Abstract
Atherosclerosis is a progressive chronic inflammation in the arterial walls. It is believed that the deposition of low-density lipoprotein (LDL) and its damage to endothelial cells play a vital role in atherosclerosis. Oxidized LDL (Ox-LDL) was confirmed to induce endothelial cell pyroptosis which plays an important role in intima inflammation and the development of atherosclerosis, but the underlying molecular mechanism needs to be explored. Here, we showed that ox-LDL upregulated the expression of mixed lineage kinase domain-like (MLKL) protein at both the mRNA and protein levels in endothelial cells, associated with the augment of pro-caspase-1 cleavage, interleukin-1β (IL-1β) maturation, pro-IL-1β production, and lactate dehydrogenase (LDH) release. Overexpression of MLKL substantially aggravated ox-LDL-induced increasing levels of caspase-1, IL-1β, pro-IL-1β, and LDH. MLKL-induced caspase-1 activation and IL-1β maturation were abolished by NLR family, pyrin domain-containing 3 (NLRP3) specific inhibitor MCC950, or extracellular high potassium concentration. Our findings indicated that MLKL is essential for regulation of ox-LDL-induced pyroptosis and inflammation through the activation of NLRP3 inflammasome, and suggested that MLKL could act as potential therapeutic targets to ameliorate atherosclerosis-related diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Coronary atherosclerosis is the basis of most coronary artery disease (CAD) and leads to the development of many other cardiovascular diseases [1]. The pathogenesis of atherosclerosis is complex and still not fully understood. It is now well accepted that atherosclerosis is a chronic inflammatory disease within the vascular walls. It always begins with the damage to the endothelial. After endothelial injury, low-density lipoprotein (LDL) deposits in vascular intima and is modified to oxidized LDL [2, 3]. Ox-LDL can activate endothelial cells, leading to increased expression of adhesion molecules and release of inflammatory cytokines [1, 4].
Pyroptosis is a novel form of programmed necrosis, which is a unique form and mechanism of programmed cell death compared with apoptosis and autophagic cell death [5]. Mechanically, pyroptosis is mainly driven by caspase-1-mediated signaling pathway. In this canonical pyroptosis signaling pathway, pathogen-associated molecular patterns (PAMPs) or danger-associated molecular patterns (DAMPs) are detected by a variety of inflammasomes, such as NLR family and pyrin domain-containing 3 (NLRP3) inflammasome, which can be activated by a range of stimuli. The NLRP3 inflammasome is currently the best characterized inflammasome and consists of NLRP3, apoptosis-associated speck-like protein containing a CARD (ASC), and caspase-1. Upon NLRP3 activation, inactive procaspase-1 cleaves into p20 and p10 subunits that form the active caspase-1, which then leads to maturation and secretion of interleukin-1β (IL-1β) and interleukin-18 (IL-18) [6]. In addition to processing pro-inflammatory cytokines, active caspase-1 further leads to plasma membrane rupture, cytoplasmic swelling, DNA fragmentation, and the release of pro-inflammatory cellular contents [7, 8].
Recent studies have shown that pyroptosis is associated with a variety of cardiovascular diseases [9]. Endothelial cell pyroptosis may lead to a series of downstream events of atherosclerosis. In endothelial cells, the caspase-1-mediated inflammasome pathway senses lipid accumulation and inflammatory mediators, and triggers pyroptosis [10,11,12]. Caspase-1 activation promotes endothelial activation. The expression levels of endothelial cell adhesion molecules were increased, and thus trigger mononuclear cell adhesion [13]. Endothelial cell pyroptosis may lead to reduced endothelial cell quantity and integrity, increasing endothelium permeability, and thus promoting smooth muscle cell migration and deposition [14]. Most importantly, pyroptosis of endothelial cells leads to the release of pro-inflammatory cytokines, such as IL-1β and IL-18, leading to vascular inflammation. As we all know, atherosclerosis is a lipid-driven inflammatory disease of the arterial intima in which the balance of pro-inflammatory and inflammation-resolving mechanisms dictates the final clinical outcome [15]. The role of inflammation caused by pyroptosis in atherosclerosis cannot be ignored.
