed and senescence-associated β-galactosidase activity was estimated. Values are presented as mean ± standard error of the mean of three replicates. An asterisk indicates a significant (*p < 0.05) difference from H2O2 control
Discussion
Osteoarthritis, the rheumatic disease, is a degenerative malady driven in part by signalling mechanisms induced by stress and inflammation-induced factors. Increased expression of pro-inflammatory cytokines and matrix metalloproteinases (MMPs) in response to endogenous and exogenous etiological factors is believed to play a major role in the development of OA via COX-2/PGE2-dependent pathways at the early stage of disease. While at the late stage, apoptosis mechanisms play a role in pathogenesis of OA. However, these two stages of OA overlap because of the crosstalk between inflammation and apoptosis (Marcu et al. 2010; Wang et al. 2013). These factors activate normally quiescent chondrocytes of cartilage leading to loss of homeostasis in the articular cartilage Thus, therapies targeting the inflammation and apoptosis in the joint will maintain homeostasis (equilibrium between anabolic and catabolic factors) in the joint and thus combating the progression of OA.
Current pharmacological treatments focus on reduction of pain and increase mobility to improve overall quality of life, but their efficacy on delaying or preventing the progression of the disease is limited (Qin et al. 2013). However, traditional ayurvedic medicines have shown to be as effective as pharmaceuticals in relieving OA symptoms. In addition these traditional medicines may exert their benefits by influencing the progression of disease. Hence, the herbal formulation containing C. longa extract standardized to polysaccharides was developed for management of pain and inflammation associated with OA. The present study was performed to investigate the effects of NR-INF-02 on cartilage homeostasis via exploring its effects on biomarkers for cartilage synthesis and degeneration in vitro. The findings suggest that NR-INF-02 significantly inhibited IL-1β-induced chondrocyte death, apoptosis, release of IL-6, IL-8, TNF-α, PGE2, ICAM-1 and COX-2 in NHAC-kn cells and NF-kB in RAW264.7 cells. In addition NR-INF-02 also inhibited IL-1β-induced damage to synthesis markers such as glycosaminoglycans and type II collagen. Further, NR-INF-02 attenuated H2O2-mediated cell senescence.
Clinical OA is now considered to be preceded by a silent “pre-radiographic” phase during which extensive metabolic (anabolic and catabolic) changes occur in the joint tissue without pain. Even before structural changes in the OA begin, the metabolic changes in the articular cartilage (ECM and chondrocytes) indicate initiation and progression of OA (Henrotin et al. 2013). Therapy targeting the metabolic changes in cartilage will aid in retarding the progression of disease course. Evidence of role of IL-1β in OA progression is well established. Exposure of IL-1β stimulates chondrocytes to produce catabolic factors resulting in chondrocyte degradative cascade of events subsequently culminating in chondrocyte death and apoptosis (López-Armada et al. 2006). In the present study, NR-INF-02 treatment did not induce proliferation of NHAC-kn cells. However, treatment with NR-INF-02 inhibited IL-1β-induced chondrocyte death and apoptosis. As apoptosis of chondrocytes is a potentially important feature of osteoarthritic cartilage degeneration, NR-INF-02 inhibitory effects on apoptosis result in protecting the cartilage degeneration.
Pro-inflammatory mediators from interleukin family (IL-1β, IL-6, IL-8, TNF-α) inflammatory signalling molecules and eicosanoids (NF-κB, COX-2 and PGE2) stimulate cartilage degrading enzymes and degrade ECM and disrupt ECM homeostasis leading to OA and associated symptoms such as pain and function disability (Lee et al. 2013). IL-1β is considered one of the key cytokines involved in the pathogenesis of OA. IL-1β induces inflammatory reactions and catabolic effects independently as well as being combined with other mediators with respect to articular cartilage and other elements of joint. IL-1β induces increase in TNFα, IL-6, IL-8, PGE2 and COX-2 while degrades ECM components viz., collagen and proteoglycans and promotes chondrocyte apoptosis (Qin et al. 2013; Wojdasiewicz et al. 2014; Hwang and Kim 2015). In the present study, NR-INF-02 significantly inhibited IL-1β-induced release of TNF-α, IL-6, IL-8, PGE2 and COX-2. Authors reported that oral administration of C. longa extract significantly decreased IL-1β. Decrease of IL-1β levels was reported to have strong association with reduction in WOMAC and VAS scores in OA subjects (Srivastava et al. 2016; Saksena et al. 2016). In a randomized placebo controlled study, NR-INF-02 administered at 1000 mg once daily for 42 days significantly (p < 0.05) decreased the severity of pain and improved the function of affected knee as assessed by validated tools such as WOMAC, VAS and CGIC in patients with painful knee osteoarthritis (Madhu et al. 2013). The plausible effects of NR-INF-02 in ameliorating OA pain and functional disability observed in randomized placebo controlled trial could partly be attributed to inhibitory effect of NR-INF-02 on catabolic factors (IL-1β, TNFα, IL-6, IL-8, COX-2, and PGE2) involved in cartilage degeneration and nociceptive stimuli. NR-INF-02 significantly decreased joint pain induced by MIA in rat model. NR-INF-02 administered as a single and multiple doses to the MIA-treated rats significantly improved the hind paw weight distribution. In addition, NR-INF-02 treatment significantly decreased PGEM (metabolite of PGE2) levels in the MIA-induced OA rats (unpublished data). These effects observed in rats on joint pain could be due to inhibitory effects of NR-INF-02 on catabolic and nociceptive factors such as cytokines, eicosanoids etc. The anti-inflammatory effects of NR-INF-02 observed in in vitro test systems re-enforce the current study findings. NR-INF-02 demonstrated strong inhibition on LPS stimulated PGE2, IL-12 production, NO and IL-6 production in-vitro (Chandrasekaran et al. 2013).
