Abstract
Severe preeclampsia (PE) is a major cause of maternal mortality and morbidity worldwide. Signal transducer and activator of transcription 3 (Stat3) signal pathway can modulate various fundamental cellular processes. However, whether Stat3 plays a role in the pathogenesis of severe PE is unknown. Therefore, in this study, the expression levels of Stat3 pathway-related genes and proteins, Stat3, pStat3, IL-6, Mcl-1L, Bcl-xL, survivin, MMP-2, and MMP-9, were evaluated by immunohistochemistry (IHC), Western blot analysis and real-time PCR in the severe preeclamptic placentas. Our results showed that Stat3 and pStat3 immunoreactivity were localized in both extravillous cytotrophoblast cells and villous trophoblast cells in the placentas. As compared with normotensive pregnancies, significantly decreased expressions of Stat3 and pStat3 proteins were observed in extravillous cytotrophoblast cells, villous trophoblast cells and entire placentas in patients with severe PE. The expression levels of Stat3, IL-6, survivin and MMP-2 mRNA were significantly decreased in severe preeclamptic placentas, while Mcl-1L, Bcl-xL and MMP-9 mRNA levels were unchanged. IHC results further confirmed that there was a significant decrease of IL-6, survivin and MMP-2 proteins expression in the severe preeclamptic placentas compared with the normal specimens. These findings suggested that decreased expression and activation of the Stat3 may be caused by decreased expression of a Stat3 upstream gene, such as IL-6. Decreased Stat3 expression and activation may play an important role in the pathogenesis of PE through regulation of the transcription of the Stat3 targeted genes survivin and MMP-2 to modulate apoptosis and invasion of placental trophoblastic cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia (PE), a pregnancy complication, is generally characterized by the development of hypertension and proteinuria after 20 weeks gestation in a previously normotensive woman (Sibai et al. 2005). PE, especially severe PE, is one of the major contributors to maternal and fetal mortality and morbidity worldwide. PE patients and their offspring also suffer from relatively high subsequent cardiovascular risks (Davison et al. 2004). Although different studies on the etiopathogenesis and mechanism of PE has been conducted, its precise pathogenesis remains uncertain in many facets (Lyall 2011). It is believed that the placenta may play a central role in the development of PE (Huppertz 2008; Myatt 2002).
Increased apoptosis and decreased invasion and migration ability of trophoblast cells in the placenta may be the major causes of PE (Davison et al. 2004; Ishihara et al. 2002; Leung et al. 2001; Rampersad and Nelson 2007; Tomas et al. 2011). A large body of research has proven that placental apoptosis is increased in PE. Increased apoptosis level was observed not only on entire preeclamptic placentas, but also on specific cell types of preeclamptic placenta (Ishihara et al. 2002; Leung et al. 2001; Rampersad and Nelson 2007; Tomas et al. 2011). Villous cytotrophoblast cells and syncytiotrophoblast cells show increased apoptosis (Tomas et al. 2011). It was also found that PE is associated with widespread apoptosis of placental cytotrophoblasts within the uterine wall (DiFederico et al. 1999). Moreover, enhanced apoptosis has been demonstrated in preeclamptic villous trophoblast cells in vitro (Crocker et al. 2003; Hu et al. 2006). Indeed, there is a close relationship between trophoblast apoptosis and invasion in the placenta of PE. In PE, increased apoptosis of trophoblasts can decrease trophoblasts invasion. Shallow trophoblast invasion of the uterine spiral arterioles subsequently leads to a failure to establish adequate uteroplacental blood flow and is therefore thought to give rise to relatively hypoxic trophoblast tissue. This, in turn, may promote an exaggerated state of oxidative stress in the placenta and increase apoptosis of trophoblast cells. Consequently, these will induce the occurrence of PE (Rampersad and Nelson 2007).
Various autocrine and paracrine factors and signal pathways have been suggested to modulate apoptosis and invasion levels of trophoblast cells, including signal transducer and activator of transcription 3 (Stat3) (Fitzgerald et al. 2008; Heazell and Crocker 2008; Jovanovic and Vicovac 2009; Onogi et al. 2011). Stat3 is activated by the entire family of IL-6-type cytokines, these cytokines signal through gp130 and related receptors, whose dimerization can subsequently result in the activation of receptor kinase activity. The activated receptor then phosphorylates and activates the Janus tyrosine kinases (JAKs), which subsequently phosphorylate the Stat3 protein (Hirano et al. 2000; Huang et al. 2010). Thereby, pStat3 migrates from the cytoplasm to the cell nucleus, where it binds to cognate DNA sequences and regulates the transcription of target genes, such as apoptosis-associated genes Mcl-1L, Bcl-xL, survivin, and invasion-related genes MMP-2 and MMP-9 (Garcia et al. 2007; Li et al. 2008; Liu et al. 2003; Xie et al. 2004).
In Stat3-deficient mice by gene targeting, Stat3-deficient embryos showed rapid degeneration between embryonic days 6.5 and 7.5, suggesting that Stat3 is essential for the early development of mouse embryos (Takeda et al. 1997). It has also been demonstrated that Stat3 is a key regulator of trophoblast invasion and that phosphorylated Stat3 enhances the invasiveness of trophoblast cells (Corvinus et al. 2003; Fitzgerald et al. 2008). However, at present, whether Stat3 plays a role in the pathogenesis of severe PE is unknown. In the current study, we determined the expression and/or activation of Stat3 signal pathway in the placenta of patients with severe PE.
Materials and methods
Study population
Placentas delivered from 27 severe preeclamptic pregnancies and 23 normal control pregnant women were obtained from The Third Affiliated Hospital of Zhengzhou University in accordance with the institution’s ethics guidelines. The severe preeclamptic patients met the diagnostic criteria based on either blood pressure ≥160 mm Hg systolic or ≥110 mm Hg diastolic on two occasions at least 6 h apart while they were on bed rest, or proteinuria ≥5 g in a 24 h urine specimen or ≥3+ on 2 random urine samples collected at least 4 h apart. Patients suffering from kidney disease, chronic hypertension, diabetes, fetal malformations, multiple gestations, and infectious diseases were excluded. None of the study subjects had signs of infections or preterm rupture of membrane. In addition, all patients underwent cesarean section without labor to avoid threatened labor.
