Abstract
Upregulation of WISP1 has been demonstrated in lung remodeling. Moreover, it has been recently found that some signaling components of WNT pathway can activate GSK3β signaling to mediate remodeling of airway smooth muscle (ASM) in asthma. Therefore, we hypothesized that WISP1, a signaling molecule downstream of the WNT signaling pathway, is involved in PI3K/GSK3β signaling to mediate ASM remodeling in asthma. Our results showed that WISP1 depletion partly suppressed OVA-induced ASM hypertrophy in vivo. In vitro, WISP1 could induce hBSMC hypertrophy and proliferation, accompanied by upregulation of levels of PI3K, p-Akt, p-GSK3β, and its own expression. TGF-β treatment could increase expression of PI3K, p-Akt, p-GSK3β, and WISP1. SH-5 treatment could partly suppress TGF-β-induced hypertrophy and proliferation of hBSMC, and depress expression of p-GSK3β and WISP1. In conclusion, WISP1 may be a potential inducer of ASM proliferation and hypertrophy in asthma. The pro-remodeling effect of WISP1 is likely due to be involved in PI3K-GSK3β-dependent noncanonical TGF-β signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Airway remodeling, a well-established feature of asthma, arises from repeated cycles of tissue damage and repair [1, 2]. It has been confirmed that smooth muscle proliferation and hypertrophy contribute to airway remodeling in asthma. The airways of patients with severe asthma have larger smooth muscle cell diameter and an increased expression of α-smooth muscle actin [3–5]. Airway smooth muscle (ASM) cells may also produce a plethora of biologically active agents like pro-inflammatory mediators, chemokines, and cytokines, which are responsible for the progression of airway remodeling pathogenesis in asthma [6, 7]. Therefore, the accumulated evidence indicates that ASM cells are one of main effector cells of pathological remodeling in airways and that the diminution of overabundant airway smooth musculature may alleviate some symptoms exhibited in asthmatics by improving air flow [8]. However, few studies have addressed the cellular mechanism of ASM remodeling in asthma. Current therapies, including corticosteroids and β2-agonists, can very well control lung inflammation and modulate the contractile function of ASM, while the pathological remodeling such as ASM hypertrophy and hyperplasia still fails to be controlled [9–11]. Thus, it is necessary to shed more light on the molecular mechanisms of increased ASM mass in airway remodeling and investigate the mediators that have the potential to be used for clinical treatments.
It has been demonstrated that some of the pro-survival and pro-fibrogenic cytokines are closely related to ASM remodeling. The cytokines mainly include interleukin (IL)-8, transforming growth factor (TGF)-β, and IL-1β. Especially, TGF-β is one of the major players in determining the structural and functional abnormalities of ASM in asthma [12]. TGF-β challenge can increase ASM cell size and expression of contractile proteins in asthmatic airway remodeling. However, it has recently been found that some components of TGF-β and WNT signaling are mutual targets of each other. For example, both glycogen synthase kinase-3β (GSK3β) and β-catenin are key components of the canonical WNT signaling [13], but GSK3β/β-catenin signaling is also involved in noncanonical TGF-β signaling [14]. Activated WNT signaling can directly induce expression of TGF-β [15] whereas TGF-β can also modulate WNT signaling in ASM cells [16, 17]. Thus, it can be speculated that some signaling components of WNT pathway may activate PI3K-GSK3β-dependent noncanonical TGF-β signaling to mediate remodeling of ASM in asthma.
The WNT1-inducible signaling pathway protein 1 (WISP1) is a cysteine-rich protein that belongs to the (Cyr61, CTGF, Nov) CCN family. It has been confirmed that WISP1 is a target of the WNT pathway and exerts diverse biological effects including cell growth, proliferation, and tissue remodeling [18–20]. WISP1 could mediate collagen deposition via activated Akt-dependent GSK3β signaling in lung in an asthmatic rat model with airway remodeling [21]. WISP1 was also shown to induce proliferation of human coronary artery SMC (ASMC) via activated Akt-dependent GSK3β/β-catenin signaling [22]. GSK3β, as a component of TGF-β signaling [23], plays a central role in regulating structure and function of ASM cells. Phosphorylation of GSK3β that is induced by TGF-β could increase ASM cell size and contractile protein expression [24, 25]. Inactivation of GSK3β can also induce ECM protein production via activated β-catenin signaling in ASM cells [26]. Therefore, it is highly likely that WISP1 is involved in GSK3β-dependent noncanonical TGF-β signaling to mediate ASM remodeling in asthma.
We hypothesized that WISP1 abnormal expression contributes to increased ASM hyperplasia and hypertrophy in OVA-challenged rats. Our results demonstrate for the first time that WISP1 depletion attenuates OVA-induced ASM remodeling in a rat model of asthma. WISP1 challenge induces hBSMC proliferation and hypertrophy via activated phosphatidylinositol 3-kinase (PI3K)/GSK3β signaling in vitro. In addition, the levels of WISP1 is not only upregulated by TGF-β challenge but is also induced by itself in hBSMC. As a whole, our results suggest that WISP1 may be a potential inducer of ASM proliferation and hypertrophy in asthma.
MATERIALS AND METHODS
Animals and Housing Conditions
Four-week-old male Sprague-Dawley rats were purchased from the Experimental Animal Center, Chongqing Medical University. Animals were housed five per plastic cages and maintained in a filter-protected air-conditioned room with controlled temperature (23 ± 2 °C), and 12-h light/dark cycles (light on 0800–2000 hours). All animal care and experimental protocols were approved by the Ethics Committee of Second Affiliated Hospital of Chongqing Medical University. All animals were handled in accordance with the guidelines of the Principle of Laboratory Animal Care [27].
Experimental Design and Animal Models
Animals were randomly divided into four groups as follows: the blank/control group (n = 6), the OVA group (n = 6), the OVA + anti-WISP1 group (n = 6), and the IgG control group (n = 6). All rats were sensitized with intraperitoneal injection of ovalbumin (1 mg, OVA) (Solarbio, Beijing, China) and aluminum hydroxide (100 mg) (Aldrich, Milwaukee, WI) in 0.9 % NaCl solution (saline 1 mL) on days 0 and 14, which was made according to previously reported method [28]. In the OVA group, rats were next challenged with OVA (50 μL) by intratracheal administration under inhalation anesthesia with isoflurane (4 days per week for 3 weeks) (Abbott Japan, Tokyo), as reported previously [29]. In the OVA + anti-WISP1 or IgG group, OVA challenge was also applied to the animals but the rats would be pretreated with anti-WISP1 antibodies (1.6 μg/mL, R&D Systems) or preimmune serum by intratracheal administration before each OVA challenge, which was done according to a previously reported method [30]. The rats in the negative blank/control group were sensitized with OVA + Al(OH)3, i.p. without any airway challenges with OVA. All rats were killed 24 h after the final challenge.
