Abstract
Recent studies indicate that high mobility group box protein 1 (HMGB1) originating from periodontal ligament (PDL) cells can be a potential regulator in the process of orthodontic tooth movement and periodontal tissue remodeling. The aim of this study is to investigate HMGB1 expression in periodontal tissue during orthodontic tooth movement in mice according to Waldo’s method. Six 7-week-old C57BL6 mice were used in these experiments. The elastic band was inserted into the teeth space between the right first and second maxillary molars. After 3 days of mechanical loading, mice were fixed with transcardial perfusion of 4 % paraformaldehyde in 0.1 M phosphate buffer (pH 7.4), and the maxillary was extracted for histochemical analyses. The histological examination revealed local PDL tear at the tension side and the formation of extensive cell-free hyaline zones at the compression side. The immunolocalization of HMGB1 was significantly presented at tension side of PDL, apical area and dental pulp, whereas at the compression side of PDL, the labeling of HMGB1 was almost undetectable as the presence of hyaline zone. Taken together, we concluded that the orthodontic tooth movement by Waldo’s method leads to histological changes and HMGB1 expression pattern that differ from those of coil spring method, including PDL tear and extensive hyaline zone which may severely destroy periodontal tissue and in turn impede tooth movement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High mobility group box protein 1 (HMGB1), a nonchromosomal nuclear protein, typically released by necrotic cells, also acts as a pro-inflammatory cytokine involved in the regulation of immune response (Andersson et al. 2002; Yang et al. 2002). HMGB1 is a protein with a highly conserved sequence among species and has dual function in cellular metabolism. Within the nucleus, it serves as a regulator of gene transcription through binding DNA, regulating chromosome architecture and inhibiting apoptosis (Lange et al. 2008). While outside the cell, it serves as an alarmin to activate the innate immune response (Wang et al. 1999). HMGB1 can be actively secreted by activated immune cells or passively released by injured/dead cells (Bianchi 2007). In case of these conditions, HMGB1 can be translocated from the cell nucleus to cytoplasm and further to extracellular space, bonds to its specific receptors-receptor for advanced glycation end-products and the toll-like receptors 2 and 4 to trigger inflammatory response and initiate tissue remodeling and repair (Dumitriu et al. 2005; Ulloa and Messmer 2006).
HMGB1 is reported to be expressed in almost all eukaryotic cells including bone cells and involved in ossification, bone remodeling and arthritis pathogenesis (Andersson and Harris 2010; Charoonpatrapong et al. 2006; Yang et al. 2008). In recent papers, HMGB1 has also been found basally expressed in periodontal tissue, e.g. in periodontal ligament (PDL) and alveolar bone, and released by Human PDL cells extracellularly and thus unregulated the expression of various pro-inflammatory and osteoclastogenic cytokines such as IL-1β, IL-6, IL-17, and RANKL by which HMGB1 could modulate alveolar bone resorption, indicating its potential role in regulating biological activity of these tissue (Kim et al. 2010). Several clinical research demonstrated that patients with periodontitis had an increased level of HMGB1 in the gingival fluid compared to the healthy controls which suggested a potential role of HMGB1 in periodontal disease (Feghali et al. 2009; Morimoto et al. 2008).
Side effects such as periodontitis, pulpitis and even root resorption accompany with orthodontic treatment may impede the tooth movement and adversely affect the therapeutic outcome. HMGB1 was shown to participate in the inflammation responses to mechanical force in periodontal tissue of orthodontic tooth movement model of rat (Wolf et al. 2013). To our knowledge, the methods used for establishing tooth movement model comprise the following two: One was described by Waldo and Rothblatt (1954) in which the elastic band was inserted into the space between the first and second maxillary molar to generate a mechanical force (Waldo and Rothblatt 1954). The other was designed following the rise of modern orthodontic technique, in which the mechanical loading pulling the first molar anteriorly was induced by a coil spring anchored to the upper first molar and incisor (Ong et al. 2000; Zhang et al. 2003). The force level generated by the second method is similar to that being applied in clinically orthodontic treatment while the first method generally produce an unstable force, which instantly reaches a climax after being placed and rapidly declines with the anterior movement of the first molar. As the initial force is always overloaded, Waldo’s method prone to induce sterile tissue necrosis in the compression side which is an obstacle to tooth movement and periodontal tissue remodeling. Recently, Wolf et al. (2013) examined the expression pattern of HMGB1 by PDL cells followed by mechanical loading using a coil spring between the first molar and the incisor in a rat tooth movement model and found a time-dependent expression of HMGB1 in both compression side and tension side of PDL. But whether the HMGB1 expression pattern of periodontal tissue in Waldo’s tooth movement model is similar to that of coil spring induced model is still unknown.
