Abstract
Risk models, informing optimal long-term medical management, seldom use natriuretic peptides (NP) in ascertaining the absolute risk of outcomes for HF patients. Individual studies evaluating the prognostic value of NPs in HF patients have reported varying effects, arriving at best estimates requires a systematic review. We systematically summarized the best evidence regarding the prognostic value of brain natriuretic peptide (BNP) and NT-proBNP in predicting mortality and hospitalizations in ambulatory heart failure (HF) patients. We searched bibliographic databases from 2005 to 2018 and included studies evaluating the association of BNP or NT-proBNP with mortality or hospitalization using multivariable Cox proportional hazard models. We pooled hazard ratios using random-effect models, explored heterogeneity using pre-specified subgroup analyses, and evaluated the certainty of evidence using the Grading of Recommendations and Development Evaluation framework. We identified 67 eligible studies reporting on 76,178 ambulatory HF patients with a median BNP of 407 pg/mL (261–574 pg/mL). Moderate to high-quality evidence showed that a 100-pg/mL increase in BNP was associated with a 14% increased hazard of mortality (HR 1.14, 95% CI 1.06–1.22); a 1-log-unit increase was associated with a 51% increased hazard of mortality (HR 1.51, 95% CI 1.41–1.61) and 48% increased hazard of mortality or hospitalization (HR 1.48, 95% CI 1.29–1.69). With moderate to high certainty, we observed a 14% independent relative increase in mortality, translating to a clinically meaningful increase in absolute risk even for low-risk patients. The observed associations may help in developing more accurate risk models that incorporate NPs and accurately prognosticate HF patients.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The prevalence of heart failure (HF) continues to rise with over 26 million people suffering from the disease worldwide [1]. By the year 2030, the anticipated prevalence of HF in the United States (US) will increase by 46% to more than 8 million adults, and the total direct medical costs of congestive HF total over $60 billion [1]. Improving prognostic assessment of HF patients may help optimize clinical management and reduce hospitalizations and mortality.
Circulating natriuretic peptide (NP) levels are useful biomarkers for detecting the presence of HF and monitoring its severity [2]. Brain natriuretic peptide (BNP) and amino-terminal (NT)-proBNP provide compensatory effects such as diuresis and inhibition of the renin–angiotensin–aldosterone system in response to increased fluid status in patients with mild HF. However, patients with chronic HF often become insensitive to the effects of NPs, resulting in a wide range of observed plasma NP levels [3].
Although BNP and NT-proBNP are well-established in international guidelines for acute HF settings, their role in the chronic setting is unclear [2, 4]. Studies evaluating NPs in relation to chronic HF prognosis and associated outcomes vary significantly in their methods of NP reporting, as well as their overall effect estimates, making interpretation and application of NP results challenging [2]. As a result, the current American College of Cardiology (ACC)/American Heart Association (AHA) and European Society of Cardiology guidelines remain without clearly defined recommendations for the use of NP levels to predict the risk of HF hospitalizations or mortality [2, 4]. To clarify the utility of NPs in predicting mortality and hospitalizations in ambulatory patients with HF, we performed a systematic review and meta-analysis.
Methods
Data sources and searches
In October 2018, with the assistance of an experienced librarian, a systematic search of bibliographic databases was conducted using terms related to HF, mortality, admission, and prognosis (Supplemental Material 1). We searched Embase, MEDLINE, Cochrane Central Register for RCTs, Cochrane database for systematic reviews, and PubMed databases for citations published since 2005. The year 2005 was chosen as a threshold because the predictive utility of NPs may differ in remote versus contemporary cohorts of patients treated with guideline-recommended HF therapies. Ethics approval was not required for this study as it includes publicly available data.
Study selection and data abstraction
The review included ambulatory adult (≥ 18 years) patients with reduced or preserved ejection fraction HF that evaluated the association of BNP or NT-proBNP with mortality and/or hospitalization using multivariable Cox proportional hazard models and reported hazard ratios (HR) and their respective 95% confidence intervals (CI). Supplemental Material 2 provides further details of the study selection and data abstraction processes.
Risk of bias and certainty assessment
We used the six domain Quality in Prognostic Studies (QUIPS) instrument to assess the risk of bias of individual studies [5]. To evaluate certainty in the evidence we used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach [6], Supplemental Material 2 provides further details of the QUIPS instrument and the GRADE approach.