Mixed lineage kinase domain-like (MLKL) protein is known as the executer of necroptosis [16]. Necroptosis is defined by activation of the receptor-interacting protein kinase (RIPK)1 and RIPK3 to form an oligomeric necrosome, which leads to the phosphorylation and activation of the effector pseudokinase MLKL [16, 17]. Once activated, MLKL multimerizes and translocates to the cell membrane, where it triggers ion release via pore formation, leading to cell swelling and rupture [18, 19]. MLKL has been found to be associated with pathological conditions like cancer, neurodegenerative diseases, and inflammatory diseases [20, 21]. Our previous findings showed that MLKL was significantly upregulated by ox-LDL in endothelial cells (ECs), smooth muscle cells (SMCs), and human myeloid leukemia mononuclear (THP-1) cells, and participated in the progress of atherosclerosis through aggravating inflammatory responses and inhibiting autophagy flux [22].
In this study, the role of MLKL in ox-LDL-triggered NLRP3 inflammasome activation in endothelial cells was studied and the possible mechanisms were also investigated.
MATERIALS AND METHODS
Reagents
Dulbecco’s modified Eagle’s medium (DMEM) and fetal bovine serum were purchased from Gibco (Grand Island Biological Company, New York, NY, USA). Antibodies against rabbit MLKL (A5579), NLRP3 (A5652), and IL-1β (A1112) were obtained from Abclonal (Woburn, MA, USA). Antibodies against mouse caspase-1 (sc-398715) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). MCC950 (CP-456773) was purchased from Selleck Chemicals (Shanghai, China).
Ox-LDL Preparation
The ox-LDL was derived from human low-density lipoprotein (LDL). At 37 °C, 2 mM CuSO4 was added overnight to oxidize (ox) the LDL, and oxidation was stopped with an excess of sodium EDTA. Agarose gel electrophoresis was used to analyze the migration of LDL. The colorimetric determination of thiobarbituric acid reactive species used malondialdehyde (MDA) as a standard, at 12.0 nM MDA per mg protein for the ox-LDL.
Cell Culture
Human umbilical vein endothelial cells (ATCC CRL-1730) were obtained from American Type Culture Collection. ECs were cultured in DMEM with 10% fetal bovine serum. Cells were incubated at 37 °C in an atmosphere of 5% CO2. Cells were seeded in 6- or 12-well plates or 60-mm dishes and grown to 70–80% confluence before use.
QRT-PCR
Total RNA from cultured cells and tissues was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) and reverse transcribed. Real-time PCR was performed on the lightCycler 480 II (Roche, Pleasanton, CA, USA) with SYBR Green Dye detection (TaKaRa Bio, Mountain View, CA, USA). All samples were assayed in triplicate. The data were analyzed using the ΔΔCt method, with GAPDH as a reference in the mRNA analysis. The primer sense and antisense sequences were as follows: MLKL: forward 5′-AGGAGGCTAATGGGGAGATAGA-3′, reverse 5′-TGGCTTGCTGTTAGAAACCTG-3′; GAPDH: forward 5′-GCACCGTCAAGGCTGAGAAC-3′, reverse 5′-TGGTGAAGACGCCAGTGGA-3′.
Immunoblot Analyses
The total protein was measured by the bicinchoninic acid protein assay kit (P0010-1; Beyotime, China). The cleavage products of each sample were separated by 12.5% SDS-PAGE. The western blots were incubated for 8 h with 1:1000-diluted primary antibodies, and then incubated 2 h at room temperature with horseradish-peroxidase-conjugated secondary antibodies. Visualization of proteins used chemiluminescence (ECL Plus Western Blot Detection System; Amersham Biosciences, Foster City, CA, USA).
Lactate Dehydrogenase Release
Cell culture supernatants were collected. LDH levels in the supernatants were determined using an LDH cytotoxicity detection kit (Dojindo Laboratories, Japan) according to the manufacturer’s protocol. The absorbance was read at 490 nm with a microplate reader.
