Abstract
A novel pump, the left atrial assist device (LAAD), is a device specifically for the treatment of heart failure with preserved ejection fraction (HFpEF). The LAAD is a mixed-flow pump that is implanted in the mitral position and delivers blood from the left atrium to the left ventricle. During the development process, we aimed to explore whether device activation in torque control (TC) mode would improve the function of the LAAD. The TC mode causes adjustment of the pump speed automatically during each cardiac cycle in order to maintain a specified torque. In this study, we tested four different TC settings (TC modes 0.9, 1.0, 1.25, and 1.5) using an in vitro mock circulatory loop. Mild, moderate, and severe diastolic heart failure (DHF) conditions, as well as normal heart condition, were simulated with the four TC modes. Also, we evaluated the LAAD in vivo with three calves. The LAAD was implanted at the mitral position with four TC settings (TC modes 0.9, 1.0, 1.1, 1.2). With LAAD support, the in vitro cardiac output and aortic pressure recovered to normal heart levels at TC 1.25 and 1.5 even under severe DHF conditions with little pump regurgitation. The TC mode tested in vivo with three calves, and it also showed favorable result without elevating the left ventricular end-diastolic pressure. These initial in vitro and in vivo results suggest that the TC mode could be potentially effective, and the LAAD could be a treatment option for HFpEF patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “heart failure (HF) with preserved ejection fraction (EF)” (HFpEF) was introduced in the late 1990s/early 2000s to describe diastolic heart failure (DHF). Today, HFpEF refers to patients who have typical symptoms of HF, such as exertional dyspnea or exercise intolerance and fluid retention, but the left ventricular (LV) EF is within the normal range (widely over 40%) without other significant valvular abnormalities [1, 2].
The more the concept of HFpEF has been recognized worldwide, the more we have learned its features; in brief, the percentage of HFpEF in all cases of HF is more than 50% and still increasing [3], and the mortality rate and reduction in quality of life are as pronounced as the natural course of HF with reduced EF (HFrEF) [4, 5]. Importantly, although various pharmacological therapies have attempted to improve the outcome of HFpEF [6,7,8,9,10,11,12], there have been no effective clinical therapies established. Diastolic dysfunction or DHF is not synonymous with HFpEF, but is a large, important subset carrying typical characteristics of HFpEF [13].
Within this context, device-based therapies that are tailored for HFpEF features are attracting attention, and several mechanical cardiac support devices have also been developed in the preclinical phase [14]. The typical HFpEF features are progressive decrease of LV relaxation and left atrial (LA) compliance, followed by higher LA pressure (LAP) and pulmonary capillary wedge pressure (PCWP), especially while exercising.
A left atrial assist device (LAAD) is our latest device for treatment of HFpEF [15]. The main idea behind this device is to reduce LAP while keeping physiological antegrade blood flow and flow pulsatility. In this study, we aimed to evaluate our new control algorithm, the torque control (TC) mode into the in vitro and in vivo experiments, and to assess each parameter of circulation and pulsatility with the LAAD TC mode under various DHF conditions.
Methods
LAAD pump
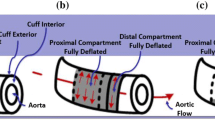
A working prototype of the LAAD (Fig. 1a–c) was developed for implantation in the mitral position (Fig. 1d). It is a mixed-flow pump directing blood from the LA to fill the LV from its position at the mitral valve level [15,16,17]. The diameter and height are both 33.5 mm, and the pump utilizes a hydrodynamic bearing for radial support of the rotating assembly and a magnetic, passive bearing to limit its axial movement.
Mock circulation loop static condition
Before the in vitro testing of the LAAD TC mode, the pressure-flow curves of the pump were obtained with a static mock loop at several pump speed settings (from 3000 to 6000 rpm) as a reference. The pressure was measured just before the LAAD (pin) and just after the LAAD (pout). The arterial resistance was changed manually in several steps to produce a range of LAAD delta pressure (pout–pin) conditions.