Data synthesis and statistical analysis
When required, NP levels and associated HR and 95% CI were converted to units of 100 pg/mL. Using an established formula [7], the NT-proBNP values reported were converted to BNP values. A subgroup analysis was performed to determine if converted BNP values provided different effect estimates in comparison to directly reported BNP values, and when there was no difference, their association with outcomes was addressed in a single meta-analysis.
Separate meta-analyses were conducted for the outcomes of all-cause mortality, composite of all-cause mortality and HF hospitalization, and composite of CV mortality and CV hospitalization. Predictors measured continuously versus categorically and predictors evaluated in log units versus those in natural units were meta-analyzed separately. A pooled HR estimate was calculated for each meta-analysis using the inverse variance method with random-effect models, considering a two-sided p-value < 0.05 statistically significant. Heterogeneity was evaluated using the I2 statistic and visual assessment of forest plots. Pre-defined subgroup analyses were performed on low risk of bias studies only. Supplemental Material 2 presents details regarding subgroup analyses. This review was prepared following the PRISMA guidelines [8].
Calculation of absolute risks
Absolute risk estimates were calculated for patients with varying levels of BNP using the calculated pooled relative risk estimates evaluating the effect of BNP (per 100-pg/mL increase) on all-cause mortality across a range of risks [9]. Baseline risks were informed by hypothetical integer scores from the MAGGIC risk prediction model [10].
Patient and public involvement
Patients were not involved in the design and conduct of this review.
Results
Study selection and characteristics
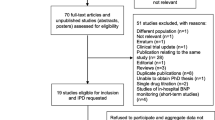
After screening 83,416 citations, 67 eligible articles reporting on 76,178 ambulatory HF patients were included (Fig. 1). Supplemental Table 1 summarizes the individual study characteristics. Included studies had median and IQRs as follows: duration of follow-up period 3.1 years (2.0–4.6 years), age 68 years (61–72 years), proportion females 28% (22–35%), LVEF 34% (30–37%), NYHA class III–IV 35% (25–50%), and BNP level of 407 pg/mL (261–574 pg/mL). The median proportion of patients using beta-blocker was 77% (59–89%), using ACEi/ARB 86% (73–93%), with implantable cardiac defibrillator 12% (6–27%) and with cardiac resynchronization therapy was 9% (5–25%).
Risk of bias of individual studies
Of the 67 studies included, we considered 21 to have a high risk of bias (Supplemental Table 2) [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. The most common reason was limitations in statistical analysis and reporting, particularly overfitting of multivariable models, building the multivariable model according to significant variables in univariable analysis, and only reporting on significant risk factors.
Association of NPs with outcomes
All-cause mortality
Sixty-five studies evaluated the association of BNP or NT-proBNP with all-cause mortality. Of these, 18 studies with 5,925 events observed evaluated BNP continuously per 100 pg/mL (10 requiring conversion from NT-proBNP), 44 studies with 16,162 events observed evaluated either BNP or NT-proBNP per 1-log unit, and 3 studies with 1,404 events observed evaluated NT-proBNP categorically for values > 3,500 pg/mL (equivalent to 1,000 pg/mL BNP).
A 100-pg/mL increase in BNP was associated with a 14% increase in hazard of all-cause mortality (HR 1.14, 95% CI 1.06–1.22; moderate certainty due to inconsistency) (Table 1, Fig. 2). High risk of bias studies underestimated the association between BNP and mortality (HR 1.00, 95% CI 1.00–1.01) when compared to low risk of bias studies (HR 1.14, 95% CI 1.06–1.22) (p-value for subgroup interaction < 0.001). There was no difference in effect estimates for converted BNP values compared to directly reported BNP values. Other subgroup analyses were not feasible due to insufficient number of low risk of bias studies.
A 1-log unit increase in NP level was associated with a 51% increase in hazard of all-cause mortality (HR 1.51, 95% CI 1.41–1.61; moderate certainty due to suspected publication bias) (Table 1, Fig. 3). The magnitude of association between NPs and mortality decreased with increasing prevalence of diabetes. To illustrate this association, in a cohort with 10% prevalence of diabetes, the hazard of all-cause mortality would increase from 1.51 to 1.65, whereas if the prevalence of diabetes were to increase to 60%, the HR would decrease to 1.28. There was no difference between studies at high versus low risk of bias. Other prespecified subgroup analyses did not change the association between NPs and all-cause mortality.
