Abstract
Current evidence shows that the majority of the damage induced during sepsis is pursuant to induction and overproduction of endogenous cytokines. Embelin has been reported to suppress cytokine expressions in inflammatory disorders. The present study was designed to investigate the effects of embelin on cecal and ligation and puncture (CLP)-induced rat sepsis. Single-dose administration of embelin 1 h after surgery significantly improved survival of rats with CLP-induced sepsis. In addition, embelin treatment reduced the serum levels of pro-inflammatory cytokines including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6 and decreased organ inflammation and injuries. Moreover, embelin suppressed the activation of p65 subunit of nuclear factor-kappa B (NF-κB) and signal transducers and activators of transcription 3 (STAT3). Collectively, these results indicated that embelin ameliorates sepsis in rats through suppressing STAT3 and NF-κB pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Sepsis remains a critical health problem and a major cause of death even in many modern intensive care units (ICU) [1, 2]. This complex syndrome is characterized by an imbalance between pro-inflammatory and anti-inflammatory response to pathogens [3]. Current evidence implies that the problem of sepsis was directly related to the exuberant production of pro-inflammatory molecules [3]. High circulating concentrations of these cytokines, such as tumor necrosis factor (TNF)-α and interleukin (IL)-1β, may indicate an increased risk of mortality [4]. Previous studies suggested that the treatments antagonizing the activities of these cytokines sometimes improve the survival in sepsis [5, 6]. In addition, the systemic inflammatory cascade in sepsis generally results in neutrophil sequestration in various organs [7]. The extravasation of neutrophils may lead to vascular dysfunction and parenchymal cell dysfunction [8]. The inappropriate activation and positioning of neutrophils also contribute to the pathological manifestations of multiple organ failure (MOF) following sepsis [9].
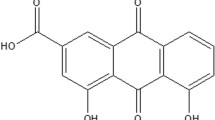
Embelin (2,5-dihydroxy-3-undecyl-1,4-benzoquinone), a major constituent of Embelia ribes Burm, is reported to possess antioxidant [10], antibacterial [11], and anti-inflammatory [12] activities. Previous study suggested that embelin has anti-inflammatory activities in irritant contact dermatitis due to the inhibition of inflammatory cytokines and the subsequent blockade of leukocyte accumulation [13]. Embelin was also found to lower myeloperoxidase (MPO) activities accompanied by reduced expression of TNF-α, IL-1β, and IL-6 in isolated colon tissue from dextran sulfate sodium-induced colitis in rats [14]. In addition, embelin has been reported to inhibit the activation of nuclear factor-kappa B (NF-κB) and signal transducers and activators of transcription 3 (STAT3) [15, 16], which mediated the expression of several important pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 during sepsis [17, 18].
However, so far, embelin has not been tested for its protective action against sepsis through its anti-inflammatory activities. Hence, the aim of the present study was to investigate the effect of embelin on pro-inflammatory cytokine expression and neutrophil infiltration in cecal and ligation and puncture (CLP)-induced rat sepsis.
METHODS AND MATERIALS
Animals
Specific pathogen-free (SPF) male Sprague-Dawley (SD) rats weighing 220–280 g were purchased from the Center for Animal Experiment of Wuhan University (Wuhan, Hubei, China). This study was approved by the Institution Animal Care and Use Committee of Wuhan University. All experiments were conducted in accordance with the guidelines of Animal Use and Care Committee of Wuhan University. Animals were maintained in individual ventilated cages under SPF conditions in the animal facility of Wuhan University.
Animal Model and Experimental Design
Rats were divided into three major groups: (1) sham group (n = 20): animals received only sham operations; (2) CLP group (n = 20): animals underwent CLP; and (3) embelin groups (3 subgroups, n = 20 in each subgroup): animals underwent CLP received an intraperitoneal injection of embelin. Polymicrobial sepsis was induced by CLP as previously described [19]. Briefly, rats were anesthetized with sodium pentobarbital (50 mg/kg, i.p., Sigma Chem Co., St. Louis, MO, USA) before the surgical procedure. A midline incision about 2 cm was made on the anterior abdomen. The cecum was isolated and the distal was ligated. Then, the cecum was punctured twice with a sterile 20-G needle and was squeezed to extrude the fecal material from the wounds. The cecum was placed back and the abdominal was closed. Animals in the sham group received a midline incision without cecal ligation and puncture. Each animal received a subcutaneous injection of 1 ml normal saline after surgery.
