Abstract
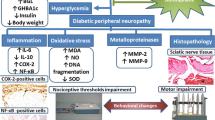
Emerging role of Nrf-2/HO-1 in pathogenesis of diabetic neuropathy has been suggested. Diabetic neuropathy is one of the most common complications of diabetes and more than 50% patients of diabetes develop diabetic neuropathy. Rutin has been well documented to show protective effect in various complications, e.g., diabetic neuropathy. However, its mechanistic insight is still not completely understood. The present study has been designed to explore the protective effect of rutin and its interaction with COX-2 inhibitor, nimesulide in diabetic neuropathy. DN (diabetic neuropathy) rats were maintained with or without rutin (100 and 200 mg/kg), nimesulide (5 and 10 mg/kg), and their combinations for 8 weeks. Body weight, serum glucose, pain assessment (mechanical allodynia, cold allodynia, mechanical hyperalgesia, and thermal hyperalgesia), and motor nerve conduction velocity (MNCV) were measured in all groups. Oxidative damage was assessed through biochemical estimation and mitochondrial ROS production, followed by inflammatory and apoptotic markers (TNF-α, caspase-3, Nrf-2, HO-1, and NF-kBp65) for their activity, protein, and gene expression. The structural changes were also reported through transmission electron microscope. Streptozotocin injection (55 mg/kg) induced diabetes reduced body weight, reduced the threshold for pain in various pain assessment parameters. Oxidative damage (increased MDA, decreased SOD, catalase, and GSH levels) increased mitochondrial ROS production followed by increased expression of inflammatory markers and decreased expression of Nrf-2/HO-1 in sciatic nerve. Treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) significantly attenuates these alterations as compared to DN control rats. Furthermore, combination of rutin (200 mg/kg) and nimesulide (10 mg/kg) significantly potentiated their protective effect which was significant as compared to their effect alone in streptozotocin-treated rats. The present study suggests the involvement of Nrf-2/HO-1 pathway in the protective effect of rutin against streptozotocin-induced diabetic neuropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic neuropathy is the most common complication of diabetes and more than 50% of diabetic patients suffer from this complication. The progression of diabetic neuropathy is multifactorial (Kumar and Mittal 2017; Van Dam 2002). However, oxidative stress and neuroinflammation remain the dominant and key role players. Hyperglycemia provides metabolic trigger for ROS generation. This ROS production leads to oxidative damage, which further results in neuroinflammation as well as neuronal damage. Nrf-2/HO-1 plays a pivotal role for defence against oxidative damage and neuroinflammation in diabetic neuropathy (Agca et al. 2014; Cardozo et al. 2013; Kumar and Mittal 2017). HO-1 expression is dependent on Nrf-2 expression. Structural aspects involve demyelination of neurons in sciatic nerves (Yang et al. 2016). The decreased expression of Nrf-2/HO-1 results in neuroinflammation (Ahmed et al. 2017). Nrf-2, body’s anti-oxidant defence mechanism has been reported as a key molecular connexion in the progression of diabetic neuropathy via inflammatory cascade and apoptotic pathway (Kumar and Mittal 2017). Studies have suggested that genetic overexpression of Nrf-2 prevents onset of diabetes and its complications (Bing et al. 2012), and decreased levels of Nrf-2 are reported in the various diabetic complications (Bhakkiyalakshmi et al. 2015; Tian et al. 2016).
Sciatic nerve is the majorly effected nerve in diabetic neuropathy. Structural and morphological aspects involve changes in myelination, neurofilaments, and mitochondria number in sciatic nerves (Ma et al. 2014; Xu et al. 2016). However, the complex interplay oxidative damage and Nrf-2/HO-1, neuroinflammation, and neuronal damage are still not fully understood.
In the current scenario, the presently available drugs are inadequate in terms of safety and efficacy, and have their own limitations in terms of side effects. Eventually, the quest for newer drug interventions or pharmacological approaches is increasing. Rutin (a bioflavonoid glycosidic derivative of quercetin) has been known for its anti-diabetic, anti-oxidant, and anti-inflammatory activities (Chua 2013; Ganeshpurkar and Saluja 2017). Rutin has also been reported to play a critical role in oxidative stress and inhibits production of various inflammatory mediators.
Rutin has been suggested to show potential as a diabetic neuropathy treatment via anti-inflammatory activity. Therefore, the present study investigated the role of rutin in diabetic neuropathy along with COX-2 inhibitors. These eicosanoids, formed by cyclooxygenase-dependent metabolism of arachidonic acid, are important physiological mediators of sciatic nerve damage. The purpose of choosing selective COX-2 inhibitor is to inhibit inducible COX-2 (there by decreasing inflammation) as COX-2 expression is mainly involved in inflammation (Quilley et al. 2011). In addition, it will not show any effect on COX-1 activity, thereby minimising risk of toxicity.
Based on this background, the present study was designed to explore the role of Nrf-2/HO-1 in the protective effect of rutin and its interaction with nimesulide against in experimental model of STZ-induced diabetic neuropathy.
Materials and methods
Animals
Male Wistar rats (200–250 g) obtained from Central Animal House, Panjab University Chandigarh were used in the current study. All the animals were acclimatized to laboratory conditions prior to experimentation. They were maintained on a 12-h light/dark cycle and water and standard laboratory diet were available ad libitum. All the experiments were performed between 9:00 and 17:00 h to avoid any circadian effect. The experimental protocol was approved by Institutional Animal Ethics Committee (IAEC) of Panjab University (PU/IAEC/S/15/29, 15/09/2015) and carried out in accordance with the guidelines of Committee for the Purpose of Control and Supervision of Experimentation on Animals (CPCSEA), Government of India, and Indian National Science Academy Guidelines for the use and care of experimental animals. All the behavioral studies were carried out by a person who is blinded to treatment groups.