Placental tissues collection
Placental samples were collected as previously described (Zhang et al. 2013a). The placental biopsies were collected within 15 min after delivery. Five small separate biopsies (2 × 2 × 1 cm) were taken from five different areas of the placenta, including one from the center portion and one from each quadrant (3, 6, 9 and 12 o’clock) of the placental maternal surface. All samples included full-thickness placental blocks. Areas with macroscopic evidence of necrosis, infarction, and calcification were avoided when collecting the samples. The blood in tissue samples was absorbed by sterile filter paper. One part of fresh placental tissues was washed with 0.9 % NaCl and then fixed with 4 % paraformaldehyde for immunohistochemistry (IHC) study. Another part was immediately snapped frozen in liquid nitrogen and then stored at −80 °C for real-time PCR and Western blot. The relevant clinical data on the study subjects are shown in Tables 1 and 2.
Immunohistochemistry
IHC was performed to assess localization and expression of relative proteins in placental sections derived from severe PE and normotensive pregnant women. In brief, placental paraffin sections were deparaffinized and hydrated through xylene and graded alcohol. Antigens were retrieved by boiling slides in relevant unmasking solution (Maixin, Fujian, China). The slides were then allowed to cool and blocked with 3 % H2O2 for 10 min to quench endogenous peroxidase activity. To reduce non-specific background staining, the sections were incubated with blocking solution for 1 h at room temperature. Subsequently, the slides were probed with the following antibodies in a humidified chamber at 4 °C overnight: anti-vimentin antibody (Maixin), anti-cytokeratin antibody (Maixin), anti-HLA-G antibody (Abcam Limited, Cambridge, UK), mouse anti-human Stat3 monoclonal antibody (Cell Signaling Technology, Beverly, MA, USA)), rabbit monoclonal antibodies to human pStat3 (CST), mouse monoclonal antibody to human IL-6 (Abcam), rabbit monoclonal antibodies to human survivin (CST), and rabbit monoclonal antibody to human MMP-2 (Abcam). After a thorough wash in PBS, the reactions were detected with MaxVision™ HRP-Polymer anti-Mouse IHC Kit and anti-Rabbit IHC Kit, respectively, and visualized by reinforced DAB Plus Kit (Maxin) according to the manufacturer’s directions. Finally, the slides were counterstained with Hematoxylin QS (Vector Laboratories, Burlingame, CA, USA), dehydrated with xylene, and mounted with VectaMount AQ (Vector Laboratories). We included several known positive breast carcinoma or cervical carcinoma specimens, and negative controls in each run. The intensities of immunostaining were graded using a conventional semiquantitative four-point scale (0, absent staining/no color; 1, weakly positive staining/pale brown color; 2, moderately positive staining/dark brown color; and 3, strongly positive staining/brownish-black color). The staining intensity was evaluated by two separate, blinded pathologists. All images were obtained by Olympus IX-71 microscope (Olympus, Tokyo, Japan) equipped with a DP-71 Digital Camera (Olympus) and were processed with Adobe Photoshop version 7.0 software (Adobe Systems, San Jose, CA, USA).
Western blot analysis
To determine the protein expression levels of Stat3 and pStat3 in placental tissues, protein lysates were extracted from placental tissues using protein extraction kit (Sangon, Shanghai, China) according to the manufacturer’s instructions. Proteins concentrations were evaluated by BCA assay (Sangon), and Western blot analysis was conducted following previously described protocols (Zhang et al. 2013a). Briefly, 70 μg of protein was separated on 10 % SDS-PAGE and electrotransferred onto nitrocellulose membrane. The membranes were blocked with 5 % nonfat milk in TBST (Stat3) or 5 % BSA (pStat3) for 2 h accordingly, and they were subsequently incubated with primary antibodies at 4°C overnight. The dilutions of Stat3, pStat3 and β-actin (Biotechnology Co. Beijing, China) were 1:2000, 1:1000 and 1:1000, respectively. On the following day, the membranes were washed in TBST three times and probed with appropriate secondary peroxidase-labeled IgG (1:15,000, Dingguo, Beijing, China) for 1 h at room temperature. The protein bands were finally visualized with ECL detection reagents (Tiangen, Beijing, China). After exposure in the darkroom, protein bands were observed on X-ray film (Eastaman Kodar Co, NY, California, USA). Quantitative analysis of Western blot was performed by densitometry with the Gel logic 2000 image system (Eastaman Kodar).
Real-time PCR assay
Real-time PCR was performed to verify the expression levels of IL-6, Stat3, Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 mRNA in severe preeclamptic and normal control placentas. Total RNA was extracted from the placental tissue with Trizol Reagent® (Life Technologies, Grand Island, NY, USA) according to the manufacturer’s recommendations. RNA was then quantified using an ultraviolet spectrophotometer at 260 nm. RNA integrity was evaluated using agarose gel electrophoresis to determine the ratio of 28S/18S rRNA in each sample. Reverse Transcriptase M-MLV kits (TaKaRa, Dalian, China) were used for reverse transcription to synthesize cDNA.
