Abstract
Frailty is a common geriatric syndrome of increased vulnerability to adverse events. The prevalence of frailty among chronic heart failure (CHF) is high and confers a greater risk of adverse events including falls, hospitalisation and mortality. There have been few studies assessing frailty in CHF. A review of the key databases was conducted from 2004 to 2014 including the key search terms ‘frail elderly’ and ‘heart failure’. The following electronic databases were searched: Medline, Cumulative Index for Nursing and Allied Health and Academic Search Complete, with reference lists being manually searched. Articles were included if frailty was assessed using a valid measuring tool in a population with a confirmed diagnosis of CHF. The search yielded a total of 393 articles with 8 articles being selected for review. The prevalence of frailty among those with CHF was high, ranging from 18 to 54 %. The frailty phenotype and geriatric assessments tools were the most common frailty measures utilised; high rates of co-morbidity, hospitalisation and mortality were identified. Frailty is common in CHF and is associated with adverse outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a common geriatric syndrome associated with loss of functionality leading to an increased vulnerability to adverse health events [1]. As frailty identifies a reduced physiological reserve across multiple systems, it helps rationalise the considerable heterogeneity that exists within the older population. The strong association of frailty with adverse events—such as increased risk of falls, hospitalisation, institutionalisation, disability and mortality [1–4]—has increased the call for frailty screening implementation into routine clinical practice for risk stratification. Frailty screening not only objectively identifies this vulnerable population, but may also assist in estimating disease prognosis and in the judicious allocation of management strategies. However, despite the prognostic and therapeutic implications, frailty is still not routinely clinically assessed [5]. A recent consensus did, however, indicate that all persons >70 years of age with a more than 5 % weight loss due to a chronic disease should be screened [6].
Multiple large-cohort studies have identified that frail patients with cardiovascular disease (CVD) have an increased risk of morbidity and mortality, above that of the general older population [7–9]. A recent systematic review identified a relationship between both conditions, with the prevalence of frailty being twofold to threefold higher in older individuals with CVD [9]. For chronic cardiovascular syndromes, such as chronic heart failure (CHF), frailty is being increasingly identified as an area of co-morbid concern. The impact of concurrent frailty and CHF is evident, given that the prevalence of CHF increases sixfold to sevenfold with increasing frailty severity [1, 3]. The elucidation of common pathological processes spanning immunological, metabolic and autonomic systems indicates a multifaceted and complex association between the two syndromes. Over the last two decades there has been increasing literature assessing the relationship between frailty and CHF. The purpose of this article is to provide a systematic review of publications that have assessed frailty in CHF, focusing on how frailty is measured, its prevalence and the impact of frailty on morbidity and mortality.
Methods
Literature search
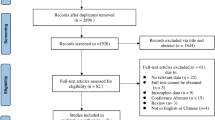
The following electronic databases were searched: Medline, Cumulative Index for Nursing and Allied Health (CINAHL) and Academic Search Complete from 2004 to 2014. The MeSH terms included ‘frail elderly’ and ‘heart failure’. Studies were included if: (1) frailty was assessed using systematically defined criteria, (2) the population had CHF with a confirmed diagnosis using reliable and validated methods, (3) used human subjects and (4) were published in English.
Results
Study selection
The search yielded a total of 393 citations which met the search criteria (Fig. 1). Of these citations two reviewers (S.R.J., H.S.K.H) excluded 365 studies, with 28 being selected for consideration based on information in the abstract. Following full-text review, a further 20 studies were excluded due to not meeting the inclusion criteria. As a result, a total of 8 articles were included in this review and are summarised in Table 1. Data extraction identified the following themes outlined below.
Frailty in chronic heart failure
Defining and measuring frailty
Due to the lack of a standardised definition and multiplicity of measures used to quantify frailty, there exists a difficulty in effectively comparing multiple studies. To date there are no validated frailty measures for clinical use within a CHF population, which presents a future challenge for further research. General commonalities do, however, exist across most frailty definitions, including aspects of muscle wastage, and subsequent physical weakness and inactivity, cognitive impairment and exhaustion. The most common definitions that have been used to determine frailty within a CHF population were the frailty phenotype (FP) [1] and a comprehensive geriatric evaluation (CGA) [10, 11] (Table 1).