Recombinant Plasmid Construction
A plasmid containing the full-length MLKL cDNA was purchased from OriGene (Rockville, MD, USA). MLKL cDNA was amplified by PCR and subcloned into the pcDNA3.1(+) vector. The correct sequence of the MLKL cDNA in the recombinant plasmid was verified by sequencing and named pcDNA-MLKL. The plasmid was used to transfect ECs using Lipofectamine 3000 transfection reagent.
siRNA Assay
Negative control siRNA (si-control) and siRNA-MLKL (si-MLKL) were purchased from Ribo Targets (Guangzhou, China). ECs and SMCs were transfected with 50 nM siRNA. Control samples for all experimental procedures were processed with a non-targeting control mimic sequence of equal concentration. Western blotting was performed to observe the efficiency of siRNA protein knockdown.
Statistical Analysis
Data were analyzed using the SPSS version 13.0 (SPSS, Chicago, IL, USA) software. Data were presented as the mean ± SD or median (interquartile range) unless otherwise indicated. The results were analyzed by one-way analysis of variance or unpaired Student’s t tests when continuous variables were normally distributed. A two-tailed P value < 0.05 was considered statistically significant.
RESULTS
Ox-LDL Upregulated MLKL Expression and Induced Pyroptosis in ECs
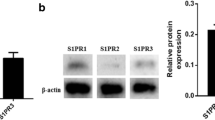
Our previous study found that MLKL was significantly increased by ox-LDL in THP-1 macrophages stimulated with ox-LDL by microarray analysis [22]. In order to verify the effects of ox-LDL on MLKL in ECs, we carried out qRT-PCR and western blot to determine the expression of MLKL in ECs treated with different concentrations of ox-LDL for 24 h. The expression of total MLKL and phosphorylated MLKL was significantly increased at both mRNA and protein levels (Fig. 1a and b).
Ox-LDL upregulated MLKL expression and induced pyroptosis in ECs. ECs were treated with ox-LDL (0, 25, 50, or 100 mg/l) for 24 h. a The expression of MLKL was determined by qRT-PCR. b Total MLKL and phosphorylated MLKL protein levels were measured by western blotting. c The expression of NLRP3, caspase-1, and IL-1β were measured by western blotting. d Proteins released to culture media were enriched by ultrafiltration centrifugation. The levels of matured IL-1β in the supernatants of the cell culture media were analyzed by western blotting. e The levels of LDH release in the supernatants of the cell culture media were analyzed. *P < 0.05. Data are represented as mean ± SD values from 3 independent experiments with each experiment done in triplicate.
Recent studies have shown that pyroptosis is involved in inflammatory reactions. It is noteworthy that pyroptosis could exacerbate the progression of atherosclerosis. To observe the effect of ox-LDL on pyroptosis in ECs, cells were treated with ox-LDL in different concentrations for 24 h. The protein levels of pro-caspase-1, caspase-1, pro-IL-1β, and IL-1β were determined, as well as the levels of secreted IL-1β in culture media. And LDH release assay was carried out to measure the release of cell content caused by pyroptosis. The results showed, as in Fig. 1, that the expressions of pro-caspase-1 is stable, but ox-LDL could induce NLRP3 upregulation, caspase-1 activation, pro-IL-1β production, IL-1β maturation and release (Fig. 1c and d), and the release of LDH (Fig. 1e). These data suggest that ox-LDL induced cell pyroptosis in ECs.
MLKL Triggered Ox-LDL-Induced Pyroptosis in ECs
Previous studies have shown that MLKL plays a crucial role in many kinds of inflammatory diseases [23,24,25,26]. We investigated whether MLKL is involved in ox-LDL-mediated pyroptosis. Firstly we treated ECs with pcDNA-MLKL to upregulate the expression of MLKL, and stimulated cells with 50 mg/ml ox-LDL for 24 h. Western blot analysis showed that MLKL upregulation aggravates ox-LDL-induced caspase-1 cleavage (Fig. 2a). The release of LDH was also increased after MLKL upregulation (Fig. 2c). Next, knockdown of MLKL reversed the increased levels of caspase-1, pro-IL-1β, and IL-1β caused by ox-LDL (Fig. 2b). The release of LDH caused by ox-LDL was also blocked by MLKL knockdown (Fig. 2d). Collectively, these data indicated that MLKL is involved in ox-LDL-induced pyroptosis.