Histopathological Study
Animal were exsanguinated by puncture, and lung tissue were obtained and fixed with 4 % formalin. Tissues were embedded in paraffin, and 4-μm sections were stained with hematoxylin and eosin (HE) for light microscopic observation. Bronchial smooth muscle mass was quantificationally assessed by measuring the thickness of smooth muscle cell layer below the airway epithelial cell basement membrane in HE-stained lung sections, as reported previously [31]. The morphological analysis was implemented via a minimum of ten fields throughout the upper and lower lung. All morphometric measurements were performed in a blinded fashion.
Immunohistochemistry
Lung tissue sections were stained immunohistochemically to assess the levels of α-smooth muscle actin (α-SMA) and WISP1. Tissues were fixed with formalin, embedded with paraffin, and cut into 5-μm serial sections. Then, these sections were deparaffinized with xylene and incubated overnight at 4 °C with a rabbit polyclonal antibody against WISP1 (Santa Cruz Biotechnologies, Santa Cruz, CA) or a monoclonal antibody against a-smooth muscle actin (Santa Cruz Biotechnologies, Santa Cruz, CA), the normal rat serum was used as a negative control. Then, sections were incubated with a biotinylated anti-rabbit secondary antibody (Santa Cruz Biotechnologies, Santa Cruz, CA) at a final dilution of 1:500. The sections were next incubated with an avidin-biotin-peroxidase complex using the Vectastain Elite ABC kit (Vector Laboratories, Burlingame, CA). The peroxidase substrate solution (DAB stain kit, Vector Labs, Burlingame, CA) was applied to the sections, followed by incubation in a dark. Finally, a light hematoxylin counterstain was applied to all sections and examined using a light microscopy.
Semiquantitative assessment of immunohistochemistry of WISP1 and α-SMA expression was performed according to a published method [32, 33]. The WISP1 levels were assessed by calculating the number of positive cells using high-power (×200) microscopy, and the final number (the percentage of positive cell score × the intensity score) was used for further statistical analysis. The degree of thickening of the smooth muscle layer was quantificationally assessed by dividing the α-SMA+ area by the length of the basement membrane. Three investigators independently evaluated the staining in a blinded manner.
Bronchial Smooth Muscle Cell Culture and Treatment
In order to further explore the effects of WISP1 on ASM cells in vitro, human bronchial smooth muscle cells (hBSMC, CHI Scientific, JiangShu, China) were purchased and maintained in basal medium supplemented with the SmGM-2 bullet kit (5 % fetal bovine serum, 0.1 % insulin, 0.1 % human epidermal growth factor, 0.2 % human fibroblast growth factor-B, and gentamicin sulfate/amphotericin B; LonzaBio), as reported previously [34]. Cells were used between passages 4 and 12 for all experiments, and divided into five groups: the control group (saline), the WISP1-treated group (WISP1), the WISP1 + SH-5-treated group (WISP1 + SH-5), the TGF-β-treated group (TGF-β), and the TGF-β + SH-5-treated group (TGF-β + SH-5). Cells in each group were plated into 96-well plates at 3000 cells per well and allowed to attach overnight. Then, cells were fed with serum-free medium containing 0.5 % bovine serum albumin (BSA), 100 μg/mL streptomycin, 100 U/mL penicillin, 2 μg/mL amphotericin B (Invitrogen, Milan), and 0.12 IU/mL insulin (Lilly, St Cloud, France) and incubated for an additional 24 h. Then, cells in the WISP1 or TGF-β group were continuously stimulated with recombinant WISP1 (0.1, 0.3, 0.6, 1.2, and 1.6 μg/mL; 24 and 48 h) (PeproTech, Rocky Hill, NJ) or TGF-β (1, 3, 5, 10, and 15 ng/mL; 24 and 48 h) (PeproTech, Rocky Hill, NJ) in serum-free medium, and phosphate-buffered saline (PBS) (Solarbio, Beijing, China) was used for the control group. For the WISP1 + SH-5 or TGF-β + SH-5 group, cells were pretreated with SH-5 (an Akt inhibitor II) (1 μM dissolved in DMSO; 1 h) before WISP1 or TGF-β stimulation. SH-5 was purchased from EMD Biosciences (San Diego, CA) and has been used both in vivo [35] and in vitro [19, 36] to selectively inhibit Akt. SH-5, as a phosphatidylino-sitol analog, can block binding of phosphatidylinositol-3,4,5-trisphos-phate to the PH domain of Akt [37]. All groups were maintained in a humidified atmosphere of 5 % CO2 at 37 °C as described previously [30]. Cell proliferation was assessed by MTT assay. The levels of WISP1 messenger RNA (mRNA) were detected by real-time RNA analysis. The levels of PI3K, p-Akt, p-GSK3β, and WISP1 protein were quantificationally detected by Western blot.
Cell Proliferation Assay
The proliferative rate of cell was examined by a colorimetric assay which utilized the capacity of live cells to change 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT, Sigma) from yellow to a purple precipitate which could be dissolved in DMSO. MTT solution was added to each well for 4 h. The medium was removed, 200 pL of DMSO was added and vibrated for 10 min. Optical densities (OD) were examined at 570 nm using a microplate reader (Multiskan MK3, Thermo Fisher Scientific, Soochow, China). Finally, viable cell ratio was calculated as follows: (absorbance of experimental group / absorbance of control group) × 100 %.
Cell Hypertrophy Assay
Cell hypertrophy was assessed by measuring the rate of protein synthesis as previously described [19, 22, 38]. Cells were plated in 24-well plates and treated with TGF-β or WISP1 for 24 and 48 h, then incubated with 0.5 μCi [3H]-leucine for an additional 6 h. In order to determine the roles of Akt signaling in TGF-β or WISP1-mediated protein synthesis, part of cells were pretreated with SH-5 before rhTGF-β or rhWISP1 challenge. The radioactivity incorporated into the trichloroacetic acid-precipitable material was detected by using a liquid scintillation counter.
Cell Migration Assay
Cell migration was analyzed as described previously using a Boyden chamber assay [39, 40]. Briefly, the serum-starved cells were separated from the culture plate using trypsin (0.5 mg/mL)-EDTA (0.2 mg/mL) solution (Invitrogen Canada Inc., Burlington, ON) and then added to Ham’s F12 medium. A polycarbonate membrane with 8-mm pore size (Neuroprobe, Gaithersburg, MD, USA) was coated with 0.01 % collagen type-I in 0.01 N HCl solution (Sigma). A 100-μL solution containing hBSMC (3 × 104 cells/mL) was added to the upper chamber of modified Boyden chamber apparatus (Neuroprobe). In the lower chamber, rhWISP1 or rhTGF-β were added as a chemoattractant. In order to determine the roles of Akt signaling in TGF-β or WISP1-mediated cell migration, cells were pretreated with SH-5 before rhTGF-β or rhWISP1 challenge. The membranes were peeled off after 4 h of incubation at 37 °C. Cells that migrated to the lower side of the membranes were fixed and stained with HemacolorH stain set (EMD Millipore, Billerica, MA, USA). The number of migrated cells was counted in six random fields using a phase contrast microscope (Carl Zeiss Canada Ltd., Toronto, ON).
