Abstract
Pinolenic acid (PNA) is a rare n-6 polyunsaturated fatty acid (n-6 PUFA) originally identified in pine seeds. Previous studies demonstrated that PNA and its elongation metabolite, Δ7-eicosatrienoic acid (Δ7-ETrA), exerted an anti-inflammatory effect in cultured cells by suppressing prostaglandin E2 (PGE2) production. The objective of this study was to further examine the in vivo anti-inflammatory properties of PNA. Using human THP-1 macrophage, we first confirmed that incorporation of PNA into cellular phospholipids suppressed the production of interleukin-6 (IL-6) (by 46%), tumor necrosis factor-α (TNF-α) (by 18%), and prostaglandin E2 (PGE2) (by 87%), and the expression of type-2 cyclooxygenase (COX-2) (by 27%). Furthermore, we demonstrated that injection of PNA or Δ7-ETrA suppressed 12-O-tetradecanoylphorbol-13-acetate (TPA)-induced mouse ear edema, as measured by ear thickness (by 15%) and biopsy weight (by up to 29%). Both PUFA also lowered proportions of infiltrated leukocytes, neutrophils, and macrophages using flow cytometric analysis. Topical application of PNA or Δ7-ETrA on mouse back skin suppressed TPA-induced pro-inflammatory mediator production, including IL-1β, IL-6, TNF-α, and PGE2, as well as the phosphorylation of p38- and JNK-mitogen-activated protein kinase (MAPK), but not that of ERK-MAPK. That no PNA or Δ7-ETrA was detected in the ear disc after the PUFA injection suggests that their anti-inflammatory effect might not be due to fatty acid incorporation, but to modulation of cell signaling. In conclusion, PNA and Δ7-ETrA exerted the in vivo anti-inflammatory effect by suppressing mouse ear edema and dorsal skin inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Pinolenic acid (PNA; Δ5,9,12-18:3) is an unusual n-6 non-methylene-interrupted fatty acid (NMIFA) and a major polyunsaturated fatty acids (PUFA) originally found in seeds of Pinaceae plants [1, 2]. PNA is metabolized from linoleic acid (LA; Δ9,12-18:2) by the action of species-specific Δ5-desaturase (Fig. 1) [3]. This pathway is different from the conversion of dihomo-γ-linolenic acid (DGLA; Δ8,11,14-20:3) to arachidonic acid (AA; Δ5,8,11,14-20:4) that occurs in most mammalian cells [4, 5]. The unique non-methylene-interrupted (or called polymethylene-interrupted) structure in the carbon-skeleton distinguishes from the more common n-6 PUFA in terms of metabolism and biological properties. For example, PNA is metabolized to Δ7-eicosatrienoic acid (Δ7-ETrA; Δ7,11,14-20:3), followed by another C2-elongation step to form Δ9-docosatrienoic acid (Δ9-DTrA; Δ9,13,16-22:3) (Fig. 1) [6,7,8].
Furthermore, incubation of cells with PNA or Δ7-ETrA modulated the fatty acid composition and lowered the proportion of AA in cellular phospholipids, and significantly decreased the production of prostaglandin E2 (PGE2) in murine macrophage, microglial, and human breast cancer cell lines [7,8,9,10]. Since several research groups have previously reported that only a small proportion of PNA or Δ7-ETrA in tissue phospholipids was detected when rats were fed pine seed oil (PSO) [1, 11, 12], it was therefore of interest to us to determine whether the low extent of incorporation of PNA or Δ7-ETrA into phospholipids could also exert a comparable anti-inflammatory effect in animal studies. However, to our knowledge, no studies have been conducted to confirm the in vivo anti-inflammatory properties of PNA.
To this end, we first determined the suppressive effect of PNA on pro-inflammatory mediator production in human macrophage-like THP-1 cells. Next, using the mouse ear edema model and the back skin model, we determined if PNA could suppress 12-O-tetradecanoylphorbol-13-acetate (TPA)-induced inflammatory responses by reducing ear swelling, pro-inflammatory cytokine and PGE2 production, as well as COX-2 gene expression. In addition, activation of inflammatory mitogen-activated protein kinases (MAPK) signaling pathways, such as p38-mitogen-activated kinase (p38), c-Jun N-terminal kinase (JNK), and extracellular signal–related kinase (ERK) were assessed in order to further explore the mechanisms underlying the anti-inflammatory properties of PNA. The results of this study confirmed the in vivo anti-inflammatory effects of PNA and advance our understanding regarding the biological properties of PNA.