Frailty phenotype
The FP [1] was developed and validated by Fried and colleagues in the Cardiovascular Health Study (CHS) and describes a patient as frail when three or more attributes are present from five specific measures: unintentional weight loss, exhaustion, slow walking speed, weakness and low physical activity. If two attributes are present, the patient is pre-frail, and less than two denotes no frailty. Due to its underlying physiological base and easy to measure elements, the FP is the most commonly implemented diagnostic criteria in research to date; however, the appropriateness of this measure within a CHF population is unclear. Given that CHF patients commonly suffer with fluid retention and are consequently on medications such as diuretics for fluid management, Fried’s variable of unintentional weight loss is difficult to quantify and is potentially masked in this population. There are also several common disease states among CHF patients that result in unintentional weight loss and further contribute to the difficulty in accurately measuring this variable [12]. Cardiac cachexia, a syndrome commonly present within the terminal stages of CHF, has not only been shown to strongly impact on disease prognosis but also results in significant muscle wastage, weight loss and weakness in cachectic CHF patients. Alternative frailty measures, such as the SHARE-FI, which have been adapted from the FP, potentially provide a suitable alternative measure of frailty in CHF patients, as the variable of unintentional weight loss has been substituted with reduced appetite. The SHARE-FI, however, has yet to be validated in CHF. Also, given the complex nature of frailty, studies are increasingly adapting the FP—which only assesses the physical deficits of frailty—to encompass both the physical and psychosocial domains.
Geriatric assessment
The second most common frailty measure used within a CHF population was a comprehensive geriatric assessment (CGA). This more holistic approach involved the inclusion of four validated geriatric tools to assess domains of functional autonomy, cognitive deterioration, emotional disturbances and social risk [10, 11]. These four validated geriatric scales were the Barthel index (<90), OARs scale (<10 in females and <6 in males), Pfeiffer test (>3 (±1, depending on educational grade)) and the short-form depression scale (and ≥1 positive response), with one abnormal result across the tools denoting frailty. This method, however, was likely to have identified aspects of disability, as well as frailty.
Prevalence
The prevalence of frailty varies depending on the population studied, study setting and the measure used to quantify frailty severity; most studies have reported a high prevalence of frailty among patients with heart failure. Across the identified articles, there was substantial variance in prevalence ranging from 18 to 54 % (Table 1). In the Cardiovascular Health Study (CHS) [1], where 5317 community-dwelling individuals were assessed for frailty using the FP, a prevalence of 6.7 % was identified. The CHS was also one of the first studies to elucidate the relationship between frailty and CHF, with frailty incurring a more than sevenfold increase in CHF prevalence (frail vs. non-frail OR 7.51; 95 % CI 4.66–12.12). In subsequent studies of community-dwelling CHF individuals, where frailty was determined using the FP, the prevalence ranged from 21 to 27 % [13–15]. While in the studies assessing frailty using the CGA the prevalence was observed as being higher, ranging from 40 to 42 % [10, 11].
Across the studies, there is a significant association of increasing frailty severity with advancing age and being female. In the study by Altimir et al. [10], in which 360 CHF outpatients were assessed for sex and age differences, frailty was identified as being significantly higher in those aged ≥70 years old (53.3 vs. 33.3 %, ρ = 0.001) and in females (62.6 vs. 33.7 %, ρ = 0.001). This trend was also identified in the follow-up study by Lupon et al. [11], in which 622 CHF outpatients were subsequently assessed. Although frailty and CHF are largely considered geriatric syndromes, frailty is not an inevitable part of ageing. In fact not all older individuals become frail, and there are also a significant proportion of younger frail people. In the two aforementioned studies, where age was stratified into younger (<70 years old) and older (>70 years old) age groups, a high proportion of ‘younger’ CHF patients were also identified as being frail.
