Abstract
In this study, we evaluated the effects of high-intensity swimming in an experimental model of acute lung injury (ALI) induced by lipopolysaccharide (LPS) on lung inflammation and antioxidant defenses. Balb/C male mice were submitted to exercise (30 min/day, 5 days/week, for a period of 3 weeks) prior to LPS instillation in the lung. Twenty-four hours after delivery of LPS (10 μg/animal), mice were euthanized and bronchoalveolar fluid (BALF) was obtained for cell counting and analysis of cytokines by ELISA. Lung tissue was used to evaluate antioxidant defenses. LPS instillation resulted in an increase in total and mononuclear cells, IL-1β, TNF-α, and IL-6 in BALF. LPS instillation also altered IL-10 and IL-ra levels in BALF and induced antioxidant defenses (glutathione, superoxide dismutase, catalase, and glutathione peroxidase) in the lung. Protein carbonyl increased in the LPS-treated animals. High-intensity swimming prevented all these changes induced by LPS. Significance: Therefore, this experimental protocol of high-intensity swimming showed a protective effect on ALI, decreasing inflammatory processes and preventing disturbances in antioxidant defenses into the lungs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Acute lung injury (ALI) or acute respiratory distress syndrome (ARDS) is the result of acute lung inflammation and noncardiogenic pulmonary edema that leads to a diffuse heterogeneous lung injury [1,2,3]. It is characterized by intense increase in neutrophil influx, pulmonary vascular permeability, and proinflammatory mediators, as well as marked endothelial and bronchial damage [1]. Furthermore, ALI may occur secondary to different etiologies, exhibiting high mortality rates [1,2,3].
Experimental ALI models have been developed to evaluate the pathophysiological mechanisms, mostly based on risk factors for the human condition, such as sepsis, gastric aspiration, reperfusion of ischemic tissue, multiple transfusions, trauma, and mechanical ventilation [4, 5]. Among several experimental models, lipopolysaccharide (LPS) administration is a well-known and established experimental model of ALI [5]. LPS promotes an inflammatory response, increasing the number of macrophages and neutrophils in bronchoalveolar lavage fluid (BALF). The increase in inflammatory cytokines, such as TNF-α, IL-1β, and IL-6, is believed to depend on LPS-induced Toll-like 4 receptor (TLR4) activation [4, 6]. In addition, an increase of oxidative stress can amplify deleterious effects of ALI [7,8,9].
The pulmonary inflammatory progression can extend for several days, which may compromise the physical conditions of patients. Clinical and experimental studies have shown that regular aerobic exercise can prevent or even abolish the development of a number of diseases, especially in intensive care unit patients. This beneficial effect of exercise has been associated to an anti-inflammatory and antioxidant protection [10,11,12,13].
Despite apparent clear benefits, the dosing of exercise intensity remains to be determined. Balducci et al. [14], for instance, demonstrated that subjects with type 2 diabetes submitted to high-intensity exercise presented a significant improvement in their inflammatory condition. High-intensity exercise decreased lung inflammation and improved oxidative status in experimental models of allergic pulmonary inflammation [15] and pollutant exposure [12]. However, little is known about the possible protective effects of high-intensity exercise training in the LPS model of pulmonary inflammation, an experimental acute condition of ALI. This highlights the need for additional experiments. Therefore, we evaluated if high-intensity exercise training can prevent pulmonary inflammation and oxidative stress-related parameters induced by LPS instillation in the lungs of mice.
MATERIALS AND METHODS
Design
This study was approved by the Review Board for Animal Studies of the Federal University of Santa Catarina (PP 00745). All animals in this study received humane care in compliance with EU Directive 2010/63/EU, which provides guidelines for animal experiments. Forty male BALB/c mice, aged 6–8 weeks (20–25 g) from our animal facility were maintained in conditions that were controlled for temperature (22 ± 2 °C), humidity (70–75%), and dark/light cycle (12 h, lights on at 06:00 am). All procedures and surgeries were approved under the Guide for the Care and Use of Laboratory Animals (National Research Council) and the Guidelines of the local University Animal Care and Use Committee.