NT-proBNP > 3,500 pg/mL versus ≤ 3,500 pg/mL (equivalent BNP value of 1,000 pg/mL) was associated with a 55% increase in hazard of all-cause mortality (HR 1.55, 95% CI 1.20–1.98; high certainty) (Table 1, Supplemental Fig. 1). Publication bias and the proposed subgroup analyses were not performed due to the low number of studies.
Composite all-cause mortality and HF hospitalizations
Seven studies with 2,758 events observed evaluated the association of BNP or NT-proBNP continuously per 1-log unit with the composite of all-cause mortality and HF hospitalizations. A 1-log unit increase in NP level was associated with a 48% increase in hazard of the composite outcome (HR 1.48, 95% CI 1.29–1.69; high certainty) (Table 1, Supplemental Fig. 2). Subgroup analyses did not explain any of the observed heterogeneity and publication bias was not evaluated due to the small number of studies.
Composite cardiovascular mortality and cardiovascular hospitalizations
Five studies with 658 events observed evaluated the association of BNP with the composite of CV mortality and CV hospitalizations. A 100-pg/mL increase in BNP was not significantly associated with the composite outcome (HR 1.06, 95% CI 0.98–1.15; moderate certainty due to imprecision) (Table 1, Supplemental Fig. 3). Publication bias and subgroup analyses were not performed for this outcome due to the low number of studies.
Absolute effect of prognostic value of BNP levels
We applied the pooled relative effect estimates of BNP per 100-pg/mL increase on all-cause mortality (Fig. 2) to illustrate the corresponding absolute increases in risk across low (100 pg/mL) and high (1,500 pg/mL) levels of BNP (Table 2). We calculated baseline risks using the MAGGIC Risk Calculator, which ranges from 0 to 50 and does not incorporate the effect of BNP. For a patient with the lowest possible MAGGIC score of 0, the baseline risk of 1-year all-cause mortality is 1.5%. The absolute effect of increasing BNP for a patient with a MAGGIC score of 0 ranges from 1 to 6% from the lowest to the highest BNP values. For a patient with a MAGGIC score of 40, the baseline risk of 1-year all-cause mortality is 52%. The absolute effect of increasing BNP for a patient with a MAGGIC score of 40 ranges from 39 to 96% from the lowest to the highest BNP values.
Discussion
Main study findings
Our meta-analyses highlight the prognostic value of both BNP and NT-proBNP in the setting of adult ambulatory patients with HF. Moderate to high certainty evidence shows a 100-pg/mL increase in a population with median BNP level of 407 pg/mL is associated with a 14% increased risk of all-cause mortality, that a 1-log-unit increase is associated with a 51% increased risk of all-cause mortality and 48% increased risk of the composite all-cause mortality or HF hospitalization. Moderate to high certainty evidence also shows that NT-proBNP levels > 3,500 pg/mL compared to ≤ 3,500 pg/mL are associated with a 55% increased risk of all-cause mortality.
The estimation of impact on absolute risks demonstrates how clinicians can use these results to evaluate prognosis in ambulatory patients with HF. For patients with high estimated baseline risk of 1-year all-cause mortality based on non-NP factors, small changes in NP can have a substantial impact on overall risk. In patients whose estimated risk is low, larger changes in BNP levels will translate into smaller changes in risk that may still be clinically meaningful. These gradients could likely have an important bearing on patient management.
Relation to previous work
Current guidelines recommend the use of BNP or NT-proBNP to establish prognosis in chronic HF [32]. The current AHA statement regarding the use of BNP for prognosis is informed by the 2005 systematic review by Doust et al. [33], which summarized only four studies and found a 35% (95% CI 22–49%) increase in the relative risk of all-cause mortality per 100-pg/mL increase. The authors did not assess the quality of evidence or estimate the impact on absolute risk and included studies reporting both unadjusted and adjusted effects, introducing the possibility of overestimation of the effect of BNP. Our meta-analysis included a larger number of high-quality studies, leading to a moderate to high level of certainty in the effect of NPs on adverse outcomes.
