Abstract
Endoplasmic reticulum stress is an important contributor to the cerebral ischemic injury. Sappanone A (SA), a kind of natural homoisoflavanone extracted from Caesalpinia sappan L, has been evidenced to exhibit anti-inflammatory and antioxidative properties. The present study aimed to investigate the potential neuroprotective effects of SA in cerebral ischemia-reperfusion injury. The potential neuroprotective effect of SA was tested in a rat model of middle cerebral artery occlusion (MCAO) allowing reperfusion and PC12 cell model of oxygen-glucose deprivation and reperfusion (OGD/R). Post-ischemic neuronal injury was evaluated by 2, 3, 5-triphenyltetrazolium chloride (TTC) and hematoxylin-eosin (H&E) staining. The levels of inflammatory factors and oxidative stress-related markers were detected using corresponding kits. Cell apoptosis was evaluated by terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) or flow cytometry, and the expression of apoptosis-associated proteins was determined using western blot analysis. Subsequently, endoplasmic reticulum stress-related proteins were detected through western blot analysis, and CCAAT/enhancer binding protein (C/EBP) homologous protein (CHOP) was overexpressed to confirm the contribution of endoplasmic reticulum stress inhibition by SA to the neuroprotective effects post OGD/R. Results revealed that SA was effective in ameliorating cerebral infarction and pathological injuries post-reperfusion following MCAO, which is associated with reduced inflammation, oxidative stress, and cell apoptosis by SA in the brain. Consistently, these neuroprotective effects of SA post ischemia-reperfusion were also observed in a PC12 cell model of OGD/R. Importantly, endoplasmic reticulum stressors, including the CHOP, the 78 kDa glucose-regulated protein 78 (GRP78), and phosphorylated eukaryotic initiation factors 2α (EIF-2α), were significantly downregulated by SA, while CHOP overexpression attenuated the beneficial effects of SA on inflammation, oxidative stress, and apoptosis in OGD/R-induced PC12 cells. These results demonstrated that SA alleviates endoplasmic reticulum stress, ameliorating inflammation, oxidative stress, and apoptosis, and thereby serves as therapeutic potential for protection against cerebral ischemia-reperfusion injury in ischemic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Ischemia, the most common form of stroke, is of high morbidity and mortality, bringing great burden to families and the society. Cerebral ischemia-reperfusion generally and irreversibly impairs brain functions by partly interrupting blood supply to the brain and resulting in thrombosis, embolism, or hypoperfusion, causing millions of deaths or disabilities every year [1, 2]. However, there has been, to date, an unfortunate lack of effective treatments for cerebral ischemic stroke.
Neuroinflammation and oxidative stress, generally occurring during ischemic stroke, are two well-known factors which induce neuronal injury and apoptosis [3]. Chinese herbs hold great potential for treating neurobiological disorders, including ischemic stroke. Sappanone A (SA) is a homoisoflavanone and a major extract from Caesalpinia sappan L, which has been evidenced to exert anti-inflammatory, antioxidative and anti-apoptotic effects against myocardial ischemia-reperfusion injury [4]. Accumulating evidence shows that inflammation, oxidative stress, and cell apoptosis are common features of endoplasmic reticulum (ER) stress, which is also a major pathology in the cerebral ischemia-reperfusion injury [5, 6]. It remains to be elucidated whether and how SA is effective in ameliorating the ER stress in the cerebral ischemic stroke.
It has been reported that the CCAAT/enhancer binding protein (C/EBP) homologous protein (CHOP), 78 kDa glucose-regulated protein 78 (GRP78), a multifunctional protein belonging to the huge HSP70 family of molecular chaperones, eukaryotic initiation factor 2 alpha (EIF-2α), and the downstream target of the eIF2α phosphorylation are marker proteins of ER stress [7,8,9]. Furthermore, these proteins have been evidenced to be regulated by nuclear erythroid 2-related factor 2 (Nrf2), a master regulator of the body’s antioxidant response which can be modulated by SA via the PKC or PI3K pathway [10]. In the present study, we sought to examine the potential protective effects of SA on middle cerebral artery occlusion (MCAO)-reperfusion rats and oxygen-glucose deprivation and reperfusion (OGD/R)-induced PC12 cells, as well as their underlying mechanisms. Our findings may identify a novel pharmaceutical approach to the treatment of cerebral ischemia-reperfusion injury.