Real-Time RNA Analysis
To evaluate WISP1 level in lung tissues and bronchial smooth muscle cells. Total RNA was extracted using the RNeasy Mini kit (Qiagen, Hilden, Germany) in accordance with the manufacturer’s instruction. The following primer sequences were used: forward (WISP1) 5′-AGGTATGGCAGAGGTGCAAG-3′ and reverse 5′-GTGTGTGTAGGCAGGGAGTG-3′. The relative quantity (RQ) was calculated by subtracting the DDCt values of the control group from the DDCt values of the experimental groups. The β-actin which was continuously expressed at a constant level in cells was used as a reference gene.
Western Blotting Analysis
The expression of PI3K, p-Akt, p-GSK3β, and WISP1 were examined by Western blotting analysis. Cells were lysed at 4 °C in RIPA buffer with protease and phosphatase inhibitors (Roche, Basel, Switzerland). Protein concentrations were determined by a BCA assay kit (Pierce). Total protein was fractionated on SDS-PAGE and transferred to the polyvinylidene fluoride (PVDF) membranes (Millipore, Billerica, MA, USA), blocked with skimmed milk and incubated overnight at 4 °C with the primary antibodies against PI3K and WISP1 (Santa Cruz Biotechnologies, Santa Cruz, CA), p-GSK3β, p-Akt (Cell Signaling Technology, Danvers, MA). Membranes were incubated for 1 h at 37 °C with secondary antibody. Quantitative results were acquired using the computerized imaging program Bio-1D (VilberLourmat Biotech. Bioprof., France). β-Actin was used as the protein loading control.
Statistical Analyses
Values are expressed as means ± SEM. The comparisons of data among groups were performed by Tukey’s post hoc test (parametric data) or by Dunn’s post hoc test (nonparametric data). Data were considered statistically significant at P < 0.05. The Sigma Stat 3.5 Software (San Jose, CA) was used for statistical analyses.
RESULTS
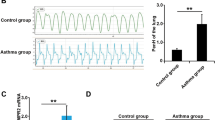
OVA Sensitization and Challenge Increases Airway Smooth Muscle Deposition
Animal models are constructed according to previously reported method [28]. We assessed the degree of smooth muscle hypertrophy (H&E staining), which is important structural change involved in airway remodeling in asthma. As shown in Fig. 1a, b, e, smooth muscle around the bronchi was significantly thickened in the OVA group (18.82 ± 1.88 μm for OVA group vs 5.71 ± 0.16 μm for PBS, p < 0.05; n = 6 sections) when compared to control. In addition, smooth muscle accumulation around the airways was verified by increased α-smooth muscle actin immunohistochemistry; these data are in agreement with the results observed from the above H&E staining analysis (34.3 ± 3.7 % for OVA group vs 9.5 ± 1.1 % for PBS, p < 0.05; n = 6 sections) (Fig. 2a, b, e). Thus, the results showed that animal models with ASM remodeling had been successfully developed in our studies.
Histological analysis of airway smooth muscle. Isolated lung tissues were fixed with 4 % formalin and dehydrated in a graded series of ethanol solutions followed by staining with hematoxylin and eosin. Peribronchiolar smooth muscle was indicated by the arrows. All images of peribronchiolar smooth muscle layer were made by merging images from different fields (scale bar = 100 μm) (a–d). The results of quantitative analysis are shown in e. Data are shown as means ± SEM (n = 3); *p < 0.05 versus PBS group, #p < 0.05 versus OVA + anti-WISP1 group, and p < 0.05 versus OVA group (e).
Assessment of degree of smooth muscle thickening by immunohistochemistry. Degree of smooth muscle thickening was calculated by dividing α-SMA+ area by the length (μm) of the BM (P) by immunohistochemistry (a–d). Arrows indicate the α-SMA+ area. Data are representative of three independent experiments (p < 0.05). Means ± SD with n = 3. Data are shown as means ± SEM (n = 3); *p < 0.05 versus PBS group, #p < 0.05 versus OVA + anti-WISP1 group, and p < 0.05 versus OVA group (e).
WISP1 Inhibition Partially Suppresses OVA-Induced Airway Smooth Muscle Accumulation in OVA-Challenged Model
In lungs from OVA + anti-WISP1-treated animals, smooth muscle accumulation around the airways was also increased when compared to control, as detected by H&E (13.30 ± 0.85 μm for OVA + anti-WISP1 group vs 5.71 ± 0.16 μm for control, p < 0.05; n = 6 sections), but it was more mild than that in the OVA group (13.30 ± 0.85 μm for OVA + anti-WISP1 group vs 18.82 ± 1.88 μm for OVA group, p < 0.05; n = 6 sections) (Fig. 1b, c, e). To further verify the degree of ASM remodeling after neutralizing α-WISP1 antibodies exposure, semiquantitative a-SMA protein analysis by immunohistochemistry was performed (22.7 ± 2.3 % for OVA + anti-WISP1 group vs 9.5 ± 1.1 % for control; 22.7 ± 2.3 % for OVA + anti-WISP1 group vs 36.1 ± 3.2 % for OVA group; p < 0.05) (Fig. 2b, c, e); the data are in agreement with the results observed from the above H&E analysis. Therefore, the results showed that attenuation of WISP1 expression could partly suppress OVA-induced smooth muscle accumulation in asthmatic animal model, indicating that WISP1 may be involved in the pathogenesis of ASM remodeling in asthma.
OVA Challenge Induces WISP1 Transcription and Expression in Lung Tissue of Animal Models
Total RNA was extracted from the pulmonary segments of all rats to detect the levels of WISP1 mRNA. In the PBS control group, mRNA levels of WISP1 relative to the amount of β-actin mRNA were 0.140 ± 0.036 (Fig. 3f). In the OVA or OVA + anti-WISP1 group, the levels of WISP1 mRNAs in the pulmonary segments were upregulated to 0.782 ± 0.113 and 0.647 ± 0.081 when compared to PBS control (Fig. 3f). These data showed that OVA exposure increased the mRNA levels of WISP1 in a rat model. In order to further analyze the changes in WISP1 protein expression after OVA exposure, semiquantitative protein analysis was performed by immunohistochemistry. This result showed that the percentages of positive cells in the OVA group were significantly higher than that in the nonsensitized rats (43.4 ± 4.1 % for OVA group vs. 7.7 ± 1.1 % for PBS control; p < 0.05) (Fig. 3a–e), and these data are also in agreement with the result observed from the above mRNA studies.
The levels of WISP1 mRNA and protein expression. The lung segments were from rats that were exposed to PBS and OVA. WISP1 protein expression was assessed by immunohistochemistry (a–e). Arrows indicate extracellular WISP1 staining. WISP1 mRNA level is presented relative to that of the β-actin (f). Data are representative of three independent experiments. The values are expressed as the means ± SEM (n = 3); *p < 0.05 versus control group (e), *p < 0.05 versus control group (f).