Induction and assessment of diabetes
Diabetes was induced by single intraperitoneal (i.p.) injection of streptozotocin (Streptozotocin, 55 mg/kg) dissolved in 0.1-M citrate buffer (pH 4.5) to overnight fasted rats. Glucose (5% w/v) supplementation was given for first 8 h to prevent hypoglycaemic shock. Blood samples were collected after 48 h of Streptozotocin injection from retro-orbital plexus under light anaesthesia and blood glucose was measured. Animals with blood glucose level more than 250 mg/dL are considered diabetic and are used for further studies. Blood glucose was measured using glucose estimation kit (AMS analysers, Italy).
Drugs and treatment schedule
Diabetic animals were divided into different groups (n = 10) (Table 1). Rutin (100 and 200 mg/kg, i.p.) (Sigma-Aldrich, USA) and nimesulide (5 and 10 mg/kg, i.p) (Panacea Biotech, Lalru, Punjab) was prepared in 0.25% w/v sodium carboxy methyl cellulose and administered for 8 weeks. Rutin (100 and 200 mg/kg, i.p) was co-administered with nimesulide (5 and 10 mg/kg, i.p) for a period of 8 weeks in diabetic animals. All drugs are freshly prepared and administered in a constant volume of 0.5 ml/100 g. Each group received drug treatment daily in the morning for 8 weeks at 10:00 am to avoid influence of circadian rhythm (Fig. 1).
Behavioral assessments
Body weight and glucose estimation
Body weights of all the animals were recorded on week 0 and week 8 before behavioral examinations. The mean weight of the animals was recorded as compared to the naive treatment and the results are expressed as percentage change in body weight as compared to naïve group on eighth week.
Calculation of % change in body weight
Serum glucose was measured using glucose estimation kit (AMS analysers, Italy).
Pain assessment
Mechanical allodynia
Allodynia was measured in rats using an automated von-frey apparatus (IITC Life Sciences, USA). Animals were placed individually in a clear plastic cage containing mesh (1 cm2 perforations). They were well adapted to the testing environment for 30 min prior to testing. A polypropylene rigid tip of 0.5 mm diameter was used to apply force to the plantar region of the left hind paw. The tip was capable of applying a maximum force of 90 g. The pressure at which the animal withdraws its paw was recorded. The test was repeated three times at the interval of 15 min and the mean value was finally calculated and recorded (Pilat et al. 2016).
Cold allodynia
Individual animals were placed on a cold plate maintained at 5 ± 1 °C which was surrounded by a Plexiglas counter. The cut-off time of 3 min was maintained. Time latency to paw licking/lifting was observed and recorded (Berrocoso et al. 2011).
Mechanical hyperalgesia
Paw withdrawal threshold was assessed by Randall–Selitto paw pressure analgesia meter (IITC Life Science, Woodland Hills, CA). Increasing pressure was applied at the plantar region of hind paw and the pressure at which animal withdraws its paw was recorded. The cut-off threshold was 250 g to avoid potential tissue damage. Test was repeated three times at the interval of 10 min and mean value was finally recorded (Santos-Nogueira et al. 2012).
Thermal hyperalgesia
Animals were placed individually on the Eddy’s hot plate maintained at 55 ± 0.5 °C. Time latency for paw licking/jumping was noted. The cut-off time of 10 s was maintained to avoid tissue damage (Kuhad and Chopra 2009).
Electrophysiological examination (MNCV)
After last set of behavioral assessments, animals were anaesthetized with thiopentone sodium 30 mg/kg. An incision was made on the left thigh and the sciatic nerve was exposed. Recording electrodes were placed superficially into the plantar region of the foot and sciatic nerve was stimulated with 3 V proximally at sciatic notch and distally at tibial notch. Mean nerve conduction velocity (MNCV) was measured using the Power Lab instrument (AD Instruments, Power Lab Chart, Australia) (Kandhare et al. 2012):
Sample collection
The rats were sacrificed and sciatic nerves were collected from each group. For transmission electron microscopy, the samples from each group (size 2 × 2 mm) were kept in TEM fixative solution at 4 °C and subjected to ultramicrotomy. For biochemical and molecular studies, sciatic nerves were dissected out and stored at − 20 °C for further estimations with ELISA. For qRT-PCR, the samples were stored in RNA later at − 80 °C.
Biochemical estimations
First, 10% (w/v) tissue homogenates of sciatic nerve were prepared in 0.1 M phosphate buffer (pH 7.4). The homogenates were centrifuged at 10,000 g at 4 °C for 15 min and the supernatants so formed were separated and used for biochemical estimations.
Lipid peroxidation
The extent of lipid peroxidation in sciatic nerves was determined by performing the procedure as previously described by Wills (1966). Malondialdehyde (MDA) is taken to be a marker of lipid peroxidation. Its reaction with thiobarbituric acid (TBA) was measured using a PerkinElmer Lambda 20 Spectrophotometer (Norwalk, CT, USA) at 532 nm. The values were calculated using molar extinction coefficient of chromophore (1.56 × 105M−1 cm−1) and expressed as nanomoles of malondialdehyde per milligram of protein.
Superoxide dismutase activity
Superoxide dismutase activity estimation was based on its ability to inhibit the reduction of nitroblue tetrazolium (NBT). This is initiated by the addition of hydroxylamine hydrochloride to the reaction mixture containing NBT and the sample. The results were expressed as unit/mg protein, where one unit of enzyme is defined as the amount of enzyme inhibiting the rate of reaction by 100%. The readings were recorded using a spectrophotometer at 560 nm (Kono 1978).