Mock circulation loop dynamic condition of nh and DHF
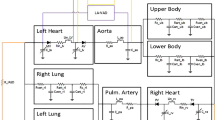
The in vitro mock circulatory loop consisted of a pneumatic mock ventricle (AB5000, ABIOMED Inc., Danvers, MA), a pneumatic driver, an adjustable arterial afterload and compliance, LA reservoir, and the LAAD (Fig. 2a). The pneumatic mock ventricle simulated a native LV, and the LAAD was placed between the LA chamber and the mock ventricle (Fig. 2a, b). The inlet valve of the mock ventricle was fixed open by the insertion of a short plastic tube to simulate the removal of the mitral valve after LAAD implantation. A mixture of water and glycerin with a specific gravity of 1.060 was used as the working fluid to simulate blood.
The heart rate of the mock ventricle was set at 80 bpm, the systolic duration was kept at 250 ms, and the pneumatic systolic driving pressure was set at 200 mm Hg (it should be noted that AB5000 pneumatic driving pressures are not the same as the pressures that are generated by the system in the flow path.). To simulate three different levels of DHF, the diastolic filling of the pneumatic ventricle was restricted by increasing the diastolic drive pressures of the pneumatic driver from −35 mm Hg at NH condition to 0 mm Hg (mild DHF), + 20 mm Hg (moderate DHF), and + 40 mm Hg (severe DHF).
The LAAD was operated at four different TC mode settings (described below), and cardiac output (CO) was measured with a flow probe (ME20PXL; Transonic Systems Inc., Ithaca, NY). The aortic pressure (AoP) and the LAP (or pin) were recorded with fluid-filled monitoring lines, pressure transducers (13-6615-50; Gould Electronics, Chandler, AZ), and amplifiers (M21018; Honeywell, Charlotte, NC). All data sets collected for this study were recorded once the loop was at steady state at a sampling rate of 1000 Hz using a PowerLab data acquisition system (ADInstruments Inc., Colorado Springs, CO) and analyzed using LabChart Pro v8.1.9 (ADInstruments Inc., Colorado Springs, CO).
TC mode on dynamic test conditions
In TC mode, the controller strives to maintain a commanded torque value. TC is used in other motor control applications; for instance, in electric vehicles, and the pump speed under TC mode, was set automatically in response to the load on the motor. We set four TC settings of 0.7, 0.8, 0.9, and 1.0 (amps torque equivalent), and for each setting, the NH condition and mild-to-severe DHF conditions were tested with a fixed arterial resistance. The pump speed, pump power, pump flow, and hemodynamics at each TC setting were recorded.
In vivo study
The in vivo study was approved by the Cleveland Clinic’s Institutional Animal Care and Use Committee (#2018–2004). A total of three male Jersey calves (mean body weight: 81.1 ± 3.1 kg) underwent the LAAD implantation with TC control mode testing. Under general anesthesia with a right lateral position, a left thoracotomy was performed on the 4th intercostal space. CO was measured with a 28-mm flow probe (28PAU113, 28PAX307; Transonic Systems Inc., Ithaca, NY) that was placed around the main pulmonary artery, and a fluid-filled LAP line was inserted in the LA. A fluid-filled (n = 1) or a micro-manometer Millar catheter (n = 2) was inserted into the LV from the LV free wall.
As for cardiopulmonary bypass, an arterial cannula was placed in the left carotid artery and a venous cannula in the right ventricle through the main pulmonary artery. After full heparinization (5 mg/kg), cardiopulmonary bypass was started. The LA was opened after aortic cross-clamping with cardioplegia. The LAAD was implanted at the mitral annulus after the mitral leaflets were resected.
After de-clamping the aorta, the LAAD was started, and cardiopulmonary bypass was gradually weaned and then stopped as the LAAD speed or torque was increased enough to keep the circulation. After confirming stable conditions, the hemodynamic, pump speed, and pump power were taken with four TC settings of pump speeds of 0.9, 1.0, 1.1, and 1.2. After recording all the data points, the animal was sacrificed with an intravenous bolus injection of Beuthanasia (75 mg/kg).