Recent work has demonstrated the prognostic value of adding NPs to existing risk prediction models for estimating the risk of mortality in patients with HF. The addition of BNP or NT-proBNP to the MAGGIC risk score resulted in significant improvements in predicting mortality in both the ambulatory HF setting [34] and among patients admitted to hospital with HF [35, 36]. Similar improvements in prognostic performance have been observed with the addition of BNP to the Seattle HF Model (SHFM) [37, 38], and NT-proBNP to both the Get With The Guidelines HF risk score and the Intermountain Risk Score [39].
Despite consistent evidence demonstrating improved prognostic performance of risk models that include NP levels, current online risk calculators, including the MAGGIC risk score and SHFM, have not been revised to incorporate NPs for use in the clinical setting. A new risk prediction model, derived from the Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in HF (PARADIGM-HF) trial population [40] and externally validated in 2 independent cohorts, now includes NT-proBNP and is available as an online calculator [41].
Our study provides further evidence on the prognostic value of BNP, which supports its routine assessment and incorporation in risk prediction models for evaluating prognosis among ambulatory patients with HF. Our review demonstrates that NPs should be considered in the context of other clinical risk factors, as changes in NP levels have a varying effect depending on a patient’s baseline risk (considering non-NP factors).
Limitations
Our search of the literature was conducted in October 2018; therefore, it may not include more recently published studies. Given the large scope of literature evaluated in this review, we believe that the studies included in the current analyses adequately inform the pooled effect estimates reported, and it is unlikely that any additional studies published would significantly alter the conclusions from our analysis. We also combined BNP and NT-proBNP effect estimates into single meta-analyses where appropriate. This was done by either converting continuous NT-proBNP per 100 pg/mL into BNP units, or by combining BNP and NT-proBNP when reported in log units. We did this to utilize as much available evidence to inform our meta-analyses and subgroup analysis of studies reporting converted BNP values and directly reported BNP values that did not demonstrate any difference in association with all-cause mortality.
Despite observing some heterogeneity in our analyses, subgroup analyses according to patient BMI, eGFR, and proportion of patients with AF, which are factors known to influence measures of BNP, were not feasible as these data were too infrequently reported. Additionally, we did not perform subgroup analysis according to proportion of patients on sacubitril/valsartan due to this data not being available in most studies. However, results from the PARADIGM-HF trial have shown consistent prognostic importance of NP values in patients with HF with reduced ejection fraction treated with sacubitril/valsartan. The authors demonstrated that, despite significant reduction, NP levels during follow-up were significantly associated with cardiovascular mortality or first hospitalization for HF in adjusted models.
One of the challenges in testing the association between NP levels and outcomes is related to its exponential increase. Assuming a linear association when in fact there is an exponential increase could lead to the overestimation of predicted risk for each unit change in predictor. In the case of BNP and NT-proBNP, logarithmic transformations are applied to allow for such analyses to be performed. However, these effect estimates cannot easily be applied into a clinical setting. An alternative is to report the effect of NP levels categorically; however, this reduces the granularity to assess their association with a given outcome. For example, NT-proBNP levels > 3,500 pg/mL versus ≤ 3,500 pg/mL were associated with a 55% increase in the risk of all-cause mortality. This creates uncertainty on how different the risk could be in a patient with a NT-proBNP level of 1,000 pg/mL in comparison to a patient with a level of 100 pg/mL.
Implications in clinical practice and research
The findings from our review support the use of either BNP or NT-proBNP when assessing prognosis and stratifying risk in patients with HF. Current guidelines, however, remain without any specific thresholds or instructions to use these biomarker levels for clinical management or for delineating patient risk. This can be attributed in part due to the heterogeneity in current RCTs that aim to discern clinical benefit for NP guided therapy compared to standard of care. Future trials may need to evaluate targeting BNP levels based on their impact on overall prognosis and not just simply a value.
Our results also support the incorporation of NP values into HF risk prediction models. Current risk models for predicting 1-year mortality in ambulatory HF patients do not typically include NP measures (HF Meta-Score [42], Seattle HF Model [43], MAGGIC score [10], 3C-HF [44]), and those that do (BCN Bio-HF [45]) only include them as optional variables. The addition of NPs to existing risk prediction models has demonstrated increased discrimination and calibration of these multivariable models to predict adverse HF outcomes [26, 38]. Incorporation of BNP or NT-proBNP into current and future risk scores may provide the most accurate interpretation of NPs for risk assessment in the context of known factors associated with HF outcomes and factors associated with increased levels of NPs (e.g., age, sex, LVEF, diabetes, obesity, and renal dysfunction).
