Abstract
This paper presents a multi-product multi-period stochastic program for an integrated blood supply chain that considers red blood cells and platelets while accounting for multi-product interactions, demand uncertainty, blood age information, blood type substitution, and three types of patients. The aim is to minimize the total cost incurred during the collection, production, inventory, and distribution echelons under centralized control. The supply chains for red blood cells and platelets intertwine at the collection and production echelons as collected whole blood can be separated into red blood cells and platelets at the same time. By adapting to a real-world blood supply chain with one blood center, three collection facilities, and five hospitals, we found a cost advantage of the multi-product model over an uncoordinated model where the red blood cell and platelet supply chains are considered separately. Further sensitivity analyses indicated that the cost savings of the multi-product model mainly come from variations in the number of whole blood donors. These findings suggest that healthcare managers are able to see tremendous improvement in cost efficiency by considering red blood cell and platelet supply chains as a whole, especially with more whole blood donations and a higher percentage of whole blood derived platelets pooled for transfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
A multi-product stochastic program for an integrated blood supply chain is presented.
-
Multi-product interactions, demand uncertainty, and platelet pooling are considered.
-
The multi-product model performs better than the uncoordinated RBC and PLT single product models.
-
Cost savings mainly come from variations in the number of whole blood donors.
-
Increasing the use of pooled platelets can reduce cost and wastage.
1 Introduction
Blood is an unmanufacturable and irreplaceable product that is necessary for surgeries and treatment of patients suffering from illnesses and accidents [38]. There are more than 4000 different kinds of components contained in blood. Of all these blood components, the three most important are red blood cells (RBC), platelets (PLT), and plasma (PLS). According to American Red Cross [6], daily demands for RBCs, PLTs, and PLS are approximately 36,000, 7000, and 10,000 units respectively in the United States. RBCs are the most abundant cell type and can be stored for up to 42 days after collection [5]. Although demand of PLTs only accounts for around 1/5 of RBCs, they play an important role in organ transplants, bone marrow transplants, cancer treatment, and general surgeries. PLTs are the most perishable blood product and have a shelf life of 5 days [5]. Unlike RBCs and PLTs, PLS is not a perishable product and can be stored for nearly 1 year [5]. Despite the importance of blood products, blood is a scarce resource and can only come from human donations. These features add the difficulty to optimize the blood supply chain especially for perishable blood products in terms of balancing wastage and shortage. As an unperishable product, handling the operational process of PLS is significantly less complex than RBCs and PLTs. Therefore, this research only focuses on optimizing the supply chain management of RBCs and PLTs in the US.
Generally, the blood supply chain is divided into four echelons: collection, production, inventory, and distribution. There are several similarities and differences between the RBC and PLT supply chains for each echelon. Both supply chains start with blood collection from donors. There are two ways of collecting RBCs or PLTs: through whole blood or apheresis. Whole blood donation is the most common donation type. One whole blood donation can produce one transfusable unit of RBC and 1/5 transfusable unit of PLT. While one apheresis donation can contribute two transfusable units of RBCs or up to three transfusable units of PLTs [7]. Here, a transfusable unit indicates a therapeutic adult dose for blood transfusion. Whole blood is usually collected by bloodmobiles. Then, it will be transported to a local blood center where whole blood is processed to extract RBCs and PLTs. However, in the US, whole blood is mainly used for producing RBCs, and the PLT components extracted from whole blood at the same time could exceed that needed for transfusions, as the demand for RBCs is much larger than PLTs. According to the AABB and National Blood Collection and Utilization surveys, in the US only around 13% of PLT transfusions use whole blood derived PLTs [10] with each transfusable unit of PLT requiring pooling of whole blood derived PLTs from 4 to 6 different donors. Pooling PLTs from different donors could increase the risk of infections; however, proper testing procedures should be able to avoid this. RBCs and PLTs are also collected by apheresis at blood centers and hospitals. Bloodmobiles can also collect apheresis derived RBCs, but are not capable to collect apheresis derived PLTs. Collected whole blood, RBCs, and PLTs need to be tested to ensure free from hepatitis viruses, HIV, and other infectious diseases that can be transmitted through blood transfusion. Once negative testing results are obtained, RBCs and PLTs, either derived from whole blood or apheresis, are appropriate for use and will be allocated to inventories at blood centers or hospitals. RBCs need to be stored in refrigerators at a temperature between 2 to 6 °C. In contrast, PLTs can be kept at room temperature but need to be agitated constantly to avoid clumping. These blood products, if stored at blood centers, are then distributed to hospitals to fulfill orders. Before transfusion at hospitals, blood compatibility between the donor and the patient needs to be determined. This process is called crossmatching.