Results
The static pressure-flow curves of the LAAD at each speed are shown in Fig. 3, and the dynamic head curves of each TC mode are illustrated in Fig. 4 (with the static data as a reference). In TC mode, the dynamic head curves followed lower pump speed during diastole and higher pump speed during systole; thus, the slopes were steeper than the speed control mode. There were regurgitant flows up to −3 L/min at the TC settings of 0.9 and 1.0 during systole, but at TC 1.25 and 1.5, almost no regurgitation was observed.
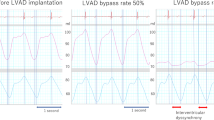
Figure 5 shows the wave forms of the flow (CO), AoP, pump speed, and pump power at TC modes 0.9, 1.0, 1.25, and 1.5, respectively, as well as the CO and AoP data without LAAD. As is consistent with our previous report [17], the AoP, CO, and pulsatility decreased with increasing DHF severity without LAAD support (Fig. 5a).
The waveforms of the hemodynamic parameters (cardiac output and aortic pressure), pump speed, and pump power under each DHF condition obtained from mock loop circulation. a Waveform of each DHF setting without LAAD, b TC mode 0.9, c TC mode 1.0, d TC mode 1.25, e TC mode 1.5. The diastolic drive pressures of the pneumatic ventricle to each setting are the following: 200/−40 mm HG (normal heart), 200/0 mm Hg (mild DHF), 200/20 mm Hg (moderate DHF), and 200/40 mm Hg (severe DHF)
With LAAD support, the AoP and the CO were maintained within the physiological range, and the pulsatility in the AoP was maintained without decreasing throughout all of the conditions of DHF, for all LAAD support modes (Fig. 5b–e). The peak AoP showed slight decreases in TC modes 0.9–1.25, but the magnitude decrease was much less than without the LAAD, and the decrease was also mitigated as the TC mode support increased. In TC mode 1.5, the level of peak AoP was almost the same as the NH condition regardless of the DHF conditions (Fig. 5e). The pump speed increased during systole, and the power showed a consistent trend with the pump speed. Nevertheless, the pump flows were still lower during systole due to higher delta pressure at low flow.
Summarized in vitro graphs of mean AoP, mean CO, mean LAP, pump power, and pump speed with each TC mode setting are illustrated in Fig. 6. The mean AoP without LAAD showed a large difference when compared with the other DHF settings, but with increased TC mode support, the difference was diminished. At CT 1.25 and 1.5, even under severe DHF mode, the mean AoP was maintained at a higher level than the NH condition without LAAD. The mean CO showed the same trend as the mean AoP (Fig. 6b), corresponding with the changes in mean pump power (Fig. 6d) and pump speed (Fig. 6e). The mean LAP showed an inverse trend to the AoP and CO (Fig. 6c).
The results of the in vivo study are illustrated in Fig. 7. Since all of the calves used in this experiment have healthy hearts without any diastolic dysfunction, the effect of the LAAD on mean AoP and mean CO was not obvious (Fig. 7a, b). However, the pump showed reducing reduction in LAP (Fig. 7c). The LV end-diastole pressure did not elevate as the torque increased and stayed almost the same in normal range (Fig. 7d). The changes in mean pump power (Fig. 7e) and pump speed (Fig. 7f) showed almost the same trend as in vitro testing.
Discussion
The LAAD is a device designed to relieve the symptoms of HFpEF by pumping blood from the LA directly to the LV. It especially targets DHF with diastolic dysfunction, in consideration of most HFpEF patients. For HFpEF patients, continuous ventricular unloading with rotary blood pumps might potentially cause severe suction events around the inflow cannula due to the smaller ventricular dimensions and reduced end-systolic and end-diastolic volumes [18, 19], and there are far fewer reports of LVAD implantation in HFpEF patients than in HF-with-reduced-EF patients.