Conclusion
With moderate to high certainty in the evidence, this systematic review and meta-analysis highlight the prognostic value of both BNP and NT-proBNP in the setting of adult ambulatory patients with HF. We also provide measures of absolute risk to aid physicians in applying these findings to the clinical context to better inform patient management, facilitate patient communication, and perform shared decision-making.
Availability of data and material
All data used in this study is published in the supplementary files provided and widely available.
References
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S (2019) Heart Disease and Stroke Statistics-2019 update: a report from the American Heart Association. Circulation 139(10):e56–e528. https://doi.org/10.1161/CIR.0000000000000659
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America. J Card Fail 23(8):628–651. https://doi.org/10.1016/j.cardfail.2017.04.014
Tanase DM, Radu S, Al Shurbaji S, Baroi GL, Florida Costea C, Turliuc MD, Ouatu A, Floria M (2019) Natriuretic peptides in heart failure with preserved left ventricular ejection fraction: from molecular evidences to clinical implications. Int J Mol Sci 20(11). https://doi.org/10.3390/ijms20112629
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology F, American Heart Association Task Force on Practice G (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16):e147-239. https://doi.org/10.1016/j.jacc.2013.05.019
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
Foroutan F, Guyatt G, Zuk V, Vandvik PO, Alba AC, Mustafa R, Vernooij R, Arevalo-Rodriguez I, Munn Z, Roshanov P, Riley R, Schandelmaier S, Kuijpers T, Siemieniuk R, Canelo-Aybar C, Schunemann H, Iorio A. Grade Guidelines 28: Use of Grade for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol. 2020 May;121:62-70. https://doi.org/10.1016/j.jclinepi.2019.12.023. Epub 2020 Jan 23. PMID: 31982539.
Masson S, Vago T, Baldi G, Salio M, De Angelis N, Nicolis E, Maggioni AP, Latini R, Norbiato G, Bevilacqua M (2002) Comparative measurement of N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in ambulatory patients with heart failure. Clin Chem Lab Med 40(8):761–763. https://doi.org/10.1515/CCLM.2002.130
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Foroutan F, Iorio A, Thabane L, Guyatt G (2019) Calculation of absolute risk for important outcomes in patients with and without a prognostic factor of interest. J Clin Epidemiol 117:46–51. https://doi.org/10.1016/j.jclinepi.2019.08.012
Pocock SJ, Ariti CA, McMurray JJ, Maggioni A, Kober L, Squire IB, Swedberg K, Dobson J, Poppe KK, Whalley GA, Doughty RN, Meta-Analysis Global Group in Chronic Heart F (2013) Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J 34(19):1404–1413. https://doi.org/10.1093/eurheartj/ehs337
Adlbrecht C, Hulsmann M, Neuhold S, Strunk G, Pacher R (2013) Prognostic utility of the Seattle Heart Failure Score and amino terminal pro B-type natriuretic peptide in varying stages of systolic heart failure. J Heart Lung Transplant 32(5):533–538. https://doi.org/10.1016/j.healun.2013.01.1048
Al-Najjar Y, Goode KM, Zhang J, Cleland JG, Clark AL (2009) Red cell distribution width: an inexpensive and powerful prognostic marker in heart failure. Eur J Heart Fail 11(12):1155–1162. https://doi.org/10.1093/eurjhf/hfp147
Berin R, Zafrir B, Salman N, Amir O (2014) Single measurement of serum N-terminal pro-brain natriuretic peptide: the best predictor of long-term mortality in patients with chronic systolic heart failure. Eur J Intern Med 25(5):458–462. https://doi.org/10.1016/j.ejim.2014.04.001