Rats were given an intraperitoneal injection of embelin (1, 10, and 100 mg/kg in subgroups 1–3, respectively; dissolved in dimethyl sulfoxide (DMSO); purchased from Selleck, Shanghai, China) 1 h after CLP under sterile conditions in the embelin groups, while rats in the sham group and CLP group were given intraperitoneal injection of DMSO (Sigma Chem Co., St. Louis, MO, USA). Liver tissue samples of five rats in each group were collected at 5 h after intraperitoneal injection of embelin or DMSO (6 h after CLP) for the measurement of p-p65 and p-STAT3. Blood and organ samples of another five rats in each group were collected at 20 h after CLP for biochemical analysis and histological evaluation. In each group, ten rats were taken for survival observation. Survival of rats was monitored at intervals of 12 h for 7 days after surgery.
Serum TNF-α, IL-1β, and IL-6 Measurement
In the present study, we measured the serum levels of TNF-α, IL-1β, and IL-6 at 20 h after CLP. Briefly, heparinized blood samples were centrifuged at 3000 rpm for 10 min at 4 °C. Thereafter, supernatants were stored at −80 °C until measurements. Plasma cytokines including TNF-α, IL-1β, and IL-6 were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits (R&D System Inc., Minneapolis, MN, USA) according to the manufacturer’s protocols.
Organ Injury Assessment
Plasma levels of lactate, cardiac troponin I (cTnI), urea nitrogen (BUN), and creatinine (Cr) were measured with an i-STAT 1 Analyzer (Abbott, Kyoto, Japan). Plasma levels of aspartate transaminase (AST), alanine transaminase (ALT), and lactate dehydrogenase (LDH) were determined using a TBA-2000FR System (TOSHIBA, Tokyo, Japan).
Myeloperoxidase Assay
The method of measuring MPO activity in organs was modified from that previously described [20]. Frozen tissues were homogenized in 50 mM of potassium phosphate buffer (pH 6.0) and centrifuged at 20,000g at 4 °C for 15 min. The supernatant was then discarded, and the pellet was resuspended in 50 mM acetic acid with 0.5 % hexadecyltrimethylammonium hydroxide detergent. After freezing and thawing for three cycles, samples were centrifuged at 20,000g for 15 min. Aliquots (0.3 ml) were added to 2.3 ml of the reaction mixture. Absorbance at 460 nm was measured immediately, and the rate of change in absorbance was used to calculate the activity of MPO. MPO activities are presented as units per milligram of tissue protein.
Western Blotting Analysis
Tissues were collected at 5 h after CLP and stored in liquid nitrogen until analysis. Proteins were extracted in lysis buffer. The concentrations of proteins were determined with a BCA protein assay kit (Pierce, Rockford, IL, USA). Proteins were then separated by SDS-PAGE and electrophoretically transferred onto membranes. The membrane was blocked with 5 % nonfat milk for 2 h at room temperature (RT) followed by the incubation with primary antibodies against p-p65 (ab119664) and p-STAT3 (ab76315) (Abcam, Shanghai, China) overnight at 4 °C and then incubated with secondary antibody (Boster, Wuhan, China). Protein bands were visualized with an ECL luminescence kit. The β-actin protein was used as an internal control.
Histological Investigation
Tissue samples were excised and fixed in 10 % neutral-buffered formalin, embedded in paraffin, cut into sections 5 μm in thickness, stained with hematoxylin-eosin, and examined under a light microscope. The histological evaluation was carried out by an expert pathologist who was blinded to the experimental details.