There are other unique attempts to develop a novel device tailored to relief the HFpEF pathology and/or symptoms, and we summarized them here by their approaching points on HFpEF pathologies.
Approaching to LA: to reduce high LAP/large LA
To decrease LAP by reducing LA volume is one of the essential points for HFpEF patient since a large LA was reported to correlate with a higher risk of hospitalization [20], and LA size was independently associated with the morbidity and mortality of HFpEF patients [11]. There are currently three ways to directly mitigate high LAP: interatrial shunting, LA-to-coronary sinus (CS) shunting, and LA blood drainage with a mechanical support.
As for the interatrial shunting, there are three percutaneous devices available so far: Interatrial Shunt Device (IASD II, Corvia Medical Inc., Tewksbury, MA) [21,22,23], V-wave device (V-wave, Caesarea, Israel) [24,25,26], and atrial flow regulator (AFR) (Occlutech, Istanbul, Turkey) [27, 28]. As its name suggests, an interatrial shunt is percutaneously placed at the interatrial septum making a hole, and it reliefs the LAP by creating a left-to-right shunt. The IASD is the most progressed device among the three, and a randomized and double-blinded phase II study has been done with 6-month/1-year results [23]. The IASD showed a high level of safety, as well as the other interatrial shunt devices. However, there is an interesting tendency; effects of the IASD to reduce PCWP or hospitalization rate were the best at 3–6-month period and then failed to improve the 1-year outcomes. This may be because the hemodynamic change in a heart induced by a left-to-right shunt is a palliative relief of high LAP and symptom, but not a physiological one, which does not directly benefit the HFpEF pathology itself. The LA-to-CS shunting, Transcatheter Atrial Shunt System (Edwards Life sciences, Irvine, CA), would introduce the similar hemodynamic changes to interatrial shunting, but technically, it requires more complicated catheter techniques during the procedure [29].
As for the usage of mechanical circulatory supports with LA cannulation, there are four possible devices: HeartWare HVAD (Medtronic, Minneapolis, MN) with an LA cannulation [30], Synergy System (Medtronic, Minneapolis, MN) [18], PulseVAD (Northern Development, Strandhaugen, Oslo), and VADovations cardiac assist system (VADovations, Oklahoma City, OK). The HeartWare HVAD is one of the representative left ventricular assist devices (LVADs), but the LA cannulation technique for HVAD is a relatively new method with limited reports. Most of the reports were congenital heart disease cases with relatively small body size patients [31], but one case report was recently published with a hypertrophic cardiomyopathy patient case [30]. The LA of HFpEF patients is typically enlarged, and LA cannulation would be more favorable because it would reduce the risk of suction event than LV cannulation. However, all of these four devices induce a non-physiological blood flow from the LA to the aorta, and this configuration has a concern of blood stagnation inside the LV. To maintain the opening of the aortic valve under this configuration, careful adjustment of the pump flow should be taken to keep the valve opening.
Approaching to LV: to enlarge LV relaxation/LV volume
Another approach to improve the LV filling is to increase the LV relaxation or to add the LV volume. There are two devises directly approach the LV: a LV expander and a valveless pulsatile pump with a single cannula to LV. As for the LV expander, the CORolla Assist Device (CorAssist Inc., Haifa, Israel) is currently the only option [32]. This is a self-expandable device attached to the endocardium and enhancing LV diastolic expansion from the inside. The efficacy and safety of this device in 10 HFpEF patients are now being tested with an open-label trial (NCT02499601) and have not been fully documented yet.
The only example of adding LV volume to the LV is the CoPulse, a valveless pulsatile pump with a single cannula connected to the LV apex [33, 34]. This pump can add around 30 mL to each LV stroke volume with the pump chamber and create pulsatile flow synchronized with the LV cardiac cycle by using the LV pressure as a signal. This device showed good results with hemodynamic effectiveness and comparable hemocompatibility to previous pumps by in vitro [34] and ex vivo [33] studies, but further in vivo studies are required before a human use. Also, although this pump drains blood synchronously only while the mitral valve is open, as far as the cannula position is at the thick LV wall of HFpEF patients, there is a concern of sucking risk.