For RBCs, it is necessary to consider crossmatching of blood types between donors and patients before transfusion as not all blood types are compatible. There are eight main blood types: A, B, AB, and O, each of which can be rhesus positive or negative. Table 1 shows the compatibility chart for substitution of blood types for RBCs [15]. As illustrated in Table 1, a person with blood type AB+ is a universal recipient who can receive blood from donors with any blood type. In an analogous fashion, a person with blood type O- is known as a universal donor. But for PLTs, while transfusing the same ABO type as the patient is the first choice, any ABO and rhesus type is possible. However, PLT demand can be classified into three types based on patients’ needs as shown in Table 2 [18]. Fresh, young, and old PLTs are defined as PLTs with an age of one day old, two to three days old, and four to five days, respectively. Fresh PLTs are needed for organ or bone marrow transplantation. Fresh or young PLTs are needed for oncology and hematology cases or cancer treatment. Other patients can use fresh, young, or old PLTs.
Most literature regarding blood supply chain management considers a single blood product such as RBCs or PLTs, we are unaware of any study that discusses a multi-product blood supply chain that considers whole blood production and apheresis production at the same time. According to Barbee [9], in 2011 donation of whole blood was approximately 13,744,000 units, in addition, nearly 1,978,000 units of RBCs and 2,516,000 units of PLTs were collected by apheresis. As an important source of blood supply, whole blood donation has great effects on both the RBC and PLT supply chains. Therefore, it is necessary to consider multiple products for accurate modeling of the supply of the blood supply chain so as to reduce the wastage of whole blood derived PLTs in the US.
Is it possible to develop a comprehensive model that comprises both the RBC and PLT supply chains, their operational processes, and connections? If it is possible, does this multi-product model perform better than an uncoordinated model where the RBC and PLT supply chains are considered separately? If it does, what are the drivers of the difference?
To answer these questions, this paper presents a novel multi-product multi-period stochastic program for a four-echelon blood supply chain that considers RBCs and PLTs while accounting for blood type substitution and three types of patients. The objective of the proposed model is to minimize total costs, including production, transportation, inventory, and wastage costs, under a centralized control system where any decision regarding production and allocation is made with a system-wide perspective. By adapting our model to a real-world case study from the Fargo-Moorhead area, North Dakota and Minnesota, USA, we found the cost advantage of a multi-product blood supply chain over an uncoordinated model where the RBC and PLT supply chains are considered separately. Further sensitivity analyses on exploring the impacts of donors and pooling percentage on system performance indicated that cost savings of the multi-product model mainly come from variations in the number of whole donors and a higher pooling percentage for whole blood derived PLTs.
2 Literature Review
There is a wealth of literature on the blood supply chain especially in recent years. Beliën and Forcé [11] and Osorio et al. [30] summarized relevant articles from 1966 to 2010 and 2014, respectively. The newest literature review of the blood supply chain was presented by Pirabán et al. [33]. Pirabán et al. [33] classified existing literature published between 2005 and February 2019 based on a new taxonomy including decision making and forecasting environments, network structure, blood products, operational processes, type of problem/planning decisions, modeling techniques, and data characteristics. Several important characteristics of the blood supply chain have been highlighted by Pirabán et al. [33] and considered by the existing literature, such as demand uncertainty[17], blood type compatibility/ABO-substitution for RBCs [22], and age-dependent demand for PLTs [20]. Pirabán et al. [33] also identified some gaps and potential directions in the blood supply chain. These gaps include consideration of multiple blood products, choosing collection methods (apheresis and whole blood donation), and multiple echelons that comprise the blood supply chain. Our research fills these gaps and considers these identified characteristics of the blood supply chain. In the following parts, we present the relevant literature on the RBC and PLT supply chains respectively, as well as the multi-product blood supply chain.
RBCs are the mostly demanded blood components. A considerable amount of research has been dedicated to the RBC supply chain [1, 21, 23, 26, 37]. However, all of these studies ignored the important characteristic of blood type compatibility for RBCs which makes them less applicable as not all blood collected is suitable to be transfused to patients with a certain blood type. Most recent works consider blood type compatibility and substitution when formulating models for RBCs [15, 17, 25, 29]. Dillon et al. [15] introduced a two-stage stochastic program for RBC inventory management that focused on minimizing operational costs, as well as blood shortage and wastage. However, this paper focused only on a single echelon which is inventory. It would be better to consider the multiple echelons of the blood supply chain so as to manage coordination and cooperation among different echelons to avoid myopic view and the bullwhip effect. Hamdan and Diabat [25] presented a mathematical model for an integrated RBC supply chain that seeks to minimize total system cost, processing and transportation time, and number of outdated units. The model accounts for blood type substitution, product perishability, stochastic supply, and stochastic demand. Though this research considered perishability of RBCs, it didn’t provide age information of RBCs in the inventory. Another limitation is that only whole blood donation was considered as a source of supply for RBCs without considering apheresis donation. Hamdan and Diabat [25] provides a good reference for us when developing our model to include the ABO substitution characteristic of RBCs, though we take age information and two sources of supply into account.