MLKL triggered ox-LDL-induced pyroptosis in ECs. a ECs were transfected with pcDNA-MLKL (overexpressed MLKL) or pcDNA (pcDNA-mock) before ox-LDL treatment(50 mg/l, 24 h), and the protein levels of pro-IL-1β, IL-1β, and caspase-1 were measured by western blotting. b ECs were transfected with si-MLKL or si-control before ox-LDL treatment(50 mg/l, 24 h), and the protein levels of pro-IL-1β, IL-1β, and caspase-1 were measured by western blotting. c ECs were transfected with pcDNA-MLKL or pcDNA before ox-LDL treatment(50 mg/l, 24 h). Fold changes of LDH release compared with pcDNA treatment group. d ECs were transfected with si-MLKL or si-control before ox-LDL treatment(50 mg/l, 24 h). Fold changes of LDH release compared with si-control treatment group. *P < 0.05 versus the control group. Data are represented as mean ± SD values from 3 independent experiments with each experiment done in triplicate.
MLKL Triggered Ox-LDL-Induced Pyroptosis via NLRP3 Inflammasome Activation
The canonical pyroptosis signaling pathway requires recognition to cell damage signals and assembly of inflammasomes. There are different kinds of inflammasomes that would lead to cell pyroptosis. Our experiment results showed that ox-LDL induced NLRP3 expression, and MLKL upregulation further increased NLRP3 protein level (Fig. 3a). And ox-LDL-induced NLRP3 upregulation was significantly suppressed by MLKL knockdown (Fig. 3b). To confirm whether MLKL triggered ox-LDL-induced pyroptosis via NLRP3 inflammasome activation, we used a specific NLRP3 inhibitor MCC950. Western blot analysis showed that after inhibiting activation of NLRP3 protein, the maturation of caspase-1 and IL-1β induced by ox-LDL were abolished, as well as MLKL triggered ox-LDL-induced maturation of caspase-1 and IL-1β (Fig. 3c), which means MLKL triggered ox-LDL-induced pyroptosis via NLRP3 inflammasome.
MLKL triggered ox-LDL-induced pyroptosis via NLRP3 inflammasome activation. a ECs were transfected with pcDNA-MLKL (overexpressed MLKL) or pcDNA (pcDNA-mock) before ox-LDL treatment (50 mg/l, 24 h), and the protein levels of NLRP3 were measured by western blotting. b ECs were transfected with si-MLKL before ox-LDL treatment (50 mg/l, 24 h), and the protein levels of NLRP3 were measured by western blotting. c ECs were treated with NLRP3 specific inhibitor MCC950, and the protein levels of caspase-1 and IL-1β were measured by western blotting. d Cell culture media were added with 50 mM potassium chloride and 50 mM sodium chloride respectively, and the protein levels of caspase-1 and IL-1β were measured by western blotting. *P < 0.05 versus the control group. Data are represented as mean ± SD values from 3 independent experiments with each experiment done in triplicate.
NLRP3 could be activated by lysosomal enzyme cathepsin B, potassium efflux, reactive oxygen species (ROS), and other cell damage signals. Among them, potassium efflux is a common step that is necessary to stimulate the activation of NLRP3 inflammatory. As we have mentioned, phosphorylated MLKL translocated to the plasma membrane where it forms cation channels that are permeable potassium. To explore whether MLKL triggers ox-LDL-induced NLRP3 inflammasome assembly through potassium efflux, exogenous potassium chloride was added into cell culture media to inhibit potassium efflux. The cleavage of caspase-1 and IL-1β was determined and the results showed that high level of extracellular potassium blocks the activation of NLRP3 inflammasome triggered by MLKL (Fig. 3d). Collectively, our findings showed that MLKL processed intracellular potassium efflux, and further triggered ox-LDL-induced pyroptosis via NLRP3 inflammasome activation.
DISCUSSION
Modern hypotheses introduce atherosclerosis as an inflammatory/lipid-based disease and NLRP3 inflammasome has been considered a link between lipid metabolism and inflammation because crystalline cholesterol and ox-LDL (two abundant components in atherosclerotic plaques) activate NLRP3 inflammasome [27]. Our findings showed that MLKL, an executor of necrosis, triggered ox-LDL-induced endothelial cell pyroptosis via NLRP3 inflammasome activation.