In the present study, we addressed the changes in HMGB1 expression by PDL and dental pulp cells in a mouse model of orthodontically induced tooth movement established by Waldo’ method. Furthermore, we investigated two osteoblast-specific factors, alkaline phosphatase (ALP) and Runx2, to explore the relationship between HMGB1 and bone remodeling. We hypothesized that the expression of HMGB1 was unregulated by mechanical force and oxygen deficiency and subsequently the protein was translocated from cell nucleus to extracellular space to initiate tissue remodeling and repair.
Materials and methods
Animal and tissue preparation
All animal experiments in this study were conducted according to the Guidelines for Animal Experimentation of Shandong University. Six 7-week-old C57BL6 mice with an average body weight of 20 g were obtained from Laboratory Animal Centre of Shandong University (Jinan, China).
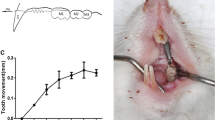
The study was performed after the mice were allowed to acclimate for 1 week. Waldo’s model was used to induce orthodontic tooth movement (Fig. 1). In brief, the elastic band of 0.5 mm thickness and 2 mm width was inserted into the teeth space between the right first and second maxillary molars under anesthesia. The untreated sides were used as control. At 3 days after orthodontic force application, all animals were anesthetized with 8 % chloral hydrate (400 mg/100 g body weight) and fixed with a transcardial perfusion of 4 % paraformaldehyde in 0.1 M phosphate buffer (PH = 7.4). Following the fixation, the maxilla were extracted and immersed in the same fixative for an additional 24 h. Then the samples were decalcified with 10 % EDTA-2Na solution for 2 weeks at 4 °C. After that the samples underwent dehydration through an ascending ethanol series and were embedded in paraffin using standard procedures. 5 μm thickness serial sections were prepared for following histological analysis.
Immunohistochemistry for HMGB1 and double staining for ALPase and TRAPase
After xylene treatment, dewaxed paraffin sections were pretreated with 0.3 % hydrogen peroxide for 30 min at room temperature. Then sections were pre-incubated with 1 % bovine serum albumin in phosphate-buffered saline (BSA-PBS) for 20 min to reduce non-specific staining. The treated sections were incubated for 2 h at room temperature with a rabbit antiserum against ALPase generated by Oda at a dilution of 1:150, or rabbit anti-HMGB1 antibody (Epitmics, Burlingame, USA) at a dilution of 1:100. They were then immersed in horseradish peroxidase (HRP)-conjugated secondary antibodies (DaKo, Glostrup, Denmark) at a dilution of 1:100 for 1 h at room temperature. The immunoreaction was visualized with diaminobenzidine (DAB) (Sigma-Aldrich, St. Louis, MO, USA). After satisfactory immunostaining, the sections treated with PBS and submerged in mixture of 3.0 mg of naphthol AS-BI phosphate, 18 mg of red violet LB salt, and 100 Mm L(+) tartaric acid (0.36 g) diluted in 30 mL of 0.1 M sodium acetate butter (PH 5.0) for 15 min at 37 °C. Staining results were assessed under light microscopy, and all sections were faintly counterstained with methyl green.