Reduced glutathione (GSH) estimation
GSH activity in the sciatic nerves was measured according to the method previously described by Ellman (1959). One milliliters of supernatants were precipitated with 1 ml of 4% sulfosalicylic acid and cold digested at 4 °C for 1 h. The samples were centrifuged at 1200 rpm for 15 min at 4 °C. To 1 ml of this supernatant, 2.7 ml of 0.1-M phosphate buffer (pH 8) and 0.2 ml of 5,5-dithiobis 2-nitrobenzoic acid (DTNB) were added. The absorbance was read immediately at 412 nm, and the results were calculated using molar extinction coefficient of chromophore (1.36 × l04 M−1 cm−1) and expressed as micromole GSH per milligram protein.
Catalase estimation
Catalase estimation is carried out by measuring the breakdown of hydrogen peroxides. The assay mixture consists of 3 ml of H2O2 phosphate buffer and 0.05 ml of supernatant of tissue homogenate (10%), and the change in absorbance is recorded at 240 nm. The results are expressed as micromole H2O2 decomposed per milligram of protein/min (Luck 1963).
Protein estimation
Protein estimations were done by biuret method utilizing bovine serum albumin as standard (Gornall et al. 1949).
Mitochondrial ROS estimation
Isolation of mitochondria
Mitochondria were isolated from the sciatic nerve as described by Puka-Sundvall et al. (2000) with minor modifications. Briefly, the sciatic nerves were homogenized in ice-cold buffer (10-mM Tris–HCl (pH 7.4), 320-mM sucrose, 5-mM EDTA, and 0.1% BSA). The 10% (w/v) homogenates were centrifuged at 2100× g for 15 min at 4 °C. After discarding pellet, the supernatants were re-centrifuged at 14,000× g for 15 min at 4 °C. The crude mitochondrial pellet was separated and washed with buffer and again centrifuged at 7000× g for 15 min at 4 °C. The final mitochondrial pellets were re-suspended in buffer [10 mM Tris–HCl (pH 7.4), 0.44 M sucrose] and the purity of mitochondrial preparation will be checked by measuring the activity of succinate dehydrogenase (King et al. 1976).
Mitochondrial ROS
ROS production by mitochondria was detected using a membrane-permeable fluorescent dye dichlorodihydrofluorescein diacetate (H2-DCFDA) as described by Wang and Joseph (1999). DCF fluorescence was measured at 485 nm excitation and 520 nm emission. ROS production was calculated using the standards with known concentrations of DCF, the product of H2-DCF oxidation. The results were expressed as pmol/min/mg protein.
ELISA
The quantification of inflammatory and apoptotic markers, i.e., TNF-α, caspase-3, and NF-kBp65 were done as per manufacturer’s instructions provided in rats TNF-α, caspase-3 (R&D systems, Minneapolis, MN, USA), and NF-kBp65 (Elabscience biotechnology Co. Ltd).
RNA isolation and qRT-PCR
Total RNA was isolated from sciatic nerve samples using Trizol reagent method as earlier described (Guerrero et al. 2012). Briefly, tissues were homogenized in RNAisoplus®reagent (Takara Bioscience Inc., Shiga, Japan). Aqueous and organic phases were separated using chloroform followed by RNA precipitation with isopropanol from aqueous phase. Integrity of the RNA samples was checked on 1.0% agarose gel and quantified by InfiniteVRM200 Pro NanoQuant (Tecan, Switzerland). RNA (1.0 μg of total RNA) was reverse transcribed to cDNA using RT-first strand synthesis kit (Qiagen, Cat. No. 205411, Hilden, Germany) as per the manufacturer’s instructions.
Relative expression of different genes was determined by quantitative RT-PCR (Applied Biosystems 7500 Fast Real-Time PCR machine) using SYBR green dye based assay (QuantiNova™ SYBR® green PCR kit, QigenGmbh, Hilden, Germany, Cat. No. 208052) under the following assay conditions: 95 °C for 10 min, followed by 40 cycles at 95 and 60 °C for 1 min. Detailed primer sequences are mentioned in Table 2. GAPDH gene was used as internal reference gene. Data were analyzed using 2−DDCt method and values were expressed in terms of fold change relative to naïve rats.
Transmission electron microscope studies
Sciatic nerve tissue samples (size: 2 × 2 mm) were fixed in karnovsky’s fixative for 6–8 h at 4 °C. These were post-fixed in 1% osmium tetroxide in 0.1-M phosphate buffer for 1 h at 4 °C. The samples were dehydrated and embedded in Araldite CY212. Thin sections were mounted on copper grids and stained with uranyl acetate and lead acetate. These were then observed under Tecnai T20 G2 microscope (Fei Company, The Netherlands) at a magnification range of 1100–9900×. Images were acquired using Digital Micrograph Software (Gatan, Inc).
Statistical analysis
Statistical analysis was performed using GraphPad Prism (Graph Pad Software, San Diego, CA). A group of ten animals (n = 10) were assigned to a specific drug treatment. Results were expressed as mean ± S.E.M. The data were analyzed by two analysis of variance (ANOVA) followed by Bonferroni post tests for behavioral parameters and one-way analysis of variance (ANOVA) followed by Tukey’s test for motor nerve conduction velocity and biochemical estimations, ELISA, and qRT-PCR. p < 0.05 was considered to be statistically significant.
Results
Body weight and serum glucose
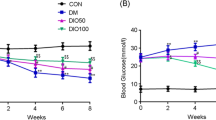
Body weight
Streptozotocin injection (55 mg/kg)-induced diabetes exhibited significant fall in body weight on eighth week as compared to naïve group (Fig. 2a). Rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) treatment for 8 weeks significantly attenuated loss in body weight as compared to DN control group. Furthermore, co-administration of rutin with nimesulide [(rutin (100 mg/kg) + nimesulide (5 mg/kg); rutin (200 mg/kg) + nimesulide (10 mg/kg)] did not produce any significant effect on the loss of body weight as compared to their effect per se in streptozotocin-treated animals (Fig. 2a).