Boule S, Semichon M, Guedon-Moreau L, Drumez E, Kouakam C, Marquie C, Brigadeau F, Kacet S, Potelle C, Escande W, Souissi Z, Lacroix D, Duhamel A, Klug D (2016) Long-term outcome of implantable cardioverter-defibrillator implantation in secondary prevention of sudden cardiac death. Arch Cardiovasc Dis 109(10):517–526. https://doi.org/10.1016/j.acvd.2016.02.008
Burkard T, Pfister O, Rickli H, Follath F, Hack D, Zaker R, Pittl U, Handschin R, Pfisterer M, Brunner-La Rocca HP, Time CHFI (2014) Prognostic impact of systemic inflammatory diseases in elderly patients with congestive heart failure. QJM 107(2):131–138. https://doi.org/10.1093/qjmed/hct205
Cauthen CA, Tong W, Jain A, Tang WH (2012) Progressive rise in red cell distribution width is associated with disease progression in ambulatory patients with chronic heart failure. J Card Fail 18(2):146–152. https://doi.org/10.1016/j.cardfail.2011.10.013
Chan MM, Santhanakrishnan R, Chong JP, Chen Z, Tai BC, Liew OW, Ng TP, Ling LH, Sim D, Leong KT, Yeo PS, Ong HY, Jaufeerally F, Wong RC, Chai P, Low AF, Richards AM, Lam CS (2016) Growth differentiation factor 15 in heart failure with preserved vs. reduced ejection fraction. Eur J Heart Fail 18(1):81–88. https://doi.org/10.1002/ejhf.431
Charach G, Argov O, Nochomovitz H, Rogowski O, Charach L, Grosskopf I (2018) A longitudinal 20 years of follow up showed a decrease in the survival of heart failure patients who maintained low LDL cholesterol levels. QJM 111(5):319–325. https://doi.org/10.1093/qjmed/hcy043
Corell P, Gustafsson F, Kistorp C, Madsen LH, Schou M, Hildebrandt P (2007) Effect of atrial fibrillation on plasma NT-proBNP in chronic heart failure. Int J Cardiol 117(3):395–402. https://doi.org/10.1016/j.ijcard.2006.03.084
Damy T, Ghio S, Rigby AS, Hittinger L, Jacobs S, Leyva F, Delgado JF, Daubert JC, Gras D, Tavazzi L, Cleland JG (2013) Interplay between right ventricular function and cardiac resynchronization therapy: an analysis of the CARE-HF trial (cardiac resynchronization-heart failure). J Am Coll Cardiol 61(21):2153–2160. https://doi.org/10.1016/j.jacc.2013.02.049
Damy T, Goode KM, Kallvikbacka-Bennett A, Lewinter C, Hobkirk J, Nikitin NP, Dubois-Rande JL, Hittinger L, Clark AL, Cleland JG (2010) Determinants and prognostic value of pulmonary arterial pressure in patients with chronic heart failure. Eur Heart J 31(18):2280–2290. https://doi.org/10.1093/eurheartj/ehq245
Ingle L, Cleland JG, Clark AL (2014) The long-term prognostic significance of 6-minute walk test distance in patients with chronic heart failure. Biomed Res Int 2014:505969. https://doi.org/10.1155/2014/505969
Jankowska EA, Rozentryt P, Witkowska A, Nowak J, Hartmann O, Ponikowska B, Borodulin-Nadzieja L, Banasiak W, Polonski L, Filippatos G, McMurray JJ, Anker SD, Ponikowski P (2010) Iron deficiency: an ominous sign in patients with systolic chronic heart failure. Eur Heart J 31(15):1872–1880. https://doi.org/10.1093/eurheartj/ehq158
Jankowska EA, Biel B, Majda J, Szklarska A, Lopuszanska M, Medras M, Anker SD, Banasiak W, Poole-Wilson PA, Ponikowski P (2006) Anabolic deficiency in men with chronic heart failure: prevalence and detrimental impact on survival. Circulation 114(17):1829–1837. https://doi.org/10.1161/CIRCULATIONAHA.106.649426
Johansson P, Brostrom A, Dahlstrom U, Alehagen U (2008) Global perceived health and ten-year cardiovascular mortality in elderly primary care patients with possible heart failure. Eur J Heart Fail 10(10):1040–1047. https://doi.org/10.1016/j.ejheart.2008.07.003
Ky B, French B, Levy WC, Sweitzer NK, Fang JC, Wu AH, Goldberg LR, Jessup M, Cappola TP (2012) Multiple biomarkers for risk prediction in chronic heart failure. Circ Heart Fail 5(2):183–190. https://doi.org/10.1161/CIRCHEARTFAILURE.111.965020
