Abstract
Sargahydroquinoic acid (SHQA) is a major plastoquinone in Sargassum macrocarpum and has shown the capacity to prevent inflammation and oxidative stress. However, the protective mechanisms were unclear. The molecular mechanisms of SHQA on ameliorating inflammation and oxidative stress have been investigated, using lipopolysaccharide (LPS)-stimulated macrophages. SHQA was isolated and purified from S. macrocarpum and the anti-inflammatory mechanisms were explored using LPS-stimulated murine macrophage RAW 264.7 cells. SHQA did not change the expression of cyclooxygenase-2 (COX-2) but inhibited the activity of COX-2. As a result, SHQA significantly diminished the secretions of nitric oxide (NO), prostaglandin E2 (PGE2), and multiple pro-inflammatory cytokines. LPS-induced activation of nuclear factor-κB (NF-κB) was inhibited by SHQA by preventing the degradation of inhibitor κB-α (IκBα). NF-κB activation was also downregulated by the inhibition of Akt phosphorylation in LPS-stimulated cells. Furthermore, SHQA induced the expression of heme oxygenase 1 via Nrf2 activation. These results indicated that SHQA inhibited LPS-induced expressions of inflammatory mediators via suppressing the Akt-mediated NF-κB pathway as well as upregulating the Nrf2/HO-1 pathway. Our findings suggest that SHQA might be a potential therapeutic agent in various inflammatory diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Inflammation is a complex biological response of body tissues against harmful stimulations. However, an excessive inflammatory response dysregulates tissue functions and eventually leads to severe tissue damages. Macrophages are major inflammatory and immune effector cells, which can be activated by exposure to bacterial lipopolysaccharide (LPS) or pro-inflammatory cytokines [1, 2]. During inflammation, pro-inflammatory cytokines, such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and IL-6, and inflammatory mediators, such as nitric oxide (NO) and prostaglandin (PG) E2, are largely produced by activated macrophages [3, 4]. Excessive production of these molecules can lead to the development of chronic diseases, such as inflammatory arthritis, cancer, and atherosclerosis [5,6,7]. Hence, substances inhibiting the production of these molecules would be developed as therapeutic agents for inflammatory diseases.
Nuclear factor-kappaB (NF-κB) is a critical regulator of inflammation as well as cell survival [8]. In response to inflammatory stimuli, inhibitory-κB kinase (IKK) is activated and initiates the phosphorylation and degradation of inhibitor of κB (IκB), which is bound to NF-κB. After dissociating from IκB, NF-kB translocates into the nucleus and promotes the transcriptions of pro-inflammatory mediators [9,10,11]. NF-κB is alternatively activated by mitogen-activated protein kinases (MAPKs), including p38 kinase, c-Jun NH2-terminal kinase (JNK), and extracellular signal-regulated kinase (ERK) [12]. Recent studies have demonstrated that the phosphatidyl inositol 3-kinase/Akt (PI3K/Akt) pathway is also responsible for the activation of NF-κB and subsequent expression of NF-κB-regulated inflammatory genes [8].
Heme oxygenase-1 (HO-1) is one major antioxidative enzyme, and it inhibits the secretion of pro-inflammatory mediators, including NO, PGE2, TNF-α, IL-6, and IL-1β as well as reactive oxygen species (ROS) by activated macrophages [13,14,15,16,17,18]. Nuclear transcription factor erythroid 2-related factor 2 (Nrf2) regulates the translation of HO-1. Upon oxidative stress challenge, Nrf2 translocates into the nucleus and binds to the antioxidant response element (ARE) promoter region of target genes such as HO-1 [19]. The anti-inflammatory reaction of HO-1 gene is exerted by suppressing the expression of pro-inflammatory mediators via NF-κB inactivation [20].
During our recent studies aiming at developing anti-inflammatory compounds from brown algae, we found sargahydroquinoic acid (SHQA) is a major component in one marine brown alga species, Sargassum macrocarpum, which was comprised to be 37.6% of its ethanolic extract. SHQA selectively accelerated cerebral blood flow through dilatation of the basilar artery without lowering systemic blood pressure [21]. It also inhibited TNF-α-induced MMP expression and age-related inflammation by suppressing the NF-kB pathway [22]. In this study, we found that SHQA showed strong anti-inflammatory activities at physiological concentrations (0.4-0.8 μM). This led us to elucidate the anti-inflammatory actions of SHQA and its molecular mechanism using LPS-activated macrophages.
MATERIALS AND METHODS
Reagents
Bovine serum albumin (BSA), 4,6′-diamidino-2-phenylindole (DAPI), 2′,7′-dichlorofluorescein diacetate (DCF-DA), dimethyl sulfoxide (DMSO), LPS, and phenylmethylsulfonyl fluoride (PMSF) were purchased from Sigma Chemical Co. (St. Louis, MO, USA). CellTiter96 AQueous One Solution Cell Proliferation assay kit, dual luciferase assay kit, pRL-TK DNA, and superscript reverse transcriptase were obtained from Promega (Madison, WI, USA). Murine NF-κB promoter/luciferase DNA was purchased from Stratagene (La Jolla, CA, USA). Primary antibodies were purchased from Abcam (Danvers, MA, USA). Alexa Fluor 488-conjugated secondary antibody, TRIzol, and Lipofectamine/Plus from Life Technology (Carlsbad, CA, USA) were used. Enhanced chemiluminescence detection kit was purchased from GE Healthcare Bio-Sciences (Piscataway, NJ, USA).