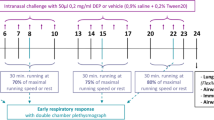
Animals were distributed into four groups, as follows (Fig. 1): (a) control group (C), mice not subjected to the swimming protocol, receiving only orotracheal saline instillation; (b) swimming group (Sw), animals submitted to the swimming protocol (30 min/day) for 15 days, and receiving orotracheal saline instillation; (c) LPS group (LPS), mice subjected to the orotracheal LPS instillation, but not submitted to the swimming protocol; (d) swimming+LPS group (Sw+LPS), mice subjected to the swimming protocol, and LPS orotracheal instillation.
High-Intensity Swimming Protocol
The swimming protocol was adapted from Kuphal et al. [16]. A box containing 35 L of water was separated into eight lanes. Soap (1 mL) was added in order to reduce surface tension and to avoid floating. The Sw and Sw+LPS groups were initially adapted to the water environment for 4 days: day 1, two periods of 30 s swimming, and a 2-h interval between swimming periods; day 2, two periods of 2 min of swimming and a 2-h interval; day 3, three periods of 10 min of swimming and a 5-min interval; and day 4, two periods of 15 min of swimming with a 5-min interval. After the adaptive period, mice were submitted to swimming for 30 min with no pause, from the 5th to the 20th day [12, 15].
The exercise intensity was determined using an adapted protocol, as stated before [17]. This protocol was considered a high-intensity exercise model, since lactate concentration in the blood remained greater than 1 mmol/L [12, 15, 17].
LPS Administration
Twenty four hours after the last swimming session, the LPS and Sw+LPS mice groups received an orotracheal instillation of 10 μg of Escherichia coli LPS (L3755, Sigma-Aldrich, St. Louis, MO, USA) suspended in 50 μL of phosphate buffered-saline (PBS). Animals from the control and Sw groups received orotracheal instillation (50 μL) of saline solution (0.9%). Animals were anesthetized with ketamine (100 mg/kg) and xylazine (10 mg/kg) intraperitoneally, prior the instillation administered by using a micropipette. The harvest was performed 24 h after LPS or saline instillation, as shown in Fig. 1.
Bronchoalveolar Lavage Fluid (BALF)
Twenty-four hours after LPS instillation, animals were anesthetized with ketamine (100 mg/kg, IP) and xylazine (10 mg/kg) intraperitoneally, and mice were euthanized by rapid exsanguination by sectioning the abdominal aorta.
A tracheotomy was performed for BALF collection, and lungs were gently rinsed three times with 0.5 mL of PBS (pH 7.2) via a tracheal cannula. After BALF collection, the chest was opened, and the heart-lung block was removed. Lungs were divided and tissue samples were weighted and separated to oxidative stress analysis.
The total cell number was counted in a Neubauer hemocytometer chamber. We also performed the differential cell count of 300 cells/mouse from BALF, after Diff-Quick staining of slides. All measurements were performed in a blinded fashion.
Analysis of Cytokines and Oxidative Stress-Related Parameters
The lung levels of TNF-α, IL-1β, IL-6, IL-10, and IL-1ra were measured from BALF by ELISA technique, according to the manufacturer’s instructions (DuoSet ELISA R&D Systems, Minneapolis, MN, USA). Results were expressed as picograms per milliliter.
Samples of fresh lung tissue (right lung) weighing approximately 40–50 mg were homogenized in HEPES buffer (20 mM, pH 7.0) and centrifuged at 20,000g, 20 min, 4 °C, and supernatant was used for enzymatic analyses and protein carbonyl.
The total glutathione (GSH-t) was measured using the Tietze method modified by Akerboom and Sies [18]. Samples were added to a reaction mixture containing 0.1 M phosphate buffer, pH 7.4, 1 mM EDTA, 0.2 mM NADPH, 0.1 mM DTNB and 0.05 U of glutathione reductase. TNB formation was followed for 5 min at 412 nm and sample t-GSH was calculated based on a standard curve.
Glutathione peroxidase (GPx) activity was measured as previously described [19]. Samples were added to a reaction mixture containing phosphate buffer 0.1 M pH 7.0, 1 mM EDTA, 1 mM GSH, 0.2 U/mL GR, and 0.2 mM NADPH. Reaction was initiated by adding 1 mM of cumene hydroperoxide and decrease in absorbance due to NADPH consumption was followed at 340 nm for 5 min.
Catalase (CAT) was analyzed by following the decrease in absorbance at 240 nm due to H2O2 decrease [20]. Samples were assayed in 50 mM phosphate buffer, pH 7.0, 0.5 mM EDTA and 0.012% triton X-100. The reaction was initiated by adding 10 mM H2O2.