Lanfear DE, Gibbs JJ, Li J, She R, Petucci C, Culver JA, Tang WHW, Pinto YM, Williams LK, Sabbah HN, Gardell SJ (2017) Targeted metabolomic profiling of plasma and survival in heart failure patients. JACC Heart Fail 5(11):823–832. https://doi.org/10.1016/j.jchf.2017.07.009
Latini R, Gullestad L, Masson S, Nymo SH, Ueland T, Cuccovillo I, Vardal M, Bottazzi B, Mantovani A, Lucci D, Masuda N, Sudo Y, Wikstrand J, Tognoni G, Aukrust P, Tavazzi L, Investigators of the Controlled Rosuvastatin Multinational Trial in Heart F, trials GI-HF (2012) Pentraxin-3 in chronic heart failure: the CORONA and GISSI-HF trials. Eur J Heart Fail 14(9):992–999. https://doi.org/10.1093/eurjhf/hfs092
Maeder MT, Rickli H, Pfisterer ME, Muzzarelli S, Ammann P, Fehr T, Hack D, Weilenmann D, Dieterle T, Kiencke S, Estlinbaum W, Brunner-La Rocca HP, Investigators TC (2012) Incidence, clinical predictors, and prognostic impact of worsening renal function in elderly patients with chronic heart failure on intensive medical therapy. Am Heart J 163 (3):407–414, 414 e401. https://doi.org/10.1016/j.ahj.2011.12.003
Poelzl G, Altenberger J, Pacher R, Ebner CH, Wieser M, Winter A, Fruhwald F, Dornaus C, Ehmsen U, Reiter S, Steinacher R, Huelsmann M, Eder V, Boehmer A, Pilgersdorfer L, Ablasser K, Keroe D, Groebner H, Auer J, Jakl G, Hallas A, Ess M, Ulmer H, Austrian Working Group on Heart F (2014) Dose matters! Optimisation of guideline adherence is associated with lower mortality in stable patients with chronic heart failure. Int J Cardiol 175(1):83–89. https://doi.org/10.1016/j.ijcard.2014.04.255
Ushigome R, Sakata Y, Nochioka K, Miyata S, Miura M, Tadaki S, Yamauchi T, Sato K, Onose T, Tsuji K, Abe R, Oikawa T, Kasahara S, Takahashi J, Shimokawa H, Investigators C (2015) Temporal trends in clinical characteristics, management and prognosis of patients with symptomatic heart failure in Japan – report from the CHART Studies. Circ J 79(11):2396–2407. https://doi.org/10.1253/circj.CJ-15-0514
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Rev Esp Cardiol (Engl Ed) 69(12):1167. https://doi.org/10.1016/j.rec.2016.11.005
Doust JA, Pietrzak E, Dobson A, Glasziou P (2005) How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ 330(7492):625. https://doi.org/10.1136/bmj.330.7492.625
Michaels A, Aurora L, Peterson E, Liu B, Pinto YM, Sabbah HN, Williams K, Lanfear DE (2020) Risk prediction in transition: MAGGIC score performance at discharge and incremental utility of natriuretic peptides. J Card Fail 26(1):52–60. https://doi.org/10.1016/j.cardfail.2019.11.016
Khanam SS, Choi E, Son JW, Lee JW, Youn YJ, Yoon J, Lee SH, Kim JY, Ahn SG, Ahn MS, Kang SM, Baek SH, Jeon ES, Kim JJ, Cho MC, Chae SC, Oh BH, Choi DJ, Yoo BS (2018) Validation of the MAGGIC (Meta-Analysis Global Group in Chronic Heart Failure) heart failure risk score and the effect of adding natriuretic peptide for predicting mortality after discharge in hospitalized patients with heart failure. PLoS ONE 13(11):e0206380. https://doi.org/10.1371/journal.pone.0206380
Sawano M, Shiraishi Y, Kohsaka S, Nagai T, Goda A, Mizuno A, Sujino Y, Nagatomo Y, Kohno T, Anzai T, Fukuda K, Yoshikawa T (2018) Performance of the MAGGIC heart failure risk score and its modification with the addition of discharge natriuretic peptides. ESC Heart Fail 5(4):610–619. https://doi.org/10.1002/ehf2.12278
AbouEzzeddine OF, French B, Mirzoyev SA, Jaffe AS, Levy WC, Fang JC, Sweitzer NK, Cappola TP, Redfield MM (2016) From statistical significance to clinical relevance: a simple algorithm to integrate brain natriuretic peptide and the Seattle Heart Failure Model for risk stratification in heart failure. J Heart Lung Transplant 35(6):714–721. https://doi.org/10.1016/j.healun.2016.01.016