Both WISP1 and TGF-β Induce hBSMC Proliferation via Akt Signaling
Abnormal activation of bronchial smooth muscle cells are important features of airway remodeling. In order to further explore the specific molecular effects of these cytokines on ASM remodeling, we assessed the effects of WISP1, TGF-β, WISP1 + SH-5 (an Akt inhibitor), and TGF-β + SH-5 exposure on bronchial smooth muscle cells (hBSMC) proliferation in vitro. Incubation of quiescent hBSMC for 48 h with WISP1 (1.2 ng/mL) or TGF-β (10 ng/mL) could induce significant proliferation (102.7 ± 12.91 and 122.7 ± 6.12 for WISP1 group and TGF-β group vs 29.33 ± 4.10 for control, p < 0.05) (Fig. 4), but the proliferation in the WISP1 + SH-5 or TGF-β + SH-5 group were partly suppressed compared with the WISP1 or TGF-β group (68.33 ± 7.42 and 93.33 ± 4.67 for WISP1 + SH-5 group and TGF-β + SH-5 group vs 102.7 ± 12.91 and 122.7 ± 6.12 for WISP1 group and TGF-β group, p < 0.05) (Fig. 4). These results showed that WISP1 or TGF-β exposure could effectively promote hBSMC proliferation, while the process can be partly inhibited by pretreatment of cells with an Akt inhibitor. We next assessed the effects of these cytokines on migration and hypertrophy of hBSMC in the following.
Assessment of proliferation rate of human bronchial smooth muscle cells. Human bronchial smooth muscle cells were seeded and cultured for 48 h. Viable cells were detected by MTT. The cell number was counted each day. Values are expressed as the means ± SEM (n = 3); *p < 0.05 versus control group, #p < 0.05 versus WISP1 group, and p < 0.05 versus TGF-β group (a, b).
WISP1 Induces hBSMC Hypertrophy, but not Migration
Increased ASM mass is a characteristic finding in fatal and nonfatal asthma. Cell hypertrophy is one of main causes for increased ASM mass in asthma. Therefore, we examined the possibility that hypertrophy of hBSMC may be induced by WISP1 challenge. Indeed, hBSMC hypertrophy is successfully induced by WISP1 stimulation, but the process could also be partly inhibited by pretreatment of cells with an Akt inhibitor (Fig. 5a). In addition, cell hypertrophy that was induced by TGF-β exposure could be also inhibited effectively by pretreatment of cells with an Akt inhibitor (Fig. 5a).
Assessment of hypertrophy and migration of human bronchial smooth muscle cells. Cell hypertrophy was assessed by measuring the rate of protein synthesis. Data are shown as means ± SEM; *p < 0.05 versus control group and p < 0.05 versus WISP1 group (a). Cell migration was analyzed using a Boyden chamber assay. The number of migrated cells was counted in six random fields using a phase contrast microscope. Data are shown as means ± SEM; #p < 0.05 versus control group (b), *p < 0.05 versus control group (d).
We also investigated the roles of these cytokines in hBSMC migration. Our results showed that migration of hBSMC was significantly increased by TGF-β stimulation (TGF-β, 10 ng/mL, 2.438 ± 0.40-fold, p < 0.05) (Fig. 5b, d), while WISP1 challenge (WISP1, 0.1, 0.3, 0.6, 1.2, and 1.6 μg/mL) had no significant effect on hBSMC migration (p > 0.05) (Fig. 5c). Moreover, TGF-β-induced hBSMC migration was also partially suppressed by a pretreatment with an Akt inhibitor (TGF-β + SH-5, 1.726 ± 0.40-fold vs TGF-β, 2.438 ± 0.40-fold, p < 0.05) (Fig. 5d). We next investigate the specific signaling that may be involved in WISP1 and TGF-β signaling in hBSMC in vitro.
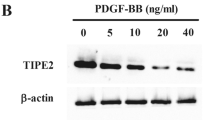
WISP1 Is Not Only Induced by TGF-β Challenge but Also Significantly Upregulated by Its Own Stimulation in hBSMC
Real-time PCR analysis of total RNA extracted from cell debris demonstrated the presence of mRNA coding for the WISP1. In the control group, the mRNA levels of WISP1 relative to the amount of β-actin mRNA were 0.138 ± 0.021 (24 h) and 0.141 ± 0.015 (48 h). In the WISP1- or TGF-β-challenged groups, the levels of WISP1 mRNA were upregulated to 0.563 ± 0.058 and 0.760 ± 0.085 (WISP1 group) or 1.067 ± 0.090 and 1.369 ± 0.051 (TGF-β group) after exposure to WISP1 or TGF-β for 24 and 48 h, respectively (Fig. 6b). However, the mRNA levels of WISP1 were suppressed by pretreatment with an Akt inhibitor before WISP1 or TGF-β exposure when compared to WISP1 or TGF-β group (WISP1 + SH-5 group, 0.350 ± 0.055 and 0.582 ± 0.059 for an exposure of 24 or 48 h; TGF-β + SH-5 group, 0.681 ± 0.060 and 0.947 ± 0.074 for an exposure of 24 or 48 h) (Fig. 6b). Therefore, our results showed that the levels of WISP1 mRNA could be upregulated by WISP1 or TGF-β challenge, while this process was markedly attenuated by pretreatment with an Akt inhibitor. Further, it was also revealed that WISP1 could be induced by itself in hBSMC. The protein levels of WISP1 were quantificationally assessed by Western blotting, and the results also suggested that TGF-β challenge could induce expression of WISP1 in hBSMC (Fig. 6a).
The levels of WISP1 mRNA and protein in human bronchial smooth muscle cells. The WISP1 mRNA level is presented relative to that of the β-actin (b). The levels of WISP1 protein was assessed by Western blotting. TGF-β induced expression of WISP1 after an exposure of 24 or 48 h; SH-5 (an Akt inhibitor) could suppress TGF-β-induced expression of WISP1 (a). Data are shown as means ± SEM; *p < 0.05 versus control group and p < 0.05 versus WISP1 group (an exposure of 48 h), #p < 0.05 versus TGF-β group (an exposure of 48 h) (b).
WISP1 Induces p-GSK3β Expression via PI3K/Akt Signaling in hBSMC
Recently, studies have found that WISP1 could induce cardiomyocyte hypertrophy via activated PI3K/Akt/GSK3β signaling [41]. Moreover, it was confirmed that Akt/GSK3β signaling is also involved in molecular mechanism of ASM remodeling [42–44]. Thus, we next explored the possibility that WISP1 was capable of stimulating Akt and/or GSK3β-dependent bronchial smooth muscle cell activation in vitro. In the control group, the protein levels of PI3K, p-Akt, and p-GSK3β relative to the amount of β-actin were 0.375 ± 0.03, 0.495 ± 0.04, and 0.396 ± 0.05. However, the protein levels of PI3K, p-Akt, and p-GSK3β in the WISP1 group were upregulated to 0.965 ± 0.08, 1.869 ± 0.08, and 1.198 ± 0.17 for an exposure of 48 h (p < 0.05) (Figs. 7c, d, 8a, b, and 9a, b), respectively. Moreover, the levels of p-Akt and p-GSK3β in the WISP1 + SH-5 group were significantly suppressed and downregulated to 0.788 ± 0.08 and 0.711 ± 0.06 for an exposure of 48 h (p < 0.05) (Figs. 8a, b and 9a, b), respectively. However, the PI3K levels were not significantly suppressed by pretreatment with an Akt inhibitor before WISP1 exposure (0.890 ± 0.09) (p > 0.05; Fig. 7c, d). As a whole, these data demonstrated that WISP1 treatment induced inactivation of GSK3β via activated PI3K/Akt signaling in hBSMC, suggesting that WISP1 could induce ASM remodeling by mediating inactivation and phosphorylation of GSK3β under activation of PI3K/Akt signaling (Fig. 10).