MATERIALS AND METHODS
Animals
A total of 50 SPF-grade male Sprague-Dawley (SD) rats (200–250 g) were provided by Shanghai Slac Animal Laboratory (Shanghai, China). All rats were housed under standard conditions with 12-h light/dark cycle, food and water ad libitum. All animal experiments were approved by the Animal Care and Use Committee of Huashan Hospital Affiliated to Fudan University.
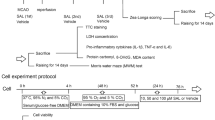
Grouping and Drug Treatment
Animals were randomly assigned into five groups (n = 10 in each group): control, MCAO, MCAO plus SA-10 (MCAO+SA 10 mg/kg), MCAO plus SA-20 (MCAO+SA 20 mg/kg), and MCAO plus SA-40 (MCAO+SA 10 mg/kg). SA (CAS No. 102067-84-5) was purchased from ChemFaces (Wuhan, China) and dissolved in DMSO (Sigma-Aldrich, St. Louis, MO, USA). SA was injected intraperitoneally every day, consecutively for 3 days. Rats in the control group received the same volume of saline (containing 0.1% DMSO). At 2 h after the last administration of drugs, the MCAO surgery was performed.
Establishment of MCAO-Reperfusion Rat Model
Reversible MCAO surgery was performed using an improved Longa-Zea method [11] 2 h after the administration of SA or vehicle. In brief, rats were anesthetized with 1% pentobarbital sodium and fixed in a supine position. Both the proximal ends of common carotid artery and external carotid artery were ligated, and the internal carotid artery was clamped temporarily. A V-shaped oblique incision was made at the bifurcation of external carotid and internal carotid arteries with vascular scissors. Then, the artery clamp was reopened while inserting a paraffin bolt through the external carotid artery stump into the internal carotid artery until a slight resistance was felt. The time was set as the beginning of embolism. The upper end of the common carotid artery was then ligated. Finally, the paraffin bolt was gently pulled back to the incision of external carotid artery 90 min after embolism to get the reperfusion, and ischemia-reperfusion injuries were evaluated 24 h later.
2, 3, 5-Triphenyltetrazolium Chloride Staining
Rats were anesthetized with overdose of 1% sodium pentobarbitone. Brains were removed, washed with saline 24-h post ischemia-reperfusion and then frozen under − 20 °C. Coronal slices of 2-mm intervals were obtained; brain sections were immersed in 1% TTC in PBS at 37 °C for 20 min, and then fixed in 4% paraformaldehyde for 6 h at 4 °C. The presence of infarction was determined by examining the areas stained without TTC. The area of cerebral infarction was qualified using the Image J software (National Institutes of Health, Bethesda, MA, USA).
Hematoxylin-Eosin Staining
Appropriate weight brain tissues were immersed in 4% paraformaldehyde for 24 h and embedded in paraffin. Subsequently, the sections were deparaffinized with graded ethanol together with xylene, and 4-μm sections were prepared for hematoxylin-eosin staining. After being dehydrated with graded ethanol and xylene, the histological structure of brain tract was observed under a light microscope (Olympus Corporation).
Measurement of Inflammatory Factors
Blood was harvested on ice and then centrifuged at 12,000g for 10 min to obtain the serum. The supernatants were collected for the detection of inflammatory factors, including the tumor necrosis factor-α (TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6) using enzyme-linked immunosorbent assay (ELISA) kits based on the manufacturer’s protocols. Abovementioned kits were purchased from Shanghai Xitang Biotechnology Co., Ltd. (Shanghai, China).