Superoxide dismutase (SOD) activity was measured according to [21]. Reaction buffer consisted of trietanolamine-diethanolamine buffer (100 mM, pH 7.4, 2.5 mM EDTA, 1.25 mM MnCl2, 0.3 mM NADH, and 1 mM 2-mercaptoethanol). Absorbance was followed at 340 nm for 5 min.
Samples were probed by dot blot for protein carbonyl content as previously described [22]. Briefly, proteins were denatured with 6% SDS and derivatized with 20 mM DNPH in 2 N HCl for 1 h at room temperature. After incubation, samples were neutralized with Tris 2 M/Glycerol 30 and 5% β-mercaptoethanol was added. A 2 μL aliquot (0.2 μg of protein) was spotted into an activated PVDF membrane and allowed to air-dry. Excess DNPH was removed by rinsing membranes with acetic acid. Membranes were blocked with nonfat dried milk and immunoblotted with anti-DNP antibody (Abcam Ab6306, 1:10000) and detected by chemiluminescence. All measurements were performed in a blinded fashion.
Statistical Analysis
Comparisons among groups were performed using Sigma Stat 3.5 software (California, EUA, 2005) by two-way analysis of variance (ANOVA), followed by Holm-Sidak test for multiple comparisons. Data showed normal distribution, analyzed by the Kolmogorov-Smirnov test. Significance levels were set at 5% (p < 0.05). Values were expressed as the mean ± SEM.
RESULTS
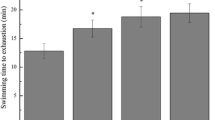
Swimming Sessions Decreased the Number of Cells in BALF
Figure 2A shows the total number of cells from the BALF. LPS instillation resulted in a fourfold increase in the total number of cells, as compared to other groups. A two-way ANOVA showed a significant effect for LPS [F(1,32) = 68.50; p < 0.001], and for the Sw×LPS interaction [F(1,32) = 40.57; p < 0.001]. LPS or exercise alone did not alter the number of mononuclear cells in BALF, however the high-intensity swimming training resulted in decreased number of these cells, as compared to the LPS group (Fig. 2B). The two-way ANOVA showed a significant effect for Sw×LPS interaction [F(1,13) = 7.15; p = 0.002].
Swimming Sessions Prevented Pulmonary Induction of Pro-inflammatory Cytokines
LPS exposure resulted in a significant increase in IL-1β (Fig. 3A), TNF-α (Fig. 3B), and IL-6 (Fig. 3C) levels in the lung. The two-way ANOVA showed a significant effect of LPS for IL-1β [F(1,19) = 8.59; p = 0.009], TNF-α [F(1,16) = 10.17; p = 0.007], and IL-6 [F(1,16) = 35.5; p < 0.001]. The swimming sessions did not affect the levels of pro-inflammatory cytokines, but completely abolished the increase induced by LPS instillation. The two-way ANOVA showed a significant effect of Sw×LPS interaction for IL-1β [F(1,19) = 5.17; p < 0.001]; TNF-α [F(1,16) = 5.34; p = 0.03]; and IL-6 [F(1,16) = 31.08; p < 0.001].
Effect of LPS Instillation on Anti-inflammatory Cytokines
LPS instillation resulted in an increase of IL-10 lung levels (Fig. 4A). The two-way ANOVA showed a significant effect for LPS [F(1,15) = 7.97; p = 0.01] and for exercise [F(1,15) = 10.4; p = 0.004]. Simultaneously, the lung levels of IL-1ra decreased in the LPS group, since the two-way ANOVA showed a significant effect for LPS [F(1,17) = 6.44; p = 0.02]. Interestingly, this decrease was not significantly attenuated by swimming sessions [F(1,17) = 1.13; p = 0.3] (Fig. 4B).
Effect of Swimming Training on Oxidative Stress-Related Parameters in the Lung Tissue
Figure 5A shows an increase of the lung levels of GSH-t induced by LPS. High-intensity swimming prevented this increase in GSH-t levels. The two-way ANOVA showed a significant effect for LPS [F(1,26) = 15.7; p < 0.001], for Sw [F(1,26) = 23.12; p < 0.001], but not for Sw×LPS interaction [F(1,26) = 3.03, p = 0.09].