Assessment of PI3K, p-Akt, and p-GSK3β levels in human bronchial smooth muscle cells. The levels of p-Akt and p-GSK3β expression that were induced by TGF-β challenge were time-dependent in hBSMC (a, b). Both TGF-β and WISP1 could induce upregulation of PI3K levels. SH-5 could not suppress WISP1- and TGF-β-induced PI3K expression (c, d). Data are shown as means ± SEM; *p < 0.05 versus control group (d).
Assessment of p-Akt levels in human bronchial smooth muscle cells. Both TGF-β and WISP1 could induce p-Akt expression. SH-5 could suppress WISP1- and TGF-β-induced p-Akt expression (a, b). Data are shown as means ± SEM; *p < 0.05 versus control group and p < 0.05 versus WISP1 group, #p < 0.05 versus TGF-β group (b).
Assessment of p-GSK3β levels in human bronchial smooth muscle cells. Both TGF-β and WISP1 could induce p-GSK3β expression. SH-5 could suppress WISP1- and TGF-β-induced p-GSK3β expression (a, b). Data are shown as means ± SEM; *p < 0.05 versus control group and p < 0.05 versus WISP1 group, #p < 0.05 versus TGF-β group (b).
TGF-β Induces WISP1 Expression via PI3K/GSK3β Signaling in hBSMC
TGF-β is one of the major players in determining the structural and functional abnormalities of ASM in asthma. It is demonstrated that TGF-β can activate β-catenin through PI3K/Akt/GSK3β signaling [14, 45, 46]. In addition, it is also shown that WISP1 could be induced by activating Akt/GSK3β signaling in human saphenous vein smooth muscle cell [22]. Thus, we next explored the possibility that TGF-β was capable of inducing expression of WISP1 via activated Akt/GSK3β signaling in hBSMC. The levels of p-Akt and p-GSK3β expression that were induced by TGF-β challenge were time-dependent in hBSMC (Fig. 7a, b). In the control group, the levels of PI3K, p-Akt, p-GSK3β, and WISP1 relative to the amount of β-actin were 0.375 ± 0.03, 0.495 ± 0.04, 0.634 ± 0.03, and 0.396 ± 0.05. In the TGF-β group, the levels of PI3K, p-Akt, p-GSK3β, and WISP1 were regulated to 1.426 ± 0.05, 1.535 ± 0.06, 1.213 ± 0.08 and 1.549 ± 0.17 for an exposure of 48 h (p < 0.05) (Figs. 7c, d, 8a, b, and 9a, b), respectively. However, the levels of p-Akt, p-GSK3β, and WISP1 in the TGF-β + SH-5 group were significantly suppressed and downregulated to 0.952 ± 0.12, 1.023 ± 0.12, and 0.807 ± 0.04 for an exposure of 48 h (p < 0.05) (Figs. 7c, d, 8a, b, and 9a, b), respectively. The PI3K levels were not significantly suppressed by pretreatment with an Akt inhibitor before TGF-β exposure (1.284 ± 0.06) (p > 0.05; Fig. 7c, d). These data suggested that TGF-β treatment resulted in upregulation of WISP1 expression via activated PI3K/Akt/GSK3β signaling in hBSMC (Fig. 10).
DISCUSSION
Our results further demonstrate that WISP1 is upregulated in a rat animal model and describe for the first time that WISP1 may be a potent and rapid inducer of ASM remodeling in asthma. In addition, both TGF-β and WISP1 challenge could induce hBSMC hypertrophy and proliferation in vitro. TGF-β could also induce WISP1 expression via activated PI3K-dependent Akt/GSK3β signaling. Further, WISP1 could induce its own expression via PI3K/GSK3β signaling in hBSMC. As a whole, our results suggest that WISP1 may be involved in PI3K-GSK3β-dependent noncanonical TGF-β signaling to mediate hypertrophy and proliferation of ASM in asthma (Fig. 10).
WISP1 is a member of the secreted Cyr61-CTGF-Nov (CCN; cysteine-rich protein 61, connective tissue growth factor) family. Venkatachalam and colleagues have reported that WISP1 could antagonize TNF-α-induced cardiomyocyte death and mediate TNF-α-induced cardiac fibroblast proliferation [47], demonstrating its pro-survival and pro-proliferative effects. It has also been reported that the differential levels of WISP1 expression during airway development are closely associated with lung function in asthma populations [48], suggesting that WISP1 might mediate asthmatic airway remodeling. Further, our previous studies demonstrated for the first time that WISP1 is upregulated in animal models of asthma and induce collagen deposition and Col1a1 and Fn1 release from lung fibroblast in vitro [22]. Cumulative evidence suggested that WISP1 plays a critical role in asthmatic airway remodeling, but its specific molecular effects on ASM remodeling are rarely reported and still maintain unclear. In this study, our results suggested that WISP1 is involved in the pathogenesis of ASM remodeling in asthma. Although we only assessed the degree of ASM remodeling by H&E analysis and detected the levels of α-smooth muscle actin by immunohistochemistry and did not examine the expression of other muscle proteins, these results have given some hints that WISP1 depletion could suppress ASM contractile protein expression to effectively attenuate OVA-induced hypertrophy of ASM in asthma. For the roles of WISP1 in airway remodeling, previous studies revealed that WISP1 could mediate lung fibroblast proliferation and collagen release [30], while our results in this study further suggested that WISP1 may be a potent and rapid inducer of ASM proliferation and hypertrophy in asthma.
Main candidate cells involved in airway remodeling include T-lymphocytes, airway epithelial cells, ASM cells, and lung fibroblast [49–51]. In particular, ASM cell is an important effector cell of pathological remodeling in airway in patients with asthma. In biopsies of the bronchial wall, increases in the mass of ASM, the crucial cell regulating bronchomotor tone, in part defines airway remodeling in severe asthma [52, 53]. Our results revealed that WISP1 depletion could attenuate OVA-induced hypertrophy of ASM in asthmatic airway remodeling, while the cellular mechanism of increased ASM mass still maintains unclear. We next assessed the effects of WISP1 on bronchial smooth muscle cells in vitro. WISP1 treatment leads to significant hBSMC hypertrophy and proliferation. The mediating effects of WISP1 on hBSMC are seemingly weaker than that of TGF-β, but the difference between them was not significant. Therefore, in vitro experimental results further suggested that WISP1 might play an important role in ASM remodeling. Although previous studies have revealed that WISP1 exerts prohypertrophic and mitogenic effects stimulating myocyte hypertrophy, fibroblast proliferation, and collagen expression [19, 30], the roles of WISP1 in hBSMC were never described and firstly revealed in this work.