MATERIALS AND METHODS
Chemicals
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), dexamethasone, dimethyl sulfoxide (DMSO), lipopolysaccharide (LPS, from Escherichia coli O26:B6), lysis buffer, protease inhibitors, TPA, triheptadecanoin, and Tween-20 were obtained from Sigma Chemical Co. (St. Louis, MO, USA). Enzyme-linked immunosorbent assay (ELISA) kits for detecting mouse or human interleukin-1β (IL-1β), IL-6, and tumor necrotic factor-α (TNF-α) were purchased from Invitrogen (Carlsbad, CA, USA). PGE2 enzyme immunoassay assay (EIA) kit was purchased by Cayman Chemicals (Ann Arbor, MI, USA). All antibodies were purchased from Cell Signaling Technology (Danver, MA, USA), except for β-actin that was obtained from Novus Biologicals (Centennial, CO, USA) and the secondary antibody was from the Sigma. Standard mixtures for gas chromatography (GC) and thin-layer chromatography (TLC) were obtained from Nu-Chek-Prep, Inc. (Elysian, MN, USA). Roswell Park Memorial Institute (RPMI) 1460 medium, fetal bovine serum (FBS), and phosphate-buffered saline (PBS) were purchased from Gibco (Carlsbad, CA, USA). All reagent-grade organic solvents were from Burdick & Jackson (Muskegon, MI, USA).
Cell Culture and Growth Conditions
The human THP-1 monocyte cell line (BCRC 60430) was supplied by Bioresource Collection and Research Center (Hsinchu, Taiwan). Monocytes were incubated in 10% (v/v) FBS-supplemented RPMI 1460 medium, and maintained in a 5% CO2 fully humidified incubator at 37 °C. THP-1 monocytes were differentiated to macrophage-like cells with 10 nM TPA for 24 h. The typical hallmarks of macrophages, such as cell adhesion and spreading morphology, were observed by optical microscopy after TPA treatment. To monitor cell viability, the methods of MTT assay and trypan blue dye exclusion were applied in this study.
Lipid Extraction and Fatty Acid Analysis
We incubated TPA-differentiated THP-1 macrophage cells with 0, 50, or 100 μM of PNA for 24 h, followed by LPS stimulation for 18 h. After harvest, cell pellets were rinsed with PBS, and total lipids of THP-1 cells were extracted using the modified Folch method described elsewhere [8, 13]. The phospholipid (PL) fraction of total lipids was then separated by TLC using a developing solvent consisting of hexane/diethyl ether/acetic acid, 80:20:1 (v/v/v). Fatty acid methyl esters (FAME) derived from the cellular phospholipids were analyzed using an Agilent 6890 gas chromatograph equipped with an autosampler, a flame-ionization detector (FID), and a fused-silica capillary column (Omegawax; 30 m × 0.32 mm, i.d., film thickness 0.25 μm, Supelco, Bellefonte, PA, USA), and the operating conditions are described elsewhere [8]. An authentic GC standard mixture was used to identify fatty acids of samples, and a fixed amount of internal standard (triheptadecanoin) was added to each sample for the quantification.
Determination of Pro-inflammatory Mediators in Macrophage-Like THP-1 Cells
To examine whether PNA might modulate the production of pro-inflammatory mediators, TPA-differentiated THP-1 cells were incubated with different concentrations (0, 10, 25, 50, or 100 μM) of PNA for 24 h, followed by the LPS stimulation (0.2 μg/mL) for 16 h. The concentrations of PGE2, TNF-α, and IL-6 from the cell supernatants were assessed using commercial enzyme immunoassay kits.
Western blot assay was used for quantification of COX-2 protein level. After sample preparation, total protein of the tissue/cell supernatant was determined using the BCA Protein Assay Reagent Kit (Pierce, Rockford, IL, USA) with bovine albumin serving as standard. Heat-denatured protein samples (10 μg) from tissue or cell lysates were separated by 10% (w/v) sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred to polyvinylidene difluoride (PVDF) membranes (Millipore, MA, USA) and blocked with 5% (w/v) skim milk. Blots were processed using primary antibodies (1:1000 dilution), and followed by reacting with a secondary antibody (1:5000 dilution of anti-mouse immunoglobulin conjugated with horseradish peroxidase). The interested immunoreactive-complexes were developed and visualized by enhanced chemiluminescence (ECL) (Merck, Darmstadt, Germany); α-tubulin expression was used as the internal control.
TPA-Induced In vivo Inflammatory Responses
Male ICR mice (8 weeks old) obtained from Animal Center of College of Medicine, National Taiwan University (Taipei, Taiwan) were used in this study. Mice were randomly grouped (6 per group) and housed in the standard barrier facility with chow diet and water provided ad libitum. All procedures were approved by the Institutional Animal Care and Use Committee of Yuanpei University of Medical Technology (IACUC Approval No. LAC10301).
To investigate the in vivo anti-inflammatory effects of PNA, both TPA-induced mouse ear edema and back skin models were employed. The left ear of ICR mice was intradermally injected with PNA or Δ7-ETrA (3 μg/10 μL in PBS) or dexamethasone, a potent anti-inflammatory agent (0.01 μg/10 μL in PBS), while right ears received an equal amount (10 μL) of PBS as the control. This amount of PNA or Δ7-ETrA (3 μg/10 μL) has been shown to be optimal for this particular experiment (data not shown). Eighteenth hours after PNA or Δ7-ETrA treatment, 10 μL of TPA solution (5 μg TPA in PBS) was injected into the same site in both ears. After 24-h TPA treatment, the change in ear thickness was measured using a vernier micro-caliper (Mitutoyo, Kanagawa, Japan). The mice were then terminated by inhalation of carbon dioxide. Each 4-mm ear punch was immediately collected and weighed. The extent of ear edema was evaluated and expressed based on the thickness and weight difference between the left and the right ears or ear disks.