Effect of rutin, nimesulide, and their combination on body weight and serum glucose in diabetic rats. a % change in body weight. b Serum glucose estimation. Data are expressed as mean ± S.E.M. a p < 0.05 as compared to naive group; b p < 0.05 as compared to DN control group; c p < 0.05 as compared to rut (100); d p < 0.05 as compared to nim (5); e p < 0.05 as compared to rut (200); f p < 0.05 as compared to nim (10). (One-way ANOVA followed by Tukey’s post test). Rut rutin (100 mg/kg), Rut (200) rutin (200 mg/kg), Nim nimesulide (5 mg/kg), Nim (10) nimesulide (10 mg/kg)
Glucose estimation
Streptozotocin injection (55 mg/kg)-induced diabetes exhibited a significant increase in serum glucose levels on eighth week as compared to naïve group (Fig. 2b). Rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) treatment for 8 weeks significantly attenuated serum glucose levels as compared to DN control group. Furthermore, co-administration of rutin with nimesulide [(rutin (100 mg/kg) + nimesulide (5 mg/kg); rutin (200 mg/kg) + nimesulide (10 mg/kg)] restored the serum glucose levels as compared to their effect per se in streptozotocin-treated animals (Fig. 2b).
Pain assessment
Mechanical allodynia
Single streptozotocin (55 mg/kg) injection significantly increased mechanical allodynia (decreased paw withdrawal threshold) from fourth to eighth week as compared to naïve group (Fig. 3a). The treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) for 8 weeks significantly raised paw withdrawal threshold from fourth to eighth week as compared to control group (Fig. 3a). However, combinations of rutin (100 and 200 mg/kg) with nimesulide (5 and 10 mg/kg) significantly potentiated their protective (raised paw withdrawal threshold) effect, respectively, as compared to their effect per se in streptozotocin diabetic group (Fig. 3a).
Effect of rutin, nimesulide, and their combination on pain assessment in diabetic rats. a Mechanical allodynia. b Cold allodynia. c Mechanical hyperalgesia. d Thermal hyperalgesia. Data are expressed as mean ± S.E.M. a p < 0.05 as compared to naive group; b p < 0.05 as compared to DN control group; c p < 0.05 as compared to rut (100); d p < 0.05 as compared to nim (5); e p < 0.05 as compared to rut (200); f p < 0.05 as compared to nim (10). (Two-way ANOVA followed by Bonferroni post test). Rut rutin (100 mg/kg), Rut (200) rutin (200 mg/kg), Nim nimesulide (5 mg/kg), Nim (10) nimesulide (10 mg/kg)
Cold allodynia
Single intraperitoneal injection of streptozotocin (55 mg/kg) significantly delayed time latency to paw licking/lifting to cold stimuli from fourth to eighth week (increased the total duration of the hind paw licking and lifting) as compared to the naïve group (Fig. 3b). The treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) for 8 weeks significantly decreased paw withdrawal latency on fourth to eighth week as compared to diabetic control group. However, combination of rutin (200 mg/kg) with nimesulide (5 and 10 mg/kg) further decreased paw withdrawal latency significantly from fourth to eighth week as compared to their effect per se in streptozotocin diabetic group (Fig. 3b).
Mechanical hyperalgesia
Single streptozotocin (55 mg/kg) injection significantly produced mechanical hyperalgesia (decreased paw withdrawal threshold) from fourth to eighth week as compared to naïve group. Treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) for 8 weeks significantly raised paw withdrawal threshold from fourth to eighth week as compared to diabetic control group (Fig. 3c). However, co-administration of rutin (100 and 200 mg/kg) with nimesulide (5 and 10 mg/kg), respectively, further influences significantly paw withdrawal threshold from fourth to eighth week as compared to their effect per se in streptozotocin diabetic group (Fig. 3c).
Thermal hyperalgesia
Single streptozotocin injection (55 mg/kg) significantly decreased paw withdrawal latency from fourth to eighth week as compared to naïve group. Eight week treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) improved paw withdrawal latency as compared to control group (Fig. 3d). However, combination of rutin (100 and 200 mg/kg) with nimesulide (5 and 10 mg/kg) did not show any significant improvement (increased paw withdrawal threshold) as compared to their effect per se in streptozotocin-induced diabetic animals (Fig. 3d).
Motor nerve conduction velocity
Streptozotocin administration (55 mg/kg) significantly reduced motor nerve conduction velocity on eighth week as compared to the naïve group. Treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) significantly improved motor nerve conduction velocity of sciatic nerve as compared to control group (Fig. 4). However, combination of rutin (100 mg/kg) and nimesulide (10 mg/kg) potentiated their protective effect (improved motor nerve conduction velocity) significantly as compared to their effect per se in streptozotocin diabetic group (Fig. 4).
Effect of rutin, nimesulide, and their combination on motor nerve conduction velocity in diabetic rats. a MNCV assembly. b Lab chart (AD instruments). c Δt calculations from lab chart. d MNCV data. Data are expressed as mean ± S.E.M. a p < 0.05 as compared to naive group; b p < 0.05 as compared to DN control group; c p < 0.05 as compared to rut (100); d p < 0.05 as compared to nim (5); e p < 0.05 as compared to rut (200); f p < 0.05 as compared to nim (10). (One-way ANOVA followed by Tukey’s post test). Rut rutin (100 mg/kg), Rut (200) rutin (200 mg/kg), Nim nimesulide (5 mg/kg), Nim (10) nimesulide (10 mg/kg)
Oxidative damage (via biochemical estimations and mitochondrial ROS)
Biochemical estimations
Intraperitoneal administration of streptozotocin significantly increased MDA and depleted SOD, catalase, and reduced glutathione levels in sciatic nerve as compared to the naïve group (Fig. 5a). Eight week treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) significantly attenuated MDA, and restored GSH and catalase enzyme activities as compared to DN control group. Furthermore, combinations of rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg), respectively, potentiated their protective effect (anti-oxidant effect, i.e., MDA, GSH, and catalase enzyme activities) which was significant as compared to their effect per se in streptozotocin-treated animals (Fig. 5a).