Isolation of SHQA
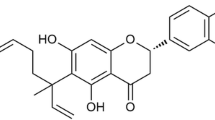
Sargassum macrocarpum was collected along the coast of Busan, South Korea in April 2018. Specimen identity was confirmed by an algologist (N.G. Kim), at the Department of Marine Biology and Aquaculture, Gyeongsang National University, South Korea. The isolation of SHQA had been described before [23]. In short, dried seaweed (1.0 kg) was extracted twice with 80% (v/v) ethanol (6 L/each). The ethanolic extract (102 g) was obtained by concentration under reduced pressure. The separation and elution conditions can be referred to [23]. The structure and chromatogram of SHQA are shown in Fig. 1.
Spectrometric Analysis of SHQA
1H- and 13C-NMR spectra were determined on a JNM ECP-400 spectrometer (JEOL, Japan), using CD3OD with tetramethylsilane as an internal standard. Heteronuclear multiple quantum correlation and heteronuclear multiple bond correlation spectra were recorded using pulsed-field gradients.
Structure Identification of SHQA
C27H36O4 (MW = 424): 1H-NMR (CD3OD, 400 MHz); 3.25 (2H, d, J = 7.4 Hz, H-1), 5.29 (1H, dt, J = 7.3 and 1.4 Hz, H-2), 2.08 (2H, m, H-4), 2.12 (2H, m, H-5), 5.14 (1H, t, J = 7.0 Hz, H-6), 2.08 (2H, m, H-8), 2.50 (2H, dt, J = 7.0 and 7.0, H-9), 5.83 (1H, t, J = 7.3 Hz, H-10), 2.21 (2H, t, J = 7.7 Hz, H-12), 2.12 (2H, m, H-13), 5.07 (1H, tt, J = 7.3 and 1.4 Hz, H-14), 1.65 (3H, s, CH3-16), 1.56 (3H, s, CH3-17), 1.59 (3H, s, CH3-19), 1.70 (3H, s, H-20), 6.38 (2H, brs, H-3′ and H-5′), 2.14 (3H, s, aromatic-CH3). 13C-NMR (CD3OD, 100 MHz); 29.6 (C-1), 124.1 (C-2), 136.8 (C-3), 40.9 (C-4), 27.6 (C-5), 125.96 (C-6), 135.5 (C-7), 40.3 (C-8), 28.9 (C-9), 142.7 (C-10), 132.9 (C-11), 36.0 (C-12), 29.0 (C-13), 124.8 (C-14), 133.3 (C-15), 25.9 (C-16), 17.8 (C-17), 171.7 (C-18), 15.96 (C-19), 16.2 (C-20), 146.5 (C-1′), 131.3 (C-2′), 114.5 (C-3′), 151.4 (C-4′), 115.7 (C-5′), 127.5 (C-6′), 16.9 (aromatic-CH3).
Cell Culture and Sample Treatment
Murine macrophages cell line RAW 264.7 cells (ATCC, Rockville, MD, USA) were maintained in Dulbecco’s modified Eagle medium containing 10% FBS, 100 units/mL penicillin, and 100 μg/mL streptomycin sulfate in a humidified incubator with 5% CO2 air condition. Cells were pretreated with SHQA at indicated concentrations for 1 h followed by stimulating with LPS (1 μg/mL).
Cytotoxicity Assay
Cell viability was determined using the CellTiter96® AQueous One Solution Cell Proliferation assay kit. Cells were seeded at a density of 5 × 104 cells/well into 96-well. After 24 h, cells were pretreated with different concentrations of SHQA for 1 h then stimulated with LPS (1 μg/mL). Twenty-four hours later, the culture medium was replaced with a mixture of 95 μL fresh culture medium and 5 μL MTS solution. After 1 h, the absorbance reading at 490 nm was acquired using a microplate reader (Glomax Multi Detection System, Promega).
Cyclooxygenase-2 Activity
Cyclooxygenase (COX)-2 activity was analyzed using an assay kit from Cayman Chemical Company (Ann Arbor, MI, USA). Cell pellets were homogenized in cold buffer (0.1 M Tris-HCl, pH 7.8 containing 1 mM EDTA) and centrifuged at 10,000×g for 15 min. The supernatant was used for COX-2 enzyme solution. One hundred microliters of assay buffer, 10 μL of hemin, and 10 μL of supernatant were mixed and then 10 μL of different concentrations of SHQA was added and mixed. The reaction mixture was incubated for 5 min at 25°C, and then 20 μL N,N,N′,N′-tetramethyl-p-phenylenediamine (TMPD) and 20 μL of arachidonic acid solution were added. After incubating for 5 min at 25°C, the absorbance at 590 nm was measured. The values were normalized by total cell number
Intracellular ROS Level
The intracellular ROS level was measured using fluorescent probe DCF-DA. Cells were seeded into a black 96-well plate at a density of 5 × 104/well. On the second day, the cells were co-treated with SHQA and LPS. Two hours later, the cells were then treated with 20 μM DCF-DA. Thirty minutes later, the fluorescence intensity was acquired as described before [24].
Measurement of NO, PGE2, TNF-α, IL-1β, and IL-6
Cells (seeded at 10 × 105 cells/well) were pretreated with SHQA (0-0.8 μM) for 1 h followed by stimulation with LPS for 24 h. Culture media were collected after centrifuging at 2000×g for 10 min and stored at −75°C before analysis. The nitrite concentration was measured as an indicator of NO production, using the Griess reaction [17]. Levels of TNF-α, IL-1β, and IL-6 were quantitatively determined using ELISA kits from R&D Systems (Minneapolis, MN, USA). PGE2 concentrations in culture media were measured using an enzyme immunoassay (EIA) kit from Cayman Chemical, according to the manufacturer’s recommended protocol.