In the second study, all hair in a 1-cm2 area of mouse back skin was removed by shaving prior to the treatment. PNA or Δ7-ETrA at the fixed dosage (3 μg/10 μL in acetone) was topically applied to the shaved back skin for 18 h, the negative control treated with vehicle. TPA (5 μg/10 μL in acetone) was then applied onto the same location of back skin [14]. After 2-h stimulation, mice were sacrificed and the treated back skin was collected for the following experiments.
Analysis of Infiltrating Leukocytes from Mouse Ear Using Flow Cytometry
In a separate experiment, mice received intradermal treatment on the ear with PUFA and/or TPA as described above. Six hours post-TPA injection, the mouse ears were excised (n = 4), split into dorsal and ventral halves, and smeared into RPMI medium to disperse cells. Six hours of TPA stimulation has been shown to be optimal for this kind of experiment (data not shown). Single-cell suspensions from inflammatory skin lesions in mouse ears were prepared using the Huang’s method described elsewhere [15]. Single-cell suspensions were then incubated in FACS buffer (PBS containing 0.5% (w/v) bovine serum albumin and 0.09% sodium azide) containing peridinin chlorophyll protein (PerCP)-conjugated anti-mouse CD45 (a leukocyte marker) (BioLegend, San Diego, CA, USA), fluorescein isothiocyanate (FITC)-conjugated anti-mouse Ly6G (a neutrophil marker) (BioLegend), and phycoerythrin (PE)-conjugated anti-mouse F4/80 (a macrophage marker) (BioLegend) for 30 min. All cell samples were analyzed with a FACSCantoTM II flow cytometer (BD Biosciences) using FACS Diva software, and the data were collated and analyzed using FlowJo software.
Detection of Cytokine Production, and COX-2 and MAPK Expression in Mouse Ear and Dorsal Skin Tissues
Mouse ear discs and back skin samples were collected according to the procedures described above. Detection methods were followed by a modification of the procedure reported by Tsai (2016) [16]. Briefly, after thickness had been measured, the ears were excised. The ear samples were homogenized using a BioMasher IIIr (Nippi Inc., Tokyo, Japan) in radioimmunoprecipitation (RIPA) buffer (G-Biosciences, St. Louis, MO, USA) supplemented with 1 mM phenylmethylsulfonyl fluoride (PMSF) for 1 min on ice. The homogenates were vortexed and then centrifuged at 10,000g for 10 min at 4 °C. The supernatant was for the determinations of PGE2, TNF-α, IL-1β, and IL-6 levels according to the manufacturer’s instruction. The COX-2 protein level of mouse ear and MAPK expression of mouse back skin tissue were determined using Western Blot assay as described above, while β-actin expression was used as the internal control.
Statistical Analyses
All data were analyzed by analysis of variance (ANOVA) and Duncan’s multiple range test using SPSS Statistics for Windows, version 17.0 (SPSS Inc. Chicago, IL, USA) to test differences between means. Mean differences among groups were considered significant at the P ≤ 0.05 levels.
RESULTS
Modulation of PNA on Macrophage Phospholipid Fatty Acid Composition
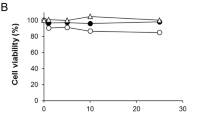
When macrophage-differentiated THP-1 cells were incubated with increasing concentrations (0, 10, 25, 50, 100, and 200 μM) of PNA, there is no significant negative effect on cell proliferation when PNA concentrations were 100 μM or less (Fig. 2a). To determine whether PNA supplementation would affect cellular phospholipid fatty acid composition, THP-1 macrophage cells were incubated with 0, 50, or 100 μM of PNA for 24 h, followed by LPS stimulation for 18 h.
Effect of pinolenic acid (PNA) on cell viability (a), and on the proportions of saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and n-6 polyunsaturated fatty acid (n-6 PUFA) and n-3 PFUA (b) in cellular phospholipids of macrophage-like THP-1 cells. 12-O-tetradecanoylphorbol-13-acetate (TPA)-differentiated THP-1 cells were incubated in a medium supplemented with different concentrations (0, 10, 25, 50, 100, or 200 μM) of PNA for 24 h, followed by LPS stimulation for 18 h. The bars indicate the mean ± SD of three independent experiments. The values with different letters are significantly different at p < 0.05.