Counting of the HMGB1 positive cells
Stained sections were observed and microscopical images were taken with a light microscope (Olympus BX-53, Tokyo, Japan). Randomly chosen images of same size including PDL tissue were captured per specimen at compression and tension sides, pulp, as well as apical areas of distal root of maxillary first molars. The number of immunoreactive cells was counted and calculated with the aid of cell analyzing software image pro plus (Media Cybernetics, Silver Spring, MD, USA). Extracellular immunoreactivity was not analyzed due to difficulties with quantification of such staining results. All operation was performed by the same person with rich experience in interpretation of histological sections. To avoid bias, the cells count was performed automatically by software after defining the corresponding thresholds.
Statistical analysis
All statistical analyses were performed using SPSS software and all values are presented as mean ± standard deviation. Differences among groups were assessed by unpaired t test and considered statistically significant when P < 0.01.
Results
Histology changes of periodontal tissue following orthodontic tooth movement
Following 3 days’ mesial movement of the upper first molar, the width of PDL at the tension side was increased as stretched by the mechanical force compared to control group (Fig. 2b, d). It was noted that the upper part of PDL at the tension side was vertically torn (Fig. 2d). Meanwhile, the PDL at compression side was squeezed and extensive cell-free hyaline zones were visible indicating sterile necrosis caused by excessively compressive force (Fig. 2b, d).
Histological alterations of periodontal tissue following orthodontic force application. a, b HE staining showed an overview of histology of periodontal tissue in control group and tooth movement group, respectively. c, d High-magnification images of the boxed area in (a, b). The width of PDL at the tension side was increased and at compression side was squeezed compared to control group. A cell-free hyaline zone was observed at the compression side. PDL periodontal ligament, D dental, P pulp, Ab alveolar bone, TS tension side, CS compression side. a, b 40×; c, d 100×
Effects of orthodontic tooth movement on osteoblasts and osteoclasts
To investigate the alveolar bone remodeling during orthodontic tooth movement, we performed ALP&TRAP double staining and immunostaining for Runx2, a key transcription factor associated with osteoblast differentiation. The double staining showed that many TRAP positive multinucleate cells were presented at the surface of alveolar bone attached to PDL at the tension side in tooth movement group compared with control group, but there was no osteoclasts observed at the compression side due to the persistence of hyaline zone (Fig. 3a, b). As for ALP staining, no significant differences were detected between two groups (Fig. 3a, b). The immunolocalization of Runx2 was moderately detected in both sides in the untreated PDL (Fig. 3c), but the protein expression was highly increased at the tension side after orthodontic force application (Fig. 3d).
Histochemistry for ALP, TRAP and Runx2. Double staining for ALP and TRAP (a, b), and immunolocalization for Runx2 (c, d). ALP staining showed no significant difference between the two groups. Increased TRAP-positive osteoclasts were found at the tension side instead of at the compression side (b). Compared to control group, intensively stained cells for Runx2 could be seen at the tension side. And there were hardly any visible Runx2 positive cells at the compression side (d). PDL periodontal ligament, d dental, P pulp, Ab alveolar bone, TS tension side, CS compression side. a–d 100×
HMGB1 expression after orthodontic tooth movement
In the untreated group, PDL at both side showed similar basal HMGB1 immunoreactivity and the immunostaining was mainly located at the cell nucleus (Fig. 4a). Following orthodontic tooth movement, HMGB1 expression in the apical area and PDL of tension side was increased significantly compared with the control group, by 4- and 2.5-fold, respectively (Figs. 4b, g, j, 5). However, the immunolabeling for HMGB1 at the compression side was almost invisible as the extensive formation of cell-free hyaline zone compared with the control (Figs. 4b, h, 5). It’s worth noting that the enhanced expression of HMGB1 protein was also observed in dental pulp cells following orthodontic tooth movement, with a threefold increase in the number of HMGB1 positive cells compared to the control group (Figs. 4b, i, 5).