Reverse Transcription-Polymerase Chain Reaction
RAW 264.7 cells plated in a 6-well culture plate were pretreated with SHQA for 1 h and stimulated with LPS for 6 h. Total RNA was isolated using TRIzol reagent and cDNA was synthesized with oligo-dT primer and M-MLV reverse transcriptase. PCR was conducted with corresponding primers (Supplementary Table 1). Images were acquired through EZ-Capture II (ATTO, Tokyo, Japan) and densitometric analysis was conducted using the CS analyzer ver. 3.00 software (ATTO).
Immunocytochemical Analysis
RAW 264.7 cells were seeded on glass coverslips in 6-well plates and cultured for 24 h. After incubation with SHQA for 1 h, cells were stimulated with LPS (1 μg/mL) for 30 min. The specific procedure for immunofluorescence analysis of NF-kB and Nrf2 has been described in our previous paper [25].
Cytosolic and Nuclear Extract Preparation
RAW 264.7 cells in 60-mm cell culture plates were pretreated with SHQA for 1 h and then stimulated with LPS for 30 min. Cytosolic and nucleus fractions were separated as previously described [23].
Transfection and Luciferase Assay
pNF-κB promoter/luciferase DNA (2 μg) along with control pRL-TK DNA (40 ng) was transfected into RAW 264.7 cells using Lipofectamine Plus reagents. Thirty-six hours later, cells were treated with SHQA for 1 h then stimulated with LPS (1 μg/mL). After 6 h, cell wells were washed with ice-cold PBS twice and cell lysate was harvested with 70 μL of lysis buffer (0.5 mM HEPES pH 7.8, 1% Triton N-101, 1 mM CaCl2, and 1 mM MgCl2). Luciferase activity was determined with a luciferase assay kit. The luciferase activity was normalized with the expression of control pRL-TK.
Western Blot Analysis
Cells were pretreated with 0.4, 0.6, and 0.8 μM of SHQA for 1 h then challenged with LPS (1 μg/mL) for indicated time durations. The specific procedures for Western blot had been described before [25].
In Vivo Pro-inflammatory Cytokine Assay
Animal studies were conducted with the experimental protocols and procedures approved by the Animal Ethics Committee of the Pukyong National University. Mice were randomly grouped (n = 3). Mice were given SHQA (10 and 20 mg/kg of body weight) with oral administration for 4 consecutive days. Mice from the control group were given 20% propylene glycol at equal volume. One hour after the last oral administration, mice were intraperitoneally injected with LPS (2.0 mg/kg). After 2 h, blood was collected by cardiac puncture, and serum was obtained by centrifuging at 800×g for 20 min. Concentrations of pro-inflammatory cytokines such as TNF-α, IL-1β, IL-6, MCP-1, and IL-17 in the serum samples were measured.
Statistical Analysis
Quantitative results were expressed as mean ± standard deviation (SD) from at least three independent experiments unless otherwise indicated. Data were analyzed using one-way analysis of variance (ANOVA), followed by Tukey’s test for post hoc analysis. Differences with a P value less than 0.05 were considered statistically significant. All analyses were carried out using SPSS, version 10.07 (SPSS Inc., Chicago, IL, USA).
RESULTS
Effect of SHQA on Secretions of NO and PGE2
To evaluate the effect of SHQA on NO production in LPS-induced macrophages, we measured the nitrite concentrations in the culture media. As shown in Fig. 2a, SHQA dose-dependently reduced LPS-induced NO secretion, and IC50 was estimated to be 0.49 ± 0.03 μM (P < 0.05). SHQA also significantly inhibited PGE2 secretion (IC50 = 1.32 ± 0.12 μM, P < 0.05, Fig. 2b). MTS assay revealed that SHQA caused no cytotoxicity at concentration up to 1.6 μM in RAW 264.7 cells (Supplementary Fig. 1). Thus, the inhibited secretions of NO and PGE2 by SHQA were not due to cytotoxicity.
Effect of SHQA on secretions of NO and PGE2 in LPS-activated RAW 264.7 cells. Cells were pretreated with different concentrations of SHQA (0.4, 0.6, 0.8 μM) for 1 h then stimulated with LPS for 24 h. The cultured media were used to measure a) NO and b) PGE2 concentrations. Data are presented as mean ± SD. # P < 0.05, compared to the control group; * P < 0.05, compared to the LPS- treated group.
Effect of SHQA on iNOS and COX-2 Expressions
To determine whether the suppression of NO and PGE2 production by SHQA was associated with reduced iNOS and COX-2 expressions, we assessed the protein and mRNA expression levels of iNOS and COX-2. As shown in Fig. 3a, SHQA markedly suppressed the LPS-mediated increase of the iNOS protein level. However, COX-2 protein expression was not altered by SHQA. Consistent with protein results, SHQA inhibited LPS-induced iNOS transcription, whereas COX-2 mRNA level was not reduced by SHQA (Fig. 3). Interestingly, SHQA did not inhibit COX-2 expression, despite the reduced PGE2 production. To clarify this discrepancy, we analyzed the effect of SHQA on COX-2 activity. As shown in Fig. 3b, SHQA strongly inhibited COX-2 activity in a dose-dependent manner.
Inhibitory effect of SHQA on expression of iNOS and COX-2 in LPS-activated RAW 264.7 cells. Cells were pretreated with SHQA for 1 h then stimulated with LPS for 16 and 24 h to determine mRNA and protein levels of a) iNOS and b) COX-2, respectively. c) Cells were pretreated with indicated concentrations of SHQA for 1 h then stimulated with LPS for 24 h. COX-2 activity was determined by COX-2 activity assay kit. COX-2 activity is normalized by total cell number. Data are presented as mean ± SD. #P < 0.05, compared to the control group; *P < 0.05, compared to the LPS- treated group.