Fatty acid analysis showed that there was no significant difference in the proportions of individual fatty acids between the control and LPS-stimulated groups (Table 1), indicating that LPS treatment had no effect on cellular phospholipid fatty acid compositions. Furthermore, inclusion of PNA in the culture medium caused the percentage of total cellular n-6 PUFA to increase markedly, from 16.1 up to 48.6% (Fig. 2b). In contrast, however, PNA decreased the proportions of monounsaturated fatty acids (MUFA) from 38.7 to 16.3% (p < 0.001) and n-3 PUFA from 7.4 to 4.0% (p = 0.001). The total contribution of saturated fatty acids (SFA) made to the fatty acid composition of cellular phospholipids was changed slightly, but not to a statistically significant extent. Table 1 shows that the proportions of PNA and Δ7-ETrA increased as the concentration of PNA in the culture medium increased. Incubation of cells with PNA also caused the percentages of other phospholipid n-6 PUFA to change significantly, including LA; γ-linolenic acid (GLA), eicosadienoic acid (EDA; C20:2n-6), and adrenic acid (ADA; C22:4n-6) increased while DGLA, AA and docosapentaenoic acid (DPA; C22:5n-6) decreased. Noteworthy was the significant increase in the proportion of LA from 2.0% in the controls to 17.1% in cells treated with PNA (100 μM). However, incubation of cells with PNA would significantly reduce levels of phospholipid AA from 11.0 to 6.3%.
Effect of PNA on Key Cellular Inflammatory Responses
To confirm whether PNA might suppress inflammatory responses, as it did in similar previous cell studies of ours [7, 8], differentiated THP-1 cells were incubated with different concentrations of PNA for 24 h, followed by 16 h of LPS stimulation. Whereas productions of TNF-α, IL-6, and PGE2 were all increased by LPS (Fig. 3A–C), incubation of cells with increasing concentrations of PNA decreased the production of TNF-α, IL-6, and PGE2 by 18, 46, and 87%, respectively. Furthermore, inflammatory COX-2 was over-expressed in cells treated with LPS (Fig. 3D). Over-expression of COX-2 was significantly suppressed when PNA was administered together with LPS.
Effects of different concentrations of PNA supplementation on the production of tumor necrosis factor-α (TNF-α) (A), interleukin-6 (IL-6) (B) and prostaglandin E2 (PGE2) (C), and on the expression of cyclooxygenase-2 (COX-2) at the translation level (D) by macrophage-like THP-1 cells. TPA-differentiated THP-1 cells were incubated with various concentrations of PNA for 24 h, and then stimulated with 0.2 μg/ml of LPS for 16 h. Cell-free supernatants were analyzed for TNF-α, IL-6, and PGE2, and cell pellets were analyzed for COX-2 protein. The bars indicate the mean ± SD of three independent experiments. The values with different letters are significantly different at p < 0.05.
Effect of PNA on TPA-Induced Mouse Ear Edema
To investigate the possible in vivo suppressive effect of PNA and its metabolite Δ7-ETrA on ear edema, mouse ears were intradermally injected with 3 μg of PUFA, followed 18 h later by TPA injection for 24 h (Fig. 4A). Figure 4B and C show that TPA caused mouse ear to swell 2.6-fold (p < 0.001) and ear biopsy weight 2.5-fold (p < 0.001) as compared with the untreated control. Injection of PNA or Δ7-ETrA significantly blunted TPA-stimulated ear edema, as measured by ear thickness, by 15% and ear biopsy weight by 29%. Furthermore, injection of dexamethasone 18 h prior to the TPA stimulation reduced ear thickness by 25%; however, no such effect on biopsy weight was found.
Effect of PNA on TPA-induced mouse ear skin inflammatory responses. Experimental design (A). Effects of PNA and Δ7-eicosatrienoic acid (Δ7-ETrA) on TPA-induced mouse ear edema by ear thickness (B) and ear biopsy weight (C). Effect of incubation time (0, 1, 2, 4, or 8 h) on TPA-stimulated ear COX-2 expression (D), and effect of PNA, Δ7-ETrA or dexamethasone (DEX) on TPA-stimulated ear COX-2 expression (E). PNA, Δ7-eicosatrienoic acid (Δ7-ETrA), DEX or vehicle was locally injected and incubated for 18 h, followed by the TPA injection. The inhibitory effects of PNA and Δ7-ETrA on TPA-stimulated mouse ear edema were evaluated by measuring the ear thickness and ear biopsy weight. Minced mouse ear samples were analyzed for protein (D and E). Each value represents the mean ± SD of six independent experiments. The values with different letters are considered as significantly different at p < 0.05 between two groups.
We also studied the suppressive effect of PNA or Δ7-ETrA on the over-expression of the major inflammatory biomarker COX-2 in mouse ear biopsy. Figure 4D shows the time course of COX-2 expression in mouse ear tissue in response to TPA (5 μg/10 μL) treatment for different time periods (0, 1, 2, 4, and 8 h). A stimulation period of 2 to 8 h proved to be optimal for studying the modulation of COX-2 expression. COX-2 was over-expressed after 2 h of TPA stimulation; however, over-expression of the enzyme was significantly suppressed to 53%, 59%, and 72% when the mouse ear was injected with PNA, Δ7-ETrA, or dexamethasone (Fig. 4E), respectively.
In a separate study, results of flow cytometric analysis showed that infiltration of different types of immune cells in mouse ear tissue, including leukocytes (CD45+), neutrophils (Ly6G+CD45+), and macrophages (F4/80+CD45+) was evident after 6 h of TPA stimulation (Fig. 5). However, topical injection of PNA or Δ7-ETrA before the TPA administration significantly reduced the numbers of infiltrated immune cells as compared with the TPA group.