Statistical Analysis
Data are expressed as percentage, number, or mean ± SD. Comparison of several means was performed using one-way and repeated measure two-way analysis of variance followed by the Tukey-Kramer test to identify significant difference between groups. The overall difference in survival rate of septic rats was determined by survival analysis, and p values were determined by the log-rank test. All p values were two-tailed, and a p value of less than 0.05 was considered significant. All data were processed by the statistical analysis software SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Embelin Decreased Serum Levels of Pro-inflammatory Cytokines in Septic Rats
Expression of inflammatory cytokines, such as TNF-α, IL-1β, and IL-6, is known to be induced by CLP. As shown in Fig. 1, serum levels of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 showed a marked rise in septic rats as compared with sham-control animals (p < 0.05, resp.). To investigate whether embelin suppresses CLP-induced overexpression of cytokines in vivo, embelin was administrated (1, 10, or 100 mg/kg body weight, i.p.) 1 h after CLP surgery. Compared to the CLP group, embelin significantly reduced the serum levels of TNF-α, IL-1β, and IL-6 in a dose-dependent manner at 20 h after surgery (p < 0.05, resp.).
Serum levels of pro-inflammatory cytokines in septic rats treated with or without embelin. Serum levels of TNF-α, IL-1β, and IL-6 were significantly increased in septic rats as compared with sham-control animals. Treatment with embelin reduced serum levels of pro-inflammatory cytokines in a dose-dependent manner. Compared to other groups, *p < 0.05, **p < 0.01; compared to the CLP group, # p < 0.05, ## p < 0.01.
Embelin Prevents Multi-organ Dysfunction
Embelin has been shown to prevent organ dysfunctions. As seen in Table 1, plasma levels of cTnI, AST, and ALT were significantly lower than those obtained from CLP rats (p < 0.05, resp.). Plasma levels of BUN and Cr also significantly decreased in the embelin group compared to the CLP group (p < 0.05, resp.). In addition, embelin treatment appeared to protect the microcirculation; plasma lactate and LDH were significantly lower in embelin-treated rats than in untreated CLP rats (p < 0.05, resp.).
Effects of Embelin on MPO Activities in Organs
As reported previously [21], organ MPO activities were increased in septic rats. In the present study, organ MPO activities in septic rats were significantly increased at 20 h after CLP (p < 0.05, resp.). Compared to the CLP group, treatment with embelin significantly reduced organ MPO activities in the embelin groups (p < 0.05, resp.) (Fig. 2). These results suggested that embelin reduced organ neutrophil infiltration in rats with CLP-induced sepsis.
Embelin Reduced CLP-Induced Activations of STAT3 and NF-κB Signaling in the Liver
In the present study, we detected NF-κB and STAT3 activations in the liver (Fig. 3). Our results showed that CLP led to significantly increased activations of NF-κB and STAT3, while treatment with embelin markedly reduced the phosphorylation of NF-κB and STAT3 in the injured liver of septic rats (p < 0.05, resp.). Besides, embelin inhibited the phosphorylation of NF-κB and STAT3 in a dose-dependent manner.
Embelin reduced CLP-induced activations of NF-κB and STAT3 in septic rats. The protein levels of p-p65 and p-STAT3 were determined using Western blot assay at 6 h after CLP. Embelin significantly decreased the phosphorylation of NF-κB p65 and STAT3 in the injured liver of septic rats. Compared to other groups, **p < 0.01; compared to the CLP group, # p < 0.05, ## p < 0.01.
Effects of Embelin on Organ Histological Changes
As seen in Fig. 4, distal ileum, lung, and liver were collected for histopathologic evaluation. On the basis of histological investigation, embelin was found to prevent the CLP-induced intestinal mucosal damage with reduced neutrophil infiltration and improved villous height. Sepsis also led to pulmonary and hepatic injuries 20 h after CLP surgery, and septic organ injuries were associated with increased neutrophil infiltration. Those injuries were significantly improved in septic animals treated with embelin.
Effects of Embelin on the Survival Rate of Septic Rats
To examine whether embelin could prevent CLP-induced death, a 7-day survival observation was carried out. As seen in Fig. 5, nine of ten rats (90 %) in the CLP group died within 1–5 days after surgery, while seven of ten (70 %) rats, four of ten (40 %) rats, and two of ten (20 %) rats died in the embelin subgroup 1–3, respectively. All rats survived in the sham-control group. The overall difference in survival rate between rats treated with or without embelin was significant (p < 0.05, resp.).