Effect of SHQA on the Production of Pro-inflammatory Cytokines
Pro-inflammatory cytokines, such as TNF-α, IL-1β, and IL-6, are secreted at the early stage of the inflammatory response and recognized as key biomarkers of inflammation. We quantified the concentrations of these cytokines in the media using ELISA kits. As shown in Fig. 4, LPS-induced TNF-α, IL-1β, and IL-6 secretions were markedly decreased by SHQA in a dose-dependent manner. These results showed that SHQA suppressed LPS-induced pro-inflammatory cytokine secretions, indicating that SHQA inhibits the initial phase of the LPS-stimulated inflammatory response.
Effect of SHQA on secretion of pro-inflammatory cytokines in LPS-stimulated RAW 264.7 cells. Cells were pretreated with SHQA for 1 h and then stimulated with LPS for 24 h. a) TNF-α, b) IL-1β, and c) IL-6 protein levels in the cultured media were determined by ELISA. The data are presented as mean ± SD. *P < 0.05 compared to the LPS- treated group.
Effect of SHQA on LPS-Induced NF-κB Activation
NF-κB, as an important transcription factor, regulates the pro-inflammatory cytokines in LPS-activated macrophages. The effects of SHQA on the transcriptional activation of NF-κB in LPS-treated macrophages were analyzed. As shown in Fig. 5a, SHQA inhibited LPS-induced NF-κB promoter activity (P < 0.05). To further determine the effect of SHQA on NF-κB, cells were pretreated with SHQA, and proteins associated with NF-κB activation were determined using Western blot. After the LPS challenge, IKKβ was markedly phosphorylated and the phosphorylation was dose-dependently suppressed by SHQA (Fig. 5b). LPS-induced degradation of IκB-α was also attenuated by SHQA pretreatment. Moreover, the elevated nuclear NF-κB level, caused by LPS, was dose-dependently suppressed by SHQA. These results demonstrated that SHQA effectively inhibited the nuclear translocation and activation of NF-κB by suppressing the phosphorylation of IKKβ and the degradation of IκB-α.
Effect of SHQA on NF-κB activation in LPS-stimulated RAW 264.7 cells. a) Cells were transfected with NF-κB promoter-containing luciferase DNA along with control pRL-TK DNA for 40 h. Transfected cells were treated with LPS in the absence or presence of SHQA for 6 h. b) Cells pretreated with SHQA for 1 h were stimulated with LPS for 30 min. Cytosolic and nuclear fractions were prepared and used for Western blot. Data are presented as mean ± SD. #P < 0.05, compared to the control group. *P < 0.05, compared to the LPS-treated group.
Effect of SHQA on the Phosphorylation of Signaling Proteins
To further elucidate the possible molecular mechanisms of SHQA on NF-κΒ inactivation in LPS-activated macrophages, we examined the effect of SHQA on the phosphorylation of Akt and MAPKs, which are implicated with NF-κΒ activation. As shown in Fig. 6, SHQA did not affect the phosphorylation of JNK, whereas SHQA dose-dependently suppressed the phosphorylation of Akt, ERK, and p38 MAPK in LPS-activated cells. These data additionally suggested that SHQA regulates the activity of NF-κB, at least partially, through inhibiting Akt, ERK, and p38 MAPK phosphorylation.
Effects of SHQA on phosphorylations of Akt and MAPKs in LPS-stimulated RAW 264.7 cells. Cells were pretreated with SHQA for 1 h then stimulated with LPS for 30 min. Cell lysates were separated with SDS-PAGE and detected by Western blot. #P < 0.05, compared to the control group. *P < 0.05, compared to the LPS- treated group.
Effect of SHQA on the Regulation of HO-1 and Nrf2
Enhanced endogenous HO-1 leads to cellular protection against oxidative damage. Thus, we determined whether SHQA induces the protein and mRNA expressions of HO-1. As shown in Fig. 7a, the productions of HO-1 protein and mRNA were induced by LPS stimulation and further augmented dose-dependently by SHQA. Moreover, SHQA remarkably inhibited LPS-induced ROS production in a dose-dependent manner (Fig. 7b).
Effect of SHQA on regulation of HO-1 and Nrf2. a) Cells were pretreated with SHQA for 1 h then stimulated with LPS for 16 or 24 h to determine mRNA or protein levels, respectively. b) Cells were treated with SHQA and LPS simultaneously for 2 h. The cells were then treated with 20 μM DCF-DA for 30 min at 37°C. Data are presented as mean ± SD. #P < 0.05, compared to the control group. *P < 0.05, compared to the LPS-treated group.
Anti-inflammatory Activity of SHQA in Mice
To investigate the in vivo anti-inflammatory activity of SHQA, the serum pro-inflammatory cytokine levels were determined by ELISA. Administration of SHQA for 4 days did not cause any changes in body weight, or serum AST and ALT levels in mice (data not shown). The LPS treatment group showed increased levels of pro-inflammatory cytokines such as TNF-α (Fig. 8a), IL-1β (Fig. 8b), IL-6 (Fig. 8c), and IL-17 (Fig. 8d) in their serum; however, SHQA administration for 4 days suppressed the elevation of these pro-inflammatory cytokines in serum.
Effect of SHQA on pro-inflammatory cytokines in serum of LPS-injected mice. Mice were administrated with indicated concentrations of SHQA for 4 days and intraperitoneally injected with LPS (2.0 mg/kg). The concentrations of a) TNF-α, b) IL-1β, c) IL-6, and d) IL-17 in the serum were measured by ELISA kits. Data are presented as mean ± SD (n = 3). #P < 0.05, compared to the control group. *P < 0.05, compared to the LPS-treated group.