NF-κB plays a crucial role in the distinctive inflammatory processes such as OA and RA, leading to cartilage destruction and articular damage. In articular chondrocytes, NF-κB activation mediates decreased expression of chondrocyte specific genes (collagen type II, link protein gene), and increased expression of MMPs (MMP-1, MMP-3, MMP-13), cytokines (IL-6, IL-8) and chemokines. Also, NF-kB involved in the regulation of apoptosis in articular chondrocytes. Thus, NF-κB appears as an attractive target for OA (Roman-Blas and Jimenez 2006). In the present study, LPS-induced NF-κB expression in RAW264.7 cells was attenuated by NR-INF-02.
Intercellular adhesion molecule-1 is expressed on synoviocytes, macropages and vascular endothelial cells more abundantly in OA tissue. ICAM-1 activates pro-inflammatory and inflammatory cascades thus resulting in inflammation and damage to cartilage (Benito et al. 2005). Synovial fluid levels of ICAM-1 correlates with WOMAC pain scores in OA subjects (Karatay et al. 2004). In the present study, NR-INF-02 significantly inhibited ICAM-1 expression in human articular chondrocytes.
ECM consists of primarily network type II collagen and proteoglycans that contain majorly glycosaminoglycans (GAG) (Gao et al. 2014). Pro-inflammatory and inflammatory cytokines have a primarily destructive impact on articular cartilage. It is a multilevel impact that involves decrease in synthesis of ECM components such as GAG and type II collagen as well as apoptosis of chondrocytes. Damage to collagen and GAG might result in disturbed chondrocyte anchorage to ECM that leads to chondrocyte apoptosis and progression of OA (Wojdasiewicz et al. 2014; Hwang and Kim 2015). The present study demonstrated chondroprotective effects of NR-INF-02 via inhibiting IL-1β-induced degradation of GAG, type II collagen and apoptosis in human articular chondrocytes.
Ageing is the greatest risk factor related to OA, and is presumed that chondrocyte senescence causes irreversible damage leading to cell death. Oxidative stress (higher ratio of oxidized glutathione to reduced glutathione) remains the culprit mechanism for chondrocyte senescence and cell death (Carlo and Loeser 2003). NR-INF-02 inhibits H2O2-induced senescence in human articular chondrocyte evident from the decrease in β-galactosidase (SA-β-gal) positively stained cells. H2O2 is known to induce oxidative stress and thus senescence. Plausibly NR-INF-02 could have inhibited chondrocyte senescence via inhibiting oxidative stress.
In conclusion, NR-INF-02 demonstrated on cartilage homeostasis in chondrocytes by inhibiting the cartilage degradative markers and improving the synthesis markers. Overall the observed beneficial effects of NR-INF-02 in preclinical and clinical trials on OA pain and inflammation could be due to the aforesaid mechanisms.