Effects of embelin on survival of septic rats. Survival of rats was monitored at intervals of 12 h for 7 days. Nine of ten (90 %) rats in the CLP group died in the first 5 days, while only two of ten (20 %) rats treated with embelin (100 mg/kg BW) died after CLP. The overall difference in survival rate between CLP group and embelin groups was significant. Compared to the CLP group, # p < 0.05, ## p < 0.01.
DISCUSSION
Various animal models have been used to investigate the pathophysiology of sepsis and to test potential therapeutics. Among those models, CLP-induced sepsis model is currently considered as gold standard in experimental sepsis studies [17, 18]. In this study, we used a rat CLP model to investigate the protective effects of embelin in sepsis. CLP-induced sepsis provoked systemic release of pro-inflammatory cytokines and neutrophil infiltrations in major organs. The injection of embelin resulted in significant decrease of serum pro-inflammatory cytokines, reduced neutrophil infiltration and NF-κB expression in organs, and improved morphology. In addition, treatment with embelin improves the survival rate of rats that underwent sepsis.
The inflammatory response that characterizes sepsis results from excessive pro-inflammatory cytokines, while the anti-inflammatory reaction fails to cause adequate immunosuppression [22]. Excessive production and release of pro-inflammatory cytokines during sepsis are associated with the uncontrolled inflammatory responses, which are attributed to tissue damage and multiple organ failure (MOF). Numerous anti-inflammatory agents have been used to prevent tissue or organ damage induced by abundant inflammatory cytokines in sepsis [23–25]. The results of those studies suggested that the anti-inflammatory agents could protect animals from septic injuries and improve survival. Embelin was also found to reduce inflammatory cytokine expressions and to inhibit neutrophil accumulation in experimental colitis and irritant contact dermatitis [13, 14]. In this study, to investigate the protective effects of embelin on CLP-induced rat sepsis, a single dose of embelin was administrated 1 h after CLP surgery. Our results showed that embelin treatment reduced serum levels of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6. In addition, treatment with embelin resulted in decreased neutrophil infiltration and improved organ morphology.
The activation of the NF-κB plays a central role in inflammation through its ability to induce transcription of pro-inflammatory genes [26]. The pathophysiology of sepsis involves complex inflammatory mediator networks, and NF-κB activation is a central event leading to the activation of these networks [27]. In addition, NF-κB activation results in increased gene expression and biosynthesis of pro-inflammatory cytokines in sepsis [28]. Previous studies suggested that suppression of NF-κB activation resulted in improved prognosis of sepsis [29, 30]. Embelin is known to suppress the activation of NF-κB induced by inflammatory and carcinogenic agents [15]. Therefore, it is possible that embelin reveals its protective effects on sepsis via inhibiting the activation of NF-κB. To test this hypothesis, we detected organ NF-κB activities in this study. Our results showed that embelin reduced organ NF-κB activities of septic rats.
STAT3, a member of the STAT family, is another important transcriptional factor mediating cytokine signaling during sepsis and septic shock. Riley et al. reported that STAT3 deficiency in neutrophils and macrophages fails to respond to IL-10 and that high levels of TNF-α are secreted after inflammatory stimuli [31]. The conditional STAT3−/− mice exhibited an increased lethality with hepatic and renal injuries in CLP-induced sepsis [32]. Those results suggested that STAT3 is crucial in regulating systemic inflammation. In addition, unphosphorylated STAT3 has been reported to mediate the anti-inflammatory pathway of alpha7nAChR and inhibit cytokine production in sepsis [33]. Moreover, inhibition of STAT3 phosphorylation is able to ameliorate sepsis in mice [34]. Our results showed that embelin significantly inhibited the phosphorylation of STAT3 in CLP-induced sepsis. Thus, it is possible that embelin ameliorated rat sepsis via downregulating the STAT3 pathway.