Notably, both of these two approaching methods are combined and used in the LAAD’s strategy. The active filling of the LV by encouraging diastolic flow from the LA directly to the LV is the concept of the LAAD. This is a unique point, as no other device exists to pump blood to the LV, possibly leading to remodeling and recovery of LV function. To confirm this, chronic in vivo experiments with DHF animal models, the methodology of which has not yet been produced, are needed.
One concern of the LAAD is the pump regurgitation during systolic phases. The LAAD, like other continuous-flow rotary pumps, does not generate pulsation unless its speed is modulated. However, the flow created at the same speed can be changed by the phase of each cardiac cycle, because continuous-flow rotary pumps, represented by LVADs, operate in conjunction with the native ventricles. Under typical mechanical cardiac support with continuous-flow LVADs, the delta pressure between the aortic and LV pressure affects the pump flow.
This means that, during diastole, the pump flow is less than systole because the delta pressure is higher between the aortic and LV pressures in diastole and the pump needs more speed to generate the same forward flow [35, 36]. This phenomenon does not interfere with the pulsatility in the LVAD setting because the lowered flow by the interaction occurs only in the diastolic phase.
For the LAAD, however, the higher delta pressure between the LA and the LV in the systolic phase can be a critical issue, because the LAAD must overcome with higher pump speed in the systolic phase; otherwise, backflow through the pump would occur if the pump speed is not high enough. Therefore, we have explored some ways to prevent backflow or regurgitation through the pump.
One idea is to preserve the mitral valve by implanting the pump at the supra-valvular level. Our previous in vitro experiment showed that the mitral valve was closed during systole with the low pump speed, and the total flow was slightly improved with the mitral valve avoiding the regurgitant flow [17]. This was an in vitro simulation study, so it will be necessary to confirm the possibility of this configuration through in vivo experiments.
The TC mode, which we have used in this in vitro and in vivo study, is another possible way to prevent the backflow, by automatically making the pump speed higher in systole and lower in diastole. This was our first attempt, since our previous LAAD simulation studies were reported with speed control mode [15,16,17], which is similar to other LVADs or continuous-flow devices. With TC modes, the dynamic head curves have successfully become steeper, decreasing pump speed during diastole and increasing during systole. By striving to maintain a certain torque, this adjustment was achieved automatically and constantly, showing better pulsatility even under a severe DHF condition. Less backflow was observed in TC mode, and hemodynamic benefits were confirmed.
This is our first report of in vitro and in vivo experiments using the TC mode of the LAAD, and there are some limitations. First, as for the in vitro simulation study using a mock circulation loop and a pneumatically driven mock ventricle, and it may not adequately simulate dynamic LV diastolic dysfunction because the diastolic drive pressure of the pneumatic ventricle was constant during each of the three DHF configurations.
Second, there are concerns with elevated LV end-diastolic pressure that could negatively affect coronary blood flow. The latter was not a focus of the current effort, but this type of interaction could be tested in a suitable model. The mock loop LV chamber is not able to increase its maximal volume toward the higher preload, so response to the high-end-diastolic pressure could be different from in vivo data. Even with the in vivo study, the calves have totally normal heart, which did not show any feature of diastolic dysfunction. Therefore, it is still possible that the LV end-diastolic pressure could become too high to maintain coronary flow in HFpEF hearts with impaired LV relaxation. Developing the bilateral ventricular mock loop with higher fidelity mock ventricles, designed for modeling HFpEF, is required, as well as further in vivo studies using large animals with HFpEF features for both short and long experimental periods. Additionally, the described model did not specifically assess the LA contractility, which in its turn could have selective effects on the LAAD performance.