In addition, our results showed that both WISP1- and TGF-β-induced abnormal activation of hBSMC could be partially suppressed by pretreatment with an Akt inhibitor. Accumulated evidences have suggested that WISP1, a target of the WNT pathway, could activate GSK3β/β-catenin signaling by inducing phosphorylation of Akt [21, 22, 54, 55]. TGF-β can also stimulate β-catenin nuclear translocation via GSK3β signaling in ASM remodeling. Therefore, it is possible that WISP1 may be involved in GSK3β-dependent noncanonical TGF-β signaling in asthmatic airway remodeling.
TGF-β, a multifunctional cytokine, is one of the major players in determining the structural and functional abnormalities of ASM in asthma [56]. TGF-β-induced activation of PI3K/Akt signaling plays an important role in pathological remodeling of multiple organs such as the lung, kidney, skin, and liver [57]. Moreover, it is revealed that WISP1 could be induced via PI3K-dependent Akt signaling in human coronary artery SMC. These results further suggested that some components of TGF-β and WNT signaling are mutual targets of each other. Therefore, we next detected the possibility that TGF-β might induce the expression of WISP1 via PI3K/GSK3β signaling. Our results showed that the levels of PI3K, p-Akt, p-GSK3β, and WISP1 were upregulated in TGF-β-treated group, but p-GSK3β and WISP1 levels could be significantly inhibited when cells were pretreated with an Akt inhibitor before TGF-β stimulation. Previous studies have demonstrated that TGF-β can modulate ASM function and phenotype through the PI3K signaling pathway [58, 59]. TGF-β can also induce the abundance of β-catenin via inactivation of GSK-3β and rescue it from proteasomal degradation, leading to a subsequent increase in active β-catenin in ASM cells [16, 26]. However, our results in this study offered new highlights and revealed that TGF-β treatment could induce upregulation of WISP1 levels by activating Akt-dependent PI3K/GSK3β signaling in hBSMC, suggesting that TGF-β-mediated WISP1 may contribute to ASM remodeling in asthma.
WISP1, a member of the CCN family of proteins, is involved in multiple signaling networks that determine cell differentiation, cell growth, and cell survival in tissues ranging from the cardiovascular-pulmonary system to the reproductive system. For example, WISP1 requires activation of PI3K and Akt pathways to promote neuronal cell survival [60]. Furthermore, WISP1 through PI3K/Akt/GSK3β signaling, induces significant proliferation of SMC derived from human saphenous vein (VSMC) [22]. Therefore, it is possible that WISP1 may activate PI3K/Akt/GSK3β signaling to induce remodeling of ASM. In this study, it was found that WISP1 could induce abnormal activation of hBSMC, accompanying with increased expression of PI3K, p-Akt, and p-GSK3β. However, WISP1-induced abnormal activation of hBSMC could be partially suppressed by pretreatment with an AKT inhibitor, accompanying with depressed expression of p-GSK3β, but the levels of PI3K were not significantly suppressed by an Akt inhibitor. Interestingly, it was found that WISP1 mRNA levels were also upregulated in WISP1-treated hBSMC, and the process was still inhibited by an Akt inhibitor. Although, it has been demonstrated that WISP1 can activate PI3K/Akt signaling to induce the pro-survival factor Survivin. Furthermore, WISP1 also stimulates PI3K-Akt-dependent GSK3β phosphorylation and β-catenin nuclear translocation in cardiomyocytes [41]. However, our results suggested for the first time that WISP1 can induce proliferation and hypertrophy of hBSMC by regulating PI3K-Akt-dependent phosphorylation of GSK3β. Meanwhile, WISP1 treatment could also induce its own expression through activating PI3K-dependent Akt/GSK3β signaling. So, it could be speculated that WISP1, following its initial induction, may sustain its own expression by autoregulation, and thereby further enhance ASM remodeling in vivo. As a whole, these results offered new insights into the potentially important role of WISP1 in asthmatic ASM remodeling and direct evidences for our previous hypothesis. As this study just preliminary revealed that WISP1 is involved in a complex mechanism of ASM remodeling, further studies are needed to fully appreciate the mechanistic roles of WISP1 in this pathological process.
ASM hypertrophy and hyperplasia in asthma involve multiple inflammatory cells and a wide array of mediators. We report here for the first time that the autocrine and paracrine effects of WISP1 can initiate and perpetuate the pathological remodeling of asthma by inducing anomalous activation of ASM cell. We do not rule out the possibility that the ASM cell undergoing proliferation and hypertrophy may be from different lineages and result from activation of distinct signal transduction pathways. However, our results demonstrate that WISP1 can mediate ASM remodeling in vivo and induce proliferation and hypertrophy of hBSMC via induced PI3K-Akt-dependent phosphorylation of GSK3β in vitro. TGF-β could also activate PI3K-dependent GSK3β signaling to induce WISP1 expression. Moreover, WISP1 could induce its own expression in hBSMC. Our future studies will investigate the downstream signaling pathways involved in WISP1-induced hBSMC activation.
References
Bousquet, J., P.K. Jeffery, and W.W. Busse. 2000. Asthma. From bronchoconstriction to airways inflammation and remodeling. American Journal of Respiratory and Critical Care Medicine 161: 1720–1745.
Kumar, R.K. 2001. Understanding airway wall remodeling in asthma: a basis for improvements in therapy? Pharmacology and Therapeutics 91: 93–104.
Chiappara, G., R. Gagliardo, and A. Siena. 2001. Airway remodelling in the pathogenesis of asthma. Current Opinion in Allergy and Clinical Immunology 1: 85–93.
Dekkers, B.G., H. Maarsingh, H. Meurs, and R. Gosens. 2009. Airway structural components drive airway smooth muscle remodeling in asthma. Proceedings of the American Thoracic Society 6(8): 683–692.
Suganuma, N., S. Ito, H. Aso, M. Kondo, M. Sato, M. Sokabe, and Y. Hasegawa. 2012. STIM1 regulates platelet-derived growth factor-induced migration and Ca2+ influx in human airway smooth muscle cells. PLoS One 7(9), e45056.
Michaeloudes, C., M.B. Sukkar, N.M. Khorasani, P.K. Bhavsar, and K.F. Chung. 2011. TGF-β regulates Nox4, MnSOD and catalase expression, and IL-6 release in airway smooth muscle cells. American Journal of Physiology. Lung Cellular and Molecular Physiology 300(2): L295–L304.
Pera, T., C. Atmaj, M. vander Vegt, A.J. Halayko, J. Zaagsma, and H. Meurs. 2012. Role for TAK1 in cigarette smoke-induced proinflammatory signaling and IL-8 release by human airway smooth muscle cells. American Journal of Physiology. Lung Cellular and Molecular Physiology 303(3): L272–L278.
Benayoun, L., A. Druilhe, M.C. Dombret, M. Aubier, and M. Pretolani. 2003. Airway structural alterations selectively associated with severe asthma. American Journal of Respiratory and Critical Care Medicine 167: 1360–1368.
Partridge, M.R., T. van der Molen, S.E. Myrseth, and W.W. Busse. 2006. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulmonary Medicine 6: 13.
Nakagawa, T., and M. Hoshino. 2004. Airway remodeling in asthma: an introduction. Clinical Reviews in Allergy and Immunology 27: 1–2.