Immunolocalization of HMGB1. a, b Low magnification images in control group and orthodontic tooth movement group. c–f, g–j Higher magnification views of the boxed areas in (a, b). In the control group, PDL at both side showed similar basal HMGB1 expression (c, d). Following orthodontic force application, HMGB1 expression was increased at the tension side (g). Interestingly, there was faint HMGB1 activity at the compression side (h). A typical cell-free hyaline could be found at the compression side (the red dotted box). The immunoreactivity of HMGB1 in the pulp (e) and apical area (f) were faint in the control group while enhanced in orthodontic tooth movement group (i, j). D dental, P pulp, Ab alveolar bone, TS tension side, CS compression side. a, b 40×; c–j 200×. (Color figure online)
Semi-quantitative assessment of HMGB1. Each value represents the mean ± SD for six animals per group. Following orthodontic tooth movement, HMGB1 expression was increased at the tension side, dental pulp and apical area, while highly decreased at the compressive side compared to control group. *P < 0.01. TS tension side, CS compression side, Ap apical area, P pulp
Discussion
Experimental orthodontic tooth movement is typically induced by either elastic band inserted into teeth space or coil spring attached to the targeted tooth. Different loading ways derived from above mentioned methods are always followed by diverse histological changes of periodontal tissue. In this study, our results demonstrated that HMGB1 expression in periodontal tissue is modulated by orthodontic tooth movement and the changes of expression pattern of HMGB1 induced by Waldo’s method differ from those triggered by coil spring method described by Wolf et al. (2013), with the enhanced immunolocalization for HMGB1 presented in the tension side of PDL, apical tissue and dental pulp while absent in the compression side of PDL as the formation and maintenance of cell-free hyaline zones.
Orthodontic tooth movement takes place as a result of bone remodeling of alveolar bone around tooth roots including bone resorption at the compression side and bone apposition at the tension side (Chang et al. 2012). In tooth movement group, bone remodeling process at the tension side was activated by the stretched PDL and many osteoclasts were present at the bone surface to act as old bone remover to initiate following bone regeneration. Although ALP expression was not significantly increased after tooth movement for 3 days, a master regulator of osteogenesis-Runx2 was elevated at the tension side, indicating a great osteogenic potential of the alveolar bone at this side (Fujita et al. 2004; Hoeppner et al. 2009; Zhang et al. 2011). The present of hyaline zone is an obstacle to the remodeling of soft and hard tissue and impedes further tooth movement (Kohno et al. 2002). Only the hyalinized tissue at the compression side be eliminated by macrophages can osteoclasts be recruited and formed here to perform bone resorption which makes further orthodontic tooth movement possible (Kurol and Owman-Moll 1998). Otherwise, further tooth movement would be obstructed if the secretion of matrix degradation-associated enzymes such as cathepsin K, MMP1 and MMP2 by macrophages or osteoclasts is disturbed, just as reported by our previous study (Lv et al. 2014).
In the tension side, PDL cells showed strong immunolabeling for HMGB1 after the application of orthodontic force which was accordance with previous report (Wolf et al. 2013). However, the periodontal tissue destructions including tear of upper PDL, attachment loss and serious periodontal inflammation were also observed in this side which were resulted from the elastic band slipped into gingival sulcus during inserting operation or chewing. The elastic band mechanically damaged the PDL while facilitating the stick of bacteria plaque to local tissue and therefore aggravated periodontal inflammation. As previously reported, periodontitis was correlated to expression and release of HMGB1 by PDL (Feghali et al. 2009). Consequently, the unregulated expression of HMGB1 was attributed to both the applied force and the local mechanical/biological invasion which in some case even leaded to the loss of tooth.