Conclusion
This initial in vitro and in vivo studies with the TC mode of the LAAD showed positive results for our hypothesis that the TC mode allows for adequate adjustment of pump speed during each simulated cardiac cycle by maintaining the torque automatically and continuously. Under in vitro DHF conditions, TC mode performs within intended design requirements, but further in vitro and in vivo studies are required to evaluate the physiological effect of the LAAD on HFpEF patients in more detail.
References
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16):e147-239. https://doi.org/10.1016/j.jacc.2013.05.019
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 esc guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the esc. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Lam CSP, Voors AA, de Boer RA, Solomon SD, van Veldhuisen DJ (2018) Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J 39(30):2780–2792. https://doi.org/10.1093/eurheartj/ehy301
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, Gong Y, Liu PP (2006) Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 355(3):260–269. https://doi.org/10.1056/NEJMoa051530
Lewis EF, Lamas GA, O’Meara E, Granger CB, Dunlap ME, McKelvie RS, Probstfield JL, Young JB, Michelson EL, Halling K, Carlsson J, Olofsson B, McMurray JJ, Yusuf S, Swedberg K, Pfeffer MA (2007) Characterization of health-related quality of life in heart failure patients with preserved versus low ejection fraction in charm. Eur J Heart Fail 9(1):83–91. https://doi.org/10.1016/j.ejheart.2006.10.012
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR (2014) Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371(11):993–1004. https://doi.org/10.1056/NEJMoa1409077
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Harty B, Heitner JF, Kenwood CT, Lewis EF, O’Meara E, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, Yang S, McKinlay SM (2014) Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 370(15):1383–1392. https://doi.org/10.1056/NEJMoa1313731
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Düngen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VC, Lefkowitz MP (2019) Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620. https://doi.org/10.1056/NEJMoa1908655
Tanaka H, Hirata KI (2018) Potential impact of sglt2 inhibitors on left ventricular diastolic function in patients with diabetes mellitus. Heart Fail Rev 23(3):439–444. https://doi.org/10.1007/s10741-018-9668-1
Tanaka H, Soga F, Tatsumi K, Mochizuki Y, Sano H, Toki H, Matsumoto K, Shite J, Takaoka H, Doi T, Hirata KI (2020) Positive effect of dapagliflozin on left ventricular longitudinal function for type 2 diabetic mellitus patients with chronic heart failure. Cardiovasc Diabetol 19(1):6. https://doi.org/10.1186/s12933-019-0985-z
Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE (2011) Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation 124(23):2491–2501. https://doi.org/10.1161/circulationaha.110.011031
Bonsu KO, Arunmanakul P, Chaiyakunapruk N (2018) Pharmacological treatments for heart failure with preserved ejection fraction-a systematic review and indirect comparison. Heart Fail Rev 23(2):147–156. https://doi.org/10.1007/s10741-018-9679-y
Persson H, Lonn E, Edner M, Baruch L, Lang CC, Morton JJ, Ostergren J, McKelvie RS (2007) Diastolic dysfunction in heart failure with preserved systolic function: need for objective evidence: results from the charm echocardiographic substudy-charmes. J Am Coll Cardiol 49(6):687–694. https://doi.org/10.1016/j.jacc.2006.08.062
Miyagi C, Miyamoto T, Karimov JH, Starling RC, Fukamachi K (2021) Device-based treatment options for heart failure with preserved ejection fraction. Heart Fail Rev. https://doi.org/10.1007/s10741-020-10067-5