Evaluation of TPA-induced immune cells by flow cytometry in mouse ear after intradermal injection of PNA or Δ7-ETrA. PNA, Δ7-ETrA or vehicle was intradermally injected and incubated for 18 h, followed by the TPA injection. Six hours after TPA injection, flow cytometric analysis of the inflammatory cells harvested from TPA-induced ear tissues was performed. Cell suspensions were incubated with anti-CD45/PerCP, anti-Ly6G/FITC, and anti-F4/80/PE, and analyzed by flow cytometry. The bars indicate the mean ± SD of four independent experiments. The values with different letters are considered as significantly different at p < 0.05 between two groups.
Effect of PNA on TPA-Induced Inflammatory Mediator Production in Mouse Back Skin
To investigate how PNA might exert its anti-inflammatory effects, a fixed amount of PNA or Δ7-ETrA was topically administered on mouse back skin for 18 h, followed by 24-h TPA administration to stimulate pro-inflammatory mediator synthesis. TPA significantly increased production of IL-1β, IL-6, TNF-α, and PGE2 in the TPA-stimulated group of animals (Fig. 6). Topical administration of PNA or Δ7-ETrA reduced the production of IL-1β by 79% or 55%, respectively (Fig. 6A). As for pro-inflammatory IL-6, PNA had a greater suppressive effect on IL-6 production (68%) than Δ7-ETrA (39%) (Fig. 6B). A comparable suppressive effect of PNA and Δ7-ETrA on production of TNF-α and PGE2 was observed (Fig. 6C and D).
Effects of PNA or Δ7-ETrA on the production of IL-1β (A), IL-6 (B), TNF-α (C), and PGE2 (D) in TPA-stimulated dorsal skin. PNA, Δ7-ETrA or vehicle was topically applied to the shaved back skin. After 18 h, TPA was applied onto the same location of back skin. The cell-free supernatants of back skin tissue homogenates were then analyzed using commercial enzyme immunoassay kits, respectively. Results are representative of three independent experiments. Data are expressed as mean ± SD. The values with different letters are considered as significantly different at p < 0.05 between the groups.
Effect of PNA on MAPK Activation in Mouse Back Skin
Relative to the non-stimulated control, topical administration of TPA onto mouse dorsal skin surface promoted phosphorylation of MAPK after 2 h stimulation (data not shown). Topical treatment of PNA or Δ7-ETrA prior to the TPA stimulation suppressed the expression of phosphorylated p38 by 55% and 81%, and JNK by 32% and 58%, respectively (Fig. 7). However, no such effect on the expression of phosphorylated ERK-MAPK was observed.
Effect of PNA or Δ7-ETrA on activated MAPK expression in TPA-stimulated mouse back skin. PNA, Δ7-ETrA or vehicle was topically applied to the shaved back skin. After 18 h, TPA was applied onto the same location of back skin. Minced mouse back skin tissues were analyzed for protein. The levels of phosphorylated p38, ERK, and JNK were determined by western blot. Results are representative of three independent experiments. Data are expressed as mean ± SD. The values with different letters are considered as significantly different at p < 0.05 between the groups.
DISCUSSION
The main finding of this study was that PNA and its elongated metabolite Δ7-ETrA exert their anti-inflammatory properties in both cell culture and animal models, in part at least, by suppressing inflammatory responses. This in vivo inhibitory effect of both rare PUFA on ear edema and pro-inflammatory mediator production could be due, in part, to the suppression of p38- and JNK-MAPK activation.
In this study, using human differentiated THP-1 macrophages, we first documented the suppressive effect of PNA on the production of pro-inflammatory mediators, similar result with those of our previous findings in human breast cancer cells [9], murine primary peritoneal macrophages, RAW264.7 macrophages [8], and BV-2 microglia [10]. We also confirmed that incorporation of PNA into macrophage lowered the proportion of phospholipid AA (Table 1). The substitution of AA by PNA and Δ7-ETrA might reduce the amount of AA substrate available for the production of pro-inflammatory eicosanoids [5]. We inferred that the more PNA and/or Δ7-ETrA incorporated into cellular phospholipids, the greater the chance that both free NMIFA released by the action of phospholipase A2 (PLA2) would competitively inhibit PGE2 production by competing with free AA for the catalytic site of COX-2 [8]. The results in Table 1 show that the proportions of LA and EDA were significantly increased (by up to 8.8- and 2.5-fold relative to the control) when differentiated macrophages were incubated with PNA. However, no such increase in both fatty acids was observed when PNA was supplemented into the culture of murine RAW264.7 macrophages [7], murine BV-2 microglial cells [10], and human HaCaT cells (data not shown). Previously, Das and colleagues demonstrated that TPA-activated Δ6-desaturase activities by increasing the conversion of LA to GLA in TPA-differentiated HL60 cells [17]. Horrobin (1993) reported that a small portion of LA could be elongated to EDA, when Δ6-desaturation of LA to GLA is blocked in mammalian cells [18]. Taken together, these results are consistent with our hypothesis that PNA significantly inhibits the activity of Δ6-desaturase in TPA-differentiated macrophages and consequently the conversion of LA to GLA, thereby accounting, in part at least, for the marked increase in the accumulation of LA and EDA, and the decreased proportion of AA in cellular phospholipids. PNA incorporation into phospholipids also impacted phospholipid fatty acid composition (Fig. 2b), modified membrane structure and fluidity, and affected the mobility of receptors and membrane proteins as well, thereby regulate influencing receptor-mediated signal transduction cascades, such as MAPK and NF-κB signaling as previously described [19,20,21,22].