Evaluation of Oxidative Stress-Related Markers
The brain tissues were obtained at the end of reperfusion, which were then cut into small pieces. These pieces were homogenized with RIPA lysis buffer, centrifuged at 12,000g for 10 min, and the supernatant was collected. The contents of reactive oxygen species (ROS) and malondialdehyde (MDA) as well as the activity of superoxide dismutase (SOD) in tissue homogenate supernatant or culture supernatant were detected using corresponding commercial kits (Nanjing Jiancheng Bioengineering Institute; Nanjing, China) in accordance with the specification provided by the supplier.
Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling Staining
The TUNEL staining was performed to evaluate cell apoptosis post ischemia-reperfusion in the hippocampus using a commercial kit labeling DNA strand breaks with FITC (Beyotime, China) according to the manufacturer’s instruction. Each section was observed under a light microscope and images were captured. The nuclei of healthy cells were stained blue, whereas those in apoptotic cells presented green staining which were identified as TUNEL-positive cells.
Cell Culture
PC12 cell line was obtained from the Cell Bank of the Chinese Academy of Sciences (Shanghai, China). Cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Gibco) supplemented with 10% FBS (Gibco) under environmental conditions of 37 °C and 5% CO2.
OGD/R and Treatment
For OGD/R, PC12 cells were washed with PBS and then transferred into a hypoxia chamber (Thermo Scientific) with 1% oxygen, 94% N2. and 5% CO2 for 2 h, after which the cells were transferred back to the standard culturing system and maintained for 24 h [12]. In the control group, cells were incubated under normoxic conditions all the time. For cultured PC12 cells, SA was employed to pretreat cells at 10 μM, 20 μM, and 30 μM for 24 h before OGD/R or normoxic manipulations.
Cell Transfection
Prior to transfection, 1 × 106 of PC12 cells were seeded into a 6-well plate. The cell monolayer was ~ 80% confluent at the time of transfection. Plasmids used for CHOP overexpression was constructed by GenePharma (Shanghai, China), and empty plasmid carrying no CHOP pcDNA was used as control. Transfection experiments were conducted using Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) according to the standard protocol. The transfection efficiency was evaluated by reverse transcription-quantitative polymerase chain reaction (RT-qPCR) and western blot analysis at 24-h post-transfection.
Cell Counting Kit-8 (CCK-8) Assay
Cell suspension was dispensed into 5000 cells/well. A total of 10 μL CCK-8 solution was added into each well, and the cell plate was then incubated for 2 h. The absorbance at 450 nm was measured using a microplate reader (BioTek-Synergy2).
Flow Cytometry
Cultured cells were harvested, digested with 0.05% trypsin in the PBS, and then collected for centrifugation at 4 °C. The bullets were collected and re-suspended in a binding buffer containing 1% Annexin V-FITC and 1% propidium iodide. Cells were then incubated in the dark. Lastly, fluorescent intensity was measured using flow cytometry (Accuri C6, BD).
RT-qPCR Analysis
Total RNA was extracted from rat brains or cultured cells using TRIzol reagent (Life Technologies, Carlsbad, CA). Subsequently, the total RNA was reversely transcribed into cDNA using a reverse transcription kit (Beijing TransGen Biotech, Beijing, China). qPCR was performed using iTaq™ Universal SYBR® Green Supermix (Bio-Rad Laboratories, Inc.) on an ABI 7500 instrument (Applied Biosystems; Foster City, CA, USA). Data was normalized by the expression level of GAPDH, a house-keeping gene. Gene expression was analyzed using the 2−△△Ct.
Western Blotting
Rat brains were removed, and the hippocampus and cortex tissues were isolated on ice for experiments. Cultured cells were harvested 1 h after OGD/R. Samples were homogenized with RIPA lysis buffer and then centrifuged at 4 °C, 12,000 rpm for 30 min. The supernatant was collected and mixed with the loading buffer. Proteins were separated in SDS-PAGE and then transferred onto nitrocellulose membranes (Merck Millipore). The membranes were then blocked with 5% non-fat milk for 1.5 h, and then incubated with primaries and secondary antibodies. The immunoreactive protein bands were visualized by the Odyssey Infrared Imaging System (LI-COR Biosciences) and analyzed using the ImageJ software.