Cell death can be observed in atherosclerosis and plays an important role in the occurrence and development of atherosclerosis lesions [28]. Pyroptosis is involved in the formation and development of atherosclerosis by promoting the release of inflammatory cytokines, which is closely related to the stability of plaques [29]. Ox-LDL can induce macrophage pyroptosis, which plays an important role in the formation of atherosclerosis and the stability of plaques [30]. It has been reported that ox-LDL and cholesterol crystals in the necrotic areas of plaque increase the levels of NLRP3, pro-IL-1β, and caspase-1, inducing cell pyroptosis [27, 31,32,33]. This phenomenon leads to the release of IL-1β, which also aggravate the inflammatory response and play the role of atherosclerosis. Our finding shows that ox-LDL upregulates the pro-IL-1β levels and activates NLRP3 inflammasome which enables autocatalytic cleavage and reassembly of pro-caspase-1 to form active caspase-1. Activated caspase-1 is responsible for cleavage of pro-IL-1β, which once processed, will be in its biologically active form ready to be released from endothelial cells, and contributes to endothelial cell pyroptosis. Considering that endothelial cells are the barrier between blood and vessel walls, ox-LDL-induced EC pyroptosis participates in the starting point of atherosclerosis injury.
Pyroptosis is executed by inflammasomes, and the most well-known inflammasome is NLRP3 inflammasome, which is thought to act as a bridge between lipid metabolism and inflammation caused by cholesterol crystals [27]. Once activated, the inflammasome forms a plate-like structure that triggers caspase-1, cytokine release, and pyroptosis [34]. Caspase-1 is expressed abundantly in atherosclerosis plaques [35, 36]. What is more, caspase-1 contents in vulnerable plaques and ruptured lesions increased significantly in patients who died from acute coronary events [37]. We confirmed that ox-LDL-induced caspase-1 activation and IL-1β maturation depend on NLPR3 in ECs, which offers novel insight into the mechanisms of arterial intima injury and inflammation caused by ox-LDL.
Necrosis is a newly discovered programmed cell death process associated with inflammatory disease [17]. MLKL is critical for necrosis, which releases molecules within the cell, leading to an inflammatory response [38]. Recent studies have shown that MLKL expression increases in people with unstable carotid atherosclerosis [39]. And phosphorylation of MLKL, which plays an important role in necrosis, can be detected in advanced atherosclerosis [40]. Our previous works show that MLKL aggravated inflammatory response caused by ox-LDL and confirm that MLKL-inhibited autophagy was mainly due to the activation of the mammalian/mechanistic target of rapamycin (mTOR)-dependent signaling pathway [22]. It has been reported that MLKL could induce activation of NLRP3 in a cell intrinsic way, which requires oligomerization and association of MLKL with cellular membranes, and subsequent reduction in intracellular potassium concentration [41, 42]. Our results also showed that MLKL induced an increase in NLRP3 inflammasome activation caused by ox-LDL. After block cell potassium efflux, the activation of caspase-1 and IL-1β was significantly attenuated. Furthermore, we put forward that MLKL triggered ox-LDL-induced NLRP3 inflammasome activation and cell pyroptosis for the first time.
Collectively, the role of MLKL in ox-LDL-induced NLRP3 inflammasome activation was demonstrated. What is more, our results also indicate the potential importance of MLKL in atherosclerosis, which may be used as both a diagnostic and therapeutic tool for the treatment of atherosclerosis.
References
Weissberg, P.L., and M.R. Bennett. 1999. Atherosclerosis-an inflammatory disease. The New England Journal of Medicine 340: 1928–1929.
Suciu, C.F., M. Prete, P. Ruscitti, E. Favoino, R. Giacomelli, and F. Perosa. 2018. Oxidized low density lipoproteins: the bridge between atherosclerosis and autoimmunity. Possible implications in accelerated atherosclerosis and for immune intervention in autoimmune rheumatic disorders. Autoimmunity Reviews 17: 366–375.
Fernandez-Friera, L., V. Fuster, B. Lopez-Melgar, B. Oliva, J.M. Garcia-Ruiz, J. Mendiguren, et al. 2017. Normal LDL-cholesterol levels are associated with subclinical atherosclerosis in the absence of risk factors. Journal of the American College of Cardiology 70: 2979–2991.