The key contribution of this study is that it documents the ability of PNA and Δ7-ETrA to significantly suppress TPA-induced ear edema by lowering both ear thickness and biopsy weight, inhibiting COX-2 expression and reducing infiltrated immune cells (Figs. 4 and 5). When we further explored the mechanisms underlying the in vivo anti-inflammatory effect of both NMIFA, we discovered a discrepancy between studies conducted in cell culture versus those performed using experimental animals. Based on results of fatty acid analysis, no detectable amounts of PNA or Δ7-ETrA in ear biopsy sample were found (data not shown). This is likely because only a small amount (3 μg) of PNA or Δ7-ETrA was injected into the ear. Once injected PUFA was diffused or/and metabolized, less of them could substitute phospholipid AA, and further competed for COX-2 with AA in ear. This observation is inconsistent with results of previous studies which documented that in cultured cells, cellular fatty acid composition and lipid-derived pro-inflammatory mediator production could be manipulated by dietary PUFA supplementation [5, 23, 24]. In contrast, the results in Fig. 7 show that levels of phosphorylated p38- and JNK-MAPK were reduced after topical application of PNA or Δ7-ETrA to mouse dorsal skin, indicating that inhibition of signal transduction rather than PUFA incorporation is the major mechanism responsible for reducing pro-inflammatory mediator production. Nevertheless, we acknowledge that down-regulating the initiation of intracellular signaling cascades might also play a role in suppressing inflammatory responses. Recent studies showed that supplementation of primary human intestinal microvascular endothelial cells (HIMEC), human MCF-7 breast cancer cells or murine RAW264.7 macrophages with PUFA, such as DHA and Δ7-ETrA, significantly reduced toll-like receptor-4 (TLR4) expression, resulting in the inhibition of IL-1β- or LPS-induced NF-κB and MAPK signaling and downstream pro-inflammatory mediator production [8, 25, 26]. Therefore, we herein suggest that in vivo anti-inflammatory effect of PNA or Δ7-ETrA might be also attributed to the suppression of TLR4-mediated p38- and JNK-MAPK signaling.
To further investigate the suppressive effects of PNA on ear edema and skin inflammation, we tested the effects of GLA, the positional isomer of PNA, on inflammatory responses in both in vitro and in vivo studies [27, 28]. Fan and Chapkin (1998) reported that GLA is readily elongated to DGLA, and that a small portion of DGLA can be further metabolized to the powerful anti-inflammatory prostaglandin E1 (PGE1) by the action of COX-2 [29]. Furthermore, DGLA can be oxygenated to 15-hydroxy-eicosatrienoic acid (15-HETrE) by 15-lipoperoxidase (15-LOX), which in turn suppresses the 5-lipoperoxidase (5-LOX)-mediated synthesis of pro-inflammatory mediators derived from AA, such as leukotrienes and thromboxane [30, 31]. Therefore, we speculate that PNA and its elongation product Δ7-ETrA are metabolized by COX-2, 15-LOX, or other enzymes induced by LPS or similar inflammatory substances, and that the novel compounds derived from PNA might suppress inflammatory responses, including lowering PGE2 production as previously reported [7, 8]. This proposed set of fatty acid reactions would also account for the fact that no suppressive effect was observed when macrophage cells were co-incubated with PNA and LPS together [7], or mouse ears were co-injected with TPA and PNA at the same time in this study (data not shown). Collectively, the anti-inflammatory effect of PNA might highly associated with the LPS or TPA stimulation after 24 h PNA administration, resulting in the synthesis of PNA-derived bioactive metabolite, which might be involved in the modulation of immune regulation. Future investigation of the existence of yet-to-be discovered PNA metabolites and their biological evaluation are warranted.
A current limitation for application of this study is that free PNA, Δ7-ETrA, or other PUFA is unstable, and this fact would raise concerns and reduce interest in free fatty acids as a future therapeutic agent. A suitable delivery system is required to ensure PNA can be preserved and successfully delivered into skin before and after intradermal injection or topical administration. Future in vivo studies involving in formulation design on the suppressive effects of PNA-containing agents on inflammatory responses are required.
In summary, we have demonstrated that PNA suppresses inflammatory responses in both cell culture and mouse-model studies. The in vivo anti-inflammatory effect of PNA and Δ7-ETrA on mouse ear edema and dorsal inflammation could be due, in part, to the suppression of p38- and JNK-MAPK activation. We speculate that novel metabolites derived from PNA and Δ7-ETrA could contribute to the suppressive effect of relatively small amounts of both of these NMIFA. Our findings supported that PNA and Δ7-ETrA are two potential anti-inflammatory agents for modulating in vitro and in vivo immune responses involved in inflammation.