Interestingly, the compression side of PDL was almost replaced by cell-free hyaline zones except for a few residual cells and exhibited negative for HMGB1. In this point, our results were contrary to that of Wolf’s which showed stronger effect of orthodontic treatment on HMGB1 expression at compression side compared to tension side (Wolf et al. 2013). In a systematic review of the literature on hyalinization in relation to experimental tooth movement in rat/mouse, the applied forces ranging from 0.012 to 0.50 N induced the first appearance of hyalinization within as early as the first 24 h and lasted for 1–34 days. In vitro studies showed that a static compressive force of 4 g/cm2 applied to human PDL cells for 8 h induced apparent translocation of HMGB1 from the nucleus to the cytoplasm (Wolf et al. 2013). Therefore, it is possible that HMGB1 protein translocation had been taken place within the first minutes/hours of force application before the hyalinization process occurred. However, the exact information about the amount of time required to complete the release of HMGB1 in PDL cells in response to mechanical force is limited. Furthermore, considering the complex biological environments in vivo especially blood supply by which oxygen and nutrients are transported, could be obstructed in the condition of over-compression (Franzen et al. 2013), it is hence difficult to judge whether the cells had been dead before HMGB1 could be expressed and released to extracellular space or most of HMGB1 expression/translocation had already happened with the first minutes/hours of force application before the hyalinization process occurred. Therefore, much earlier time points, maybe on accuracy of hours after application would be of interest to future investigations to ascertain what really happened on PDL cells. Furthermore, the mechanical force delivered by coil spring was set to 0.5 N in wolf’s experimental tooth movement model of rat and they reported the formation of cell-free hyaline zone at the compression side with a mount of compressed PDL cells expressing increased HMGB1. Yet, no study has been found to quantify the amount of force generated by Waldo’s method since the presence of various interference factors including the size and component of elastic band as well as species used. However it seems that the extent and area of hyaline zone induced by Waldo’s method in our experiment is much larger than that of coil spring method. Base on this result, it can be hypothesized that the mount of mechanical force delivered by inserted elastic band is greater than 0.5 N, at least at initial phase. But the accurate mount of force generated by elastic band over time during tooth movement is still need to be further investigated to precisely evaluate its effect on local periodontal tissue.
The mechanical force used to induce orthodontic tooth movement may lead to transient pulpitis as a result of serious inflammatory response such as circulatory disturbances (Mostafa et al. 1991), depression of the tissue respiration rate (Hamersky et al. 1980), apoptosis (Rana et al. 2001) and edema (Taspinar et al. 2003). Especially, anoxic conditions of dental pulp was induced by decreased blood flow following mechanical loading (Sano et al. 2002). HMGB1 is also reported to be secreted by somatic cells, including pituicyte, enterocytes and hepatocytes, under hypoxic condition (Klune et al. 2008). It is therefore reasonable to speculate that hypoxia in dental pulp could induce the cytoplasmic expression and release of HMGB1, initiating the immune response. Recent study has confirmed the expression of HMGB1 and its receptor RAGE in adult dental pulp fibroblasts (Sugars et al. 2007) and the cytoplasmic expression of HMGB1 as well as increased mRNA expression of HMGB1 and RAGE were also observed in inflamed pulp tissues compared to that in healthy dental pulp (Zhang et al. 2014). Taken together, our results that showed the increased expression of HMGB1 in dental pulp fibroblasts are consistent with the inflammatory status during orthodontic tooth movement and previous reports.
In summary, our results show that the expression pattern of HMGB1 at periodontal tissue following orthodontic tooth movement induced by Waldo’s method exhibited some unique features compared with that induced by coil spring method, involving additional expression in apical area and dental pulp as well as the undetectable expression at the compression side due to the hyaline zone. Furthermore, the way of loading and uncertain magnitude of force generated by the squeezed elastic band leaded to overt and extensive hyaline zone formation at the compression side and severe PDL injury at the tension side which could impede tooth movement process and result in unfavorable side effects such as pulpitis and periodontitis (Fig. 6). Overall, the method introduced by Waldo is not a satisfying approach to induce smooth orthodontic tooth movement.