Fukamachi K, Horvath DJ, Karimov JH, Kado Y, Miyamoto T, Kuban BD, Starling RC (2020) Left atrial assist device to treat patients with heart failure with preserved ejection fraction: initial in vitro study. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2019.12.110
Kado Y, Polakowski AR, Kuban BD, Horvath DJ, Miyamoto T, Karimov JH, Starling RC, Fukamachi K (2020) The effects of preserving mitral valve function on a left atrial assist device: an in vitro mock circulation loop study. Asaio j. https://doi.org/10.1097/mat.0000000000001257
Kado Y, Polakowski AR, Kuban BD, Horvath DJ, Miyamoto T, Karimov JH, Starling RC, Fukamachi K (2020) Left atrial assist device function at various heart rates using a mock circulation loop. Int J Artif Organs:391398820977508. https://doi.org/10.1177/0391398820977508
Burkhoff D, Maurer MS, Joseph SM, Rogers JG, Birati EY, Rame JE, Shah SJ (2015) Left atrial decompression pump for severe heart failure with preserved ejection fraction: theoretical and clinical considerations. JACC Heart Fail 3(4):275–282. https://doi.org/10.1016/j.jchf.2014.10.011
Moscato F, Wirrmann C, Granegger M, Eskandary F, Zimpfer D, Schima H (2013) Use of continuous flow ventricular assist devices in patients with heart failure and a normal ejection fraction: a computer-simulation study. J Thorac Cardiovasc Surg 145(5):1352–1358. https://doi.org/10.1016/j.jtcvs.2012.06.057
Issa O, Peguero JG, Podesta C, Diaz D, De La Cruz J, Pirela D, Brenes JC (2017) Left atrial size and heart failure hospitalization in patients with diastolic dysfunction and preserved ejection fraction. J Cardiovasc Echogr 27(1):1–6. https://doi.org/10.4103/2211-4122.199064
Kaye DM, Petrie MC, McKenzie S, Hasenfuβ G, Malek F, Post M, Doughty RN, Trochu JN, Gustafsson F, Lang I, Kolodziej A, Westenfeld R, Penicka M, Rosenberg M, Hausleiter J, Raake P, Jondeau G, Bergmann MW, Spelman T, Aytug H, Ponikowski P, Hayward C (2019) Impact of an interatrial shunt device on survival and heart failure hospitalization in patients with preserved ejection fraction. ESC Heart Fail 6(1):62–69. https://doi.org/10.1002/ehf2.12350
Kaye DM, Nanayakkara S (2019) Interatrial shunt device for heart failure with preserved ejection fraction. Front Cardiovasc Med 6:143. https://doi.org/10.3389/fcvm.2019.00143
Shah SJ, Feldman T, Ricciardi MJ, Kahwash R, Lilly S, Litwin S, Nielsen CD, van der Harst P, Hoendermis E, Penicka M, Bartunek J, Fail PS, Kaye DM, Walton A, Petrie MC, Walker N, Basuray A, Yakubov S, Hummel SL, Chetcuti S, Forde-McLean R, Herrmann HC, Burkhoff D, Massaro JM, Cleland JGF, Mauri L (2018) One-year safety and clinical outcomes of a transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction in the reduce elevated left atrial pressure in patients with heart failure (REDUCE LAP-HF I) trial: a randomized clinical trial. JAMA Cardiol 3(10):968–977. https://doi.org/10.1001/jamacardio.2018.2936
Rodés-Cabau J, Bernier M, Amat-Santos IJ, Ben Gal T, Nombela-Franco L, García Del Blanco B, Kerner A, Bergeron S, Del Trigo M, Pibarot P, Shkurovich S, Eigler N, Abraham WT (2018) Interatrial shunting for heart failure: early and late results from the first-in-human experience with the v-wave system. JACC Cardiovasc Interv 11(22):2300–2310. https://doi.org/10.1016/j.jcin.2018.07.001
Guimarães L, Bergeron S, Bernier M, Rodriguez-Gabella T, Del Val D, Pibarot P, Eigler N, Abraham WT, Rodés-Cabau J (2020) Interatrial shunt with the second-generation v-wave system for patients with advanced chronic heart failure. EuroIntervention 15(16):1426–1428. https://doi.org/10.4244/eij-d-19-00291