CONCLUSION
Our results indicate that embelin may have beneficial effects in a rat model of sepsis that mimics the systemic release of pro-inflammatory cytokines, organ inflammation, and injuries via suppressing the activation of NF-κB p65 and STAT3. Thus, the treatment with embelin may be effective in improving the prognosis of sepsis.
REFERENCES
Ortíz, G., C. Dueñas, F. Rodríguez, et al. 2014. Epidemiology of sepsis in Colombian intensive care units. Biomédica 34: 40–47.
Levy, M.M., M.P. Fink, J.C. Marshall, et al. 2001. SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Critical Care Medicine 2003(31): 1250–1256.
Hotchkiss, R.S., and I.E. Karl. 2003. The pathophysiology and treatment of sepsis. New England Journal of Medicine 348: 138.
Hack, C.E., L.A. Aarden, and L.G. Thijs. 1997. Role of cytokines in sepsis. Advances in Immunology 66: 95–101.
Lally, K.P., E. Cruz, and H. Xue. 2000. The role of anti-tumor necrosis factor-α and interleukin-10 in protecting murine neonates from Escherichia coli sepsis. Journal of Pediatric Surgery 35: 852–854. discussion 855.
Panacek, E.A., J.C. Marshall, T.E. Albertson, et al. 2004. Efficacy and safety of the monoclonal anti-tumor necrosis factor antibody F(ab’)2 fragment afelimomab in patients with severe sepsis and elevated interleukin-6 levels. Critical Care Medicine 32: 2173–2182.
Işeri, S.O., G. Sener, B. Saglam, et al. 2005. Oxytocin protects against sepsis-induced multiple organ damage: role of neutrophils. Journal of Surgical Research 126: 73–81.
Neviere, R.R., G. Cepinskas, W.S. Madorin, et al. 1999. LPS pretreatment ameliorates peritonitis-induced myocardial inflammation and dysfunction: role of myocytes. American Journal of Physiology 277: H885–H892.
Brown, K.A., S.D. Brain, J.D. Pearson, et al. 2006. Neutrophils in development of multiple organ failure in sepsis. Lancet 368: 157–169.
Joshi, R., J.P. Kamat, and T. Mukherjee. 2007. Free radical scavenging reactions and antioxidant activity of embelin: biochemical and pulse radiolytic studies. Chemico-Biological Interactions 167: 125–134.
Chitra, M., S. Devi, and E. Sukumar. 2003. Antibacterial activity of embelin. Fitoterapia 74: 401–403.
Chitra, M., E. Sukumar, V. Suja, et al. 1994. Antitumor, anti-inflammatory and analgesic property of embelin, a plant product. Chemotherapy 40: 109–113.
Kalyan Kumar, G., R. Dhamotharan, N.M. Kulkarni, et al. 2011. Embelin reduces cutaneous TNF-α level and ameliorates skin edema in acute and chronic model of skin inflammation in rats. European Journal of Pharmacology 662: 63–69.
Kumar, G.K., R. Dhamotharan, N.M. Kulkarni, et al. 2011. Embelin ameliorates dextran sodium sulfate-induced colitis in rats. International Immunopharmacology 11: 724–731.
Ahn, K.S., G. Sethi, and B.B. Aggarwal. 2007. Embelin, an inhibitor of X chromosome-linked inhibitor-of-apoptosis protein, blocks nuclear factor-κB (NF-κB) signaling pathway leading to suppression of NF-κB-regulated antiapoptotic and metastatic gene products. Molecular Pharmacology 71: 209–219.
Heo, J.Y., H.J. Kim, S.M. Kim, et al. 2011. Embelin suppresses STAT3 signaling, proliferation, and survival of multiple myeloma via the protein tyrosine phosphatase PTEN. Cancer Letters 308: 71–80.
Abraham, E. 2003. Nuclear factor-kB and its role in sepsis-associated organ failure. Journal of Infectious Diseases 187(Suppl 2): S364–S369.
Yu, Z., W. Zhang, and B.C. Kone. 2002. Signal transducers and activators of transcription 3 (STAT3) inhibits transcription of the inducible nitric oxide synthase gene by interacting with nuclear factor kappaB. Biochemical Journal 367: 97–105.