Statistical Analysis
Data were presented as means ± standard deviation, analyzed or plotted using GraphPad Prism 8.0. Quantitative, and were compared using the Student’s t test or one-way analysis of variance (ANOVA) followed by Turkey’s post hoc test. A value of p less than 0.05 was considered statistically significant.
RESULTS
SA Decrease Cerebral Ischemic Area and Relieves Brain Injury in Rats Post MCAO-Reperfusion
To test the potential neuroprotective effect of SA in vivo on cerebral ischemic stroke, different doses of SA, i.e., 10 mg/kg, 20 mg/kg, and 40 mg/kg, respectively, were administrated intraperitoneally 1 h prior to MCAO. It was found that MCAO prominently induced cerebral ischemia compared with the control group, while SA significantly decreased the ischemic area and brain tissue injury in a dose-dependent way in comparison with the model group, as revealed by TTC staining (Fig. 1a and b) and H&E staining (Fig. 1c). These data indicated a neuroprotective role of SA in MCAO-reperfusion injury.
SA decreased cerebral ischemic area and relieved brain injury in rats post MCAO-reperfusion. a TTC staining was used to evaluate the volume of the cerebral infarction. b The percentage of infarct volume was calculated. ***p < 0.001 vs. control; ###p < 0.001 vs. MCAO. c The pathologic changes of brain tissues were assessed using H&E staining.
SA Alleviates Neuroinflammation, Oxidative Stress, and Cell Apoptosis Induced by MCAO-Reperfusion
Subsequently, we examined whether SA is effective in regulating inflammation and oxidative stress in rats with MCAO. As displayed in Fig. 2a–c, the levels of inflammatory factors, including the TNF-α, IL-1β, and IL-6, were notably elevated compared with the control group, which were dose-dependently reduced following SA treatment in contrast to rats in the model group. Consistently, SA ameliorated oxidative stress in rats with cerebral ischemia-reperfusion injury, as indicated by decreased levels of both ROS and MDA and increased activity of SOD antioxidant enzyme in dose-dependent ways (Fig. 2d–f). To study the effects of SA on cell apoptosis post MCAO-reperfusion, TUNEL staining was employed to evaluate the rat brain slices. As shown in Fig. 3a, a large number of neurons underwent apoptosis following MCAO-reperfusion compared to the control. Noticeably, SA administration dose-dependently rescued the number of apoptotic cells in brain tissues of rats with MCAO-reperfusion injury. Meanwhile, the expression of anti-apoptotic protein Bcl-2 was markedly downregulated, accompanied by upregulated expression of apoptotic proteins including Bax and cleaved caspase-3 in the MCAO group in comparison with the control group, which was reversed by SA intervention (Fig. 3b). Taken together, these results evidenced that SA significantly ameliorated the neuroinflammation, oxidative stress, and cell apoptosis in rat following cerebral ischemic stroke.
SA alleviates neuroinflammation and oxidative stress in rat induced by MCAO-reperfusion. a, b, c The contents of TNF-α, IL-1β, and IL-6 in serum were determined by ELISA kits. d, e, f ROS and MDA levels as well as SOD activity in brain tissues were examined by commercially available kits. ***p < 0.001 vs. control; #p < 0.05, ###p < 0.001 vs. MCAO.
SA Attenuates ER Stress in Rat Following MCAO-Reperfusion Injury
ER stress is a major cause of neuronal injury in the ischemia-reperfusion process. Since inflammation and oxidative stress are general characters of ER stress, we next explored how SA regulated ER stress post MCAO-reperfusion. The expression of two ER stress markers CHOP and GRP87 was remarkably increased in the MCAO group, which was dose-dependently reversed by SA treatment (Fig. 4). Besides, though the total level of another ER stress marker EIF-2α was not changed by neither MCAO nor SA, its phosphorylation was prominently upregulated by MCAO but downregulated following SA administration (Fig. 4). These data together suggest that SA is effective in alleviating ER stress post MCAO-reperfusion.