References
Anandakumar S, Joseph JA, Bethapudi B, Agarwal A, Jung E-B (2014) Anti-inflammatory effects of turmeric (Curcuma longa L.) extract on acute and chronic inflammation models. J Korean Soc Food Sci Nutr 43:612–617
Bauer DC, Hunter DJ, Abramson SB, Attur M, Corr M, Felson D et al (2006) Classification of osteoarthritis biomarkers: a proposed approach. Osteoarthr Cartil 14:723–727. https://doi.org/10.1016/j.joca.2006.04.001
Beg S, Swain S, Hasan H, Barkat M, Hussain MS (2011) Systematic review of herbals as potential anti-inflammatory agents: recent advances, current clinical status and future perspectives. Pharmacogn Rev 5:120–137. https://doi.org/10.4103/0973-7847.91102
Benito MJ, Veale DJ, FitzGerald O, van den Berg WB, Bresnihan B (2005) Synovial tissue inflammation in early and late osteoarthritis. Ann Rheum Dis 64:1263–1267. https://doi.org/10.1136/ard.2004.025270
Bharathi B, Sasikumar M, Ramanaiah I, Deepak M, Chandrasekaran CV (2017) Bioactive Turmerosaccharides from Curcuma longa extracts (NR-INF-02): potential ameliorating effect on osteoarthritis pain. Pharmacogn Mag 13(Suppl S3):623–627. https://doi.org/10.4103/pm.pm_465_16
Carlo MD, Loeser RF (2003) Increased oxidative stress with aging reduces chondrocyte survival: correlation with intracellular glutathione levels. Arthritis Rheumatol 48:3419–3430. https://doi.org/10.1002/art.11338
Chandrasekaran CV, Sundarajan K, Edwin JR, Gururaja GM, Mundkinajeddu D, Agarwal A (2013) Immune-stimulatory and anti-inflammatory activities of Curcuma longa extract and its polysaccharide fraction. Pharmacogn Res 5:71–79. https://doi.org/10.4103/0974-8490.110527
Cheng W, Wu D, Zuo Q, Wang Z, Fan W (2013) Ginsenoside Rb1 prevents interleukin-1 beta induced inflammation and apoptosis in human articular chondrocytes. Int Orthop 37:2065–2070. https://doi.org/10.1007/s00264-013-1990-6
Choi CH, Kim TH, Sung YK, Choi CB, Na YI, Yoo H, Jun JB (2014) SKI306X inhibition of glycosaminoglycan degradation in human cartilage involves down-regulation of cytokine-induced catabolic genes. Korean J Intern Med 29:647–655. https://doi.org/10.3904/kjim.2014.29.5.647
Dai SM, Shan ZZ, Nakamura H, Masuko-Hongo K, Kato T, Nishioka K, Yudoh K (2006) Catabolic stress induces features of chondrocyte senescence through overexpression of caveolin 1: possible involvement of caveolin 1-induced down-regulation of articular chondrocytes in the pathogenesis of osteoarthritis. Arthritis Rheumatol 54:818–831. https://doi.org/10.1002/art.21639
Gao Y, Liu S, Huang J, Guo W, Chen J, Zhang L et al (2014) The ECM-cell interaction of cartilage extracellular matrix on chondrocytes. Biomed Res Int 2014:648459. https://doi.org/10.1155/2014/648459
Haseeb A, Chen D, Haqqi TM (2013) Delphinidin inhibits IL-1β-induced activation of NF-κB by modulating the phosphorylation of IRAK-1Ser376 in human articular chondrocytes. Rheumatology 52:998–1008. https://doi.org/10.1093/rheumatology/kes363
Henrotin Y, Priem F, Mobasheri A (2013) Curcumin: a new paradigm and therapeutic opportunity for the treatment of osteoarthritis: curcumin for osteoarthritis management. Springerplus 1:56. https://doi.org/10.1186/2193-1801-2-56
Hwang HS, Kim HA (2015) Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int J Mol Sci 16:26035–26054. https://doi.org/10.3390/ijms161125943
Karatay S, Kiziltunc A, Yildirim K, Karanfil RC, Senel K (2004) Effects of different hyaluronic acid products on synovial fluid levels of intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 in knee osteoarthritis. Ann Clin Lab Sci 34:330–335
Kienzle G, von Kempis J (1998) Vascular cell adhesion molecule 1 (CD106) on primary human articular chondrocytes: functional regulation of expression by cytokines and comparison with intercellular adhesion molecule 1 (CD54) and very late activation antigen 2. Arthritis Rheumatol 41:1296–1305. https://doi.org/10.1002/1529-0131(199807)41:7
Lane NE, Brandt K, Hawker G, Peeva E, Schreyer E, Tsuji W, Hochberg MC (2011) OARSI-FDA initiative: defining the disease state of osteoarthritis. Osteoarthr Cartil 19:478–482. https://doi.org/10.1016/j.joca.2010.09.013
Lee AS, Ellman MB, Yan D, Kroin JS, Cole BJ, van Wijnen AJ, Im HJ (2013) A current review of molecular mechanisms regarding osteoarthritis and pain. Gene 527:440–447. https://doi.org/10.1016/j.gene.2013.05.069