Compared to RBCs, PLTs are much more perishable as they have a very short shelf life. Most recent studies consider age-based PLT supply chains or inventory models [2, 16, 34, 35]. Besides much shorter shelf life, another important difference of PLTs compared to RBCs is age-dependent demand as certain types of patients may require certain ages of PLTs [13]. This characteristic has been addressed by several papers working on PLT supply chain [18, 19, 23, 24, 36]. Gunpinar and Centeno [23] developed a stochastic integer program for a two-level supply chain consisting of one blood center and one hospital that explicitly accounts for the age of blood units, demand for two types of patients, and demand uncertainty. On the basis of Gunpinar and Centeno [23], Ensafian and Yaghoubi [18] enlarged the PLT supply chain both horizontally and vertically by considering four echelons including collection, production, inventory, and distribution with 18 collection facilities, one blood center, and 10 hospitals. They considered two collection approaches of PLTs and three different types of patients. Our consideration of two sources of supply and three types of demand are mainly derived from the above two articles.
After examining the literature on the RBC and PLT supply chains respectively, let’s focus on the multi-product supply chain. Although research regarding multi-product supply chains for nonperishable items is common [3, 27, 28], there is little work that addresses perishable products. The first study that considered multiple perishable products was Deuermeyer and Pierskalla [14]. They considered a new system with two products and two production processes where one of the production processes was capable to produce both products. This is exactly what we saw in the blood supply chain in which whole blood donation can generate both RBCs and PLTs while apheresis donation can generate either RBCs or PLTs. There is very limited research in the blood supply chain that considers multiple products. Arvan et al. [8] presented an integrated supply chain that includes donation sites, testing and processing labs, blood banks, and demand points. Four blood products were considered in the proposed model: whole blood, RBCs, PLS, and PLTs. The goals were minimizing the total operational cost and the total time that blood products remain in the network before being consumed. However, this model didn’t account for apheresis donation as well as shortages and outdates of blood products. Osorio et al. [31] presented a combination of an integrated simulation-based model and an integer linear optimization model focusing on the collection and production echelons that account for blood type substitution and perishability. This study considered four blood products: RBCs, PLS, PLTs, and cryoprecipitate, and five production processes: whole blood fractionation using triplex bag, quadruple bag A, and quadruple bag B respectively, and apheresis production for RBCs and PLTs. However, the proposed optimization model was limited to the collection and production stages and the age information of products in the inventory was unknown. Zahiri and Pishvaee [39] formulated a novel multi-period location allocation problem for a blood supply chain that focused on minimizing total costs and unmet demand. This research considered multiple blood products, which are RBCs, PLTs, and PLS. In addition, blood type substitution for RBCs and PLS were taken into account. However, the model didn’t consider the time spent on inventory at the main center for blood products when talking about perishing, which limits its usefulness. None of these articles consider the multiple production processes including whole blood separation and apheresis production in a multi-product blood supply chain. As both RBCs and PLTs can be produced through whole blood and apheresis, and whole blood separation can generate both blood products, it is necessary to consider a multi-product blood supply chain that coordinates different types of production processes and maintains an appropriate inventory level.
In this study, we formulate a multi-product multi-period stochastic program for an integrated blood supply chain that accounts for demand uncertainty, blood type substitution for RBCs, and age-dependent demand for PLTs. The aim is to provide tactical and operational decisions on blood collection, production, and allocation and explore the benefits of a coordinated multi-product model on performance improvement. Our study contributes to the literature in two ways. First, we present the first multi-product stochastic program for an integrated blood supply chain that considers the coordination of different types of blood production processes. Considering the common supply of RBCs and PLTs through whole blood separation, it is realistic to consider a multi-product model in the blood supply chain. This paper enriches the limited literature in the blood supply chain that considers multiple products, multiple echelons, and multiple collection methods. Second, we investigate the benefits of the multi-product model on reducing total cost and shortage by comparing it to an uncoordinated model where the RBC and PLT supply chains are considered separately.