Effect of rutin, nimesulide, and their combination on oxidative damage by biochemical estimations in diabetic rats. a Biochemical estimations. i) Reduced glutathione estimation. ii) Malondialdehyde estimation. iii) Superoxide dismutase estimation. iv) Catalase estimation. b Mitochondrial ROS estimation. Data are expressed as mean ± S.E.M. a p < 0.05 as compared to naive group; b p < 0.05 as compared to DN control group; c p < 0.05 as compared to rut (100); d p < 0.05 as compared to nim (5); e p < 0.05 as compared to rut (200); f p < 0.05 as compared to nim (10). (One-way ANOVA followed by Tukey’s post test). Rut rutin (100 mg/kg), Rut (200) rutin (200 mg/kg), Nim nimesulide (5 mg/kg), Nim (10) nimesulide (10 mg/kg)
Mitochondrial ROS
Intraperitoneal administration of streptozotocin significantly increased mitochondrial ROS production in sciatic nerve as compared to the naïve group (Fig. 5b). Eight weeks treatment with rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) significantly attenuated mitochondrial ROS production as compared to DN control group. Furthermore, combinations of rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg), respectively, potentiated their protective effect (decreased mitochondrial ROS production) which was significant as compared to their effect per se in streptozotocin-treated animals (Fig. 5b).
Inflammatory markers (NF-kBp65, TNF-α, and caspase-3) assessments (via ELISA)
Single injection of streptozotocin (55 mg/kg) significantly increased NF-kB p65, TNF-α and caspase-3 as compared to naïve rats. Rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) treatment for 8 weeks significantly attenuated NF-kBp65, TNF-α and caspase-3 activity as compared to DN control group. Furthermore, combination of rutin (100 mg/kg and 200 mg/kg) with nimesulide (5 and 10 mg/kg) for 8 weeks significantly potentiated their protective effect (attenuated NF-kBp65, TNF-α and caspase-3 activity) which was significant as compared to their effect per se in streptozotocin-treated animals (Fig. 6a).
Effect of rutin, nimesulide, and their combination on inflammatory marker activity and gene expression in diabetic rats. a Levels of key inflammatory markers in sciatic nerve (NF-kBp65, TNF-alpha, and caspase-3). b Gene expression of Nrf-2 and HO-1 in sciatic nerve. Data are expressed as mean ± S.E.M. a p < 0.05 as compared to naive group; b p < 0.05 as compared to DN control group; c p < 0.05 as compared to rut (100); d p < 0.05 as compared to nim (5); e p < 0.05 as compared to rut (200); f p < 0.05 as compared to nim (10). (One-way ANOVA followed by Tukey’s post test). Rut rutin (100 mg/kg), Rut (200) rutin (200 mg/kg), Nim nimesulide (5 mg/kg), Nim (10) nimesulide (10 mg/kg)
Nrf2 and HO-1 gene expression (via qRT-PCR)
The above experiments demonstrated the involvement of inflammatory cascade in diabetic nephropathy. Based on this, the key neuroinflammatory marker in concern, i.e., Nrf-2 and HO-1 (Nrf-2 dependent) was further indicated by gene expression studies using qRT-PCR (Fig. 7). qRT-PCR also manifest the upsurge in relative Nrf-2 and HO-1 mRNA expression in DN control rats to be reversed by rutin (200 mg/kg) and its combination with nimesulide (10 mg/kg) treatment groups. However, the relative Nrf-2 and HO-1 mRNA expression remained unchanged in case of nimesulide (10 mg/kg) group as compared to DN control group (Fig. 6b).
Effect of rutin, nimesulide, and their combination on sciatic nerve under transmission electron microscope. (Magnification: 1100–9900X). a Naïve. b DN control. c Rutin (100 mg/kg). d Rutin (200 mg/kg). e Nimesulide (5 mg/kg). f Nimesulide (10 mg/kg). g Rutin (100 mg/kg) + Nimesulide (5 mg/kg). h Rutin (200 mg/kg) + Nimesulide (10 mg/kg)
Microscopic studies (via TEM)
Intraperitoneal administration of streptozotocin (55 mg/kg) treatment significantly showed demyelination, dense neurofilaments, and increased mitochondrial number after eighth weeks as compared to naive group of animals. Rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) treatment for 8 week significantly showed less dense neurofilaments and less increase in mitochondrial number, improved demyelination as compared to DN control rats (Fig. 7). Besides, nimesulide (5 and 10 mg/kg) treated animals, shows more vacuole formation as compared to Rutin (100 and 200 mg/kg). However, combination of rutin (200 mg/kg) and nimesulide (10 mg/kg) restored the changes as compared to their effect alone in DN control rats (Fig. 7).
Discussion
Streptozotocin is a glucosamine-nitrourea derivative, possessing cytotoxic action mediated by reactive oxygen species, liberation of toxic amounts of NO, alkylation, and damages of DNA which result in rapid destruction of pancreatic β-cells. Studies have reported the antinociceptive effect of rutin in various animal models of neuropathic pain (Azevedo et al. 2013; Hernandez-leon et al. 2016). In the present study, single intraperitoneal injection of STZ decreased the body weight as well as the threshold of various pain assessments (mechanical allodynia, cold allodynia, mechanical hyperalgesia, and thermal hyperalgesia). Rutin, nimesulide, and their combinations did not produce any significant reversal of decreased body weight, but the threshold levels were restored in pain assessment in DN control rats.