Morbidity and mortality
In a study by McNallan et al. [16], the majority (60 %) of community-dwelling CHF individuals had a Charlson co-morbidity index of ≥3, with frailty severity significantly associated with an increasing disease burden. Despite the fact that most CHF patients have a high degree of co-morbidity and frailty, this population is underrepresented in RCTs [17]. Consequently, the lack of data creates limited evidence for best practice management in this vulnerable population. Furthermore, even though it is well documented that frailty increases the risk of hospitalisation in the general older population, there has been little-to-no evidence reported within a CHF population. Pulignano et al.’s study [18] was the only identified study assessing frailty in an outpatient CHF population which reported hospitalisation data; frail individuals were identified as having a significantly higher rate of hospitalisation (20.5 vs. 13.3 %; P = 0.01).
There have been a limited number of studies assessing the impact of frailty on mortality within a CHF population. From the studies that have been identified, frailty was associated with an increasing risk of mortality [11, 16, 18, 19]. Cacciatore et al. [19] assessed the predictive role of frailty in long-term (12 years) mortality in patients with (n = 120) and without CHF (n = 1139). In this study, frailty was independently associated with increasing mortality risk in both the CHF (HR 1.48; 95 % CI 1.04–2.11; ρ = 0.032) and non-CHF populations (HR 1.36; 95 % CI 1.17–1.57; ρ < 0.001), with frailty being a stronger predictor of mortality in those with CHF. During the 12-year follow-up period, 0 % of the CHF patients with severe frailty (stage 3) survived past 9 years, compared with 45 % with mild frailty (stage 1). Similar results were identified in the study by Lupon et al. [11] of 622 CHF outpatients, where frailty was an independent predictor of 1-year mortality, even after adjustment for known CHF correlates (HR 2.09; 95 % CI 1.11–3.92; ρ = 0.022). When the data from this study were categorised into older (≥70 years old) and younger (<70 years old) age groups, a high mortality was observed across both groups. Interestingly, however, the predictive ability of frailty was more distinct in the younger group (12.5 vs. 3.3 %; ρ = 0.001) rather than in the older group (19.8 vs. 7.5 %; ρ = 0.003); suggesting the role of frailty screening for early detection of younger frail CHF patients. The last study to assess mortality by McNallan et al. [16] of 223 community-dwelling CHF individuals also identified a twofold increase in mortality, while adjusting for sex, age and left-ventricular ejection fraction (HR 2.04 (95 % CI 0.99–4.18); ρ = 0.05), while intermediate frailty conferred no significantly increased risk.
Discussion
Frailty identifies a state of vulnerability and is associated with a poor prognosis. The major finding of this review is that CHF patients who are frail are more likely to experience higher rates of morbidity and mortality. This finding is consistent with the proposition that frail CHF patients have an increased susceptibility to stressful events such that even minor stressors are more likely to be associated with clinical worsening and the need for hospitalisation. The association between frailty and adverse outcomes in CHF patients is further strengthened by the high rate of co-morbidity particularly in elderly CHF patients [17]. Frail CHF patients also experience greater disability and more rapid progression to death than non-frail CHF patients. This vulnerability to stressful events is being proposed to explain the considerable heterogeneity in health outcomes across both the older and younger CHF populations.
As frailty screening provides an ideal means of identifying those who are ‘biologically aged’ as opposed to ‘chronologically aged’, the use of frailty as a risk stratification tool has been gaining increased attention. This is particularly important as chronological age alone is not reflective of health status, as the association between age and health can be extremely variable [20]. The implication of frailty screening in clinical practice not only objectively identifies this vulnerable population, but may also assist in estimating disease prognosis and in the judicious allocation of disease management strategies. The objective identification of frail patients is essential as many healthcare workers intuitively make decisions regarding patient care based on their apparent ‘robustness’—mainly as a precaution against iatrogenesis [21]; but as many patients who appear robust are actually frail, this ‘end-of-the-bed’ clinical impression may not always be accurate. This is becoming increasingly important as the ageing population and more effective treatments for hypertension and ischaemic heart disease, including acute myocardial infarction, are resulting in a highly co-morbid older CHF population; with many of these ‘high-risk’ CHF patients then being referred for further treatments. With the increasing advent of advanced device therapy interventions—for instance mechanical circulatory support (MSC) and transcatheter aortic valve replacements (TAVR)—there is an urgent need for improved patient screening selection for these high-cost and potentially highly morbid procedures. Indeed, as the chronological age of patients referred for cardiac surgery has been increasing steadily, there has been a movement towards the implementation of frailty screening to assess cardiosurgical operative risk as current surgical risk stratification tools inadequately reflect a patient’s ‘biological’ age [22].