The instillation of LPS resulted in an increased SOD activity (Fig. 5B) in the lung tissue, when compared to the control group. Swimming training prevented this increase in SOD activity. The two-way ANOVA showed a significant effect for LPS [F(1,18) = 43.75; p < 0.001] and LPS×Sw interaction [F(1,18) = 25.71; p < 0.001].
The instillation of LPS did not alter GPx activity (Fig. 5C) in the lung tissue, when compared to the control group. The two-way ANOVA showed a significant effect for exercise [F(1,19) = 24.46; p = 0.003], and for LPS×Sw interaction [F(1,19) = 4.74; p = 0.04].
Similarly, LPS effect on high-intensity exercise alone did not alter lung CAT activity (Fig. 5D), but a tendency to increase was reverted by exercise training. The two-way ANOVA was significant for Sw [F(1,15) = 11.8; p = 0.004] and for LPS×Sw interaction [F(1,15) = 11.88; p = 0.004].
Oxidative damage was detected by oxidative modification of proteins as carbonyl content. As depicted in Fig. 6, LPS instillation in the lung induced an increase in carbonyl content and high-intensity exercise training prevented this increase.
DISCUSSION
The inflammatory cell influx to the lungs is one of the most characteristic features of ALI at early stages [23, 24]. Despite the massive migration of cells to BALF induced by LPS treatment, the high-intensity swimming group presented lower mononuclear and total cell count, as compared to the Sw group. These results corroborate previous data, showing that low-intensity swimming decreases cell infiltration in an animal model of ALI by using intranasal instillation of LPS [25]. Nevertheless, low-intensity daily exercise for 5 weeks was unable to prevent the increase in total cell count as well as lymphocyte infiltration in BALF in the same model [26]. In another study, low-intensity exercise during 4 weeks decreased cell count and improved lung function after Streptococcus pneumoniae infection [27]. Thus, the reasons that low-intensity exercise is not always effective in preventing lung infiltration of inflammatory cells are not clear. These differences may be attributed, in part, to the exercise protocol applied, since the type, the timing of implementation of aerobic exercise, and the induction pathway can result in distinctive outcomes, as reviewed [28]. The high-intensity swimming protocol used here was also effective in decreasing the cell count in BALF in experimental models of allergic asthma induced by exposure to ovalbumin or diesel exhaust particles [12, 15].
In fact, an increase in cell influx to the lungs in LPS-induced ALI is closely related to cell recruitment by pro-inflammatory cytokines, such as TNF-α and IL-1β [29]. In this study, we showed that IL-1β, TNF-α, and IL-6 were increased in the BALF of the LPS group, corroborating previous experimental studies [6, 26, 29]. Activated monocytes and macrophages are the major in vivo sources of endogenous TNF-α synthesis [30]. In our experiment, mononuclear cell count was decreased and the increase in TNF-α levels induced by LPS was abolished, reinforcing the anti-inflammatory effects of high-intensity swimming.
TNF-α leads to the secretion of various cytokines, such as IL-1β and IL-6, two potent mediators of lung inflammatory response, which play a leading role in an inflammatory cascade response in ALI [31]. In our study, high-intensity swimming performed before ALI induction prevented the increase of IL-1β and IL-6 levels in BALF of LPS-treated mice. These results contrast to low-intensity exercise response that failed to prevent LPS-induced increase in BALF IL-1β and IL-6. In this same experiment, the exercise protocol even potentiated the LPS effect in promoting IL-1β increase [26]. Nevertheless, low-intensity exercise is able to ameliorate lung function and to prevent the TNF-α increase in the lung of LPS treated mice, which was not the case for IL-1β [25, 26]. In this regard, high-intensity exercise may have a better therapeutic value, since LPS-induced increase in IL-1β and IL-6 was attenuated by the present swimming protocol.
It is already known that aerobic exercise can increase IL-10 levels, systemic and/or locally. Interestingly, some studies also described a resolving role of IL-10 in ALI [13], emphasizing the importance of controlling the initial inflammatory stages of ALI. This can be accomplished by decreasing the alveolar cell influx [32], as shown in Fig. 2. Furthermore, in our study, the levels of IL-10 in BALF were significantly increased in the swimming and LPS groups, which was not altered by the swimming protocol. In addition, the LPS group showed a decrease of BALF IL-1ra, while the swimming protocol prevented this decrease. These data reinforce the idea that high-intensity exercise has beneficial effects by preventing the increase in pro-inflammatory and ameliorating the levels of anti-inflammatory cytokines (IL-10 and IL-1ra).