The study has also observed the capability of rutin to lower blood glucose levels (Niture et al. 2014). In line with this, the present study also demonstrates the decrease in levels of serum glucose with rutin. A further, MNCV measurements, oxidative damage demonstrated that Streptozotocin i.p. (55 mg/kg) resulted in diabetic neuropathy at eighth week. Reports document the reduction in nerve blood flow and peripheral nerve perfusion leading to conduction deficits (Coppey et al. 2001). At the end of study (eighth week), DN control rats have showed decreased motor nerve conduction velocity of sciatic nerve as compared to naïve group. Rutin, nimesulide, and their combinations have restored decreased motor nerve conduction velocity as compared to DN control rats. The decrease in MNCV was restored by rutin, nimesulide, and their combinations, suggesting less nerve damage.
Despite, pathophysiology of diabetic neuropathy being multifactorial, oxidative stress and neuroinflammation has been reported to be the leading cause of progression of diabetic neuropathy (Kumar and Mittal 2017; Van Dam 2002). The oxidative stress a critical role player in nerves due to their lower anti-oxidant capacity. In the present study, rutin, nimesulide, and their combinations modulated the biochemical activities of various stress biomarkers (MDA levels, SOD, GSH, and catalase activity) as compared to DN control rats. Along with this, we examined the role of mitochondrial ROS production in sciatic nerve in diabetic neuropathy. It was found that rutin, nimesulide, and their co-treatment has attenuated the increase in mitochondrial ROS production as compared to DN control rats. In the present study, combination of rutin with nimesulide showed superior reversal of the progression of diabetic neuropathy in DN control rats as compared to their individual effects. These results are substantiated with the studies which displayed the mitochondrial damage or ROS production also impairs nerve functions (Coppey et al. 2001; Van Dam 2002).
The previous studies have reported the generation of dense neurofilaments and increased mitochondrial number in sciatic nerve of diabetic rats as compared to naïve rats (Ma et al. 2014; Sameni and Panahi 2011; Xu et al. 2016). In line with the reported studies, the structural changes in sciatic nerve were observed by transmission electron microscope (TEM imaging) which revealed that the DN control group had damaged sciatic nerve as compared to naïve animals. The structural degradation involved damage to myelin sheath, vacuole formation, dense neurofilaments, and increased mitochondrial number as compared to naïve rats. Rutin (100 and 200 mg/kg) and nimesulide (5 and 10 mg/kg) have restored these structural damages to sciatic nerve as compared DN control rats. In addition, the significant restoration in structural degeneration was observed in combined treatment of Rutin (200 mg/kg) and nimesulide (10 mg/kg), in which myelin sheath has restored (striations of myelin sheath are visible); neurofilaments along with mitochondrial number have decreased and are comparable to naïve rats.
Nrf2 being an anti-oxidant defence plays a critical role in diabetic neuropathy (Kaspar et al. 2009). Especially under stressful conditions, Nrf2 plays a major role in maintaining homeostasis. Nrf2 pathway has been suggested to play a significant role in anti-oxidant defence mechanism (Negi et al. 2011a). Nrf2 and HO-1 (heme oxygenase-1) have been suggested to have protective effect against diabetic neuropathy (Negi et al. 2015, Mittal and Kumar 2017). Nrf2 acts as a hub for the progression of oxidative damage and neuroinflammation. Although rutin has been studied in various models of diabetic neuropathy (Tian et al. 2016; Je et al. 2002), but to the best of our knowledge, the present study is the first study to explore potential role of rutin in the cross-talk between neuroinflammation and oxidative stress (via Nrf-2/HO-1/NF-kB signalling pathway) in streptozotocin-induced diabetic neuropathy (Fig. 8).
The expressions of various inflammatory markers along with Nrf-2 and HO-1 gene were measured. It was found that levels of NF-kBp65, TNF-α and caspase-3 were raised in DN control rats. However, the levels of gene expression of Nrf-2 and HO-1 were found to be decreased in DN control rats. Rutin, nimesulide and their co-treatment ameliorates the increased levels of inflammatory and apoptotic markers, namely NF-kBp65, TNF-α and caspase-3 as compared to DN control rats. Rutin was more potent than nimesulide in ameliorating these protective effects. Apart from this, levels of Nrf-2 and HO-1 gene expression were restored in rutin and rutin in combination with nimesulide as compared to DN control rats but nimesulide alone did not produce any significant change in levels of Nrf-2 and HO-1 gene expression as compared to DN control rats.
Studies have shown that p65 overexpression results in downregulation or even diminished the nrf2-ARE signalling (Negi et al. 2011b). RelA (p65) promotes HDAC3 association with Mafk, thus, preventing heterodimer formation with nrf2, and, therefore, decreasing expression of ARE-related genes. Both nrf2 and p65 act as competitive binding site for transcriptional co-activators CBP (CREB-binding protein)-p300 complex (Li et al. 2008). CBP interacts with neh4 and neh5 domain within nrf2, resulting in acetylation of neh1 domain. P65 has more affinity to bind with CBP as compared to nrf2 complex. The p65 has been reported to show dual role on nrf2 activity. In the absence of nrf2, NF-kB exacerbates, which further causes rise in cytokine levels (Li et al. 2008). In addition, Nrf2 activation is known to inhibit NF-kB activation, and NF-kB has been known in inhibition of Nrf2 (Negi et al. 2011c; Ganesh Yerra et al. 2013), suggesting that the cross-talk between NF-kB activation and Nrf-2 inhibition results in neuroinflammation.