Barnes, P.J., and I.M. Adcock. 2009. Glucocorticoid resistance in inflammatory diseases. Lancet 373: 1905–1917.
Halayko, A.J., T. Tran, S.Y. Ji, A. Yamasaki, and R. Gosens. 2006. Airway smooth muscle phenotype and function: interactions with current asthma therapies. Current Drug Targets 7: 525e40.
Yeganeh, B., S. Mukherjee, L.M. Moir, and K. Kumawat. 2013. Novel non-canonical TGF-β signaling networks: emerging roles in airway smooth muscle phenotype and function. Pulmonary Pharmacology & Therapeutics 26(1): 50–63.
Baarsma, H.A., A.I. Spanjer, G. Haitsma, L.H. Engelbertink, and H. Meurs. 2011. Activation of Wnt/beta-catenin signaling in pulmonary fibroblasts by TGF-beta is increased in chronic obstructive pulmonary disease. PLoS One 6, e25450.
Carthy, J.M., F.S. Garmaroudi, Z. Luo, and B.M. McManus. 2011. Wnt3a induces myofibroblast differentiation by upregulating TGF-β signaling through Smad2 in a beta-catenin-dependent manner. PLoS One 6, e19809.
Gosens, R., H.A. Baarsma, I.H. Heijink, T.A. Oenema, and A.J. Halayko. 2010. De novo synthesis of {beta}-catenin via H-Ras and Mek regulates airway smooth muscle growth. FASEB Journal 24: 757e68.
Kumawat, K., M.H. Menzen, I.S. Bos, H.A. Baarsma, P. Borger, M. Roth, M. Tamm, A.J. Halayko, M. Simoons, A. Prins, D.S. Postma, M. Schmidt, and R. Gosens. 2013. Noncanonical WNT-5A signaling regulates TGF-β-induced extracellular matrix production by airway smooth muscle cells. FASEB Journal 27(4): 1631–1643.
Xu, L., R.B. Corcoran, J.W. Welsh, D. Pennica, and A.J. Levine. 2000. WISP-1 is a Wnt-1- and β-catenin-responsive oncogene. Genes and Development 14: 585–595.
Colston, J.T., S.D. de la Rosa, and M. Koehler. 2007. Wnt-induced secreted protein 1 is a prohypertrophic and profibrotic growth factor. Am J Physiol H eart Circ Physiol 293: H1839–H1846.
Jiang, F., C.J. Parsons, and B. Stefanovic. 2006. Gene expression profile of quiescent and activated rat hepatic stellate cells implicates Wnt signaling pathway in activation. Journal of Hepatology 45: 401–409.
Yang, M., X. Zhao, and Y. Liu. 2013. A role for WNT1-inducible signaling protein-1 in airway remodeling in a rat asthma model. International Immunopharmacology 17(2): 350–357.
Reddy, V.S., A.J. Valente, and P. Delafontaine. 2011. Interleukin-18/WNT1-inducible signaling pathway protein-1 signaling mediates human saphenous vein smooth muscle cell proliferation. Journal of Cellular Physiology 226(12): 3303–3315.
Katoh, M., and M. Katoh. 2006. Cross-talk of WNT and FGF signaling pathways at GSK3beta to regulate beta-catenin and SNAIL signaling cascades. Cancer Biology and Therapy 5(9): 1059–1064.
Deng, H., G.A. Dokshin, J. Lei, A.M. Goldsmith, and K.N. Bitar. 2008. Inhibition of glycogen synthase kinase-3beta is sufficient for airway smooth muscle hypertrophy. Journal of Biological Chemistry 283(15): 10198–10207.
Oenema, T.A., M. Smit, L. Smedinga, K. Racké, A.J. Halayko, H. Meurs, and R. Gosens. 2012. Muscarinic receptor stimulation augments TGF-β1-induced contractile protein expression by airway smooth muscle cells. American Journal of Physiology. Lung Cellular and Molecular Physiology 303(7): L589–L597.
Baarsma, H.A., M.H. Menzen, A.J. Halayko, H. Meurs, H.A. Kerstjens, and R. Gosens. 2011. Beta-catenin signaling is required for TGF-β1-induced extracellular matrix production by airway smooth muscle cells. American Journal of Physiology. Lung Cellular and Molecular Physiology 301(6): L956–L965.
National Research Council. 1996. Guide for the care and use of laboratory animals, 21–55. Washington, DC: National Academy Press.
Nabe, T., C.L. Zindl, Y.W. Jung, R. Stephens, and A. Sakamoto. 2005. Induction of a late asthmatic response associated with airway inflammation in mice. European Journal of Pharmacology 521: 144–155.
Ho, W., and A. Furst. 1973. Intratracheal instillation method for mouse lungs. Oncology 27: 385–393.
Königshoff, M., M. Kramer, and N. Balsara. 2009. WNT1-inducible signaling protein-1 mediates pulmonary fibrosis in mice and is upregulated in humans with idiopathic pulmonary fibrosis. Journal of Clinical Investigation 119(4): 772–787.
Cho, J.Y., M. Miller, K.J. Baek, J.W. Han, J. Nayar, and S.Y. Lee. 2004. Inhibition of airway remodeling in IL-5-deficient mice. Journal of Clinical Investigation 113(4): 551–560.
Qiao, Chong, W. Chunhui, Z. Jiao, L. Caixia, and S. Tao. 2012. Elevated expression of KiSS-1 in placenta of Chinese women with early-onset preeclampsia. PLoS One 7(11), e48937.
Nabe, T., T. Morishita, K. Matsuya, A. Ikedo, M. Fujii, N. Mizutani, and S. Yoshino. 2011. Complete dependence on CD4+ cells in late asthmatic response, but limited contribution of the cells to airway remodeling in sensitized mice. Journal of Pharmacological Sciences 116(4): 373–383.
Bogard, A.S., C. Xu, and R.S. Ostrom. 2011. Human bronchial smooth muscle cells express adenylyl cyclase isoforms 2, 4, and 6 in distinct membrane microdomains. Journal of Pharmacology and Experimental Therapeutics 337(1): 209–217.
Cui, X.L., A.M. Schlesier, E.L. Fisher, C. Cerqueira, and R.P. Ferraris. 2005. Fructose-induced increases in neonatal rat intestinal fructose transport involve the PI3-kinase/Akt signaling pathway. American Journal of Physiology. Gastrointestinal and Liver Physiology 288: G1310–G1320.
Kierbel, A., A. Gassama-Diagne, K. Mostov, and J. Engel. 2005. The phosphoinositol-3-kinase-protein kinase B/Akt pathway is critical for Pseudomonas aeruginosa strain PAK internalization. Molecular Biology of the Cell 16: 2577–2585.
Kozikowski, A.P., H. Sun, J. Brognard, and P.A. Dennis. 2003. Novel PI analogues selectively block activation of the pro-survival serine/threonine kinase Akt. Journal of the American Chemical Society 125: 1144–1145.
Chandrasekar, B., S. Mummidi, W.C. Claycomb, and R. Mestril. 2005. Interleukin-18 is a prohypertrophic cytokine that acts through a phosphatidylinositol 3-kinase-phosphoinositide-dependent kinase-1-Akt-GATA4 signaling pathway in cardiomyocytes. Journal of Biological Chemistry 280(6): 4553–4567.