DISCUSSION
Health beneficial actions of S. macrocarpum have been associated with its high levels of meroterpenoids in the ethanolic extract. Recently we reported that ethanolic extract of S. macrocarpum showed anti-inflammatory activity in both in vivo and in vitro models [23, 26]. The quantitative analysis result showed that the content of SHQA was estimated to be 37.6% of the extract, suggesting that SHQA is a major compound in the extract of S. macrocarpum. Thus, we isolated SHQA from S. macrocarpum to investigate its anti-inflammatory mechanisms using RAW 264.7 macrophages. The anti-inflammatory effects of SHQA were, at least partly, attributed to the inhibition of the NF-κB signal pathway. Additionally, we found that Nrf2 and reduced cellular ROS level also play a critical role in inhibiting LPS-induced inflammatory response by SHQA.
SHQA selectively accelerated cerebral blood flow through dilatation of the basilar artery without lowering systemic blood pressure [21]. In a recent report, SHQA isolated from S. yezoense inhibited TNFα-induced MMP-2/-9 expression by suppressing AP-1 and NF-kB pathways via PPARα [22].
SHQA did not inhibit the production of COX-2, which is responsible for PGE2 production. Thus, we analyzed the inhibitory activity of SHQA on COX-2 activity and found that SHQA had strong COX-2 inhibitory activity (IC50, 0.46 ± 0.02 μM). Thus, we confirmed that the inhibition of PGE2 by SHQA was caused by its COX-2 inhibitory activity.
Adverse effects of excess NO are attributed to NO itself as an inflammatory factor and peroxynitrite that is produced by the reaction of NO and superoxide, leading to the oxidative damage of cellular molecules. Under pathophysiological conditions, a large amount of NO produced by iNOS provokes inflammatory progress and acts synergistically with pro-inflammatory cytokines [27]. Compounds capable of suppressing NO production may be attractive anti-inflammatory agents, and for this reason, the suppressive effects of natural compounds on NO production have been intensively studied for developing anti-inflammatory agents [23, 25, 28]. In this study, we found that SHQA remarkably inhibited iNOS protein and mRNA expressions in LPS-stimulated RAW 264.7 cells, leading to inhibition of NO production. PGE2 is also a key inflammatory mediator, whose production is primarily regulated by COX-2 [29]. Recent studies have shown that in vivo and in vitro treatments with natural compounds reduce inflammation by suppressing COX-2 [30]. In this study, SHQA directly inhibited the production of PGE2 through inhibiting COX-2 activity, but not COX-2 protein and mRNA expressions. LPS-injected mice are a classical animal model for evaluating potential anti-inflammatory agents because they show systemic inflammation [30]. Pro-inflammatory cytokines, including TNF-α, IL-6, and IL-1β, are related to the systemic signal of inflammation [31]. Also, high levels of pro-inflammatory cytokines contribute to various inflammatory diseases such as atherosclerosis, liver disease, and inflammatory arthritis [7, 32]. SHQA suppressed the releases of TNF-α, IL-1β, and IL-6 in LPS-activated macrophages. Similarly, we found that SHQA suppressed the levels of IL-1β, IL-6, IL-17, and TNF-α in the serum of LPS-stimulated mice (Fig. 7), indicating SHQA would be a promising candidate of therapeutic agent for inflammatory diseases. This is, to our knowledge, the first study to address the inhibition of pro-inflammatory cytokines in vivo by SHQA.
NF-κB is a critical transcription factor in the regulation of inflammatory mediators and pro-inflammatory cytokines [33, 34]. In a normal condition, NF-κB is sequestered by IκB-α in the cytoplasm. LPS initiates the activation of NADPH oxidase in immune cells and provokes ROS production, leading to activation of NF-κB through phosphorylation of IKKβ and degradation of IκB-α. The free NF-κB moves from cytosol to the nucleus and controls the expression of inflammatory genes [35,36,37]. In this study, we demonstrated that SHQA strongly suppresses the protein levels of NF-κB in the nucleus and cytosol in LPS-treated cells, based on Western blot analysis. Moreover, SHQA effectively inhibits IKKβ phosphorylation and IκB-α degradation, suggesting that inhibition of NF-κB activation by SHQA is largely attributed by inhibition of phosphorylation of IKKβ and degradation of IκB-α.
Induction of HO-1 attenuates oxidative damage and shows anti-inflammatory properties, which was demonstrated by in vitro and in vivo inflammatory models [38, 39]. The anti-inflammatory mechanism of HO-1 can be explained by the enzymatic degradation of pro-inflammatory heme and the production of anti-inflammatory CO and biliverdin, which is subsequently converted into bilirubin, a strong antioxidant [38]. HO-1 is transcriptionally regulated by Nrf2, a basic transcription factor required for cell protection against oxidative stress. LPS-induced ROS activates Nrf2 and leads to the overproduction of HO-1 [40]. Nrf2-mediated enhanced HO-1 by lutein repressed inflammatory responses via downregulating NF-κB signaling in LPS-stimulated BV2 cells, indicating that HO-1 is associated with inhibition of inflammation [41, 42]. In the present study, we found that SHQA dose-dependently increased HO-1 expression via Nrf2 activation. This report is, to our best knowledge, the novel findings to address that SHQA accomplished anti-inflammatory exertion through Nrf2/HO-1 pathway in LPS-stimulated cells.