References
Sugano, M., I. Ikeda, K. Wakamatsu, and Y. Oka. 1994. Influence of Korean pine (Pinus koraiensis)-seed oil containing cis-5, cis-9, cis-12-octadecatrienoic acid on polyunsaturated fatty acid metabolism, eicosanoid production and blood pressure. British Journal of Nutrition 72: 775–783.
Wolff, R.L., O. Lavialle, F. Pédrono, E. Pasquier, L.G. Deluc, A.M. Marpeau, and K. Aitzetmüller. 2001. Fatty acid composition of Pinaceae as taxonomic markers. Lipids 36: 439–451.
Wolff, R.L., W.W. Christie, F. Pédrono, and A.M. Marpeau. 1999. Arachidonic, eicosapentaenoic, and biosynthetically related fatty acids in the seed lipids from a primitive gymnosperm, Agathis robusta. Lipids 34: 1083–1097.
Leonard, A.E., B. Kelder, E.G. Bobik, L.-T. Chuang, J.M. Parker-Barnes, J.M. Thurmond, P.E. Kroeger, J.J. Kopchick, Y.-S. Huang, and P. Mukerji. 2000. cDNA cloning and characterization of human ∆5-desaturase involved in the biosynthesis of arachidonic acid. Biochemical Journal 347: 719–724.
Innes, J.K., and P.C. Calder. 2018. Omega-6 fatty acids and inflammation. Prostaglandins, Leukotrienes and Essential Fatty Acids 132: 41–48.
Tanaka, T., T. Takimoto, J.-I. Morishige, Y. Kikuta, T. Sugiura, and K. Satouchi. 1999. Non-methylene-interrupted polyunsaturated fatty acids: Effective substitutes for arachidonate of phosphatidylinositol. Biochemical and Biophysical Research Communication 264: 683–688.
Chuang, L.-T., P.-J. Tsai, C.-L. Lee, and Y.-S. Huang. 2009. Uptake and incorporation of pinolenic acid reduces n-6 polyunsaturated fatty acid and downstream prostaglandin formation in murine macrophage. Lipids 44: 217–224.
Huang, W.-C., P.-J. Tsai, Y.-L. Huang, S.-N. Chen, and L.-T. Chuang. 2014. PGE2 production suppressed by chemically-synthesized Δ7-eicosatrienoic acid in macrophages through the competitive inhibition of COX-2. Food and Chemical Toxicology 66: 122–133.
Chen, S.-J., C.-P. Hsu, C.-W. Li, J.-H. Lu, and L.-T. Chuang. 2011. Pinolenic acid inhibits human breast cancer MDA-MB-231 cell metastasis in vitro. Food Chemistry 126: 1708–1715.
Chen, S.-J., L.-T. Chuang, J.-S. Liao, W.-C. Huang, and H.-H. Lin. 2015. Phospholipid incorporation of non-methylene-interrupted fatty acids (NMIFA) in murine microglial BV-2 cells reduces pro-inflammatory mediator production. Inflammation 38: 2133–2145.
Tanaka, T., T. Hattori, M. Kouchi, K. Hirano, and K. Satouchi. 1998. Non-methylene-interrupted polyenoic fatty acids: Structural characterization and metabolism by fatty acid chain elongation system in rat liver. In Essential fatty acids and eicosanoids, ed. R.A. Tiemersma, R. Armstrong, R.W. Kelly, and R. Wilson, 229–233. Champaign: American Oil Chemists’ Society Press.
Pasquier, E., W.M. Ratnayake, and R.L. Wolff. 2001. Effects of delta5 polyunsaturated fatty acids of maritime pine (Pinus pinaster) seed oil on the fatty acid profile of the developing brain of rats. Lipids 36: 567–574.
Folch, J., M. Lees, and G.H. Sloane-Stanley. 1957. A simple method for the isolation and purification of total lipids from animal tissues. Journal of Biological Chemistry 226: 497–509.
Robertson, F.M., M.S. Ross, K.L. Tober, B.W. Long, and T.M. Oberyszyn. 1996. Inhibition of pro-inflammatory cytokine gene expression and papilloma growth during murine multistage carcinogenesis by pentoxifylline. Carcinogenesis 17: 1719–1728.
Huang, W.-C., T.-H. Tsai, C.-J. Huang, Y.-Y. Li, J.-H. Chyuan, L.-T. Chuang, and P.-J. Tsai. 2015. Inhibitory effects of wild bitter melon leaf extract on Propionibacterium acnes-induced skin inflammation in mice and cytokine production in vitro. Food and Function 6: 2550–2560.
Tsai, P.-J., W.-C. Huang, M.-C. Hsieh, P.-J. Sung, Y.-H. Kuo, and W.-H. Wu. 2016. Flavones isolated from Scutellariae radix suppress Propionibacterium acnes-induced cytokine production in vitro and in vivo. Molecules 21: 15.
Das, U.N., M.E. Begin, and G. Ells. 1992. Fatty acid changes during the induction of differentiation of human promyelocytic leukemia (HL-60) cells by phorbolmyristate acetate. Prostaglandins, Leukotrienes and Essential Fatty Acids 146: 235–239.
