Abstract
Transforming growth factor-beta 1 (TGF-β1) is a multifunctional cytokine that plays a pivotal role in airway remodeling observed in the asthmatic airways. C to T base substitution at -509 promoter position in the TGF-β1 gene leads to its increased expression which contributes to airway remodeling in bronchial asthma. We sought to evaluate the association of TGF-β1 -509 C/T promoter variant with clinical asthma and varying degrees of disease severity. Three hundred and eighty-two clinically diagnosed asthma patients and 410 healthy controls were enrolled for the study. Patients were classified into severity classes according to the Global Initiative for Asthma (GINA) guidelines. TGF-β1 -509 C/T genotyping was carried out by amplification refractory mutation system polymerase chain reaction (ARMS-PCR) technique. In the present study, we found significantly higher frequency of TT genotype in asthma patients compared to controls (for TT vs. CC, p = 0.020). In addition, a significant difference was observed in the frequency of C and T allele in patients and controls (for T vs. C, p = 0.029). The heterozygous “CT” genotype was higher in moderate and severe asthmatics compared to mild subset of patients (for mild vs. moderate, p = 0.037). However, there was no significant distribution and association of variant allele with the severity subsets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Asthma is a chronic inflammatory disorder of the airways characterized by bronchial hyper-responsiveness that leads to airway remodeling and intractable airflow obstruction. Airways of individuals with asthma are characterized by a Th2-type inflammation, with an increased number of inflammatory cells that release mediators which trigger bronchoconstriction, mucus secretion, and airway remodeling. A number of mediators have the ability to induce structural changes; in particular, transforming growth factor-beta 1 (TGF-β1) has shown to affect many structural cells in vitro and in vivo and has been well-implicated in the remodeling process in asthma [1, 2]. Patients with asthma express increased TGF-β1 in the bronchoalveolar lavage (BAL) fluid in response to segmental allergen challenge, and TGF-β1 levels in the airway epithelium and submucosa correlate to airway basement membrane thickness, suggesting a direct role for TGF-β1 in airway remodeling [3]. In addition, bronchial biopsies of airway-smooth muscle tissue have shown higher mRNA expression for TGF-β1 from asthmatic patients as compared to non-asthmatic controls [4, 5].
These aforementioned findings clearly imply that TGF-β1 has a critical role to play in asthma pathogenesis. TGF-β1 is a seven-exon gene localized in chromosome 19q13.2 [6] which synthesizes 390 amino acid TGF-β1 prepropeptide. A particular C to T base substitution at position -509 from the first major transcription initiation site in the gene has been linked to promoter activity enhancement [7]. The T allele of TGF-β1 is associated with increased serum levels of TGF-β1 [8, 9] and IgE [10]. In view of the above, the present study was aimed to investigate the possible association of -509 C/T polymorphism with asthma susceptibility and with varying degrees of severity.
MATERIALS AND METHODS
Study Population
Three hundred and eighty-two asthma patients diagnosed by physician were recruited from Government General and Chest Hospital (Gandhi Medical College and Osmania Medical College, Hyderabad, India). No patient had evidence of chronic obstructive pulmonary disease, bronchiectasis, or any other lung disorder. Informed consent was obtained from all the subjects selected for the study. Epidemiological details such as age, gender, age of onset, addictions, inhabitation, and allergic information were taken through personal interview with the help of a standard questionnaire. A total of 410 age- and gender-matched participants who neither had evidence nor family history of asthma served as healthy controls. All the controls were recruited from the same demographic area and belonged to the same ethnic group as that of the patients. The study protocol was approved by the ethics committee at our institution.