While there was a significant variance in frailty prevalence among the identified studies, it was also noted that when frailty was assessed using the CGA methods, as opposed to the FP method, the prevalence range was identified as higher. As the CGA is a set of validated geriatric tools, it is likely to have identified elements of disability as well as frailty, two distinct, yet causally related, clinical entities. There are two discourses of thought regarding the differentiation of frailty and disability: one in which frailty is the preceding and dynamic step prior to disability, a perception more typical of the phenotypic approach [23], which is in contention with the idea that, given the considerable overlap between frailty and disability, elements of disability should be included within frailty measures to more accurately position a patient’s level of frailty severity [24]. It is likely that those individuals who were identified as having mild frailty as determined by a graded CGA method were still captured as ‘pre-frail’ using the phenotypic tool, thus resulting in the overestimation using the CGA. Nevertheless, the lack of a consensual definition, results in either the overestimation of prevalence using the CGA method or the underestimation using the FP. Only further highlighting the need for a unanimous and agreed upon frailty measure. In a similar systematic review of frailty among community-dwelling older persons [25], despite the substantial variance in prevalence, there was a statistically significant difference in sex, with more females than males presenting as frail (female 9.6, 95 % CI 9.2–10.0 %; males 5.2, 95 % CI 4.9–5.5 %) [17]. These trends were also identified in this review with higher frailty prevalence with being female. In a CHF population, female patients more typically present as HFpEF with advanced age and a high co-morbidity burden. The additive threat of frailty in this particular group of patients incurs an increased risk of non-cardiac-related morbidity and mortality such as falls, leading to recurrent rehospitalisation [3].
The considerable overlap that exists between frailty and CHF—with each syndrome increasing the incidence and prevalence of the other [26]—is likely due to commonalities in shared pathophysiological development. Although research in determining the biological correlates of frailty is still emerging, there have been several established biomarkers. Frail patients are more likely to be vitamin D deficient and have higher interleukin-6 levels, tumour necrosis factor α (TNFα), clotting factors (i.e. factor VIII) and an increased C-reactive protein (CRP) sensitivity [27–29]. Due to the increased number of systemically circulating inflammatory markers, frailty has been described as pro-inflammatory state. A recent analysis of the Women’s Health and Ageing Studies I and II [30] also identified that the probability of being frail increased with the number of concomitant inflammatory-related diseases. In the above-mentioned study, the combination of CVD and depression was the second most widespread disease pattern identified, helping to further elucidate a clinical profile of the highly co-morbid frail patient. Furthermore, frailty and depression have been shown to have significant prognostic impacts on 1-year mortality and hospitalisations in CHF patients [11].
CHF, like frailty, is a systemic syndrome. Pro-inflammatory cytokines have also been well established as contributing to the development, adverse prognosis and progression of CHF. High levels of inflammatory markers in CHF patients—such as IL-6, CRP and TNFα—have been associated with skeletal muscle loss, cardiac cachexia and declining physical function [31], which in turn manifest as weakness, sarcopenia and physical dependence, symptoms that are common to the frailty syndrome. There is still, however, a considerable amount unknown about the mechanistic links between frailty and CHF. In the HABC study [26] frailty severity was associated with increasing inflammatory markers, glycaemia and adiposity. When adjusted for these variables, however, the association between frailty severity and the risk of developing incident heart failure was only mildly attenuated, suggesting that there are undiscovered variables influential in the association between frailty and CHF.