CHOP Overexpression Abolishes the Neuroprotective Effect of SA in OGD/R-Induced PC12 cells
To test whether the neuroprotective effect of SA against cerebral ischemic stroke is dependent on its anti-ER stress function, we upregulated ER stress by overexpressing CHOP in an in vitro model of ischemia-reperfusion injury in PC12 cells. It was found that OGD/R induction decreased the viability of PC12 cells compared with the control group, which was partly and dose-dependently rescued by SA administration 2 h prior to OGD/R (Fig. 5a). Consistent with in vivo results, OGD/R enhanced the expression levels of CHOP, GRP78, and phospho-EIF1α, while prior administration of SA dose-dependently downregulated those proteins (Fig. 5b), indicating the alleviation of ER stress by SA in OGD/R. Importantly, with the overexpression of CHOP with plasmid (Fig. 5c and d), the effects of SA in decreasing inflammatory factors, including TNF-α, IL-1β, and IL-6, in OGD/R were abolished compared to the empty vector group (Fig. 5e–g). Similarly, the antioxidative effect of SA in OGD/R was also hindered by CHOP overexpression, as indicated by increased levels of ROS and MDA, and decreased activity of SOD antioxidant enzyme in OGD/R cells compared with the vector control group (Fig. 5h–j). Moreover, prominent cell apoptosis resulting from OGR/R was significantly ameliorated by SA in a dose-dependently manner, as shown by decreased apoptotic cells measured by flow cytometry (Fig. 6a and b) and downregulated expression of pro-apoptosis proteins, Bax and cleaved caspase-3, as well as upregulated expression of anti-apoptotic protein Bcl-2 (Fig. 6c). However, CHOP overexpression significantly inhibited the effect of SA on OGD/R-induced cell apoptosis. To sum up, these findings suggest that the beneficial effect of SA in ameliorating inflammation, oxidative stress, and apoptosis in ischemic stroke was at least partly dependent on its function of alleviating ER stress.
CHOP overexpression abolished the protective effect of SA on inflammation and oxidative stress in OGD/R-induced PC12 cells. a Cell viability was evaluated using a CCK-8 kit. b Western blot analysis was employed to examine the expression of ER-related proteins. ***p < 0.001 vs. control; ##p < 0.01, ###p < 0.001 vs. OGD/R. c and d The expression of CHOP was determined using RT-qPCR and western blot analysis, respectively. **p < 0.01, ***p < 0.001 vs. Oe-NC. e, f, g The contents of inflammatory factors including TNF-α, IL-1β, and IL-6 were detected using corresponding ELISA kits. h, i, j The levels of ROS and MDA as well as the activity of SOD were determined using commercially available kits. ***p < 0.001 vs. control; #p < 0.05, ##p < 0.01, ###p < 0.001 vs. OGD/R; △△△p < 0.001 vs. OGD/R + SA-30 μM + Oe-NC.
CHOP overexpression reversed the protective effect of SA on apoptosis in OGD/R-induced PC12 cells. a and b Cell apoptosis was detected using flow cytometry. c The expression of apoptosis-related proteins was examined using western blot analysis. ***p < 0.001 vs. control; #p < 0.05, ###p < 0.001 vs. OGD/R; △△△p < 0.001 vs. OGD/R + SA-30 μM + Oe-NC.
DISCUSSION
The treatment for neuronal injuries induced by cerebral ischemia-reperfusion remains a challenge in clinic, to date. Blood vessel recanalization is not effective in restoring brain function since the process of ischemia-reperfusion has been evidenced to induce prominent neuroinflammation and oxidative stress [13, 14], both of which are unfavorable for neuronal survival and neural circuits repairing in ischemic stroke [3]. In recent years, natural extracts from herbs have gained increasing interest for their therapeutic potentials in protecting the neuronal injury against the cerebral ischemic stroke [5, 15,16,17]. Here, we demonstrated that SA, a major extract from Caesalpinia sappan L, is effective in ameliorating neuronal damages in the process of cerebral ischemic-reperfusion by inhibiting ER stress.