Cumulative information derived from experimental reports has proven that NF-κB and Nrf2 are key regulators for maintaining the balance of cellular redox status and responding to inflammation [43]. Both pathways share common effectors and regulatory proteins for their activation; however, they control opposite cellular processes that lead to either cytoprotection or pathological development [44]. As evidence of crosstalk between NF-κB and Nrf2, NF-κB activation is suppressed by various phytochemicals activating Nrf2; however, detailed mechanistic evidence of Nrf2 role on NF-κB signaling is still unclear [41]. PI3K/Akt and MAPKs are critical signaling proteins connected with the transcriptional regulation of NF-κB and Nrf2 by degrading their respective inhibitors, IκB-α and Keap1, respectively [45, 46]. Lutein suppressed inflammatory responses through attenuating NF-kB activation by inhibiting the phosphorylation of p38 MAPK, JNK, and Akt, while promoting Nrf2 activation by ERK phosphorylation in LPS-stimulated BV2 cells [42]. In this study, we found that the phosphorylation of Akt, ERK, and p38 was suppressed by SHQA, suggesting Akt and MAPK pathways are involved in the repressed LPS-induced NF-κB activation by SHQA.
In conclusion, we demonstrated that SHQA inhibited the production of NO, PGE2, and multiple cytokines, including TNF-α, IL-6, and IL-1β in LPS-activated RAW 264.7 cells. The anti-inflammatory action of SHQA is associated with the inhibition of the NF-κB pathway as well as the activation of the Nrf2 pathway. Moreover, SHQA suppressed PGE2 production by direct inhibition of COX-2 activity. Oral administration of SHQA alleviated systemic inflammation in mice via reducing circulatory pro-inflammatory cytokines. Verification of SHQA’s anti-inflammatory action in cellular and animal models will be beneficial to further the application of SHQA in the therapeutic agent for inflammatory diseases.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Code Availability
None.
Abbreviations
- Akt:
-
Phosphatidylinositol 3-kinase (PI3K)/protein kinase B
- BSA:
-
Bovine serum albumin
- COX-2:
-
Cyclooxygenase 2
- DAPI:
-
4,6′-Diamidino-2-phenylindole
- DCF-DA:
-
4,6′-Diamidino-2-phenylindole
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- DMSO:
-
Dimethyl sulfoxide
- ECL:
-
Enhanced chemiluminescence
- ELISA:
-
Enzyme-linked immunosorbent assay
- ERK:
-
Extracellular signal-regulated kinase
- FBS:
-
Fetal bovine serum
- GAPDH:
-
Glyceraldehyde 3-phosphate dehydrogenase
- HMBC:
-
Heteronuclear multiple bond correlation
- HMQC:
-
Heteronuclear multiple quantum correlation
- HO-1:
-
Heme oxygenase 1
- IL-1β:
-
Interleukin-1 β
- IL-6:
-
Interleukin-6
- IκB-α:
-
Inhibitor of κB-α
- IKK:
-
Inhibitory κB kinase
- iNOS:
-
Inducible nitric oxide synthase
- JNK:
-
c-Jun NH2-terminal kinase
- LPS:
-
Lipopolysaccharide
- MAPKs:
-
Mitogen-activated protein kinases
- NF-κB:
-
Nuclear factor-κB
- NO:
-
Nitric oxide
- Nrf2:
-
Nuclear transcription factor-E2-related factor 2
- PBS:
-
Phosphate-buffered saline
- PGE2 :
-
Prostaglandin E2
- PMSF:
-
Phenylmethylsulfonyl fluoride
- ROS:
-
Reactive oxygen species
- SDS-PAGE:
-
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis
- TBST:
-
Tris-buffered saline with 0.05% Tween 20
- TNF-α:
-
Tumor necrosis factor-alpha
References
Guha, M., and N. Mackman. 2001. LPS induction of gene expression in human monocytes. Cellular Signalling 13 (2): 85–94.
Xie, Q., R. Whisnant, and C. Nathan. 1993. Promoter of the mouse gene encoding calcium-independent nitric oxide synthase confers inducibility by interferon gamma and bacterial lipopolysaccharide. The Journal of Experimental Medicine 177 (6): 1779–1784.
Marks-Konczalik, J., S.C. Chu, and J. Moss. 1998. Cytokine-mediated transcriptional induction of the human inducible nitric oxide synthase gene requires both activator protein 1 and nuclear factor kappaB-binding sites. The Journal of Biological Chemistry 273 (35): 22201–22208.
Vane, J.R., J.A. Mitchell, I. Appleton, A. Tomlinson, D. Bishop-Bailey, J. Croxtall, and D.A. Willoughby. 1994. Inducible isoforms of cyclooxygenase and nitric-oxide synthase in inflammation. Proceedings of the National Academy of Sciences of the United States of America 91 (6): 2046–2050.
Libby, P. 2006. Inflammation and cardiovascular disease mechanisms. The American Journal of Clinical Nutrition 83 (2): 456S–460S.
Solinas, G., F. Marchesi, C. Garlanda, A. Mantovani, and P. Allavena. 2010. Inflammation-mediated promotion of invasion and metastasis. Cancer Metastasis Reviews 29 (2): 243–248.
Jean-Gilles, D., L. Li, H. Ma, T. Yuan, C.O. Chichester III, and N.P. Seeram. 2012. Anti-inflammatory effects of polyphenolic-enriched red raspberry extract in an antigen-induced arthritis rat model. Journal of Agricultural and Food Chemistry 60 (23): 5755–5762.
Ivashkiv, L.B. 2011. Inflammatory signaling in macrophages: transitions from acute to tolerant and alternative activation states. European Journal of Immunology 41 (9): 2477–2481.
Pan, M.H., H.M. Hong, C.L. Lin, A.Z. Jhang, J.H. Tsai, V. Badmaev, K. Nagabhushanam, C.T. Ho, and W.J. Chen. 2011. Se-methylselenocysteine inhibits lipopolysaccharide-induced NF-kappaB activation and iNOS induction in RAW 264.7 murine macrophages. Molecular Nutrition & Food Research 55 (5): 723–732.