Tousoulis, D., E. Oikonomou, E.K. Economou, F. Crea, and J.C. Kaski. 2016. Inflammatory cytokines in atherosclerosis: current therapeutic approaches. European Heart Journal 37: 1723–1732.
Bergsbaken, T., S.L. Fink, and B.T. Cookson. 2009. Pyroptosis: host cell death and inflammation. Nature Reviews. Microbiology 7: 99–109.
Gross, O., A.S. Yazdi, C.J. Thomas, M. Masin, L.X. Heinz, G. Guarda, et al. 2012. Inflammasome activators induce interleukin-1alpha secretion via distinct pathways with differential requirement for the protease function of caspase-1. Immunity 36: 388–400.
Miao, E.A., I.A. Leaf, P.M. Treuting, D.P. Mao, M. Dors, A. Sarkar, S.E. Warren, M.D. Wewers, and A. Aderem. 2010. Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nature Immunology 11: 1136–1142.
Van Opdenbosch, N., and M. Lamkanfi. 2019. Caspases in cell death, inflammation, and disease. Immunity 50: 1352–1364.
Zhaolin, Z., L. Guohua, W. Shiyuan, and W. Zuo. 2019. Role of pyroptosis in cardiovascular disease. Cell Proliferation 52: e12563.
Yin, Y., X. Li, X. Sha, H. Xi, Y.F. Li, Y. Shao, J. Mai, A. Virtue, J. Lopez-Pastrana, S. Meng, D.G. Tilley, M.A. Monroy, E.T. Choi, C.J. Thomas, X. Jiang, H. Wang, and X.F. Yang. 2015. Early hyperlipidemia promotes endothelial activation via a caspase-1-sirtuin 1 pathway. Arteriosclerosis, Thrombosis, and Vascular Biology 35: 804–816.
Xi, H., Y. Zhang, Y. Xu, W.Y. Yang, X. Jiang, X. Sha, X. Cheng, J. Wang, X. Qin, J. Yu, Y. Ji, X. Yang, and H. Wang. 2016. Caspase-1 inflammasome activation mediates homocysteine-induced pyrop-apoptosis in endothelial cells. Circulation Research 118: 1525–1539.
Zhang, Y., X. Li, A.L. Pitzer, Y. Chen, L. Wang, and P.L. Li. 2015. Coronary endothelial dysfunction induced by nucleotide oligomerization domain-like receptor protein with pyrin domain containing 3 inflammasome activation during hypercholesterolemia: beyond inflammation. Antioxidants & Redox Signaling 22: 1084–1096.
Sadeghi, H., A. Lockmann, A.C. Hund, U.K. Samavedam, E. Pipi, K. Vafia, et al. 2015. Caspase-1-independent IL-1 release mediates blister formation in autoantibody-induced tissue injury through modulation of endothelial adhesion molecules. Journal of Immunology 194: 3656–3663.
Wang, L., Y. Chen, X. Li, Y. Zhang, E. Gulbins, and Y. Zhang. 2016. Enhancement of endothelial permeability by free fatty acid through lysosomal cathepsin B-mediated Nlrp3 inflammasome activation. Oncotarget 7: 73229–73241.
Back, M., A.J. Yurdagul, I. Tabas, K. Oorni, and P.T. Kovanen. 2019. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nature Reviews. Cardiology 16: 389–406.
Quarato, G., C.S. Guy, C.R. Grace, F. Llambi, A. Nourse, D.A. Rodriguez, R. Wakefield, S. Frase, T. Moldoveanu, and D.R. Green. 2016. Sequential engagement of distinct MLKL phosphatidylinositol-binding sites executes necroptosis. Molecular Cell 61: 589–601.
Dhuriya, Y.K., and D. Sharma. 2018. Necroptosis: a regulated inflammatory mode of cell death. Journal of Neuroinflammation 15: 199.
Xia, B., S. Fang, X. Chen, H. Hu, P. Chen, H. Wang, and Z. Gao. 2016. MLKL forms cation channels. Cell Research 26: 517–528.