A schema to illustrate potential functions of HMGB1 in periodontal tissue remodeling during orthodontic tooth movement. At the condition of mechanical stress or anoxia stimulation, HMGB1 would translocate from the nucleus of periodontal ligament cells to the cytoplasm, further into the extracellular environment. Then the extracellular HMGB1 binds to its receptors expressed on the preosteoblasts, osteoclast precursors and monocytes to induce the differentiation of osteoblasts, osteoclasts and macrophages for the following periodontal tissue remodeling
References
Andersson U, Harris HE (2010) The role of HMGB1 in the pathogenesis of rheumatic disease. Biochim Biophys Acta 1799:141–148. doi:10.1016/j.bbagrm.2009.11.003
Andersson U, Erlandsson-Harris H, Yang H, Tracey KJ (2002) HMGB1 as a DNA-binding cytokine. J Leukoc Biol 72:1084–1091
Bianchi ME (2007) DAMPs, PAMPs and alarmins: all we need to know about danger. J leukoc Biol 81:1–5. doi:10.1189/jlb.0306164
Chang HW, Huang HL, Yu JH, Hsu JT, Li YF, Wu YF (2012) Effects of orthodontic tooth movement on alveolar bone density. Clin Oral Investig 16:679–688. doi:10.1007/s00784-011-0552-9
Charoonpatrapong K et al (2006) HMGB1 expression and release by bone cells. J Cell Physiol 207:480–490. doi:10.1002/jcp.20577
Dumitriu IE et al (2005) Release of high mobility group box 1 by dendritic cells controls T cell activation via the receptor for advanced glycation end products. J Immunol 174:7506–7515
Feghali K, Iwasaki K, Tanaka K, Komaki M, Machigashira M, Ishikawa I, Izumi Y (2009) Human gingival fibroblasts release high-mobility group box-1 protein through active and passive pathways. Oral Microbiol Immunol 24:292–298. doi:10.1111/j.1399-302X.2009.00508.x
Franzen TJ, Brudvik P, Vandevska-Radunovic V (2013) Periodontal tissue reaction during orthodontic relapse in rat molars. Eur J Orthod 35:152–159. doi:10.1093/ejo/cjr127
Fujita T et al (2004) Runx2 induces osteoblast and chondrocyte differentiation and enhances their migration by coupling with PI3K-Akt signaling. J Cell Biol 166:85–95. doi:10.1083/jcb.200401138
Hamersky PA, Weimer AD, Taintor JF (1980) The effect of orthodontic force application on the pulpal tissue respiration rate in the human premolar. Am J Orthod 77:368–378
Hoeppner LH, Secreto F, Jensen ED, Li X, Kahler RA, Westendorf JJ (2009) Runx2 and bone morphogenic protein 2 regulate the expression of an alternative Lef1 transcript during osteoblast maturation. J Cell Physiol 221:480–489. doi:10.1002/jcp.21879
Kim YS, Lee YM, Park JS, Lee SK, Kim EC (2010) SIRT1 modulates high-mobility group box 1-induced osteoclastogenic cytokines in human periodontal ligament cells. J Cell Biochem 111:1310–1320. doi:10.1002/jcb.22858
Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A (2008) HMGB1: endogenous danger signaling. Mol Med 14:476–484. doi:10.2119/2008-00034.Klune
Kohno T, Matsumoto Y, Kanno Z, Warita H, Soma K (2002) Experimental tooth movement under light orthodontic forces: rates of tooth movement and changes of the periodontium. J Orthod 29:129–135
Kurol J, Owman-Moll P (1998) Hyalinization and root resorption during early orthodontic tooth movement in adolescents. Angle Orthod 68:161–165. doi:10.1043/0003-3219(1998)068<0161:HARRDE>2.3.CO;2
Lange SS, Mitchell DL, Vasquez KM (2008) High mobility group protein B1 enhances DNA repair and chromatin modification after DNA damage. Proc Natl Acad Sci USA 105:10320–10325. doi:10.1073/pnas.0803181105
Lv S et al (2014) Histochemical examination of cathepsin K, MMP1 and MMP2 in compressed periodontal ligament during orthodontic tooth movement in periostin deficient mice. J Mol Histol 45:303–309. doi:10.1007/s10735-013-9548-x