Alvira, C.M. 2014. Nuclear factor-kappa-B signaling in lung development and disease: one pathway, numerous functions. Birth Defects Research. Part A, Clinical and Molecular Teratology 100 (3): 202–216.
Barnes, P.J., and M. Karin. 1997. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. The New England Journal of Medicine 336 (15): 1066–1071.
Vanden Berghe, W., et al. 1998. p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways are required for nuclear factor-kappaB p65 transactivation mediated by tumor necrosis factor. The Journal of Biological Chemistry 273 (6): 3285–3290.
Chen, H.G., K.L. Xie, H.Z. Han, W.N. Wang, D.Q. Liu, G.L. Wang, and Y.H. Yu. 2013. Heme oxygenase-1 mediates the anti-inflammatory effect of molecular hydrogen in LPS-stimulated RAW 264.7 macrophages. International Journal of Surgery 11 (10): 1060–1066.
Lee, J.W., C.J. Bae, Y.J. Choi, S.I. Kim, Y.S. Kwon, H.J. Lee, S.S. Kim, and W. Chun. 2014. 3,4,5-trihydroxycinnamic acid inhibits lipopolysaccharide (LPS)-induced inflammation by Nrf2 activation in vitro and improves survival of mice in LPS-induced endotoxemia model in vivo. Molecular and Cellular Biochemistry 390 (1-2): 143–153.
Otterbein, L.E., F.H. Bach, J. Alam, M. Soares, H. Tao Lu, M. Wysk, R.J. Davis, R.A. Flavell, and A.M.K. Choi. 2000. Carbon monoxide has anti-inflammatory effects involving the mitogen-activated protein kinase pathway. Nature Medicine 6 (4): 422–428.
Wiesel, P., L.C. Foster, A. Pellacani, M.D. Layne, C.M. Hsieh, G.S. Huggins, P. Strauss, S.F. Yet, and M.A. Perrella. 2000. Thioredoxin facilitates the induction of heme oxygenase-1 in response to inflammatory mediators. The Journal of Biological Chemistry 275 (32): 24840–24846.
Suh, G.Y., Y. Jin, A.K. Yi, X.M. Wang, and A.M.K. Choi. 2006. CCAAT/enhancer-binding protein mediates carbon monoxide-induced suppression of cyclooxygenase-2. American Journal of Respiratory Cell and Molecular Biology 35 (2): 220–226.
Oh, G.S., H.O. Pae, B.S. Lee, B.N. Kim, J.M. Kim, H.R. Kim, S.B. Jeon, W.K. Jeon, H.J. Chae, and H.T. Chung. 2006. Hydrogen sulfide inhibits nitric oxide production and nuclear factor-kappaB via heme oxygenase-1 expression in RAW264.7 macrophages stimulated with lipopolysaccharide. Free Radical Biology & Medicine 41 (1): 106–119.
Nguyen, T., P. Nioi, and C.B. Pickett. 2009. The Nrf2-antioxidant response element signaling pathway and its activation by oxidative stress. The Journal of Biological Chemistry 284 (20): 13291–13295.
Heo, S.J., S.H. Cha, K.N. Kim, S.H. Lee, G. Ahn, D.H. Kang, C. Oh, Y.U. Choi, A. Affan, D. Kim, and Y.J. Jeon. 2012. Neuroprotective effect of phlorotannin isolated from Ishige okamurae against H(2)O(2)-induced oxidative stress in murine hippocampal neuronal cells, HT22. Applied Biochemistry and Biotechnology 166 (6): 1520–1532.
Park, B.G., W.S. Shin, Y. Um, S. Cho, G.M. Park, D.S. Yeon, S.C. Kwon, J. Ham, B.W. Choi, and S. Lee. 2008. Selective vasodilatation effect of sargahydroquinoic acid, an active constituent of Sargassum micracanthum, on the basilar arteries of rabbits. Bioorganic & Medicinal Chemistry Letters 18 (8): 2624–2627.
Jeon, Y., Y. Jung, M.C. Kim, H.C. Kwon, K.S. Kang, Y.K. Kim, and S.N. Kim. 2014. Sargahydroquinoic acid inhibits TNFalpha-induced AP-1 and NF-kappaB signaling in HaCaT cells through PPARalpha activation. Biochemical and Biophysical Research Communications 450 (4): 1553–1559.
Joung, E.-J., W.G. Gwon, T. Shin, B.M. Jung, J.S. Choi, and H.R. Kim. 2017. Anti-inflammatory action of the ethanolic extract from Sargassum serratifolium on lipopolysaccharide-stimulated mouse peritoneal macrophages and identification of active components. Journal of Applied Phycology 29 (1): 563–573.
Lim, S., et al., Evaluation of antioxidant activities of various solvent extract from Sargassum serratifolium and its major antioxidant components. 2019. 278: p. 178-184.
Joung, E.J., B. Lee, W.G. Gwon, T. Shin, B.M. Jung, N.Y. Yoon, J.S. Choi, C.W. Oh, and H.R. Kim. 2015. Sargaquinoic acid attenuates inflammatory responses by regulating NF-kappaB and Nrf2 pathways in lipopolysaccharide-stimulated RAW 264.7 cells. International Immunopharmacology 29 (2): 693–700.
Gwon, W.-G., E.J. Joung, T. Shin, T. Utsuki, N. Wakamatsu, and H.R. Kim. 2018. Meroterpinoid-rich fraction of the ethanol extract from Sargassum serratifolium suppresses TNF-α-induced monocytes adhesion to vascular endothelium and vascular inflammation in high cholesterol-fed C57BL/6J mice. Journal of Functional Foods 46: 384–393.