Murphy, J.M., P.E. Czabotar, J.M. Hildebrand, I.S. Lucet, J.G. Zhang, S. Alvarez-Diaz, R. Lewis, N. Lalaoui, D. Metcalf, A.I. Webb, S.N. Young, L.N. Varghese, G.M. Tannahill, E.C. Hatchell, I.J. Majewski, T. Okamoto, R.C.J. Dobson, D.J. Hilton, J.J. Babon, N.A. Nicola, A. Strasser, J. Silke, and W.S. Alexander. 2013. The pseudokinase MLKL mediates necroptosis via a molecular switch mechanism. Immunity 39: 443–453.
Van Hoecke, L., S. Van Lint, K. Roose, A. Van Parys, P. Vandenabeele, J. Grooten, et al. 2018. Treatment with mRNA coding for the necroptosis mediator MLKL induces antitumor immunity directed against neo-epitopes. Nature Communications 9: 3417.
Zhang, S., M.B. Tang, H.Y. Luo, C.H. Shi, and Y.M. Xu. 2017. Necroptosis in neurodegenerative diseases: a potential therapeutic target. Cell Death & Disease 8: e2905.
Guo, F.X., Q. Wu, P. Li, L. Zheng, S. Ye, X.Y. Dai, C.M. Kang, J.B. Lu, B.M. Xu, Y.J. Xu, L. Xiao, Z.F. Lu, H.L. Bai, Y.W. Hu, and Q. Wang. 2019. The role of the LncRNA-FA2H-2-MLKL pathway in atherosclerosis by regulation of autophagy flux and inflammation through mTOR-dependent signaling. Cell Death and Differentiation 26: 1670–1687.
Najafov, A., A.K. Mookhtiar, H.S. Luu, A. Ordureau, H. Pan, P.P. Amin, et al. 2019. TAM kinases promote necroptosis by regulating oligomerization of MLKL. Molecular Cell 75: 457–468.e4.
Yuan, J., P. Amin, and D. Ofengeim. 2019. Necroptosis and RIPK1-mediated neuroinflammation in CNS diseases. Nature Reviews. Neuroscience 20: 19–33.
Zhao, Q., X. Yu, M. Li, Y. Liu, Y. Han, X. Zhang, X.M. Li, X.X. Wu, J. Qin, J. Fang, and H. Zhang. 2019. MLKL attenuates colon inflammation and colitis-tumorigenesis via suppression of inflammatory responses. Cancer Letters 459: 100–111.
Liu, W., B. Chen, Y. Wang, C. Meng, H. Huang, X.R. Huang, J. Qin, S.R. Mulay, H.J. Anders, A. Qiu, B. Yang, G.J. Freeman, H.J. Lu, H.Y. Lin, Z.H. Zheng, H.Y. Lan, Y. Huang, and Y. Xia. 2018. RGMb protects against acute kidney injury by inhibiting tubular cell necroptosis via an MLKL-dependent mechanism. Proceedings of the National Academy of Sciences of the United States of America 115: E1475–E1484.
Paramel, V.G., L. Folkersen, R.J. Strawbridge, B. Halvorsen, A. Yndestad, T. Ranheim, et al. 2016. NLRP3 inflammasome expression and activation in human atherosclerosis. Journal of the American Heart Association 5.
Rayner, K.J. 2017. Cell death in the vessel wall: the good, the bad, the ugly. Arteriosclerosis, Thrombosis, and Vascular Biology 37: e75–e81.
Zhou, W., C. Chen, Z. Chen, L. Liu, J. Jiang, Z. Wu, et al. 2018. NLRP3: a novel mediator in cardiovascular disease. Journal of Immunology Research 2018: 5702103.
Lin, J., X. Shou, X. Mao, J. Dong, N. Mohabeer, K.K. Kushwaha, et al. 2013. Oxidized low density lipoprotein induced caspase-1 mediated pyroptotic cell death in macrophages: implication in lesion instability? PLoS One 8: e62148.
Usui, F., K. Shirasuna, H. Kimura, K. Tatsumi, A. Kawashima, T. Karasawa, S. Hida, J. Sagara, S’. Taniguchi, and M. Takahashi. 2012. Critical role of caspase-1 in vascular inflammation and development of atherosclerosis in Western diet-fed apolipoprotein E-deficient mice. Biochemical and Biophysical Research Communications 425: 162–168.