As frailty is considered a dynamic syndrome, presenting as a continuum from robust health to severe frailty, there is the potential for an important ‘interventional window’. Unlike CHF, where management is aimed at slowing or halting disease progression, interventional strategies for frailty can potentially result in syndrome reversal—a unique feature of any progressive and geriatric condition. Clinically, the implications for frailty screening among CHF patients allow for the optimal allocation of intervention resources to those most likely to benefit. In a study by Pulignano et al. [18], where 173 older CHF patients were randomised to either usual care or a multidisciplinary management, the mild-to-moderately frail patients experienced a significantly reduced risk of hospitalisation and mortality. Opportunely, this mild-to-moderate group is the predominate cohort among most CHF populations, allowing for the possibility of high impact interventions. The reversibility of frailty within the CHF population presents as a complex area for further research as it raises many yet unaddressed questions. It is still unknown why some patients, irrespective of age and heart failure severity, become frail and why frailty either improves or worsens in patients after the advent of advanced treatment options such as MCS or TAVR. Particularly in patients with end-stage disease, the logic behind the reversibility of frailty may come down to the pathological processes behind the different types of frailty; namely the proportion of cardiac cachexia to age related/co-morbidity induced frailty in these patients; however, further research is necessary to start answering these questions.
The frailty consensus [6] identified four key therapeutic interventions as appropriate for physical frailty: physical exercise, nutritional intervention, vitamin D supplementation and polypharmacy reduction. Physical exercise interventions improve muscle strength and physical ability, with translatable recovery in frailty-associated sarcopenia and weakness. Exercise-based CHF interventions have also been identified as improving the myocardial aerobic capacity, muscle strength, while reducing all-cause and HF-related hospitalisations [32]. Nutritional supplements, particularly with protein-enrich derivatives, is not only a therapeutic intervention for frailty, but also a core therapeutic component for cachectic CHF patients. This is particularly important as sarcopenia is a hallmark of cardiac cachexia and is a key aspect in the development of frailty. Intervention strategies that manage aspects of sarcopenia—like those stated in the consensus—have the potential to profoundly impact the clinical trajectory of a frail patient with CHF. Although best practice guidelines for the management of frailty have been published [33], these are based on recommendations for frail community-dwelling individuals and outpatient populations, which as highlighted in this review are different to those with concomitant CHF. The existence of these generalised—yet non-disease-specific guidelines—underlines the increasing recognition of frailty as a significant contributor to worse outcomes. Yet, as there are no established guidelines for the management of frailty in patients with advanced heart failure, recommendations need to be made, which lead the incorporation of frailty into to current care models of heart failure.
Conclusion
Frailty is common in patients with CHF. The increased recognition of the cardiogeriatric factors in CHF underscores the importance of assessing and managing frailty. Achieving consensus on measurement and modes of assessment can increase the capacity to prevent, identify and manage frailty.
References
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci 56(3):M146–M157
Rockwood K, Howlett SE, MacKnight C, Beattie BL, Bergman H, Hébert R et al (2004) Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol Ser A Biol Sci Med Sci 59(12):1310–1317
Woods NF, LaCroix AZ, Gray SL, Aragaki A, Cochrane BB, Brunner RL et al (2005) Frailty: emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study (WHI-OS). J Am Geriatr Soc 53(8):1321–1330
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381(9868):752–762
Lacas A, Rockwood K (2012) Frailty in primary care: a review of its conceptualization and implications for practice. BMC Med 10(1):4
Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabei R et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397
Newman AB, Gottdiener JS, McBurnie MA, Hirsch CH, Kop WJ, Tracy R et al (2001) Associations of subclinical cardiovascular disease with frailty. J Gerontol Ser A Biol Sci Med Sci 56(3):M158–M166