Assessment of Severity
The patients were classified into three severity groups based on forced expiratory volume (FEV)1 % predicted as having mild (intermittent and persistent; FEV1 > 80 %), moderate (FEV1 60–80 %), or severe (FEV1 < 60 %) as defined by the Global Initiative for Asthma guidelines [11]. Lung function variables Forced Expiratory Volume in 1 Second (FEV1) Peak Expiratory Flow (PEF) and Forced Vital Capacity (FVC) of the patient were measured by pulmonary function test. The test was performed using a spirometer (Viasys Healthcare, Micromedical Limited, Kent, England) before and 15 min after bronchodilator inhalation (Salbutamol, 200 μg); the procedure as devised by the American Thoracic Society Standards [12]. The results were expressed as a percentage of the predicted normal value using Hankinson’s age- and race-adjusted prediction equation [13].
Genotyping of TGF-β1 -509 C/T Polymorphism
Genomic DNA was isolated from whole blood samples obtained from patients and control subjects by salting-out procedure [14]. The genotype for TGF-β1 C-509T (rs1800469) was determined by means of amplification refractory mutation system polymerase chain reaction (ARMS-PCR) method. Briefly, two complementary reactions were established for each allele consisting of target DNA; allele-specific ARMS primers (RC for C allele and RT for T allele) and the common primer (CF). A 349-bp region (-488 to -836 from the transcription start site) in the TGF-β1 gene promoter was targeted for amplification. The primers used are as follows: antisense (common forward) 5′CTA CGG CGT GGA GTG CTG AG3′, sense (reverse C-allele-specific) 5′AAG GGG CAA CAG GAC ACC TGG G3′, and sense (reverse T-allele-specific) 5′AAG GGG CAA CAG GAC ACC TGG A 3′. The optimized reaction mixture of 20 μl contained 100 ng of genomic DNA, 1× reaction buffer, 1.5 μM MgCl2, 30 μM of each dNTP, 0.16 μM of each primer, and 0.3 U of Taq DNA polymerase. The PCR amplification reaction consisted of initial denaturation at 94 °C for 4 min, followed by 35 cycles at 94 °C for 30 s, 61 °C for 20 s, and 72 °C for 30 s. The final extension step was at 72 °C for 6 min. The PCR products were electrophoresed on 2 % agarose gel stained with ethidium bromide and were visualized under ultraviolet light with a 100-bp ladder.
Statistical Analysis
Hardy–Weinberg equilibrium was tested for TGF-β1 -509 C/T variant. Any deviation in the allele and genotype frequencies between cases and healthy controls and within severity groups was tested for statistical significance using Yates’ corrected χ2 test and the odds ratio at 95 % confidence interval (C.I.) using Open EPI6 online statistical software (Open EPI v 2.3.1, from the Department of Epidemiology, Rollins School of public health, Emory University, Atlanta, GA 30322, USA). All the p values were two-sided, and the level of significance was considered at p < 0.05.
RESULTS
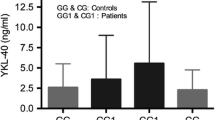
A total of 382 physician-diagnosed asthmatics and 410 healthy controls were recruited for the study. The demographic characteristics of patients and controls are presented in Table 1. In the study, there was no significant difference in number of males and females in both patient and control groups; however, the number of females were marginally higher in both the groups. Non-smokers were significantly higher in both cases and controls (p value = 0.001). The mean duration from which the patients were suffering was found to be 10.5 years. One hundred and fifty-four (40.31 %) patients had a family history of asthma whereas 228 (59.69 %) showed absence of family history. Out of the 382 asthma subjects, 96 (25.13 %), 124 (32.46 %), and 162 (42.41 %), respectively, belonged to mild, moderate, and severe classes of asthma. The lung function variables (FEV1, PEF, and FVC) with respect to severity classes are represented in Table 2. The genotypic distribution in asthmatics and healthy controls is shown in Table 3. In the co-dominant model of inheritance, the TT genotype was significantly found to be higher in patients than in controls (patients vs. controls, TT vs. CC, odds ratio (OR) at 95 % C.I. = 1.54 (1.08–2.19), p = 0.02, χ 2 = 5.3). Even the dominant genetic inheritance models showed significant results supporting the recessive genotype as being more common in asthma subjects (patients vs. controls, CT + TT vs. CC, OR at 95 % C.I. = 1.385 (1.03–1.84), p = 0.03, χ 2 = 4.591). However, there was no significant genotypic distribution in the recessive genetic inheritance model (CC + CT vs. TT, OR at 95 % C.I. = 1.37 (1.00–1.87), p = 0.06, χ 2 = 3.56). When allele frequencies were compared, the frequency of mutant allele “T” was significantly elevated in case patients than in their healthy counterparts (patients vs. controls; T vs. C, OR at 95 % C.I. = 1.325 (1.00–1.17), p = 0.029, χ 2 = 3.57) indicating considerable association of T allele in asthma subjects. Genotype and allelic distribution within severity groups was not notably significant, except in the case of a co-dominant inheritance model wherein the frequency of CT genotype was significantly higher in moderate as well as in severe subsets in comparison to mild subset of patients: (mild vs. moderate, OR at 95 % C.I. = 2.194 (1.101–4.370), p = 0.037, χ 2 = 4.311) and (mild vs. severe, OR at 95 % C.I. = 2.589 (1.336–5.019), p = 0.007, χ 2 = 7.213). Furthermore, there was neither significant association of the genotypes in the dominant and recessive inheritance model nor association of mutant allele within severity subsets. The genotypic distribution within the severity groups’, i.e., mild vs. moderate, mild vs. severe, and moderate vs. severe, is represented in Table 4.
DISCUSSION
Recent understanding of genetics has now recognized that asthma does not follow simple Mendelian mode of inheritance and is now characterized as a multifactorial disorder of the airways brought about by complex interaction between genetic and environmental factors. Several genes have been linked to asthma susceptibility of which one being TGF-β1 has shown to have a profound effect in the etiology of asthma. The transforming growth factor has now surfaced as a key mediator and a good candidate responsible for the subepithelial fibrosis observed in asthmatic lung. It is now known to activate multiple intracellular pathways, of which similar to mothers against decapentaplegic (Smad) proteins-mediated pathway is an important signaling pathway central to asthma pathogenesis [15]. Earlier studies on the mechanism of TGF-β1 in airway remodeling have shown that it activates gene transcription via binding to a heterodimeric receptor TGF-β1—a part of the activin receptor-like kinase (ALK) family [16]. TGF-β1 receptor I phosphorylate members of the Smad protein family initiate nuclear translocation and transcription leading to airway remodeling. TGF-β1 via the MAPK pathway, and by upregulation of the integrin receptor a5b1, further encourages the airway remodeling process by increasing the airway-smooth muscle mass [17]. A particular study has shown that -509 C/T polymorphism is located within a Yin Yang1 (YY1) consensus binding site [18]. Transfection with the construct containing the T-allele-enhanced YY1 binding and increased promoter activity compared to the C allele results in increased serum levels of TGF-β1 [8].
In the present study, we found positive association of this promoter variant in asthma. Our results demonstrate that the TT genotype was highly associated with clinical asthma (p = 0.020). When allelic frequencies were compared, mutant “T” allele frequency was found to be significantly higher in patients than in healthy controls, implying T allele as a risk factor in asthma pathogenesis (p = 0.029).
The numbers of previous studies have reported associations between polymorphisms in the TGF-β1 gene and the risk of asthma; nevertheless, the results have been contradictory. Our results are in accordance with studies from the population of the United Kingdom and the United States where C-509T demonstrated elevated risk of developing asthma [18, 7]. In contrast, the polymorphism was not associated with asthma risk in subjects of Czech [19], German [20], or Hong Kong [21] origin. According to a meta-analysis report [22], the risk appeared to be more evident in Asians rather than in Caucasian subjects, suggesting a possible influence of different genetic backgrounds and environmental exposures. Among Asians, Nagpal et al., in 2005 [23], found significant association in the North and West Indian populations; furthermore, Xia et al., in 2006, reported that polymorphism was to play a pronounced role in asthma susceptibility in Chinese population [24] alleviation.