For the Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 genes, a relative standard curve method and analysis method were used as previously described (Zhang et al. 2011b). The sequences of the Mcl-1L primers used were 5′-CCTTCCAAGGCATGCTTCG-3′ (sense), 5′-GTCTTCAAGTGTTTAGCCAC-3′ (anti-sense), and 5′-ATGAGAGTCACAATCCTGCCCCA-3′ (probe). The sequences of the Bcl-xL primers used were 5′-GCTGGGATACTTTTGTGGAACT-3′ (sense), 5′-TCATTTCCGACTGAAGAGTGAG-3′ (anti-sense), and 5′-CGGCCACAGTCATGCCCGTC-3′ (probe). The sequences of the survivin primers used were 5′-GTTGCGCTTTCCTTTCTGTC-3′ (sense), 5′-CGCAGTTTCCTCAAATTCTTTC-3′ (anti-sense), and 5′-TTCTTGGCTCTTTCTCTGTCCAG-3′ (probe). The sequences of the MMP-2 primers used were 5′-ACCAGATCACATACAGGATC-3′ (sense), 5′-CTCTCCATCATGGATTCGAG-3′ (anti-sense), and 5′-TACACACCTGATCTGGACCCAGA-3′ (probe). The sequences of the MMP-9 primers used were 5′-AGATGCGTGGAGAGTCGAAATC-3′ (sense), 5′-GGTTCGCATGGCCTTCAGT-3′ (anti-sense), and 5′-AAGCAACTGTCCCTGCCCGAGACC-3′ (probe). The sequences of the β-actin primers used were 5′-GCGAGAAGATGACCCAGATC-3′ (sense), 5′-ACCGGAGTCCATCACGATG-3′ (anti-sense), and 5′-CTTCAACACCCCAGCCATGTACG-3′ (probe). The final real-time PCR reaction system (20 μL) was composed of 10 μL of 2× Taq PCR Master Mix (Lifefeng, Shanghai, China), 0.5 μL each of 12.5 μM forward and reverse primers (Sangon), 2.5 μL of 2.5 μM Taqman probe (Sangon), 0.5 μL of ROXII (Sangon), 2.5 μL of 2.5 mM Mg2+ (Sangon), 1 μL of template cDNA and 2.5 μL of RNA-free H2O. The PCR amplification was performed with initial denaturation at 95 °C for 2 min, and followed by 40 cycles at 95 °C for 15 s, and 60 °C for 1 min. The amplified transcripts were quantified in comparison to a standard curve, employing β-actin as the internal control. For IL-6 and Stat3, real-time PCR was also performed as previously described (Zhang et al. 2013b). The sequences of the Stat3 primers used were 5′-CTCAAGATTGACCTAGAGAC-3′ (sense), and 5′-TGGGATTGTTGGTCAGCATG-3′ (anti-sense). The sequences of the IL-6 primers used were 5′-TGAACTCCTTCTCCACAAGC-3′ (sense), and 5′-AGGTGAGTGGCTGTCTGTG-3′ (anti-sense). We used the 2−ΔΔCt method to analyze IL-6 and Stat3 mRNA expression level, and β-actin was used as the internal control. As a negative control for all reactions, preparations lacking RNA were used in place of the cDNA. All samples were run in triplicate and were performed using an Applied Biosystems 7500 instrument (ABI, Foster City, CA, USA).
Statistical analysis
Statistical analysis was undertaken using SPSS 17.0 software. Data are presented as the mean ± SD. For comparisons between the two groups, we used an unpaired Student’s t test, Mann–Whitney U test, Kruskal–Wallis test or Chi square (χ2) test as appropriate. P < 0.05 value was considered as statistically significant.
Results
Location of Stat3 and pStat3 proteins in the placentas of severe PE and control patients
Villous trophoblast cells (VT) were easily distinguished form extravillous cytotrophoblast cells (EVT) and decidual cells by hematoxylin and eosin (H&E) (Fig. 1a, b). However, it is difficult to identify EVT and decidual cells in term placentas through morphology alone. It has been reported that decidual cells are distinguished by positive vimentin staining and negative cytokeratin staining, while EVT are identified by negative vimentin staining, positive cytokeratin and positive HLA-G staining (Lockwood et al. 2008b). Therefore, severe preeclamptic and control placentas were immunostained for vimentin, cytokeratin and HLA-G. As expected, EVT in sections from severe preeclamptic placentas and normal specimens were identified by negative vimentin staining (Fig. 1c, d), positive cytokeratin staining (Fig. 1e, f) and positive HLA-G staining (Fig. 1g, h). IHC was then performed to determine whether severe preeclamptic and normal placentas express Stat3 and pStat3 proteins. The results showed that immunostaining of Stat3 (Fig. 2a–f) and pStat3 (Fig. 3a–f) were localized in EVT, as well as VT in the two groups. Both cytoplasmic and nuclear immunostaining of Stat3 was detected. Stat3 was mainly expressed in the cell cytoplasm, with some in the nucleus (Fig. 2e, h), while specific localization of immunostaining with pStat3 was observed in the cell nucleus (Fig. 3e, h). IHC staining of breast carcinoma specimen with Stat3 (Fig. 2g, h) and pStat3 (Fig. 3g, h) was used as positive control. For negative control, IHC staining of breast carcinoma specimen was carried out using PBS buffer instead of primary antibody (Figs. 2i, 3i).
Identification of extravillous trophoblast (EVT) cells in placentas of severe preeclampsia (PE) and normal control groups. a, b Representative H&E staining of placental tissue sections generated from severe PE and normal control groups. c, d Immunohistochemistry (IHC) staining of vimentin in paraffin sections of severe preeclamptic and normal placentas. e, f IHC staining of cytokeratin in placentas derived from two groups. g, h IHC staining of severe preeclamptic and clinically normal placentas with HLA-G antibody. Arrows indicate EVT. Slides were viewed with an Olympus IX-71 microscope at a magnification of ×200. All images were captured with a DP-71 Digital Camera and processed with Adobe Photoshop version 7.0 software
Expression level of Stat3 was decreased in extravillous trophoblast (EVT) and villous trophoblast (VT) of severe preeclamptic placentas as determined by immunohistochemistry (IHC). a–f Representative results from IHC staining with Stat3 antibody of placental specimens collected from severe preeclampsia (PE) and normotensive pregnant women. g–h Breast carcinoma specimen was used as positive control. i IHC was carried out using PBS buffer instead of primary antibody served as negative control. j Summary of Stat3 staining in EVT from severe preeclamptic and normal placentas. k Distribution of Stat3 immunohistochemical staining scores in VT of two groups. Panels b, e and h are high magnification images of panels a, d and g, respectively. Left panel magnification ×200; middle panel magnification ×400; right panel magnification ×200. Arrows in a–h indicated positive expression of Stat3
Decreased pStat3 expression was observed in severe preeclamptic placentas as determined by immunohistochemistry (IHC). a–f Examples of cases immunostained for pStat3 in paraffin sections from severe preeclamptic and normal control placentas. g–h Breast carcinoma specimen was used as positive control. i Primary antibody was omitted as negative control. j Distribution of pStat3 immunohistochemical staining scores in extravillous trophoblast (EVT) from 27 of severe preeclamptic placentas and 23 normal placentas. k Summary of Stat3 staining in villous trophoblast (VT) of two groups. Panels b, e and h are high magnification images of panels a, d and g, respectively. Left panel magnification ×200; middle panel magnification ×400; right panel magnification ×200. Arrows in a–h indicated positive expression of pStat3
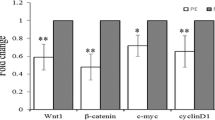
A significant reduction of Stat3 and pStat3 proteins expression in the severe preeclamptic placentas
To test the expression levels of Stat3 and pStat3 proteins in severe preeclamptic placentas, IHC was first conducted in placental tissues sections collected from 27 severe PE and 23 normotensive pregnant women. The results showed that both Stat3 and pStat3 displayed weaker staining intensity in the EVT of severe PE group (Figs. 2a, b, 3a, b) than the control group (Figs. 2d, e, 3d, e). The same results were found in VT of the two groups. For VT, the immunostaining of Sat3 and pStat3 was significant reduced in the severe PE group (Figs. 2c, 3c) compared with that in the normal control group (Figs. 2f, 3f). The immunostaining intensities of Stat3 and pStat3 were then categorized in Figs. 2j, k and 3j, k. The staining intensity of Stat3 was significant weaker in EVT and VT of the severe preeclamptic placentas than that of normal control placentas (χ2 = 11.373, P = 0.010; χ2 = 11.809, P = 0.008, respectively). Both EVT and VT of severe preeclamptic placentas had remarkable lower expression levels of pStat3 protein than matched control specimens (χ2 = 9.825, P = 0.020; χ2 = 9.477, P = 0.024, respectively).