Purser JL, Kuchibhatla MN, Fillenbaum GG, Harding T, Peterson ED, Alexander KP (2006) Identifying frailty in hospitalized older adults with significant coronary artery disease. J Am Geriatr Soc 54(11):1674–1681
Afilalo J, Karunananthan S, Eisenberg MJ, Alexander KP, Bergman H (2009) Role of frailty in patients with cardiovascular disease. Am J Cardiol 103(11):1616–1621
Altimir S, Lupon J, Gonzalez B, Prats M, Parajon T, Urrutia A et al (2005) Sex and age differences in fragility in a heart failure population. Eur J Heart Fail 7(5):798–802
Lupon J, Gonzalez B, Santaeugenia S, Altimir S, Urrutia A, Mas D et al (2008) Prognostic implication of frailty and depressive symptoms in an outpatient population with heart failure. Rev Esp Cardiol 61(8):835–842
Morley JE, Thomas DR, Wilson MM (2006) Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr 83(4):735–743
Boxer R, Kleppinger A, Ahmad A, Annis K, Hager D, Kenny A (2010) The 6-minute walk is associated with frailty and predicts mortality in older adults with heart failure. Congest Heart Fail 16(5):208–213
Boxer RS, Wang Z, Walsh SJ, Hager D, Kenny AM (2008) The utility of the 6-minute walk test as a measure of frailty in older adults with heart failure. Am J Geriatr Cardiol 17(1):7–12
McNallan SM, Singh M, Chamberlain AM, Kane RL, Dunlay SM, Redfield MM et al (2013) Frailty and healthcare utilization among patients with heart failure in the community. J Am Coll Cardiol Heart Fail 1(2):135–141
McNallan SM, Chamberlain AM, Gerber Y, Singh M, Kane RL, Weston SA et al (2013) Measuring frailty in heart failure: a community perspective. Am Heart J 166(4):768–774
Murad K, Kitzman DW (2012) Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management. Heart Fail Rev 17(4–5):581–588
Pulignano G, Del Sindaco D, Di Lenarda A, Tarantini L, Cioffi G, Gregori D et al (2010) Usefulness of frailty profile for targeting older heart failure patients in disease management programs: a cost-effectiveness, pilot study. J Cardiovasc Med 11(10):739–747
Cacciatore F, Abete P, Mazzella F, Viati L, Della Morte D, D’Ambrosio D et al (2005) Frailty predicts long-term mortality in elderly subjects with chronic heart failure. Eur J Clin Investig 35(12):723–730
Lloyd-Sherlock P, McKee M, Ebrahim S, Gorman M, Greengross S, Prince M et al (2012) Population ageing and health. Lancet 379(9823):1295–1296
Mitty E (2010) Iatrogenesis, frailty, and geriatric syndromes. Geriatr Nurs 31(5):368–374
Afilalo J, Mottillo S, Eisenberg MJ, Alexander KP, Noiseux N, Perrault LP et al (2012) Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circ Cardiovasc Qual Outcomes 5(2):222–228
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G (2004) Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Ser A Biol Sci Med Sci 59(3):M255–M263
Theou O, Rockwood MRH, Mitnitski A, Rockwood K (2012) Disability and co-morbidity in relation to frailty: how much do they overlap? Arch Gerontol Geriatr 55(2):e1–e8
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60(8):1487–1492
Khan H, Kalogeropoulos AP, Georgiopoulou VV, Newman AB, Harris TB, Rodondi N et al (2013) Frailty and risk for heart failure in older adults: the health, aging, and body composition study. Am Heart J 166(5):887–894
Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH et al (2002) Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med 162(20):2333–2341
Boxer RS, Dauser DA, Walsh SJ, Hager WD, Kenny AM (2008) The association between vitamin D and inflammation with the 6-minute walk and frailty in patients with heart failure. J Am Geriatr Soc 56(3):454–461
Phan HM, Alpert JS, Fain M (2008) Frailty, inflammation, and cardiovascular disease: evidence of a connection. Am J Geriatr Cardiol 17(2):101–107
Chang SS, Weiss CO, Xue QL, Fried LP (2012) Association between inflammatory-related disease burden and frailty: results from the Women’s Health and Aging Studies (WHAS) I and II. Arch Gerontol Geriatr 54(1):9–15
Anker SD, von Haehling S (2004) Inflammatory mediators in chronic heart failure: an overview. Heart 90(4):464–470
Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal H et al (2014) Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev 4:Cd003331
Turner G, Clegg A (2014) Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing 43(6):744–747
Conflict of interest
None.
Ethical standard
The manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jha, S.R., Ha, H.S.K., Hickman, L.D. et al. Frailty in advanced heart failure: a systematic review. Heart Fail Rev 20, 553–560 (2015). https://doi.org/10.1007/s10741-015-9493-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-015-9493-8