In the present study, we found in the co-dominant inheritance model that the CT genotype was elevated both in moderate and severe asthmatics when compared to mild asthmatics. The heterozygous genotype “CT” perhaps may play a vital role in elevating the severity, for which the rationale is unknown and demands further investigation. In the further perusal, we did not find significant association of the genotypes either in the dominant inheritance model or in the recessive inheritance model; in addition, there was not any significant association of mutant allele within the severity subsets. Since asthma is a multifactorial disorder, linking a single gene with severity becomes tough. In contrast to the present study, Pulleyn et al., in 2001 [18] and Mak et al., in 2006 [21], have found a significant difference in the genotype frequency between patients with mild and severe asthma. This is the first study from Southern India reporting association of TGF-β1 -509 promoter variant with asthma while studies carried out in the Western and Northern populations of India also showed considerable association of the variant with asthma susceptibility. It is worthy to note that -509 C/T polymorphism is likely a candidate variant responsible in asthma risk in the Indian subcontinent.
CONCLUSION
In summary, we have shown the significant association of TGF-β1 -509 C/T variant with asthma risk in the South Indian population. In addition, we found higher frequency of heterozygous genotype CT in the co-dominant inheritance model in both moderate and severe asthmatics relative to mild asthmatics. However, we did not find any notable association of polymorphism with other inheritance models within the severity groups.
References
Makinde, T., R.F. Murphy, and D.K. Agrawal. 2007. The regulatory role of TGF-β in airway remodeling in asthma. Immunology and Cell Biology 85(5): 348–356.
Halwani, R., S. Al-Muhsen, H. Al-Jahdali, and Q. Hamid. 2011. Role of transforming growth factor-β in airway remodeling in asthma. American Journal of Respiratory Cell and Molecular Biology 44(2): 127–133.
Redington, A.E., J. Madden, A.J. Frew, R. Djukanovic, W.R. Roche, S.T. Holgate, and P.H. Howarth. 1997. Transforming growth factor-β 1 in asthma: measurement in bronchoalveolar lavage fluid. American Journal of Respiratory and Critical Care Medicine 156(2): 642–647.
Berger, P., P.O. Girodet, H. Begueret, O. Ousova, D.W. Perng, R. Marthan, et al. 2003. Tryptase-stimulated human airway smooth muscle cells induce cytokine synthesis and mast cell chemotaxis. The FASEB Journal 17(14): 2139–2141.
Xie, S., M.B. Sukkar, R. Issa, N.M. Khorasani, and K.F. Chung. 2007. Mechanisms of induction of airway smooth muscle hyperplasia by transforming growth factor-β. American Journal of Physiology-Lung Cellular and Molecular Physiology 293(1): L245.
Fujii, D., J.E. Brissenden, R. Derynck, and U. Francke. 1986. Transforming growth factor β gene maps to human chromosome 19 long arm and to mouse chromosome 7. Somatic Cell and Molecular Genetics 12(3): 281–288.
Salam, M.T., W.J. Gauderman, R. McConnell, P.C. Lin, and F.D. Gilliland. 2007. Transforming growth factor-β1 C-509T polymorphism, oxidant stress, and early-onset childhood asthma. American Journal of Respiratory and Critical Care Medicine 176(12): 1192.
Grainger, D.J., K. Heathcote, M. Chiano, H. Snieder, P.R. Kemp, J.C. Metcalfe, et al. 1999. Genetic control of the circulating concentration of transforming growth factor type β1. Human Molecular Genetics 8(1): 93–97.