Western blot was then performed to further verify the protein expression levels of Stat3 and pStat3 in the entire placentas of severe PE. As expected, statistically significant decreased expression levels of Stat3 and pStat3 were observed in severe preeclamptic placentas as compared with those of normal control placentas (0.486 ± 0.052 vs 1.000 ± 0.248, P < 0.001; 0.485 ± 0.047 vs 1.000 ± 0.068, P = 0.001, respectively; Fig. 4). It is notable that the placenta is a complex organ containing various cells, such as syncytiotrophoblasts, cytotrophoblasts, extravillous cytotrophoblasts, fibroblasts, macrophages, immunological cells and hofbauer cells (Castellucci and Kaufmann 2006; Unek et al. 2014). Although the placenta was washed several times, and interstitial tissues were wiped out as thoroughly as possible when we extracted protein, it was still impossible to obtain single trophoblast cells from the placenta. Therefore, objectively, the Western blot results indicate the Stat3 and pStat3 expression level in the entire placenta, but not only in trophoblast cells.
Western blot analysis of Stat3 and pStat3 proteins expression in severe preeclamptic and normal control placentas. a Representative bands of Stat3 and pStat3 proteins in placentas derived from normal pregnancies and pregnancies complicated with severe preeclampsia (PE). b Relative Stat3 and pStat3 expression in placentas of two groups was analyzed by densitometry. For comparison of the two groups, the mean intensity value of the control group was arbitrarily set at 1. Data from severe preeclampsia were then normalized to the expression level in normal control group. ** indicated P value <0.05
Decreased Stat3 and IL-6 gene expression level in placentas derived from severe preeclamptic pregnant women
As previously demonstrated, a significant reduction of Stat3 and pStat3 protein expression was observed in the placentas of severe PE as compared with that of normotensive pregnant women. To examine whether this change occurs at the post-transcriptional or transcriptional level, Stat3 mRNA expression level was measured using real-time PCR. The results suggested that there was a statistically significant decrease of Stat3 mRNA expression in the severe preeclamptic placentas compared with the control specimens (0.521 ± 0.022 vs 1.000 ± 0.033, P = 0.048; Fig. 5).
It has been proven that decreased Stat3 phosphorylation can be induced by decreased Stat3 gene and/or protein expression in numerous cancers, including choriocarcinoma. Moreover, a decreased expression level of upstream gene and/or protein in the Stat3 pathway, such as IL-6, has the ability to lead to a decline in Stat3 phosphorylation. It is well known that IL-6 exerts biological effects by binding to its receptors on target cells. The binding of IL-6 to IL-6R can subsequently trigger the phosphorylation of Stat3. Therefore, we further evaluated the expression level of IL-6 mRNA in the placentas collected from 27 pregnant women with severe PE and 23 women with normotensive control pregnancies. Reduced IL-6 mRNA level was found in severe preeclamptic placentas when compared with normal placentas (0.537 ± 0.026 vs 1.00 ± 0.0312, P = 0.040; Fig. 5).
Alteration of expression of IL-6 protein in severe preeclamptic placentas
To elucidate the expression level of IL-6 protein in severe PE, we performed IHC on the paraffin sections of severe preeclamptic and normal control placentas. IHC results confirmed that expression of IL-6 was detected in EVT and VT of the study group and the matched controls (Fig. 6a–d). The specific localization of immunostaining with IL-6 was mainly detected in membrane and/or cytoplasm in EVT and VT. Cervical carcinoma specimen was used as positive control (Fig. 6e). For negative control, IHC was carried out using PBS buffer instead of primary antibody (Fig. 6f). Notably, the IHC results demonstrated that IL-6 expression was significantly decreased in both EVT and VT of severe preeclamptic placentas as compared to normal controls (Fig. 6a–d, g, h, χ2 = 8.573, P = 0.036 and χ2 = 8.209, P = 0.042, respectively), which was consistent with the results of real-time PCR that severe preeclamptic placentas had lower expression levels of IL-6 mRNA than matched controls.
Decreased IL-6 protein expression was exhibited in severe preeclamptic placentas as determined by immunohistochemistry (IHC). a–d Representative immunohistochemical images of placental sections of severe preeclampisa (PE) and normal control. e Paraffin section from a known IL-6-positive cervical carcinoma tissue served as positive control. f IHC staining without primary antibody was suggested as negative control. g Distribution of IL-6 immunohistochemical staining scores in extravillous trophoblast (EVT) from 27 of severe preeclamptic placentas and 23 normal placentas. h Summary of IL-6 staining in villous trophoblast (VT) of two groups. Magnification: ×400; Arrows indicated positive expression of IL-6
Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 mRNA expression levels in severe PE
A number of reports have suggested that pStat3 can regulate the transcription of Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 in numerous diseases, especially in human cancer. To confirm whether there is aberrant Mcl-1L, Bcl-xL, MMP-2 and MMP-9 mRNA expression in severe preeclampsia, real-time PCR was performed to determine the relative gene expression levels. The results revealed that compared with the control group, the expression levels of survivin and MMP-2 mRNA were significantly decreased in severe preeclamptic placentas (5.483 ± 0.594 vs 8.227 ± 0.594, P < 0.001; 2.782 ± 0.190 vs 3.816 ± 0.715, P < 0.001, respectively; Fig. 7), while Mcl-1L, Bcl-xL and MMP-9 mRNA expression levels were unchanged in severe preeclamptic placentas when compared to control specimens (4.924 ± 0.270 vs 5.832 ± 0.194, P = 0.575; 5.614 ± 0.344 vs 6.016 ± 0.173, P = 0.102; 6.415 ± 0.228 vs 6.724 ± 0.105, P = 0.074, respectively; Fig. 7).