In fact, neuroinflammation is a common feature in cerebral ischemic stroke [3, 18]. Calming inflammation has long been selected as an effective strategy for the prevention and treatment of neuronal injury in stroke [19, 20]. SA has been evidenced to inhibit the production of nitric oxide and pro-inflammatory factors in lipopolysaccharide-induced inflammation and mortality, via modulation of Nrf2 and NF-κB signaling [21]. Similarly, SA was also reported to prevent the inflammation-mediated bone loss and inhibit RANKL-induced osteoclastogenesis in mouse bone marrow macrophages [22]. In the present study, we found an anti-inflammation role of SA in cerebral ischemia and reperfusion.
Moreover, we also observed an effect of SA on another feature causing neuronal injury in the process cerebral ischemia-reperfusion, i.e., oxidative stress. In combination with neuroinflammation, ROS is generated during the oxidative stress, leading to neuronal damages in ischemic stroke [23]. Antioxidative agents have been tested in preclinical and clinical studies for their potential in treating neuronal injuries caused by ischemia-reperfusion [24]. SA was recently reported to be effective in preventing oxidative responses in myocardial ischemia-reperfusion injury, thus protecting brain functions, via coordinating cellular antioxidant defenses and maintaining redox balance by modulating Nrf2 signaling through the PKC or PI3K pathway [10]. Another study also found an antioxidative role of SA in the hypoxia/reoxygenation-induced cardiomyocyte injury by suppressing mitochondrial apoptosis and inhibiting the PI3K signaling pathway [4]. Consistent with these findings, we found here that SA reduced the production of ROS and MDA, while increasing SOD in the cerebral ischemia-reperfusion.
Both neuroinflammation and oxidative stress are inducing factors of cell apoptosis, which results in brain damage and eventually leads to disability or mortality. An anti-apoptotic benefit of SA has been reported against hypoxia, via downregulating miR-15a and activating the Wnt-β-catenin and PI3K-AKT pathways [25]. Indeed, we found that SA dose-dependently facilitated cell survival both in vivo and in vitro in ischemic stroke.
Inflammation, oxidative stress, and cell apoptosis are common features of ER stress [26], which are well-known to be associated with neuronal damages in the process of ischemic-reperfusion injury [27, 28]. We found in the present study that the neuroprotective effect of SA on ischemic stroke was dependent on its action of alleviating the ER stress. Interestingly, SA inhibited the elevation of inflammatory factors through modulating Nrf2 signaling [10, 21], while Nrf2 has been evidenced to further regulate the expression and functions of both CHOP and GRP87 [29, 30], two key effectors and maker proteins indicating the ER stress [31]. Although whether and how Nrf2 regulates the phosphorylation of EIF-2α, another ER stressor [8], remain to be elucidated, we did find that prior administration of SA downregulated the level of CHOP, GRP78, and phospho-EIF-2α. Importantly, enhancing ER stress by overexpression of CHOP significantly abolished the neuroprotective efficiency against ischemic stroke, suggesting that SA inhibits inflammation, oxidative stress, and cell apoptosis via inhibiting ER stress.
In conclusion, findings in the present study demonstrate that SA exerts anti-neuroinflammatory, antioxidative, and anti-apoptotic effects during cerebral ischemia-reperfusion injury through ameliorating ER stress. These data indicate a therapeutic potential of SA in cerebral ischemic stroke.
Data availability
All data present in the paper is available for reasonable request to the corresponding author.
References
Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018. 392(10159):1736-88.
Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018. 392(10159):1684-735.
Esenwa, C.C., and M.S. Elkind. 2016. Inflammatory risk factors, biomarkers and associated therapy in ischaemic stroke. Nat Rev Neurol. 12 (10): 594–604.
Shi X, Tao G, Ji L, Tian G. Sappanone A alleviates hypoxia/reoxygenation-induced cardiomyocytes injury through inhibition of mitochondrial apoptosis and activation of PI3K-Akt-Gsk-3beta pathway. Biosci Rep. 2020. 40(2).