Studies have suggested that an imbalance between oxidants and antioxidants is deeply involved in the pathogenesis of ALI [33]. In this context, the generation of reactive oxygen species (ROS) is increased. There are numerous potential sources of ROS, including infiltrated leukocytes (neutrophils), parenchymal cells (epithelial and endothelial cells), and circulating oxidant-generating enzymes [34]. Clinical and preclinical studies have demonstrated that the levels of oxidatively damaged proteins are increased in the BALF of ARDS patients and LPS-treated animals [35, 36].
It has been found that LPS treatment can induce SOD in the rodent lung [27, 37, 38], as well as catalase [39] and glutathione peroxidase [27]. Glutathione synthesis was increased significantly in several tissues, including the lung of septic animals, leading to an increment in glutathione levels during the acute phase of sepsis [40, 41]. These increased antioxidant defenses may be a consequence of Nrf2 activation [42, 43]. However, at different dosing or time points decrease in antioxidant defenses has also been reported [44,45,46]. In this study, LPS responses are in line with the observation of increased antioxidant defenses (GSH, SOD, and CAT).
A 2-month protocol of physical exercise before LPS instillation may prevent the oxidative damage caused by experimental lung injury, suggesting that exercise may have an important protective role [47, 48]. Since the inflammation process seems to be reduced by exercise, the signaling controlling antioxidant response, such as Nrf2 activation [43], may be weakened. Thus, the maintenance of GSH-t levels and GPx, SOD, and CAT activity at control levels suggests an attenuation of oxidative damage. This idea is reinforced by the finding that LPS-induced protein oxidation was prevented by the high-intensity swimming protocol (Fig. 6).
CONCLUSIONS
Overall, a 3-week protocol of high-intensity swimming prior to LPS-induced ALI was able to prevent the increase in inflammatory markers in BALF, including inflammatory cell count, and pro-inflammatory cytokines (IL-1β, TNF-α, and IL-6). Furthermore, changes in anti-inflammatory cytokines (IL-1ra and IL-10), antioxidant defenses (GSH-t, SOD, CAT, and GPx), and oxidatively damaged proteins induced by LPS treatment were attenuated by exercise training. The lack of information regarding the relevance of high-intensity exercise as a protective protocol highlights the importance of our work. Nevertheless, our study presents some limitations, such as data related to exact mechanism by which high-intensity exercise decreases lung inflammation. Future studies could include analysis of Nrf2 activation, as well as the involvement of other antioxidant systems. Furthermore, translational process from experimental studies to clinical practice is intrinsically complex. Nevertheless, high-intensity exercise stands as an alternative to be further evaluated, since the presented data are promising.
References
Matthay, M.A., L.B. Ware, and G.A. Zimmerman. 2012. The acute respiratory distress syndrome. The Journal of Clinical Investigation 122 (8): 2731–2740.
ARDS Definition Task Force. Ranieri, V.M., G.D. Rubenfeld, B.T. Thompson, N.D. Ferguson, E. Caldwell, E. Fan, L. Camporota and a.S. Slutsky. 2012. Acute respiratory distress syndrome: the Berlin Definition. The Journal of the American Medical Association 307 (23): 2526–2533.
Bein, T., S. Grasso, O. Moerer, M. Quintel, C. Guerin, M. Deja, A. Brondani, and S. Mehta. 2016. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Medicine 42 (5): 699–711.
Matute-Bello, G., C.W. Frevert and T.R. Martin. 2008. Animal models of acute lung injury. The American Journal of Physiology Lung Cellular and Moleular Physiology 295 (3): 379–399.
Chen, H., C. Bai, and X. Wang. 2010. The value of the lipopolysaccharide-induced acute lung injury model in respiratory medicine. Expert Review of Respiratory Medicine 4 (6): 773–783.
Ulich, T.R., L.R. Watson, S.M. Yin, K.Z. Guo, P. Wang, H. Thang, and J. del Castillo. 1991. The intratracheal administration of endotoxin and cytokines. I. Characterization of LPS-induced IL-1 and TNF mRNA expression and the LPS-, IL-1-, and TNF-induced inflammatory infiltrate. American Journal of Pathology 138 (6): 1485–1496.