Horrobin, D.F. 1993. Fatty acid metabolism in health and disease: The role of delta-6-desaturase. American Journal of Clinical Nutrition 57: 732S–736S.
Wong, S.W., M.J. Kwon, A.M. Choi, H.P. Kim, K. Nakahira, and D.H. Hwang. 2009. Fatty acids modulate Toll-like receptor 4 activation through regulation of receptor dimerization and recruitment into lipid rafts in a reactive oxygen species-dependent manner. Journal of Biological Chemistry 284: 27384–27392.
Kim, W., N.A. Khan, D.N. McMurray, I.A. Prior, N. Wang, and R.S. Chapkin. 2010. Regulatory activity of polyunsaturated fatty acids in T-cell signaling. Progress in Lipid Research 49: 250–261.
Tsai, P.-J., W.-C. Huang, S.-W. Lin, S.-N. Chen, H.-J. Shen, H. Chang, and L.-T. Chuang. 2018. Juniperonic acid incorporation into the phospholipids of murine macrophage cells modulates pro-inflammatory mediator production. Inflammation 41: 1200–1214.
Monmai, C., S.H. Go, I.S. Shin, S.G. You, H. Lee, S.B. Kang, and W.J. Park. 2018. Immune-enhancement and anti-inflammatory activities of fatty acids extracted from Halocynthia aurantium tunic in RAW264.7 cells. Marine Drugs 16: E309.
McDaniel, J.C., K. Massey, and A. Nicolaou. 2011. Fish oil supplementation alters levels of lipid mediators of inflammation in microenvironment of acute human wounds. Wound Repair and Regeneration 19: 189–200.
Raederstorff, D., M. Pantze, H. Bachmann, and U. Moser. 1996. Anti-inflammatory properties of docosahexaenoic and eicosapentaenoic acids in phorbol-ester-induced mouse ear inflammation. International Archives of Allergy and Immunology 111: 284–290.
Hwang, J.K., H.N. Yu, E.M. Noh, J.M. Kim, O.Y. Hong, H.J. Youn, S.H. Jung, K.B. Kwon, J.S. Kim, and Y.R. Lee. 2017. DHA blocks TPA-induced cell invasion by inhibiting MMP-9 expression via suppression of the PPAR-γ/NF-κB pathway in MCF-7 cells. Oncology Letters 13: 243–249.
Ibrahim, A., K. Mbodji, A. Hassan, M. Aziz, N. Boukhettala, M. Coëffier, G. Savoye, P. Déchelottec, and R. Marion-Letelliera. 2011. Anti-inflammatory and antiangiogenic effect of long-chain n-3 polyunsaturated fatty acids in intestinal microvascular endothelium. Clinical Nutrition 30: 678–687.
Ziboh, V.A. 1996. The biological/nutritional significance of γ-linolenic acid in the epidermis: metabolism and generation of potent biological modulators. In γ-Linolenic acid: Metabolism and its roles in nutrition and medicine, ed. Y.-S. Huang and D.E. Mills, 118–128. Champaign: American Oil Chemists’ Society Press.
Simon, D., P.A. Eng, S. Borelli, R. Kägi, C. Zimmermann, C. Zahner, J. Drewe, L. Hess, G. Ferrari, S. Lautenschlager, B. Wüthrich, and P. Schmid-Grendelmeier. 2014. Gamma-linolenic acid levels correlate with clinical efficacy of evening primrose oil in patients with atopic dermatitis. Advances in Therapy 31: 180–188.
Fan, F.-Y., and R.S. Chapkin. 1998. Importance of dietary γ-linolenic acid in human health and nutrition. Journal of Nutrition 128: 1411–1414.
Ziboh, V.A., S. Naguwa, K. Vang, J. Wineinger, B.M. Morrissey, M. Watnik, and M.E. Gershwin. 2004. Suppression of leukotriene B4 generation by ex-vivo neutrophils isolated from asthma patients on dietary supplementation with gammalinolenic acid-containing borage oil: possible implication in asthma. Clinical and Developmental Immunology 11: 13–21.
Sergeant, S., E. Rahbar, and F.H. Chilton. 2016. Gamma-linolenic acid, dihommo-gamma linolenic, eicosanoids and inflammatory processes. European Journal of Pharmacology 785: 77–86.
Acknowledgments
The authors are grateful to Professor Robert H. Glew, PhD, for editing our manuscript.
Funding
This work was supported in part by research grants from the Ministry of Science and Technology, Executive Yuan, Taiwan (MOST 104-2320-B-264-002- and MOST 105-2320-B-264-001) and the Tao Yuan General Hospital, Ministry of Health and Welfare, The Executive Yuan, Taiwan (PTH10408), respectively.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All procedures were approved by the Institutional Animal Care and Use Committee of Yuanpei University of Medical Technology (IACUC Approval No. LAC10301).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, SJ., Huang, WC., Shen, HJ. et al. Investigation of Modulatory Effect of Pinolenic Acid (PNA) on Inflammatory Responses in Human THP-1 Macrophage-Like Cell and Mouse Models. Inflammation 43, 518–531 (2020). https://doi.org/10.1007/s10753-019-01134-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-019-01134-7