Goncharova, E.A., D.A. Goncharov, and V.P. Krymskaya. 2006. Assays for in vitro monitoring of human airway smooth muscle (ASM) and human pulmonary arterial vascular smooth muscle (VSM) cell migration. Nature Protocols 1: 2933–2939.
Zhang, J., L. Shan, L. Koussih, N.S. Redhu, A.J. Halayko, J. Chakir, and A.S. Gounni. 2012. Pentraxin 3 (PTX3) expression in allergic asthmatic airways: role in airway smooth muscle migration and chemokine production. PLoS One 7(4), e34965.
Balachandar, V., D. Sumanth, K.V. Prabhu, and M. Srinivas. 2010. WNT1-inducible signaling pathway protein-1 activates diverse cell survival pathways and blocks doxorubicin-induced cardiomyocyte death. Cellular Signalling 22(5): 809–820.
Jude, J.A., K.G. Tirumurugaan, B.N. Kang, R.A. Panettieri, T.F. Walseth, and M.S. Kannan. 2012. Regulation of CD38 expression in human airway smooth muscle cells: role of class I phosphatidylinositol 3 kinases. American Journal of Respiratory Cell and Molecular Biology 47(4): 427–435.
Bentley, J.K., H. Deng, M.J. Linn, J. Lei, G.A. Dokshin, D.C. Fingar, K.N. Bitar, W.R. Henderson Jr., and M.B. Hershenson. 2009. Airway smooth muscle hyperplasia and hypertrophy correlate with glycogen synthase kinase-3(β) phosphorylation in a mouse model of asthma. American Journal of Physiology. Lung Cellular and Molecular Physiology 296(2): L176–L184.
Mohamed, J.S., M.A. Lopez, and A.M. Boriek. 2010. Mechanical stretch up-regulates microRNA-26a and induces human airway smooth muscle hypertrophy by suppressing glycogen synthase kinase-3β. Journal of Biological Chemistry 285(38): 29336–29347.
Clifford, R.L., K. Deacon, and A.J. Knox. 2008. Novel regulation of vascular endothelial growth factor-a (Vegfa) by transforming growth factor (Beta)1: requirement for Smads, (beta)-catenin, and Gsk(beta). Journal of Biological Chemistry 283(51): 35337–35353.
Cheon, S.S., P. Nadesan, R. Poon, and B.A. Alman. 2004. Growth factors regulate beta-catenin-mediated Tcf-dependent transcriptional activation in fibroblasts during the proliferative phase of wound healing. Experimental Cell Research 293(2): 267–274.
Venkatachalam, K., B. Venkatesan, A.J. Valente, P.C. Melby, S. Nandish, J.E. Reusch, R.A. Clark, and B. Chandrasekar. 2009. WISP1, a pro-mitogenic, pro-survival factor, mediates tumor necrosis factor-alpha (TNF-alpha)-stimulated cardiac fibroblast proliferation but inhibits TNF-alpha-induced cardiomyocyte death. Journal of Biological Chemistry 284(21): 14414–14427.
Sunita, S., T. Kelan, and C. Vincent. 2010. A role for Wnt signaling genes in the pathogenesis of impaired lung function in asthma. American Journal of Respiratory and Critical Care Medicine 181: 328–336.
Broide, David H. 2008. Immunologic and inflammatory mechanisms that drive asthma progression to remodeling. Journal of Allergy and Clinical Immunology 121(3): 560–572.
Murphy, J., R. Summer, and A. Fine. 2008. Stem cells in airway smooth muscle: state of the art. Proceedings of the American Thoracic Society 5(1): 11–14.
Yu, F., X. Zhao, C. Li, Y. Li, Y. Yan, and L. Shi. 2012. Airway stem cells: review of potential impact on understanding of upper airway diseases. Laryngoscope 122(7): 1463–1469.
Damera, G., K.M. Druey, P.R. Cooper, V.P. Krymskaya, R.J. Soberman, Y. Amrani, and T. Hoshi. 2012. An RGS4-mediated phenotypic switch of bronchial smooth muscle cells promotes fixed airway obstruction in asthma. PLoS One 7(1), e28504.
Panettieri Jr., R.A., R. Covar, and E. Grant. 2008. Natural history of asthma: persistence versus progression—does the beginning predict the end? Journal of Allergy and Clinical Immunology 121: 607–613.
Bergmann, C., A. Akhmetshina, C. Dees, K. Palumbo, P. Zerr, C. Beyer, and J. Zwerina. 2011. Inhibition of glycogen synthase kinase 3β induces dermal fibrosis by activation of the canonical Wnt pathway. Annals of the Rheumatic Diseases 70(12): 2191–2198.
Rahmani, M., J.T. Read, J.M. Carthy, P.C. McDonald, and B.W. Wong. 2005. Regulation of the versican promoter by the β-catenin-T-cell factor complex in vascular smooth muscle cells. Journal of Biological Chemistry 280: 13019–13028.
Halayko, A.J., T. Tran, S.Y. Ji, A. Yamasaki, and R. Gosens. 2006. Airway smooth muscle phenotype and function: interactions with current asthma therapies. Current Drug Targets 7(5): 525–540.
Li, H.Y., Q.G. Zhang, J.W. Chen, S.Q. Chen, and S.Y. Chen. 2013. The fibrotic role of phosphatidylinositol-3-kinase/Akt pathway in injured skeletal muscle after acute contusion. International Journal of Sports Medicine 34(9): 789–794.
Yi, J.Y., I. Shin, and C.L. Arteaga. 2005. Type I transforming growth factor beta receptor binds to and activates phosphatidylinositol 3-Kinase. Journal of Biological Chemistry 280: 10870–10876.
Moir, L.M., T. Trian, Q. Ge, and P.R. Shepherd. 2011. Phosphatidylinositol 3-kinase isoform-specific effects in airway mesenchymal cell function. Journal of Pharmacology and Experimental Therapeutics 337: 557–566.
Wang, S., Z.Z. Chong, Y.C. Shang, and K. Maiese. 2012. Wnt1 inducible signaling pathway protein 1 (WISP1) blocks neurodegeneration through phosphoinositide 3 kinase/Akt1 and apoptotic mitochondrial signaling involving Bad, Bax, Bim, and Bcl-xL. Current Neurovascular Research 9(1): 20–31.
Acknowledgments
We are indebted to all members of the Molecular Medicine Laboratory and Experimental Animal Center of Chongqing Medical University. This study was supported by Chongqing Municipal Health Bureau 2011 Medical Scientific Research Project Funds (Key Project).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Mingjin Yang and Yuejun Du contributed equally to this work and should be regarded as co-first authors.
Rights and permissions
About this article
Cite this article
Yang, M., Du, Y., Xu, Z. et al. Functional Effects of WNT1-Inducible Signaling Pathway Protein-1 on Bronchial Smooth Muscle Cell Migration and Proliferation in OVA-Induced Airway Remodeling. Inflammation 39, 16–29 (2016). https://doi.org/10.1007/s10753-015-0218-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0218-x