Stat3 signal pathway target genes Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 mRNA expression levels in severe preeclampsia and in normal control groups. Mcl-1L, Bcl-xL, survivin, MMP-2 and MMP-9 mRNAs quantification was shown with the gene copies normalized relative to the β-actin mRNA level (log copies). Compared with the normal control group, the mRNA expression level of survivin and MMP-2 was statistically decreased in severe preeclamptic placentas, while Mcl-1L, Bcl-xL and MMP-9 mRNA levels were unchanged. ** indicated P value <0.05
Aberrant expression levels of survivin and MMP-2 proteins in the placentas collected from patients with severe PE
IHC was then performed to determine whether altered expression levels of survivin and MMP-2 proteins are present in preeclamptic placentas. Our findings suggested that survivin was mainly expressed in the cell nucleus, and specific MMP-2 protein staining was mainly observed in cell cytoplasm (Fig. 8a–l). Survivin and MMP-2 immunoreactivity was shown both EVT and VT of placentas of two groups (Fig. 8a–h). Paraffin sections from a known survivin-positive breast carcinoma and MMP-2-positive cervical carcinoma tissues served as positive controls, respectively (Fig. 8i, k), and PBS buffer instead of primary antibody was used as negative control (Fig. 8j, l). Expression levels of survivin and MMP-2 were then evaluated by semiquantitative analysis of IHC staining, and the results were shown in Fig. 8m–p. Interestingly, the expression level of survivin showed no significant differences in EVT of the two groups (Fig. 8m, χ2 = 1.785, P = 0.618), while the intensity of survivin was lower in VT of severe preeclamptic tissues as compared with that of normal control (Fig. 8n, χ2 = 8.305, P = 0.040). As expected, a significantly decreased expression level of MMP-2 protein was present in EVT, as well as VT of severe preeclamptic placentas as compared with that of matched controls (Fig. 8o, p, χ2 = 17.025, P = 0.001 and χ2 = 7.493, P = 0.024, respectively), which was consistent with the real-time PCR results that severe preeclamptic placentas exhibited lower expression levels of survivin and MMP-2 mRNA than control placentas.
Decreased expression levels of survivin and MMP-2 proteins in severe preeclamptic placentas. a–h Representative images from IHC staining of placental sections derived from severe preeclamptic and normal pregnant women with survivin and MMP-2. i, k Breast carcinoma or cervical carcinoma tissues were used as positive control. j, l PBS buffer instead of primary antibody was used as negative control. m, n Distribution of survivin immunohistochemical staining scores in extravillous trophoblast (EVT) and villous trophoblast (VT) from 27 of severe preeclamptic placentas and 23 normal placentas, respectively. o, p Summary of MMP-2 staining in EVT and VT of two groups, respectively. Magnification: ×400; Arrows indicated positive expression of survivin and MMP-2, respectively
Discussion
In the present study, we demonstrated that the expression levels of Stat3 and pStat3 proteins were significantly decreased in EVT, VT and the entire placenta of severe PE compared with normal controls as determined by IHC in paraffin sections and Western blot in frozen specimens. Our findings indicated that a decreased expression level of Stat3 protein may contribute to decreased Stat3 phosphorylation in severe PE. Previously, IHC results revealed that the expression level of pStat3 was lower in trophoblast cells of term placentas than that in first trimester human placentas, and preeclamptic placentas showed the lowest expression level of pStat3 (Weber et al. 2009). It has been further suggested that trophoblast cells of PE-disturbed placentas expressed less Stat3 and pStat3 than those of healthy third-trimester control placentas as determined by IHC and immunofluorescence (IF; Weber et al. 2012). In previous studies, IHC and IF were used to investigate the placental distribution of Stat3 and pStat3 in preeclamptic placental trophoblast cells. However, placental trophoblast cells include EVT and VT, and the placenta is a complex organ containing a variety of cells, not only trophoblast cells. Therefore, the expression and activation levels of Stat3 in EVT and VT of severe preeclamptic placentas were analyzed in our current study. Moreover, to determine the expression levels of Stat3 and pStat3 in the entire severe preeclamptic placentas, Western blot, which can identify the protein level in fresh or frozen tissues, was employed. Thus, our results may reveal more representative Stat3 and pStat3 expression levels in the severe preeclamptic placentas, not only in trophoblast cells. Reflective of our findings that decreased Stat3 protein expression may lead to lower pStat3 expression in PE patients, we further demonstrated that declined Stat3 may be a response to decreased Stat3 gene transcription. Our results showed that Stat3 mRNA was decreased in severe PE as well indicating that this aberration may initially occur at the gene transcriptional level.
IL-6, an upstream gene of the Stat3 signal pathway, can simulate Stat3 protein phosphorylation, which subsequently induces targeted gene transcription, such as MMP-2, MMP-9 and survivin. This is one way for IL-6 to take part in various biological processes, including anti-apoptosis, modulation of invasion and migration, and the immune response (Chen et al. 2009; Guo et al. 2012). IL-6 has been demonstrated to stimulate cell migration, invasion and integrin expression in the human trophoblast-derived HTR-8/SVneo cells, and both exogenous and endogenous IL-6 can stimulate trophoblast cell migration and invasion (Jovanovic and Vicovac 2009). IL-6 has been consistently suggested to be present at higher blood serum concentrations in preeclamptic patients than in normal pregnancies (Xie et al. 2011), while the expression level of IL-6 in preeclamptic placentas remains controversial. Previous observations showed that IL-6 expression was either unchanged or even reduced in preeclamptic compared with control placentas (Lockwood et al. 2008a). In agreement with previous findings that IL-6 mRNA is decreased in preeclamptic placentas (Benyo et al. 2001), our results showed that there was a remarkable decreased expression level of IL-6 mRNA and protein in severe preeclamptic placentas compared with normal controls. Decreased IL-6 mRNA may induce decreased IL-6 protein expression, which subsequently lead to decreased Stat3 phosphorylation as our results showed in the current study. Therefore, our findings revealed that both decreased Stat3 mRNA/protein and decreased Stat3 upstream gene IL-6 may contribute to the decreased Stat3 activation in severe PE. Although preeclamptic placentas express less IL-6 than normal placentas, elevated IL-6 concentration is reported in the blood serum of PE. In preeclamptic pregnancies, IL-6 does not appear to be produced by the placenta itself; the phagocytosis of dead trophoblastic cells by endothelial cells may lead endothelial cells to secrete IL-6, which subsequently cause the activation of additional endothelial cells, allowing the systemic spreading of endothelial activation and increased IL-6 serum concentration.