Wang, W., P. Liu, C. Hao, L. Wu, W. Wan, and X. Mao. 2017. Neoagaro-oligosaccharide monomers inhibit inflammation in LPS-stimulated macrophages through suppression of MAPK and NF-kappaB pathways. Scientific Reports 7: 44252.
Joung, E.J., M.S. Lee, J.W. Choi, J.S. Kim, T. Shin, B.M. Jung, J.I. Kim, and H.R. Kim. 2012. Anti-inflammatory effects of phlorofucofuroeckol B-rich ethyl acetate fraction obtained from Myagropsis myagroides on lipopolysaccharide-stimulated RAW 264.7 cells and mouse edema. International Immunopharmacology 14 (4): 471–480.
Norberg, J.K., E. Sells, H.H. Chang, S.R. Alla, S. Zhang, and E.J. Meuillet. 2013. Targeting inflammation: multiple innovative ways to reduce prostaglandin E(2). Pharm Pat Anal 2 (2): 265–288.
Niu, X., Q. Mu, W. Li, H. Yao, H. Li, and H. Huang. 2014. Esculentic acid, a novel and selective COX-2 inhibitor with anti-inflammatory effect in vivo and in vitro. European Journal of Pharmacology 740: 532–538.
Hanada, T., and A. Yoshimura. 2002. Regulation of cytokine signaling and inflammation. Cytokine & Growth Factor Reviews 13 (4-5): 413–421.
Packard, R.R., and P. Libby. 2008. Inflammation in atherosclerosis: from vascular biology to biomarker discovery and risk prediction. Clinical Chemistry 54 (1): 24–38.
Karin, M., and A. Lin. 2002. NF-kappaB at the crossroads of life and death. Nature Immunology 3 (3): 221–227.
Li, Q., and I.M. Verma. 2002. NF-kappaB regulation in the immune system. Nature Reviews. Immunology 2 (10): 725–734.
Kanarek, N., and Y. Ben-Neriah. 2012. Regulation of NF-kappaB by ubiquitination and degradation of the IkappaBs. Immunological Reviews 246 (1): 77–94.
Karin, M., and M. Delhase. 2000. The I kappa B kinase (IKK) and NF-kappa B: key elements of proinflammatory signalling. Seminars in Immunology 12 (1): 85–98.
Kundu, J.K., Y.K. Shin, and Y.J. Surh. 2006. Resveratrol modulates phorbol ester-induced pro-inflammatory signal transduction pathways in mouse skin in vivo: NF-kappaB and AP-1 as prime targets. Biochemical Pharmacology 72 (11): 1506–1515.
Ryter, S.W., and A.M. Choi. 2016. Targeting heme oxygenase-1 and carbon monoxide for therapeutic modulation of inflammation. Translational Research 167 (1): 7–34.
Paine, A., B. Eiz-Vesper, R. Blasczyk, and S. Immenschuh. 2010. Signaling to heme oxygenase-1 and its anti-inflammatory therapeutic potential. Biochemical Pharmacology 80 (12): 1895–1903.
Lee, I.S., J. Lim, J. Gal, J.C. Kang, H.J. Kim, B.Y. Kang, and H.J. Choi. 2011. Anti-inflammatory activity of xanthohumol involves heme oxygenase-1 induction via NRF2-ARE signaling in microglial BV2 cells. Neurochemistry International 58 (2): 153–160.
Qin, S., and D.X. Hou. 2016. Multiple regulations of Keap1/Nrf2 system by dietary phytochemicals. Molecular Nutrition & Food Research 60 (8): 1731–1755.
Wu, W., Y. Li, Y. Wu, Y. Zhang, Z. Wang, and X. Liu. 2015. Lutein suppresses inflammatory responses through Nrf2 activation and NF-kappaB inactivation in lipopolysaccharide-stimulated BV-2 microglia. Molecular Nutrition & Food Research 59 (9): 1663–1673.
Wardyn, J.D., A.H. Ponsford, and C.M. Sanderson. 2015. Dissecting molecular cross-talk between Nrf2 and NF-kappaB response pathways. Biochemical Society Transactions 43 (4): 621–626.
Buelna-Chontal, M., and C. Zazueta. 2013. Redox activation of Nrf2 & NF-kappaB: a double end sword? Cellular Signalling 25 (12): 2548–2557.
Bonizzi, G., and M. Karin. 2004. The two NF-kappaB activation pathways and their role in innate and adaptive immunity. Trends in Immunology 25 (6): 280–288.
de Vries, H.E., M. Witte, D. Hondius, A.J.M. Rozemuller, B. Drukarch, J. Hoozemans, and J. van Horssen. 2008. Nrf2-induced antioxidant protection: a promising target to counteract ROS-mediated damage in neurodegenerative disease? Free Radical Biology & Medicine 45 (10): 1375–1383.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2019R1I1A3A0105969012).
Author information
Authors and Affiliations
Contributions
E.J., L.C., B.L., W.G., S.P., and H.K. conceived and planned the experiments. E.J. and W.G. performed the experiments and analyzed the data. L.C., B.L., and S.P were major contributors in writing the manuscript. H.K. supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The authors confirm that any aspect of the work covered in this manuscript that has involved experimental animals has been conducted with approvals by the Animal Ethics Committee of the Pukyong National University.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 196 kb)
Rights and permissions
About this article
Cite this article
Joung, EJ., Cao, L., Lee, B. et al. Sargahydroquinoic Acid, a Cyclooxygenase-2 Inhibitor, Attenuates Inflammatory Responses by Regulating NF-κB Inactivation and Nrf2 Activation in Lipopolysaccharide-Stimulated Cells. Inflammation 44, 2120–2131 (2021). https://doi.org/10.1007/s10753-021-01488-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-021-01488-x