Oxidative stress and neuroinflammation works in an inter-related fashion. Keap-1/Nrf-2/ARE signalling pathway mainly regulates anti-inflammatory gene expression and inhibits progression of inflammation. Along with anti-inflammatory, this signalling pathway also regulates the expression of anti-oxidant genes (Palsamy et al. 2011; Huang et al. 2015). The key molecular connexion for these pathways being Nrf-2. This suggests the ameliorative effect of rutin in neuroinflammation and oxidative stress by acting through Nrf-2. In oxidative stress signalling, the imbalance in anti-oxidant production and Nrf-2/HO-1 decrease leads to overexpression of levels of stress-related biochemical (Wang et al. 2017). HO-1 is an inducible form of Heme Oxygenase. It catalyses the degradation of heme to free iron (Fe2+) and carbon monoxide (CO). Heme acts as pro-inflammatory marker and CO acts as anti-inflammatory compound. This crucial step stands for the protective effect of HO-1, which in turn depends upon levels of Nrf-2 (Yama et al. 2015). In neuroinflammatory signalling, the decreased levels of Nrf-2 lead to increase in various inflammatory markers (esp. NF-kB) and resulted in disease progression (Fig. 8).
Conclusion
Rutin ameliorates the streptozotocin-induced behavioral, electrophysiological, biochemical, molecular, as well as gene expression alterations by Nrf-2/HO-1 and NF-kB signalling pathway. The connexions in neuroinflammatory and oxidative stress being decrease in Nrf-2 levels and rutin restored the levels of Nrf-2. Along with rutin, nimesulide has shown additive effect in the potential protective effect of rutin through anti-inflammatory action on COX-2 inhibition. This concludes that the rutin via Nrf-2/HO-1 and NF-kB signalling pathway ameliorates the progression of streptozotocin-induced diabetic neuropathy. However, the complex mechanistic cascade involved is still need to be refolded and further explored to understand the complete mechanism.
References
Agca CA, Tuzcu M, Hayirli A, Sahin K (2014) Taurine ameliorates neuropathy via regulating NF-kappaB and Nrf2/HO-1 signaling cascades in diabetic rats. Food Chem Toxicol 71:116–121
Ahmed SM, Luo L, Namani A, Wang XJ, Tang X (2017) Nrf2 signaling pathway: pivotal roles in inflammation. Biochim Biophys Acta 1863:585–597
Azevedo MI et al (2013) The antioxidant effects of the flavonoids rutin and quercetin inhibit oxaliplatin-induced chronic painful peripheral neuropathy. Mol Pain 9:53
Berrocoso E et al (2011) Evaluation of milnacipran, in comparison with amitriptyline, on cold and mechanical allodynia in a rat model of neuropathic pain. Eur J Pharmacol 655:46–51
Bhakkiyalakshmi E, Sireesh D, Rajaguru P, Paulmurugan R, Ramkumar KM (2015) The emerging role of redox-sensitive Nrf2–Keap1 pathway in diabetes. Pharmacol Res 91:104–114
Bing L, Shujun L, Lining M, Lu C (2012) Prevention of diabetic complications by activation of Nrf-2: diabetic cardiomyopathy and nephropathy. Exp Diabetes Res 2012:1–7
Cardozo LF et al (2013) Nutritional strategies to modulate inflammation and oxidative stress pathways via activation of the master antioxidant switch Nrf2. Biochimie 95:1525–1533
Chua LS (2013) A review on plant-based rutin extraction methods and its pharmacological activities. J Ethnopharmacol 150:805–817
Coppey LJ, Gellett JS, Davidson EP, Dunlap JA, Lund DD, Yorek MA (2001) Effect of antioxidant treatment of streptozotocin-induced diabetic rats on endoneurial blood flow, motor nerve conduction velocity, and vascular reactivity of epineurial arterioles of the sciatic nerve. Diabetes 50:1927–1937
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Ganesh Yerra V, Negi G, Sharma SS, Kumar A (2013) Potential therapeutic effects of the simultaneous targeting of the Nrf2 and NF-kappaB pathways in diabetic neuropathy. Redox Biol 1:394–397
Ganeshpurkar A, Saluja AK (2017) The pharmacological potential of rutin. Saudi Pharm J 25:149–164
Gornall AG, Bardawill CJ, David MM (1949) Determination of serum proteins by means of the biuret reaction. J Biol Chem 177:751–766
Guerrero L et al (2012) Inhibition of angiotensin-converting enzyme activity by flavonoids: structure-activity relationship studies. PLoS One 7:e49493
Hernandez-Leon A, Fernandez-Guasti A, Gonzalez-Trujano ME (2016) Rutin antinociception involves opioidergic mechanism and descending modulation of ventrolateral periaqueductal grey matter in rats. Eur J Pain 20:274–283
Huang Y, Li W, Su ZY, Kong AN (2015) The complexity of the Nrf2 pathway: beyond the antioxidant response. J Nutr Biochem 26:1401–1413
Je HD et al (2002) Combination of vitamin C and rutin on neuropathy and lung damage of diabetes mellitus rats. Arch Pharm Res 25:184–190
Kandhare AD, Raygude KS, Ghosh P, Ghule AE, Bodhankar SL (2012) Neuroprotective effect of naringin by modulation of endogenous biomarkers in streptozotocin induced painful diabetic neuropathy. Fitoterapia 83:650–659
Kaspar JW, Niture SK, Jaiswal AK (2009) Nrf 2: INrf2 (Keap1) signaling in oxidative stress. Free Radic Biol Med 47:1304–1309