IL-6 has been shown to increase the activity of MMP-2 in primary first trimester cytotrophoblast cells in culture, and Stat3 has the ability to regulate targeted gene MMP-2 transcription. MMP-2 is a gelatinase that cleaves type IV collagen and is considered a key molecule in the human trophoblast invasion process (Isaka et al. 2003; Shiozaki et al. 2003; Staun-Ram et al. 2004; Wang et al. 2013; Xie et al. 2004). We demonstrated that the expression level of MMP-2 was significantly decreased in severe preeclamptic placentas compared with normal controls. Similar to IL-6 expression level in PE, the expression of MMP-2 also remains controversial. Previous studies reported thatMMP-2 expression was either reduced or unchanged in preeclamptic placentas compared to normal controls (Omran et al. 2011; Zhang et al. 2011a), whereas the pregnancies with PE have higher plasma MMP-2 concentration than healthy pregnancies (Palei et al. 2012). It also has been suggested that the expression level of survivin was regulated by Stat3 in numerous cells, including trophoblast cells. Survivin is a member of the inhibitor of apoptosis protein (IAP) family, which plays important roles in trophoblast proliferation and survival. Consistent with previous studies (Li et al. 2012), our data obtained from 27 severe preeclamptic placentas and 23 normal placentas showed that both the mRNA level and protein levels of survivin in severe preeclamptic placentas are significantly reduced compared with that in normal placentas. However, the expression level of survivin in preeclamptic placentas has been controversially reported. Reports have shown that the survivin gene is reduced in preeclamptic placentas compared with normal specimens, whereas the protein level of survivin is not correlated to its gene level in preeclamptic placentas, and no remarkable alteration in the protein level of survivin has been observed between preeclamptic placentas and normal controls by applying Western blot and IHC (Muschol-Steinmetz et al. 2013). The study that compared 8 preeclamptic placentas with 8 normal placentas also showed that there is no significant difference in protein expression of survivin between preeclamptic placentas and normal pregnancy placentas (Heazell et al. 2008). The explanation for these contradictions may be the differences in patients, sample size, gestational ages, antibodies used and experimental methods among different studies. In the current study, our results suggested that decreased MMP-2 and survivin expression, which are regulated by Stat3, may be directly linked to reduced trophoblast apoptosis and invasion in severe PE. In addition, Mcl-1L, Bcl-xL and MMP-9 mRNA expression were unchanged between severe PE and normal controls. Previous studies also demonstrated that Mcl-1L mRNA expression was unchanged between PE and preterm normotensive age-matched control placentas, whereas Mcl-1S expression was significantly increased in PE (Soleymanlou et al. 2007).
Since the rate of apoptosis in the placentas of patients who undergo premature delivery is increased (Demendi et al. 2012) and that some cytokines, such as IL-6, are abnormal (Gulati et al. 2012), to avoid the effects of premature delivery on the apoptosis and cytokines expression levels, the length of gestation in our normal control group was greater than 37 weeks. However, in the present study, the severe preeclamptic group included women with pregnancies complicated by preterm labor. It is well known that the women with PE experience higher incidence of spontaneous and induced preterm birth than normal pregnant women, and it is therefore difficult to include severe preeclamptic patients who do not have preterm labor. For example, the clinical characteristics of study participants, including 100 women with PE and 100 normotensive pregnant women indicated that average gestational age at delivery from the PE group was 4.9 weeks earlier than that of the normal control group (Xu et al. 2014). It also has been shown that patients with PE (n = 53) had obviously lower gestational age (weeks) at delivery compared with normal pregnancies (n = 50) (32.4 ± 3.7 vs 39.0 ± 1.0, P < 0.001; Cozzi et al. 2012). Moreover, the diagnosis of PE includes severe PE and mild PE, and maternal outcome in women with severe PE is worse than that in patients with mild PE. Reports revealed that gestational age (weeks) at delivery of severe PE group (n = 53) was significantly lower than mild PE (n = 27; 32 vs 37, P < 0.001; Robinson et al. 2006). However, apoptosis increases as pregnancy progresses (Halperin et al. 2000; Smith and Baker 1999), and we found a decreased expression level of Stat3 pathway-related genes in severe preeclamptic placentas compared with control term placentas, whose gestational age was significantly greater than those from patients with PE. It is reasonable to speculate that the expression of some Stat3 pathway genes would be further decreased in preeclamptic placentas when compared with a gestational aged-matched normal control group, and that the statistical differences would be much more significant than those found in this study.
In summary, we found decreased expression and activation of Stat3 in severe preeclamptic placentas, which may be caused by decreased Stat3 gene transcription and/or decreased IL-6. Furthermore, we demonstrated that the expressions of Stat3 downstream genes survivin and MMP-2 were reduced in preeclamptic placentas. These findings indicate that the aberrant expression and activation of Stat3 may contribute to the pathogenesis of PE by regulating trophoblast cells apoptosis and invasion.