Ward, P.A. 2010. Oxidative stress: acute and progressive lung injury. Annals of the New York Academy of Science 1203: 53–59.
Sarma, J.V., and P.A. Ward. 2011. Oxidants and redox signaling in acute lung injury. Comprehensive Physiology 1 (3): 1365–1381.
Wilcox, M.E., and M.S. Herridge. 2011. Lung function and quality of life in survivors of the acute respiratory distress syndrome (ARDS). La Presse Médicale 40 (12): 595–603.
Vieira, R.P., A.C. Toledo, L.B. Silva, F.M. Almeida, N.R. Damaceno-Rodrigues, E.G. Caldini, A.B.G. Santos, D.H. Rivero, D.C. Hizume, F.D.T.Q.S. Lopes, C.R. Olivo, H.C. Castro-Faria-Neto, M.A. Martins, P.H.N. Saldiva, and M. Dolhnikoff. 2012. Anti-inflammatory effects of aerobic exercise in mice exposed to air pollution. Medicine and Science in Sports and Exercise 44 (7): 1227–1234.
Souza, L.C., C.B. Filho, A.T.R. Goes, L.D. Fabbro, M.G. de Gomes, L. Savegnago, M.S. Oliveira, and C.R. Jesse. 2013. Neuroprotective effect of physical exercise in a mouse model of Alzheimer’s disease induced by β-amyloid1 40 peptide. Neurotoxicity Research 24 (2): 148–163.
Ávila, L.C.M., T.R. Bruggemann, F. Bobinski, M.D. da Silva, R.C. Oliveira, D.F. Martins, L. Mazzardo-Martins, M.M.M.F. Duarte, L.F. de Souza, A. Dafre, R. de P. Vieira, A.R.S. Santos, K.C. Bonorino, and D. de C. Hizume Kunzler. 2015. Effects of high-intensity swimming on lung inflammation and oxidative stress in a murine model of DEP-induced injury. Public Library of Science 10 (9).
Petersen, A.M.W., and B.K. Pedersen. 2005. The anti-inflammatory effect of exercise. Journal of Applied Physiology 98 (4): 1154–1162.
Balducci, S., S. Zanuso, A. Nicolucci, F. Fernando, S. Cavallo, P. Cardelli, S. Fallucca, E. Alessi, C. Letizia, A. Jimenez, F. Fallucca, and G. Pugliese. 2010. Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutrition, Metabolism and Cardiovascular Diseases 20 (8): 608–617.
Brüggemann, T.R., L.C.M. Ávila, B. Fortkamp, F.R. Greiffo, F. Bobinski, L. Mazzardo-Martins, D.F. Martins, M.M.M.F. Duarte, A. Dafre, A.R.S. Santos, M.D. Silva, L.F. Souza, R.P. Vieira, and D.C. Hizume-Kunzler. 2015. Effects of swimming on the inflammatory and redox response in a model of allergic asthma. International Journal of Sports Medicine 36 (2): 579–584.
Kuphal, K.E., E.E. Fibuch, and B.K. Taylor. 2007. Extended swimming exercise reduces inflammatory and peripheral neuropathic pain in rodents. The Journal of Pain 8 (12): 989–997.
Ferreira, J.C.B., N.P.L. Rolim, J.B. Bartholomeu, C.A. Gobatto, E. Kokubun, and P.C. Brum. 2007. Maximal lactate steady state in running mice: effect of exercise training. Clinical and Experimental Pharmacology Physiology 34 (8): 760–765.
Akerboom, T.P., and H. Sies. 1981. Assay of glutathione, glutathione disulfide, and glutathione mixed disulfides in biological samples. Methods in Enzymology 77: 373–382.
Wendel, A. 1981. Glutathione peroxidase. Methods in Enzymology 77: 325–333.
Aebi, H. 1984. Catalase in vitro. Methods in Enzymology 105: 121–126.
Paoletti, F., D. Aldinucci, A. Mocali, and A. Caparrini. 1986. A sensitive spectrophotometric method for the determination of superoxide dismutase activity in tissue extracts. Analytical Biochemistry 154 (4): 536–541.
Levine, R.L., J.A. Williams, E.R. Stadtman, and E. Shacter. 1994. Carbonyl assays for determination of oxidatively modified proteins. Methods in Enzymology 233: 346–357.