Shi, X., W.L. Xie, W.W. Kong, D. Chen, and P. Qu. 2015. Expression of the NLRP3 inflammasome in carotid atherosclerosis. Journal of Stroke and Cerebrovascular Diseases 24: 2455–2466.
Zhang, L., L. Lu, X. Zhong, Y. Yue, Y. Hong, Y. Li, and Y. Li. 2019. Metformin reduced NLRP3 inflammasome activity in Ox-LDL stimulated macrophages through adenosine monophosphate activated protein kinase and protein phosphatase 2A. European Journal of Pharmacology 852: 99–106.
Schneider, K.S., C.J. Gross, R.F. Dreier, B.S. Saller, R. Mishra, O. Gorka, et al. 2017. The inflammasome drives GSDMD-independent secondary pyroptosis and IL-1 release in the absence of caspase-1 protease activity. Cell Reports 21: 3846–3859.
Gage, J., M. Hasu, M. Thabet, and S.C. Whitman. 2012. Caspase-1 deficiency decreases atherosclerosis in apolipoprotein E-null mice. The Canadian Journal of Cardiology 28: 222–229.
Hendrikx, T., M.L. Jeurissen, P.J. van Gorp, M.J. Gijbels, S.M. Walenbergh, T. Houben, et al. 2015. Bone marrow-specific caspase-1/11 deficiency inhibits atherosclerosis development in Ldlr(−/−) mice. The FEBS Journal 282: 2327–2338.
Zheng, F., Z. Gong, S. Xing, and Q. Xing. 2014. Overexpression of caspase-1 in aorta of patients with coronary atherosclerosis. Heart, Lung & Circulation 23: 1070–1074.
Gong, Y.N., C. Guy, J.C. Crawford, and D.R. Green. 2017. Biological events and molecular signaling following MLKL activation during necroptosis. Cell Cycle 16: 1748–1760.
Karunakaran, D., M. Geoffrion, L. Wei, W. Gan, L. Richards, P. Shangari, E.M. DeKemp, R.A. Beanlands, L. Perisic, L. Maegdefessel, U. Hedin, S. Sad, L. Guo, F.D. Kolodgie, R. Virmani, T. Ruddy, and K.J. Rayner. 2016. Targeting macrophage necroptosis for therapeutic and diagnostic interventions in atherosclerosis. Science Advances 2: e1600224.
Szobi, A., E. Goncalvesova, Z.V. Varga, P. Leszek, M. Kusmierczyk, M. Hulman, et al. 2017. Analysis of necroptotic proteins in failing human hearts. Journal of Translational Medicine 15: 86.
Gutierrez, K.D., M.A. Davis, B.P. Daniels, T.M. Olsen, P. Ralli-Jain, S.W. Tait, et al. 2017. MLKL activation triggers NLRP3-mediated processing and release of IL-1beta independently of gasdermin-D. Journal of Immunology 198: 2156–2164.
Conos, S.A., K.W. Chen, D. De Nardo, H. Hara, L. Whitehead, G. Nunez, et al. 2017. Active MLKL triggers the NLRP3 inflammasome in a cell-intrinsic manner. Proceedings of the National Academy of Sciences of the United States of America 114: E961–E969.
Funding
This work was supported by the National Natural Sciences Foundation of China (grant numbers 81871701 and 81772244), the Natural Science Fund of Guangdong (grant numbers 2020B1515020013, 2017A030313532 and 2017A030313535), and the Science and Technology Program of Guangzhou (grant number 201704020213).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Qian Wu and Xin He designed the study, performed most part of the experiments, analyzed and interpreted the data, and wrote the manuscript. Li-Mei Wu, Ru-Yi Zhang, and Li-Min Li performed part of the experimental procedures. Chang-Meng Wu, Yuan-Bin Lu, Bing Hu, Chao Shi, Zhi-Feng Lu, and Biao Yang contributed to data acquisition. Lei Zheng, Yan-Wei Hu, and Qian Wang provided financial support and guided the completion of the project. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, Q., He, X., Wu, LM. et al. MLKL Aggravates Ox-LDL-Induced Cell Pyroptosis via Activation of NLRP3 Inflammasome in Human Umbilical Vein Endothelial Cells. Inflammation 43, 2222–2231 (2020). https://doi.org/10.1007/s10753-020-01289-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01289-8