References
Benyo DF, Smarason A, Redman CW, Sims C, Conrad KP (2001) Expression of inflammatory cytokines in placentas from women with preeclampsia. J Clin Endocrinol Metab 86:2505–2512
Castellucci M, Kaufmann P (2006) Basic structure of the villous trees. In: Pathology of the human placenta. Springer, New York, pp 50–120. doi:10.1007/0-387-26742-5_6
Chen Q, Stone P, Ching LM, Chamley L (2009) A role for interleukin-6 in spreading endothelial cell activation after phagocytosis of necrotic trophoblastic material: implications for the pathogenesis of pre-eclampsia. J Pathol 217:122–130. doi:10.1002/path.2425
Corvinus FM, Fitzgerald JS, Friedrich K, Markert UR (2003) Evidence for a correlation between trophoblast invasiveness and STAT3 activity. Am J Reprod Immunol 50:316–321
Cozzi V, Garlanda C, Nebuloni M, Maina V, Martinelli A, Calabrese S, Cetin I (2012) PTX3 as a potential endothelial dysfunction biomarker for severity of preeclampsia and IUGR. Placenta 33:1039–1044. doi:10.1016/j.placenta.2012.09.009
Crocker IP, Cooper S, Ong SC, Baker PN (2003) Differences in apoptotic susceptibility of cytotrophoblasts and syncytiotrophoblasts in normal pregnancy to those complicated with preeclampsia and intrauterine growth restriction. Am J Pathol 162:637–643. doi:10.1016/S0002-9440(10)63857-6
Davison JM et al (2004) New aspects in the pathophysiology of preeclampsia. J Am Soc Nephrol 15:2440–2448. doi:10.1097/01.ASN.0000135975.90889.60
Demendi C, Borzsonyi B, Vegh V, Nagy ZB, Rigo J Jr, Pajor A, Joo JG (2012) Gene expression patterns of the Bcl-2 and Bax genes in preterm birth. Acta Obstet Gynecol Scand 91:1212–1217. doi:10.1111/j.1600-0412.2012.01428.x
DiFederico E, Genbacev O, Fisher SJ (1999) Preeclampsia is associated with widespread apoptosis of placental cytotrophoblasts within the uterine wall. Am J Pathol 155:293–301. doi:10.1016/S0002-9440(10)65123-1
Fitzgerald JS, Poehlmann TG, Schleussner E, Markert UR (2008) Trophoblast invasion: the role of intracellular cytokine signalling via signal transducer and activator of transcription 3 (STAT3). Hum Reprod Update 14:335–344. doi:10.1093/humupd/dmn010
Garcia MG et al (2007) High expression of survivin and down-regulation of Stat-3 characterize the feto-maternal interface in failing murine pregnancies during the implantation period. Placenta 28:650–657. doi:10.1016/j.placenta.2006.09.010
Gulati S, Bhatnagar S, Raghunandan C, Bhattacharjee J (2012) Interleukin-6 as a predictor of subclinical chorioamnionitis in preterm premature rupture of membranes. Am J Reprod Immunol 67:235–240. doi:10.1111/j.1600-0897.2011.01084.x
Guo Y, Xu F, Lu T, Duan Z, Zhang Z (2012) Interleukin-6 signaling pathway in targeted therapy for cancer. Cancer Treat Rev 38:904–910. doi:10.1016/j.ctrv.2012.04.007
Halperin R, Peller S, Rotschild M, Bukovsky I, Schneider D (2000) Placental apoptosis in normal and abnormal pregnancies. Gynecol Obstet Investig 50:84–87
Heazell AE, Crocker IP (2008) Live and let die—regulation of villous trophoblast apoptosis in normal and abnormal pregnancies. Placenta 29:772–783. doi:10.1016/j.placenta.2008.07.003
Heazell AE, Buttle HR, Baker PN, Crocker IP (2008) Altered expression of regulators of caspase activity within trophoblast of normal pregnancies and pregnancies complicated by preeclampsia. Reprod Sci 15:1034–1043. doi:10.1177/1933719108322438
Hirano T, Ishihara K, Hibi M (2000) Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene 19:2548–2556. doi:10.1038/sj.onc.1203551
Hu C, Smith SD, Pang L, Sadovsky Y, Nelson DM (2006) Enhanced basal apoptosis in cultured term human cytotrophoblasts is associated with a higher expression and physical interaction of p53 and Bak. Placenta 27:978–983. doi:10.1016/j.placenta.2005.11.004
Huang WL, Yeh HH, Lin CC, Lai WW, Chang JY, Chang WT, Su WC (2010) Signal transducer and activator of transcription 3 activation up-regulates interleukin-6 autocrine production: a biochemical and genetic study of established cancer cell lines and clinical isolated human cancer cells. Mol Cancer 9:309. doi:10.1186/1476-4598-9-309
Huppertz B (2008) Placental origins of preeclampsia: challenging the current hypothesis. Hypertension 51:970–975. doi:10.1161/HYPERTENSIONAHA.107.107607
Isaka K et al (2003) Expression and activity of matrix metalloproteinase 2 and 9 in human trophoblasts. Placenta 24:53–64
Ishihara N, Matsuo H, Murakoshi H, Laoag-Fernandez JB, Samoto T, Maruo T (2002) Increased apoptosis in the syncytiotrophoblast in human term placentas complicated by either preeclampsia or intrauterine growth retardation. Am J Obstet Gynecol 186:158–166
Jovanovic M, Vicovac L (2009) Interleukin-6 stimulates cell migration, invasion and integrin expression in HTR-8/SVneo cell line. Placenta 30:320–328. doi:10.1016/j.placenta.2009.01.013
Leung DN, Smith SC, To KF, Sahota DS, Baker PN (2001) Increased placental apoptosis in pregnancies complicated by preeclampsia. Am J Obstet Gynecol 184:1249–1250. doi:10.1067/mob.2001.112906
Li JJ et al (2008) Mcl-1 is regulated by IL-6 and mediates the survival activity of the cytokine in a model of late stage prostate carcinoma. In: Hormonal carcinogenesis V, vol 617. Advances in experimental medicine and biology. Springer, New York, pp 547–555. doi:10.1007/978-0-387-69080-3_56
Li CF, Gou WL, Li XL, Wang SL, Yang T, Chen Q (2012) Reduced expression of survivin, the inhibitor of apoptosis protein correlates with severity of preeclampsia. Placenta 33:47–51. doi:10.1016/j.placenta.2011.10.008
Liu H, Ma Y, Cole SM, Zander C, Chen KH, Karras J, Pope RM (2003) Serine phosphorylation of STAT3 is essential for Mcl-1 expression and macrophage survival. Blood 102:344–352. doi:10.1182/blood-2002-11-3396
Lockwood CJ et al (2008a) Preeclampsia-related inflammatory cytokines regulate interleukin-6 expression in human decidual cells. Am J Pathol 172:1571–1579. doi:10.2353/ajpath.2008.070629