King TE, Ohnishi T, Winter DB, Wu JT (1976) Biochemical and EPR probes for structure-function studies of iron sulfur centers of succinate dehydrogenase. Adv Exp Med Biol 74:182–227
Kono Y (1978) Generation of superoxide radical during autoxidation of hydroxylamine and an assay for superoxide dismutase. Arch Biochem Biophys 186:189–195
Kuhad A, Chopra K (2009) Tocotrienol attenuates oxidative-nitrosative stress and inflammatory cascade in experimental model of diabetic neuropathy. Neuropharmacol 57:456–462
Kumar A, Mittal R (2017) Nrf2: a potential therapeutic target for diabetic neuropathy. Inflammopharmacol 25:393–402
Li W et al (2008) Activation of Nrf2-antioxidant signaling attenuates NFkappaB-inflammatory response and elicits apoptosis. Biochem Pharmacol 76:1485–1489
Luck H (1963) Catalase spectrophotometric method. Academic Press, New York
Ma S, Liu D, Deng J, Peng Y (2014) Protective effect of mulberry flavonoids on sciatic nerve alloxan-induced diabetic rats. Braj J Pharm Sci 50:765–771
Negi G, Kumar A, Joshi RP, Sharma SS (2011a) Oxidative stress and Nrf2 in the pathophysiology of diabetic neuropathy: old perspective with a new angle. Biochem Biophys Res Commun 408:1–5
Negi G, Kumar A, Sharma SS (2011b) Melatonin modulates neuroinflammation and oxidative stress in experimental diabetic neuropathy: effects on NF-kappaB and Nrf2 cascades. J Pineal Res 50:124–131
Negi G, Kumar A, Sharma SS (2011c) Nrf2 and NF-kappaB modulation by sulforaphane counteracts multiple manifestations of diabetic neuropathy in rats and high glucose-induced changes. Curr Neurovasc Res 8:294–304
Negi G, Nakkina V, Kamble P, Sharma SS (2015) Heme oxygenase-1, a novel target for the treatment of diabetic complications: focus on diabetic peripheral neuropathy. Pharmacol Res 102:158–167
Niture NT, Ansari AA, Naik SR (2014) Anti-hyperglycemic activity of rutin in streptozotocin-induced diabetic rats: an effect mediated through cytokines, antioxidants and lipid biomarkers. Ind J Exp Biol 52:720–727
Palsamy P, Subramanian S (2011) Resveratrol protects diabetic kidney by attenuating hyperglycemia-mediated oxidative stress and renal inflammatory cytokines via Nrf2-Keap1 signaling. Biochim Biophys Acta 1812:719–731
Pilat D et al (2016) Blockade of IL-18 signaling diminished neuropathic pain and enhanced the efficacy of morphine and buprenorphine. Mol Cell Neurosci 71:114–124
Puka-Sundvall M et al (2000) Impairment of mitochondrial respiration after cerebral hypoxia-ischemia in immature rats: relationship to activation of caspase-3 and neuronal injury. Brain Res Dev Brain Res 125:43–50
Quilley J, Santos M, Pedraza P (2011) Renal protective effect of chronic inhibition of COX-2 with SC-58236 in streptozotocin-diabetic rats. Am J Physiol Heart Circul Physiol 300:H2316–H2322
Sameni H, Panahi M (2011) The effect of co-administration of 4-Methylcatechol and Progesterone on sciatic nerve function and neurohistological alterations in streptozotocin-induced diabetic neuropathy in rats. Cell J 13:31–38
Santos-Nogueira E, Redondo Castro E, Mancuso R, Navarro X (2012) Randall-Selitto test: a new approach for the detection of neuropathic pain after spinal cord injury. J Neurotrauma 29:898–904
Tian R et al (2016) Rutin ameliorates diabetic neuropathy by lowering plasma glucose and decreasing oxidative stress via Nrf2 signaling pathway in rats. Eur J Pharmacol 771:84–92
van Dam PS (2002) Oxidative stress and diabetic neuropathy: pathophysiological mechanisms and treatment perspectives. Diabetes Met Res Rev 18:176–184
Wang H, Joseph JA (1999) Quantifying cellular oxidative stress by dichlorofluorescein assay using microplate reader. Free Rad Biol Med 27:612–616
Wang X et al (2017) Tenuigenin inhibits LPS-induced inflammatory responses in microglia via activating the Nrf2-mediated HO-1 signaling pathway. Eur J Pharmacol 809:196–202
Wills ED (1966) Mechanisms of lipid peroxide formation in animal tissues. Biochem J 99:667–676
Xu X, Zhang D, Liao J, Wang Q, Qiu W (2016) Galanin and its receptor system promote the repair of injured aciatic nerves in diabetic rats. Neural Regen Res 11:1517–1526
Yama K, Sato K, Abe N, Murao Y, Tatsunami R, Tampo Y (2015) Epalrestat increases glutathione, thioredoxin, and heme oxygenase-1 by stimulating Nrf2 pathway in endothelial cells. Redox Biol 4:87–96
Yang X et al (2016) Paeoniflorin protects Schwann cells against high glucose induced oxidative injury by activating Nrf2/ARE pathway and inhibiting apoptosis. J Ethnopharmacol 185:361–369
Acknowledgements
The present study was funded by Department of science and technology (DST), (Grant SR/WOS-A/LS-1324/2014 dated 14.05.2015), New Delhi has been gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no conflict of interest.
Additional information
Ruchika Mittal (nee Garg).
Rights and permissions
About this article
Cite this article
Mittal, R., Kumar, A., Singh, D.P. et al. Ameliorative potential of rutin in combination with nimesulide in STZ model of diabetic neuropathy: targeting Nrf2/HO-1/NF-kB and COX signalling pathway. Inflammopharmacol 26, 755–768 (2018). https://doi.org/10.1007/s10787-017-0413-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-017-0413-5