Williams, D.L., T. Ha, C. Li, et al. 1999. Early activation of hepatic NFkappaB and NF-IL6 in polymicrobial sepsis correlates with bacteremia, cytokine expression, and mortality. Annals of Surgery 230: 95–104.
Hillegass, L.M., D.E. Griswold, B. Brickson, et al. 1990. Assessment of myeloperoxidase activity in whole rat kidney. Journal of Pharmacological Methods 24: 285–295.
Rittirsch, D., M.S. Huber-Lang, M.A. Flierl, et al. 2009. Immunodesign of experimental sepsis by cecal ligation and puncture. Nature Protocols 4: 31–36.
Sagy, M., Y. Al-Qaqaa, and P. Kim. 2013. Definitions and pathophysiology of sepsis. Current Problems in Pediatric and Adolescent Health Care 43: 260–263.
Gong, X., L. Zhang, R. Jiang, et al. 2013. Anti-inflammatory effects of mangiferin on sepsis-induced lung injury in rats via up-regulation of heme oxygenase-1. Journal of Nutritional Biochemistry 24: 1173–1181.
Zou, Y., T. Tao, Y. Tian, et al. 2013. Ginsenoside Rg1 improves survival in a murine model of polymicrobial sepsis by suppressing the inflammatory response and apoptosis of lymphocytes. Journal of Surgical Research 183: 760–766.
Albayrak, A., Z. Halici, B. Polat, et al. 2013. Protective effects of lithium: a new look at an old drug with potential antioxidative and anti-inflammatory effects in an animal model of sepsis. International Immunopharmacology 16: 35–40.
Baldwin Jr., A.S. 1996. The NF-kappa B and I kappa B proteins: new discoveries and insights. Annual Review of Immunology 14: 649–683.
Liu, S.F., and A.B.. Malik. 2006. NF-κB activation as a pathological mechanism of septic shock and inflammation. American Journal of Physiology - Lung Cellular and Molecular Physiology 290: L622–L645.
Brown, M.A., and W.K. Jones. 2004. NF-kappaB action in sepsis: the innate immune system and the heart. Frontiers in Bioscience 9: 1201–1217.
Ang, S.F., S.M. Moochhala, P.A. MacAry, et al. 2011. Hydrogen sulfide and neurogenic inflammation in polymicrobial sepsis: involvement of substance P and ERK-NF-kB signaling. PLoS ONE 6: e24535.
Zhang, Y., Li, R., Zhu, J., et al. 2014. Etomidate increases mortality in septic rats through inhibition of nuclear factor kappa-B rather than by causing adrenal insufficiency. J Surg Res.
Riley, J.K., K. Takeda, S. Akira, et al. 1999. Interleukin-10 receptor signaling through the JAK-STAT pathway. Requirement for two distinct receptor-derived signals for anti-inflammatory. Journal of Biological Chemistry 274: 16513–16521.
Matsukawa, A., K. Takeda, S. Kudo, et al. 2003. Aberrant inflammation and lethality to septic peritonitis in mice lacking STAT3 in macrophages and neutrophils. Journal of Immunology 171: 6198–6205.
Peña, G., B. Cai, J. Liu, et al. 2010. Unphosphorylated STAT3 modulates alpha7 nicotinic receptor signaling and cytokine production in sepsis. European Journal of Immunology 40: 2580–2589.
Guo, W., W. Liu, G. Chen, et al. 2012. Water-soluble andrographolide sulfonate exerts anti-sepsis action in mice through down-regulating p38 MAPK, STAT3 and NF-κB pathways. International Immunopharmacology 14: 613–619.
ACKNOWLEDGMENTS
We would like to thank the Center for Animal Experiment of Wuhan University (Wuhan, Hubei, China) for the assistance in animal experiment.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, XL., Huang, L. & Cao, J. Embelin Reduces Systemic Inflammation and Ameliorates Organ Injuries in Septic Rats Through Downregulating STAT3 and NF-κB Pathways. Inflammation 38, 1556–1562 (2015). https://doi.org/10.1007/s10753-015-0130-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0130-4