Ueda, T., Niimi, A., Matsumoto, H., Takemura, M., Yamaguchi, M., Matsuoka, H., et al. TGFB1 promoter polymorphism C-509T and pathophysiology of asthma. Journal of Allergy and Clinical Immunology 121(3): 659–664.
Hobbs, K., J. Negri, M. Klinnert, L.J. Rosenwasser, and L. Borish. 1998. Interleukin-10 and transforming growth factor-β promoter polymorphisms in allergies and asthma. American Journal of Respiratory and Critical Care Medicine 158(6): 1958–1962.
Global Initiative for Asthma. 2002. Global strategy for asthma management and prevention. NIH Publication (02–3659).
Miller, M.R., J.A.T.S. Hankinson, V. Brusasco, F. Burgos, R. Casaburi, A. Coates, et al. 2005. Standardisation of spirometry. European Respiratory Journal 26(2): 319–338.
Hankinson, J.L., J.R. Odencrantz, and K.B. Fedan. 1999. Spirometric reference values from a sample of the general US population. American Journal of Respiratory and Critical Care Medicine 159(1): 179–187.
Lahiri, D.K., and J.I. Nurnberger Jr. 1991. A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Research 19(19): 5444.
Sagara, H., T. Okada, K. Okumura, H. Ogawa, C. Ra, T. Fukuda, and A. Nakao. 2002. Activation of TGF-beta/Smad2 signaling is associated with airway remodeling in asthma. Journal of Allergy and Clinical Immunology 110: 249–254.
Derynck, R., and Y.E. Zhang. 2003. Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature 425(6958): 577–584.
Chen, G., and N. Khalil. 2006. TGF-β1 increases proliferation of airway smooth muscle cells by phosphorylation of map kinases. Respiratory Research 7(1): 2.
Pulleyn, L.J., R. Newton, I.M. Adcock, and P.J. Barnes. 2001. TGFβ1 allele association with asthma severity. Human Genetics 109(6): 623–627.
Bučková, D., L. Izakovičová Hollá, P. Beneš, V. Znojil, and J. Vácha. 2001. TGF‐β1 gene polymorphisms. Allergy 56(12): 1236–1237.
Heinzmann, A., E. Bauer, K. Ganter, T. Kurz, and K.A. Deichmann. 2005. Polymorphisms of the TGF‐β1 gene are not associated with bronchial asthma in Caucasian children. Pediatric Allergy and Immunology 16(4): 310–314.
Mak, J.C., H. Leung, S.P. Ho, B.K. Law, A.S. Ho, W.K. Lam, et al. 2006. Analysis of TGF-β1 gene polymorphisms in Hong Kong Chinese patients with asthma. Journal of Allergy and Clinical Immunology 117(1): 92–96.
Zhang, Y., J. Zhang, J. Huang, X. Li, C. He, Tian, et al. 2010. Polymorphisms in the transforming growth factor‐β1 gene and the risk of asthma: A meta‐analysis. Respirology 15(4): 643–650.
Nagpal, K., S. Sharma, C. B-Rao, S. Nahid, P.V. Niphadkar, S.K. Sharma, and B. Ghosh. 2005. TGFβ1 haplotypes and asthma in Indian populations. Journal of Allergy and Clinical Immunology 115(3): 527–533.
Yang, X.X., F.X. Li, Y.S. Wu, D. Wu, J.Y. Tan, and M. Li. 2011. Association of TGF-β1, IL-4 and IL-13 gene polymorphisms with asthma in a Chinese population. Asian Pacific Journal of Allergy and Immunology 29(3): 273–277.
Acknowledgments
The cooperation extended by the superintendent of GGCH and the principals of GMC and OMC, Hyderabad, and staff is highly acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bandaru, S., Marri, V.K., Akka, J. et al. Association of Transforming Growth Factor-Beta 1 Promoter Variant -509 C/T with Bronchial Asthma in South Indian Population. Inflammation 38, 409–414 (2015). https://doi.org/10.1007/s10753-014-0045-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-0045-5