Gong, D.J., L. Wang, Y.Y. Yang, J.J. Zhang, and X.H. Liu. 2019. Diabetes aggravates renal ischemia and reperfusion injury in rats by exacerbating oxidative stress, inflammation, and apoptosis. Ren Fail. 41 (1): 750–761.
Xu, B., Y. Qin, D. Li, N. Cai, J. Wu, L. Jiang, L. Jie, Z. Zhou, J. Xu, and H. Wang. 2020. Inhibition of PDE4 protects neurons against oxygen-glucose deprivation-induced endoplasmic reticulum stress through activation of the Nrf-2/HO-1 pathway. Redox Biol. 28: 101342.
Han, J., R. Murthy, B. Wood, B. Song, S. Wang, B. Sun, H. Malhi, and R.J. Kaufman. 2013. ER stress signalling through eIF2alpha and CHOP, but not IRE1alpha, attenuates adipogenesis in mice. Diabetologia. 56 (4): 911–924.
Leitman, J., B. Barak, R. Benyair, M. Shenkman, U. Ashery, F.U. Hartl, and G.Z. Lederkremer. 2014. ER stress-induced eIF2-alpha phosphorylation underlies sensitivity of striatal neurons to pathogenic huntingtin. Plos One. 9 (3): e90803.
Chern, Y.J., J. Wong, G. Cheng, A. Yu, Y. Yin, D.F. Schaeffer, et al. 2019. The interaction between SPARC and GRP78 interferes with ER stress signaling and potentiates apoptosis via PERK/eIF2alpha and IRE1alpha/XBP-1 in colorectal cancer. Cell Death Dis. 10 (7): 504.
Shi, X., G. Tao, L. Ji, and G. Tian. 2020. Sappanone A protects against myocardial ischemia reperfusion injury by modulation of Nrf2. Drug Des Devel Ther. 14: 61–71.
Trotman-Lucas, M., M.E. Kelly, J. Janus, and C.L. Gibson. 2019. Middle cerebral artery occlusion allowing reperfusion via common carotid artery repair in mice. J Vis Exp. 143.
Zhu, J.R., Y.F. Tao, S. Lou, and Z.M. Wu. 2010. Protective effects of ginsenoside Rb(3) on oxygen and glucose deprivation-induced ischemic injury in PC12 cells. Acta Pharmacol Sin. 31 (3): 273–280.
Mizuma, A., J.S. You, and M.A. Yenari. 2018. Targeting reperfusion injury in the age of mechanical thrombectomy. Stroke. 49 (7): 1796–1802.
Wood, H. 2018. Selective neuronal loss could limit penumbral rescue after stroke. Nat Rev Neurol. 14 (7): 380–381.
Li X, Ren Z, Wu Z, Fu Z, Xie H, Deng L, et al. Steric effect of antioxidant Diels-Alder-type adducts: a comparison of Sanggenon C with Sanggenon D. Molecules. 2018. 23(10).
Zelova, H., Z. Hanakova, Z. Cermakova, K. Smejkal, A.S. Dall, P. Babula, et al. 2014. Evaluation of anti-inflammatory activity of prenylated substances isolated from Morus alba and Morus nigra. J Nat Prod. 77 (6): 1297–1303.
Martel, J., D.M. Ojcius, C.J. Chang, C.S. Lin, C.C. Lu, Y.F. Ko, S.F. Tseng, H.C. Lai, and J.D. Young. 2017. Anti-obesogenic and antidiabetic effects of plants and mushrooms. Nat Rev Endocrinol. 13 (3): 149–160.
Stoll, G., and B. Nieswandt. 2019. Thrombo-inflammation in acute ischaemic stroke - implications for treatment. Nat Rev Neurol. 15 (8): 473–481.
Flemming, A. 2019. Calming inflammation to prevent stroke damage. Nat Rev Immunol. 19 (8): 473.
Liu, Q., E.M. Johnson, R.K. Lam, Q. Wang, Y.H. Bo, E.N. Wilson, et al. 2019. Peripheral TREM1 responses to brain and intestinal immunogens amplify stroke severity. Nat Immunol. 20 (8): 1023–1034.