Guimaraes L, Del Val D, Bergeron S, O’Connor K, Bernier M, Rodés-Cabau J (2020) Interatrial shunting for treating acute and chronic left heart failure. Eur Cardiol 15:e18. https://doi.org/10.15420/ecr.2019.04
Rajeshkumar R, Pavithran S, Sivakumar K, Vettukattil JJ (2017) Atrial septostomy with a predefined diameter using a novel Occlutech atrial flow regulator improves symptoms and cardiac index in patients with severe pulmonary arterial hypertension. Catheter Cardiovasc Interv 90(7):1145–1153. https://doi.org/10.1002/ccd.27233
Patel MB, Samuel BP, Girgis RE, Parlmer MA, Vettukattil JJ (2015) Implantable atrial flow regulator for severe, irreversible pulmonary arterial hypertension. EuroIntervention 11(6):706–709. https://doi.org/10.4244/eijy15m07_08
Simard T, Labinaz M, Zahr F, Nazer B, Gray W, Hermiller J, Chaudhry SP, Guimaraes L, Philippon F, Eckman P, Rodés-Cabau J, Sorajja P, Hibbert B (2020) Percutaneous atriotomy for levoatrial-to-coronary sinus shunting in symptomatic heart failure: first-in-human experience. JACC Cardiovasc Interv 13(10):1236–1247. https://doi.org/10.1016/j.jcin.2020.02.022
Kiamanesh O, Rankin K, Billia F, Badiwala MV (2020) Left ventricular assist device with a left atrial inflow cannula for hypertrophic cardiomyopathy. JACC: Case Reports 2 (13):2090–2094. https://doi.org/10.1016/j.jaccas.2020.10.006
Ma M, Yarlagadda VV, Rosenthal DN, Maeda K (2017) A novel inflow cannulation strategy for pediatric mechanical circulatory support in small left ventricles. J Thorac Cardiovasc Surg 154(3):e47–e48. https://doi.org/10.1016/j.jtcvs.2017.03.034
Burlacu A, Simion P, Nistor I, Covic A, Tinica G (2019) Novel percutaneous interventional therapies in heart failure with preserved ejection fraction: an integrative review. Heart Fail Rev 24(5):793–803. https://doi.org/10.1007/s10741-019-09787-0
Escher A, Choi Y, Callaghan F, Thamsen B, Kertzscher U, Schweiger M, Hübler M, Granegger M (2020) A valveless pulsatile pump for heart failure with preserved ejection fraction: hemo- and fluid dynamic feasibility. Ann Biomed Eng 48(6):1821–1836. https://doi.org/10.1007/s10439-020-02492-2
Granegger M, Dave H, Knirsch W, Thamsen B, Schweiger M, Hübler M (2019) A valveless pulsatile pump for the treatment of heart failure with preserved ejection fraction: a simulation study. Cardiovasc Eng Technol 10(1):69–79. https://doi.org/10.1007/s13239-018-00398-8
Tang PC, Pagani FD (2018) Continuous-flow device engineering and pump technology. Cardiol Clin 36(4):451–463. https://doi.org/10.1016/j.ccl.2018.06.001
Hosseinipour M, Gupta R, Bonnell M, Elahinia M (2017) Rotary mechanical circulatory support systems. J Rehabil Assist Technol Eng 4:2055668317725994. https://doi.org/10.1177/2055668317725994
Acknowledgements
We would like to show our greatest appreciation to David J. Horvath for helpful discussions and advice on this manuscript.
Funding
This study was supported by funding from the National Heart, Lung, and Blood Institute; National Institutes of Health (NIH); NIH Center for Accelerated Innovation at Cleveland Clinic (NCAI-CC); and (NIH-NHLBI 1UH54HL119810; NCAI-19–12-APP-CCF) (PI: Kuban).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kiyotaka Fukamachi, Jamshid H. Karimov, and Randall C. Starling are co-inventors of the LAAD. The other coauthors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyagi, C., Kuban, B.D., Flick, C.R. et al. Left atrial assist device for heart failure with preserved ejection fraction: initial results with torque control mode in diastolic heart failure model. Heart Fail Rev 28, 287–296 (2023). https://doi.org/10.1007/s10741-021-10117-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10117-6