3 Problem Description
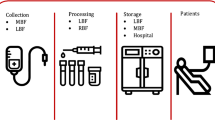
In this study, we investigate a centralized blood supply chain system with multiple perishable products within multiple periods considering one regional blood center, several blood collection facilities, and hospitals. The aim is to minimize the total cost incurred in the collection, production, inventory, and distribution echelons. As a multi-product system, two supply chains are considered: the RBC supply chain and the PLT supply chain. The two supply chains intertwine at the collection and production echelons through whole blood donation and separation.
3.1 Problem Description
The structure of the blood supply chain is depicted in Fig. 1. There are three types of facilities considered: bloodmobiles, the blood center, and hospitals. All of these facilities can be used for collecting blood, but bloodmobiles can only collect whole blood and apheresis derived RBCs, and the blood center and hospitals mainly collect apheresis derived RBCs and PLTs. Blood units collected through bloodmobiles are then transported to the blood center and separated into RBCs and PLTs. Thus, the inventory of whole blood is considered to be zero. After performing bacterial testing, suitable blood products are either put into inventory or distributed to different hospitals. Three types of patients are taken into account for PLTs and blood type crossmatching and substitution are considered for RBCs.
Within the multi-period supply chain, the demand for both blood products differs day by day, as does the production schedule at the blood center. Each hospital orders each blood product based on estimated demand and remaining inventory before the start of each day. At the beginning of each day, the blood center distributes ordered blood products to different hospitals, then updates its current inventory by adding newly collected or produced units and removing any expired units as well as units that have been distributed, and finally making a new production plan based on remaining inventory and estimated total orders from the hospitals. On the other hand, hospitals receive different blood products with different age distributions from the blood center. These received units together with the units stored at the inventory of each hospital are used for satisfying different types of demand. Since demand for RBCs and PLTs fluctuates day by day and is unknown when operational decisions are made, it is necessary to address the issue of demand uncertainty. According to Birge and Louveaux [12], stochastic programming is a useful and popular approach to deal with uncertainty. Therefore, a multi-period stochastic program is applied to the blood supply chain. For each day, the supply of whole blood and apheresis derived blood products is decided prior to the realization of uncertainty, while other decisions including production, distribution, and inventory are made without knowing the specific demand for each product. Table 3 shows the sequence of daily events at the blood center and hospitals.
According to the above description, the main assumptions of the blood supply chain are:
-
It takes two days to process and test whole blood units [18], while only one day is needed for performing bacterial tests on apheresis derived blood products. This later assumption is based on conversations with a manager at a local blood center.
-
Demand for RBCs is much larger than demand for PLTs [6]. Therefore, to satisfy demand for RBCs, a large amount of whole blood units will be collected as an important source of supply. We assume that all the PLTs produced in the whole blood collection will be pooled and utilized for transfusion.
-
Lead time for transportation between any two facilities is zero and does not influence the age of transported blood units. As we are considering a blood supply chain in a local area, the geographic distance between the collection sites and the blood center or between the blood center and hospitals is relatively small.
-
Shortage is not allowed for both RBCs and PLTs. This indicates that the blood supply is sufficient to fulfill the demand of the blood supply chain. Generally, blood donated by voluntary unpaid donors is enough to maintain daily blood demand under non-disaster situations. But if unexpected sudden demand occurs for a short time period, like a serious car accident, blood centers and hospitals can pay some money to recruit donors or encourage family/friend donors to avoid blood shortage.
3.2 Two-stage stochastic programming approach
The demand for RBCs and PLTs at hospitals is not fixed and may change day to day, so demand uncertainty must be taken into consideration. Birge and Louveaux [12] pointed out that stochastic programming is a popular approach in dealing with uncertainty in modeling problems.
This paper presents a scenario-based two-stage stochastic program to account for demand uncertainty for the multi-product blood supply chain. In the two-stage framework, decision variables are categorized as first stage and second stage variables. The first-stage decisions, also called “here-and-now” decisions, are independent of scenarios and are made before revealing uncertainty. In our study, the first-stage decisions include the collection and production of whole blood and apheresis derived RBCs and PLTs at different collection facilities, the blood center, and hospitals. The second-stage decisions, also referred as “wait-and-see” decisions, are scenario-dependent and are determined to account for changes after the realization of uncertainty. The second stage decisions are those referring to the daily operation of the blood center and hospitals, specifically, the distribution, inventory, demand fulfillment, and wastage.