Lee, S., S.Y. Choi, Y.Y. Choo, O. Kim, P.T. Tran, C.T. Dao, B.S. Min, and J.H. Lee. 2015. Sappanone A exhibits anti-inflammatory effects via modulation of Nrf2 and NF-kappaB. Int Immunopharmacol. 28 (1): 328–336.
Choo, Y., P.T. Tran, B. Min, O. Kim, H.D. Nguyen, S. Kwon, et al. 2017. Sappanone A inhibits RANKL-induced osteoclastogenesis in BMMs and prevents inflammation-mediated bone loss. Int Immunopharmacol. 52: 230–237.
Rodrigo, R., R. Fernandez-Gajardo, R. Gutierrez, J.M. Matamala, R. Carrasco, A. Miranda-Merchak, and W. Feuerhake. 2013. Oxidative stress and pathophysiology of ischemic stroke: novel therapeutic opportunities. CNS Neurol Disord Drug Targets. 12 (5): 698–714.
Li, P., R.A. Stetler, R.K. Leak, Y. Shi, Y. Li, W. Yu, et al. 2018. Oxidative stress and DNA damage after cerebral ischemia: potential therapeutic targets to repair the genome and improve stroke recovery. Neuropharmacology 134 (Pt B): 208–217.
Kang, C., J. Gao, M. Kang, X. Liu, Y. Fu, and L. Wang. 2019. Sappanone A prevents hypoxia-induced injury in PC12 cells by down-regulation of miR-15a. Int J Biol Macromol. 123: 35–41.
Zeeshan, H.M., G.H. Lee, H.R. Kim, and H.J. Chae. 2016. Endoplasmic reticulum stress and associated ROS. Int J Mol Sci. 17 (3): 327.
Hong, J., K. Kim, J.H. Kim, and Y. Park. 2017. The role of endoplasmic reticulum stress in cardiovascular disease and exercise. Int J Vasc Med. 2017: 2049217.
Xin, Q., B. Ji, B. Cheng, C. Wang, H. Liu, X. Chen, J. Chen, and B. Bai. 2014. Endoplasmic reticulum stress in cerebral ischemia. Neurochem Int. 68: 18–27.
Chang, Y.J., Y.P. Huang, Z.L. Li, and C.H. Chen. 2012. GRP78 knockdown enhances apoptosis via the down-regulation of oxidative stress and Akt pathway after epirubicin treatment in colon cancer DLD-1 cells. Plos One. 7 (4): e35123.
Zong, Z.H., Z.X. Du, N. Li, C. Li, Q. Zhang, B.Q. Liu, et al. 2012. Implication of Nrf2 and ATF4 in differential induction of CHOP by proteasome inhibition in thyroid cancer cells. Biochim Biophys Acta. 1823 (8): 1395–1404.
Dauer, P., N.S. Sharma, V.K. Gupta, B. Durden, R. Hadad, S. Banerjee, V. Dudeja, A. Saluja, and S. Banerjee. 2019. ER stress sensor, glucose regulatory protein 78 (GRP78) regulates redox status in pancreatic cancer thereby maintaining “stemness”. Cell Death Dis. 10 (2): 132.
Author information
Authors and Affiliations
Contributions
Meihua Wang and Zhilin Chen designed this study, performed experiments, and interpreted the data. Lei Yang collected the data, searched the literature, and wrote the manuscript. Lei Ding revised the manuscript. All authors read and approval the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All animal studies were approved by the Animal Care and Use Committee of Huashan Hospital Affiliated to Fudan University.
Consent for publication
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, M., Chen, Z., Yang, L. et al. Sappanone A Protects Against Inflammation, Oxidative Stress and Apoptosis in Cerebral Ischemia-Reperfusion Injury by Alleviating Endoplasmic Reticulum Stress. Inflammation 44, 934–945 (2021). https://doi.org/10.1007/s10753-020-01388-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01388-6