May HT, Horne BD, Levy WC, Kfoury AG, Rasmusson KD, Linker DT, Mozaffarian D, Anderson JL, Renlund DG (2007) Validation of the Seattle Heart Failure Model in a community-based heart failure population and enhancement by adding B-type natriuretic peptide. Am J Cardiol 100(4):697–700. https://doi.org/10.1016/j.amjcard.2007.03.083
Boralkar KA, Kobayashi Y, Moneghetti KJ, Pargaonkar VS, Tuzovic M, Krishnan G, Wheeler MT, Banerjee D, Kuznetsova T, Horne BD, Knowlton KU, Heidenreich PA, Haddad F (2019) Improving risk stratification in heart failure with preserved ejection fraction by combining two validated risk scores. Open Heart 6(1):e000961. https://doi.org/10.1136/openhrt-2018-000961
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, Investigators P-H, Committees, (2014) Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371(11):993–1004. https://doi.org/10.1056/NEJMoa1409077
Simpson J, Jhund PS, Lund LH, Padmanabhan S, Claggett BL, Shen L, Petrie MC, Abraham WT, Desai AS, Dickstein K, Kober L, Packer M, Rouleau JL, Mueller-Velten G, Solomon SD, Swedberg K, Zile MR, McMurray JJV (2020) Prognostic models derived in PARADIGM-HF and validated in ATMOSPHERE and the Swedish Heart Failure Registry to predict mortality and morbidity in chronic heart failure. JAMA Cardiol 5(4):432–441. https://doi.org/10.1001/jamacardio.2019.5850
Alba AC, Walter SD, Guyatt GH, Levy WC, Fang J, Ross HJ, Lee DS (2018) Predicting survival in patients with heart failure with an implantable cardioverter defibrillator: the heart failure meta-score. J Card Fail 24(11):735–745. https://doi.org/10.1016/j.cardfail.2017.11.002
Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, Anand I, Maggioni A, Burton P, Sullivan MD, Pitt B, Poole-Wilson PA, Mann DL, Packer M (2006) The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 113(11):1424–1433. https://doi.org/10.1161/CIRCULATIONAHA.105.584102
Senni M, Parrella P, De Maria R, Cottini C, Bohm M, Ponikowski P, Filippatos G, Tribouilloy C, Di Lenarda A, Oliva F, Pulignano G, Cicoira M, Nodari S, Porcu M, Cioffi G, Gabrielli D, Parodi O, Ferrazzi P, Gavazzi A (2013) Predicting heart failure outcome from cardiac and comorbid conditions: the 3C-HF score. Int J Cardiol 163(2):206–211. https://doi.org/10.1016/j.ijcard.2011.10.071
Lupon J, de Antonio M, Vila J, Penafiel J, Galan A, Zamora E, Urrutia A, Bayes-Genis A (2014) Development of a novel heart failure risk tool: the barcelona bio-heart failure risk calculator (BCN bio-HF calculator). PLoS ONE 9(1):e85466. https://doi.org/10.1371/journal.pone.0085466
Acknowledgements
The authors would like to acknowledge Yu Tong Lu, Kimberly Lau, Helen Liu, Madeleine Stein, Kathleen O’Brien, Alanna Rigobon, Derrick Chang, Alessia Borgo, and Nigar Sekercioglu for their contributions to the data collection process for this systematic review.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
TAB, CC, FF, HJR, GG, and ACA conceived the study idea. TT wrote the first draft of the manuscript. AOC designed the search strategy. TAB, CC, FF, AM, JFD, NNFH, RS, and NE screened the abstracts and full texts, acquired the data, and judged the risk of bias in the studies. TAB performed the data analysis. TAB is the guarantor. All authors interpreted the data analysis and critically revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was not required for this study as it includes publicly available data.
Consent for publication
No human subjects were involved in the study. Consent for publication was not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Buchan, T.A., Ching, C., Foroutan, F. et al. Prognostic value of natriuretic peptides in heart failure: systematic review and meta-analysis. Heart Fail Rev 27, 645–654 (2022). https://doi.org/10.1007/s10741-021-10136-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10136-3