Sato, K., M.B. Kadiiska, A.J. Ghio, J. Corbett, Y.C. Fann, S.M. Holland, R.G. Thurman, and R.P. Mason. 2002. In vivo lipid-derived free radical formation by NADPH oxidase in acute lung injury induced by lipopolysaccharide: a model for ARDS. Federation of American Societies for Experimental Biology 16 (13): 1713–1720.
Hagiwara, S., H. Iwasaka, K. Togo and T. Noguchi, A. 2008. Neutrophil elastase inhibitor, sivelestat, reduces lung injury following endotoxin-induced shock in rats by inhibiting HMGB1. Inflammation 31 (4) 227–234.
Ramos, D.S., C.R. Olivo, F.D.T. Quirino Santos Lopes, A.C. Toledo, M.A. Martins, R.A. Lazo Osório, M. Dolhnikoff, W. Ribeiro, and R. de P. Vieira. 2010. Low-intensity swimming training partially inhibits lipopolysaccharide-induced acute lung injury. Medicine and Science in Sports and Exercise 42 (1): 113–119.
Reis Gonçalves, C.T., C.G. Reis Gonçalves, F.M. de Almeida, F.D.T.Q. dos Santos Lopes, A.C.C. dos Santos Durão, F.A. dos Santos, L.F.F. da Silva, T. Marcourakis, H.C. Castro-Faria-Neto, R. de P. Vieira, and M. Dolhnikoff. 2012. Protective effects of aerobic exercise on acute lung injury induced by LPS in mice. Critical Care 16 (5): R199.
Olivo, C.R., E.N. Miyaji, M.L.S. Oliveira, F.M. Almeida, J.D. Lourenço, R.M. Abreu, P.M.M. Arantes, F.D. Lopes, and M.A. Martins. 2014. Aerobic exercise attenuates pulmonary inflammation induced by Streptococcus pneumoniae. Journal of Applied Physiology 117 (9): 998–1007.
Luks, V., A. Burkett, L. Turner, and S. Pakhale. 2013. Effect of physical training on airway inflammation in animal models of asthma: a systematic review. BMC Pulmonary Medicine 13: 24.
Reutershan, J., M.A. Morris, T.L. Burcin, D.F. Smith, D. Chang, M.S. Saprito, and K. Ley. 2006. Critical role of endothelial CXCR2 in LPS-induced neutrophil migration into the lung. The Journal of Clinical Investigation 116 (3): 695–702.
Decker, T., M.L. Lohmann-Matthes, and G.E. Gifford. 1987. Cell-associated tumor necrosis factor (TNF) as a killing mechanism of activated cytotoxic macrophages. The Journal of Immunology 138 (3): 957–962.
Guo, H., J.B. Callaway, and J.P.-Y. Ting. 2015. Inflammasomes: mechanism of action, role in disease, and therapeutics. Nature Medicine 21 (7): 677–687.
Xu, S., M. Xu, G.-G. Li, C. Wang, H. Song, and J. Bai. 2016. Early recruitment of IL-10-producing B cells into alveoli improved the resolution of acute lung injury. Cellular Physiology and Biochemistry 38 (5): 1752–1760.
Park, H.S., S.R. Kim, and Y.C. Lee. 2009. Impact of oxidative stress on lung diseases. Respirology 14 (1): 27–38.
Rosanna, D.P., and C. Salvatore. 2012. Reactive oxygen species, inflammation, and lung diseases. Current Pharmaceutical Design 18 (26): 3889–3900.
Sittipunt, C., K.P. Steinberg, J.T. Ruzinski, C. Myles, S. Zhu, R.B. Goodman, L.D. Hudson, S. Matalon, and T.R. Martin. 2001. Nitric oxide and nitrotyrosine in the lungs of patients with acute respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine 163 (2): 503–510.
da Cunha, A.A., F.B. Nunes, A. Lunardelli, V. Pauli, R.H. Amaral, L.M. de Oliveira, V.C. Saciura, G.L. da Silva, M.G.S. Pires, M.V.F. Donadio, D.A. da S. Melo, F. Dal-Pizzol, J.C.F. Moreira, G.A. Behr, C.L. Reichel, J.L. Rosa, and J.R. de Oliveira. 2011. Treatment with N-methyl-d-aspartate receptor antagonist (MK-801) protects against oxidative stress in lipopolysaccharide-induced acute lung injury in the rat. International Immunopharmacology 11 (6): 706–711.