Morimoto Y et al (2008) Tumor necrosis factor-alpha stimulates gingival epithelial cells to release high mobility-group box 1. J Periodontal Res 43:76–83. doi:10.1111/j.1600-0765.2007.00996.x
Mostafa YA, Iskander KG, El-Mangoury NH (1991) Iatrogenic pulpal reactions to orthodontic extrusion. Am J Orthod Dentofacial Orthop 99:30–34. doi:10.1016/S0889-5406(05)81677-4
Ong CK, Walsh LJ, Harbrow D, Taverne AA, Symons AL (2000) Orthodontic tooth movement in the prednisolone-treated rat. Angle Orthod 70:118–125. doi:10.1043/0003-3219(2000)070<0118:OTMITP>2.0.CO;2
Rana MW, Pothisiri V, Killiany DM, Xu XM (2001) Detection of apoptosis during orthodontic tooth movement in rats. Am J Orthod Dentofacial Orthop 119:516–521. doi:10.1067/mod.2001.113654
Sano Y, Ikawa M, Sugawara J, Horiuchi H, Mitani H (2002) The effect of continuous intrusive force on human pulpal blood flow. Eur J Orthod 24:159–166
Sugars R, Karlstrom E, Christersson C, Olsson ML, Wendel M, Fried K (2007) Expression of HMGB1 during tooth development. Cell Tissue Res 327:511–519. doi:10.1007/s00441-006-0293-2
Taspinar F, Akgul N, Simsek G, Ozdabak N, Gundogdu C (2003) The histopathological investigation of pulpal tissue following heavy orthopaedic forces produced by rapid maxillary expansion. J Int Med Res 31:197–201
Ulloa L, Messmer D (2006) High-mobility group box 1 (HMGB1) protein: friend and foe. Cytokine Growth Factor Rev 17:189–201. doi:10.1016/j.cytogfr.2006.01.003
Waldo CM, Rothblatt JM (1954) Histologic response to tooth movement in the laboratory rat; procedure and preliminary observations. J Dent Res 33:481–486
Wang H et al (1999) HMG-1 as a late mediator of endotoxin lethality in mice. Science 285:248–251
Wolf M, Lossdorfer S, Kupper K, Jager A (2013) Regulation of high mobility group box protein 1 expression following mechanical loading by orthodontic forces in vitro and in vivo. Eur J Orthod. doi:10.1093/ejo/cjt037
Yang H, Wang H, Czura CJ, Tracey KJ (2002) HMGB1 as a cytokine and therapeutic target. J Endotoxin Res 8:469–472. doi:10.1179/096805102125001091
Yang J, Shah R, Robling AG, Templeton E, Yang H, Tracey KJ, Bidwell JP (2008) HMGB1 is a bone-active cytokine. J Cell Physiol 214:730–739. doi:10.1002/jcp.21268
Zhang D, Goetz W, Braumann B, Bourauel C, Jaeger A (2003) Effect of soluble receptors to interleukin-1 and tumor necrosis factor alpha on experimentally induced root resorption in rats. J Periodontal Res 38:324–332
Zhang Y, Su J, Yu J, Bu X, Ren T, Liu X, Yao L (2011) An essential role of discoidin domain receptor 2 (DDR2) in osteoblast differentiation and chondrocyte maturation via modulation of Runx2 activation. J Bone Miner Res 26:604–617. doi:10.1002/jbmr.225
Zhang X, Jiang H, Gong Q, Fan C, Huang Y, Ling J (2014) Expression of high mobility group box 1 in inflamed dental pulp and its chemotactic effect on dental pulp cells. Biochem Biophys Res Commun 450:1547–1552. doi:10.1016/j.bbrc.2014.07.027
Acknowledgments
This study was partially supported by the National Nature Science Foundation of China (Nos. 81271965; 81470719; 81311140173) and Specialized Research Fund for the Doctoral Program of Higher Education (No. 20120131110073) to Li M.
Conflict of interest
The authors have no competing financial interests to disclose in relation to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Shengyu Lv and Juan Li have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Lv, S., Li, J., Feng, W. et al. Expression of HMGB1 in the periodontal tissue subjected to orthodontic force application by Waldo’s method in mice. J Mol Hist 46, 107–114 (2015). https://doi.org/10.1007/s10735-014-9606-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-014-9606-z