Liu Q, Lu Z, Wu H, Zheng L (2015) Chondroprotective effects of taurine in primary cultures of human articular chondrocytes. Tohoku J Exp Med 235:201–213. https://doi.org/10.1620/tjem.235.201
López-Armada MJ, Caramés B, Lires-Deán M, Cillero-Pastor B, Ruiz-Romero C, Galdo F, Blanco FJ (2006) Cytokines, tumor necrosis factor-alpha and interleukin-1beta, differentially regulate apoptosis in osteoarthritis cultured human chondrocytes. Osteoarthr Cartil 14:660–669. https://doi.org/10.1016/j.joca.2006.01.005
Madhu K, Chanda K, Saji MJ (2013) Safety and efficacy of Curcuma longa extract in the treatment of painful knee osteoarthritis: a randomized placebo controlled trial. Inflammopharmacology 21:129–136. https://doi.org/10.1007/s10787-012-0163-3
Marcu KB, Otero M, Olivotto E, Borzi RM, Goldring MB (2010) NF-kappaB signaling: multiple angles to target OA. Curr Drug Targets 11:599–613
Nakata K, Ono K, Miyazaki J, Olsen BR, Muragaki Y, Adachi E, Yamamura K et al (1993) Osteoarthritis associated with mild chondrodysplasia in transgenic mice expressing alpha 1 (IX) collagen chains with a central deletion. Proc Natl Acad Sci USA 90:2870–2874. https://doi.org/10.1073/pnas.90.7.2870
Pulai JI, Chen H, Im HJ, Kumar S, Hanning C, Hegde PS, Loeser RF (2005) NF-kappa B mediates the stimulation of cytokine and chemokine expression by human articular chondrocytes in response to fibronectin fragments. J Immunol 174:5781–5788
Qin J, Liu Y, Liu J, Li J, Tan Y, Li X et al (2013) Effect of Angelica sinensis polysaccharides on osteoarthritis in vivo and in vitro: a possible mechanism to promote proteoglycans synthesis. Evid Based Complement Altern Med 2013:794761. https://doi.org/10.1155/2013/794761
Roman-Blas JA, Jimenez SA (2006) NF-kappaB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthr Cartil 14:839–948. https://doi.org/10.1016/j.joca.2006.04.008
Saksena AK, Srivastava S, Khattri S, Kumar S (2016) Efficacy of Curcuma longa in osteoarthritis: association of IL-1β, IL-10 and MMP-9 with severity of disease. J Immunol 196:13
Sandell L, Aigner T (2001) Articular cartilage and changes in arthritis: cell biology of osteoarthritis. Arthritis Res 3:107–113. https://doi.org/10.1186/ar148
Sokolove J, Lepus CM (2013) Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskelet Dis 5:77–94. https://doi.org/10.1177/1759720X12467868
Sophia Fox AJ, Bedi A, Rodeo SA (2009) The basic science of articular cartilage structure, composition, and function. Sports Health 1:461–468. https://doi.org/10.1177/1941738109350438
Srivastava S, Saksena AK, Khattri S, Kumar S, Dagur RS (2016) Curcuma longa extract reduces inflammatory and oxidative stress biomarkers in osteoarthritis of knee: a four-month, double-blind, randomized, placebo-controlled trial. Inflammopharmacology 24:377–388
Terry DE, Rees-Milton K, Pruss C, Hopwood J, Carran J, Anastassiades TP (2007) Modulation of articular chondrocyte proliferation and anionic glycoconjugate synthesis by glucosamine (GlcN), N-acetyl GlcN (GlcNAc) GlcN sulfate salt (GlcN.S) and covalent glucosamine sulfates (GlcN-SO4). Osteoarthr Cartil 15:946–956. https://doi.org/10.1016/j.joca.2007.02.010
Wang P, Guan PP, Guo C, Zhu F, Konstantopoulos K, Wang ZY (2013) Fluid shear stress-induced osteoarthritis: roles of cyclooxygenase-2 and its metabolic products in inducing the expression of proinflammatory cytokines and matrix metalloproteinases. FASEB J 27:4664–4677. https://doi.org/10.1096/fj.13-234542
Wojdasiewicz P, Poniatowski ŁA, Szukiewicz D (2014) The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediat Inflamm 2014:561459. https://doi.org/10.1155/2014/561459
Wu C, Zhao W, Zhang X, Chen X (2015) Neocryptotanshinone inhibits lipopolysaccharide-induced inflammation in RAW264.7 macrophages by suppression of NF-κB and iNOS signaling pathways. Acta Pharm Sin B 5:323–329. https://doi.org/10.1016/j.apsb.2015.01.010
Acknowledgements
The authors are thankful to Indo–Spanish Joint Programme, Department of Biotechnology (DBT) of India, Centre for the development of Industrial Technology (CDTI) of Spain for providing partial financial assistance to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Velusami, C.C., Richard, E.J. & Bethapudi, B. Polar extract of Curcuma longa protects cartilage homeostasis: possible mechanism of action. Inflammopharmacol 26, 1233–1243 (2018). https://doi.org/10.1007/s10787-017-0433-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-017-0433-1