Mitchell, J., H. Jiang, L. Berry, and B. Meyrick. 1996. Effect of antioxidants on lipopolysaccharide-stimulated induction of mangano superoxide dismutase mRNA in bovine pulmonary artery endothelial cells. Journal of Cellular Physiology 169 (2): 333–340.
Dirami, G., D. Massaro, and L.B. Clerch. 1999. Regulation of lung manganese superoxide dismutase: species variation in response to lipopolysaccharide. American Journal of Physiology 276 (5 Pt 1): L705–L708.
Lima Trajano, E.T., C. Sternberg, M. Caetano, M.A. Santos Silva, L.C. Porto, J.C. Santos, M.L. Ribeiro, C.B. Magalhães, W.A. Zin, C.F. Benjamim, and S.S. Valença. 2011. Endotoxin-induced acute lung injury is dependent upon oxidative response. Inhalation Toxicology 23 (14): 918–926.
Biolo, G., R. Antonione, and M. De Cicco. 2007. Glutathione metabolism in sepsis. Critical Care Medicine 35 (9): S591–S595.
Malmezat, T., D. Breuillé, P. Capitan, P.P. Mirand, and C. Obled. 2000. Glutathione turnover is increased during the acute phase of sepsis in rats. Journal of Nutrition 130 (5): 1239–1246.
Nakasone, M., K. Nakaso, Y. Horikoshi, T. Hanaki, Y. Kitagawa, T. Takahashi, Y. Inagaki, and T. Matsura. 2016. Preconditioning by low dose LPS prevents subsequent LPS-induced severe liver injury via Nrf2 activation in mice. Yonago Acta Medica 59 (3): 223–231.
Yu, J., J. Shi, L. Gong, S. Dong, Y. Xu, Y. Zhang, X. Cao, and L. Wu. 2014. Role of Nrf2/ARE pathway in protective effect of electroacupuncture against endotoxic shock-induced acute lung injury in rabbits. Public Library of Science 9 (8): e104924.
Yeh, C.H., J.J. Yang, M.L. Yang, Y.C. Li, and Y.H. Kuan. 2014. Rutin decreases lipopolysaccharide-induced acute lung injury via inhibition of oxidative stress and the MAPK–NF-κB pathway. Free Radical Biology and Medicine 69: 249–257.
Su, Z.Q., Z.Z. Mo, J.B. Liao, X.X. Feng, Y.Z. Liang, X. Zhang, Y.H. Liu, X.Y. Chen, Z.W. Chen, Z.R. Su, and X.P. Lai. 2014. Usnic acid protects LPS-induced acute lung injury in mice through attenuating inflammatory responses and oxidative stress. International Immunopharmacology 22 (2): 371–378.
Du, Q., C. Wang, N. Zhang, G. Li, M. Zhang, L. Li, Q. Zhang, and J. Zhang. 2014. In vivo study of the effects of exogenous hydrogen sulfide on lung mitochondria in acute lung injury in rats. BMC Anesthesiology 14: 117.
Dos Santos Cunha, W.D., M.V. Giampietro, D.F. De Souza, M. Vaisberg, M.C.L. Seelaender, and L.F. Rosa. 2004. Exercise restores immune cell function in energy-restricted rats. Medicine and Science in Sports and Exercise 36 (12): 2059–2064.
Heffner, J.E., and J.E. Repine. Pulmonary strategies of antioxidant defense. The American Review of Respiratory Disease 140 (2): 531–554.
Funding
This work was supported by the State University of Santa Catarina and Research Support Foundation of Santa Catarina.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Review Board for Animal Studies of the Federal University of Santa Catarina (PP 00745). All animals in this study received humane care in compliance with EU Directive 2010/63/EU, which provides guidelines for animal experiments.
Rights and permissions
About this article
Cite this article
Cardoso, G.H., Petry, D.M., Probst, J.J. et al. High-Intensity Exercise Prevents Disturbances in Lung Inflammatory Cytokines and Antioxidant Defenses Induced by Lipopolysaccharide. Inflammation 41, 2060–2067 (2018). https://doi.org/10.1007/s10753-018-0849-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-018-0849-9