Lockwood CJ et al (2008b) Preeclampsia-related inflammatory cytokines regulate interleukin-6 expression in human decidual cells. Am J Pathol 172:1571–1579. doi:10.2353/ajpath.2008.070629
Lyall F (2011) The placenta in preeclampsia. In: The placenta. Wiley-Blackwell, pp 246–252. doi:10.1002/9781444393927.ch32
Muschol-Steinmetz C, Friemel A, Kreis NN, Reinhard J, Yuan J, Louwen F (2013) Function of survivin in trophoblastic cells of the placenta PloS one 8:e73337. doi:10.1371/journal.pone.0073337
Myatt L (2002) Role of placenta in preeclampsia. Endocrine 19:103–111. doi:10.1385/ENDO:19:1:103
Omran OM, Shokry M, Ismail H, Omar G, Rezk M (2011) Expression of matrix metalloproteinases 2 and 9 in human trophoblasts of normal and preeclamptic placentas. Int J Health Sci 5:21–23
Onogi A et al (2011) Hypoxia inhibits invasion of extravillous trophoblast cells through reduction of matrix metalloproteinase (MMP)-2 activation in the early first trimester of human pregnancy. Placenta 32:665–670. doi:10.1016/j.placenta.2011.06.023
Palei AC, Sandrim VC, Amaral LM, Machado JS, Cavalli RC, Duarte G, Tanus-Santos JE (2012) Association between matrix metalloproteinase (MMP)-2 polymorphisms and MMP-2 levels in hypertensive disorders of pregnancy. Exp Mol Pathol 92:217–221. doi:10.1016/j.yexmp.2012.01.008
Rampersad R, Nelson DM (2007) Trophoblast biology, responses to hypoxia and placental dysfunction in preeclampsia. Front Biosci J Virtual Library 12:2447–2456
Robinson CJ, Johnson DD, Chang EY, Armstrong DM, Wang W (2006) Evaluation of placenta growth factor and soluble Fms-like tyrosine kinase 1 receptor levels in mild and severe preeclampsia. Am J Obstet Gynecol 195:255–259. doi:10.1016/j.ajog.2005.12.049
Shiozaki A, Kataoka K, Fujimura M, Yuki H, Sakai M, Saito S (2003) Survivin inhibits apoptosis in cytotrophoblasts. Placenta 24:65–76
Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365:785–799. doi:10.1016/S0140-6736(05)17987-2
Smith SC, Baker PN (1999) Placental apoptosis is increased in post-term pregnancies. Br J Obstet Gynaecol 106:861–862
Soleymanlou N et al (2007) Hypoxic switch in mitochondrial myeloid cell leukemia factor-1/Mtd apoptotic rheostat contributes to human trophoblast cell death in preeclampsia. Am J Pathol 171:496–506. doi:10.2353/ajpath.2007.070094
Staun-Ram E, Goldman S, Gabarin D, Shalev E (2004) Expression and importance of matrix metalloproteinase 2 and 9 (MMP-2 and -9) in human trophoblast invasion. Reprod Biol Endocrinol 2:59. doi:10.1186/1477-7827-2-59
Takeda K et al (1997) Targeted disruption of the mouse Stat3 gene leads to early embryonic lethality. Proc Natl Acad Sci USA 94:3801–3804
Tomas SZ, Prusac IK, Roje D, Tadin I (2011) Trophoblast apoptosis in placentas from pregnancies complicated by preeclampsia. Gynecol Obstet Investig 71:250–255. doi:10.1159/000320289
Unek G, Ozmen A, Mendilcioglu I, Simsek M, Korgun ET (2014) Immunohistochemical distribution of cell cycle proteins p27, p57, cyclin D3, PCNA and Ki67 in normal and diabetic human placentas. J Mol Histol 45:21–34. doi:10.1007/s10735-013-9534-3
Wang L, Zhang D, Yu Y, Guan H, Qiao C, Shang T (2013) RNA interference-mediated silencing of laminin receptor 1 (LR1) suppresses migration and invasion and down-regulates matrix metalloproteinase (MMP)-2 and MMP-9 in trophoblast cells: implication in the pathogenesis of preeclampsia. J Mol Histol 44:661–668. doi:10.1007/s10735-013-9515-6
Weber M, Kuhn C, Schulze S, Jeschke U, Markert UR (2009) Immunohistochemical analysis of STAT3 and its phosphorylated forms in human placenta. J Reprod Immunol 81:172. doi:10.1016/j.jri.2009.06.249
Weber M et al (2012) Expression of signal transducer and activator of transcription 3 (STAT3) and its activated forms is negatively altered in trophoblast and decidual stroma cells derived from preeclampsia placentae. Histopathology 60:657–662. doi:10.1111/j.1365-2559.2011.04063.x
Xie TX, Wei D, Liu M, Gao AC, Ali-Osman F, Sawaya R, Huang S (2004) Stat3 activation regulates the expression of matrix metalloproteinase-2 and tumor invasion and metastasis. Oncogene 23:3550–3560. doi:10.1038/sj.onc.1207383
Xie C, Yao MZ, Liu JB, Xiong LK (2011) A meta-analysis of tumor necrosis factor-alpha, interleukin-6, and interleukin-10 in preeclampsia. Cytokine 56:550–559. doi:10.1016/j.cyto.2011.09.021
Xu L, Lee M, Jeyabalan A, Roberts JM (2014) The relationship of hypovitaminosis D and IL-6 in preeclampsia. Am J Obstet Gynecol 210(149):e141–e147. doi:10.1016/j.ajog.2013.09.037
Zhang H, Long Q, Ling L, Gao A, Li H, Lin Q (2011a) Elevated expression of KiSS-1 in placenta of preeclampsia and its effect on trophoblast. Reprod Biol 11:99–115
Zhang X et al (2011b) Carnosine pretreatment protects against hypoxia-ischemia brain damage in the neonatal rat model. Eur J Pharmacol 667:202–207. doi:10.1016/j.ejphar.2011.06.003
Zhang Z, Zhang L, Jia L, Wang P, Gao Y (2013a) Association of Wnt2 and sFRP4 expression in the third trimester placenta in women with severe preeclampsia. Reprod Sci (Thousand Oaks, Calif) 20:981–989. doi:10.1177/1933719112472740
Zhang Z, Zhang L, Jia L, Wang P, Gao Y (2013b) Association of Wnt2 and sFRP4 expression in the third trimester placenta in women with severe preeclampsia. Reprod Sci. doi:10.1177/1933719112472740
Acknowledgments
This work was supported by Grants from the Science and Technology Fund for Innovative Talents of Henan Province (No. 124200510005), the Key Scientific and Technological Project of Henan Province (No. 112102310089), and the Science and Technology Fund for Innovation Leading Research Team of Zhengzhou City (No. 131PCXTD624).
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Yang, X., Zhang, L. et al. Decreased expression and activation of Stat3 in severe preeclampsia. J Mol Hist 46, 205–219 (2015). https://doi.org/10.1007/s10735-015-9613-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-015-9613-8