4 Mathematical Formulation
4.1 Model notation
The complete notation for the multi-product supply chain model is summarized as follows.
Sets | |
N | Age of blood products, n ∈ N |
K | Demand type for blood products, k ∈ K |
I | Hospitals, i ∈ I |
J | Blood collection facilities, j ∈ J |
T | Time periods, t ∈ T |
E | Blood types, α, α′ ∈ E |
Γ | Different blood product types, σ ∈ Γ |
Ξ | Scenarios, ε ∈ Ξ |
Parameters | |
γ | Fraction of valid whole blood units used for separation process |
βσ | Quantity of blood product type σ obtained from one apheresis donation |
gσ | Quantity of blood product type σ obtained from one whole blood separation |
Nσ | Lifetime of blood product σ |
Wjtα | Number of whole blood donors with blood type α at collection facility j on day t |
Xjtασ | Number of apheresis donors with blood type α for blood product σ at collection facility j on day t, σ = RBC |
Xitασ | Number of apheresis donors with blood type α for blood product σ at hospital i on day t |
X0tασ | Number of apheresis donors with blood type α for blood product σ at the blood center on day t |
F | Fixed cost of producing blood components from whole blood at the blood center |
V | Operation cost per unit of whole blood separation at the blood center |
L | Procurement cost per unit of whole blood |
Y | Pooling cost per transfusable unit of PLTs derived from whole blood |
pσ | Apheresis production cost per unit of blood product σ |
hσ | Unit holding cost of blood product σ per day |
Gj | Unit transportation cost from blood collection facility j to the blood center |
Hi | Unit transportation cost from the blood center to hospital i |
vσ | Wastage cost per unit of blood product σ |
ditkασε | Patient demand of type k and blood type α for blood product σ at hospital i on day t under scenario ε |
Dkσ | Set of ages for blood product σ associated with demand type k |
\({\pi}_{\alpha {\alpha}^{\prime }}\) | 1 if the demand for blood type α can be alternatively fulfilled with blood type α′, 0 otherwise |
Ciσ | Capacity of blood product σ at hospital i |
C0σ | Capacity of blood product σ at the blood center |
\({C}_{i\sigma}^{Initial}\) | Upper bound for initial inventory of blood product σ at hospital i |
w | Percentage of whole blood derived PLTs used for pooling |
uσ | Maximum percentage of apheresis donation for blood product σ |
Pε | Probability of scenario ε |
Variables | |
Aitασ | Quantity of apheresis donation for blood product σ with blood type α at hospital i on day t |
A0tασ | Quantity of apheresis donation for blood product σ with blood type α at the blood center on day t |
Ajtασ | Quantity of apheresis donation for blood product σ with blood type α at collection facility j on day t, σ = RBC |
Bjtα | Quantity of whole blood donation with blood type α at collection facility j on day t |
Qtασ | Quantity of blood product σ with blood type α produced from whole blood at the blood center on day t |
Iitnασε | Quantity of blood product σ aged n with blood type α in the inventory of hospital i at the beginning of day t under scenario ε |
I0tnασε | Quantity of blood product σ aged n with blood type α in the inventory of the blood center at the beginning of day t under scenario ε |
Ritnασε | Quantity of blood product σ aged n with blood type α shipped to hospital i on day t under scenario ε |
Oitσε | Outdated quantity of blood product σ at hospital i on day t under scenario ε |
O0tσε | Outdated quantity of blood product σ at the blood center on day t under scenario ε |
\({U}_{itn\alpha {\alpha}^{\prime}\sigma \varepsilon}\) | Quantity of blood product σ aged n with blood type α′ in the inventory of hospital i used to satisfy demand of blood type α on day t under scenario ε, \(\forall i,t,n,\sigma, {\pi}_{\alpha {\alpha}^{\prime }}=1\) |
Zt | 1 if blood products are produced from whole blood at the blood center on day t, 0 otherwise |
4.2 Mathematical model
Based on the defined parameters and variables, a multi-stage multi-product stochastic model is formulated. The objective is to minimize the expected total operational cost of the multi-product blood supply chain across all scenarios. This cost comprises of 15 cost components in the multi-stage blood supply chain:
-
Production costs on day t:
Whole blood procurement cost with blood type α at collection facility j: L ∗ Bjtα
Fixed production cost of blood products derived from whole blood: F ∗ Zt
Variable whole blood production cost with blood type α: \(V\ast {\sum}_{j=1}^J{B}_{jt\alpha}\ast \gamma\)
Pooling cost of whole blood derived PLTs with blood type α: Y ∗ w ∗ Qtασ, σ = PLT
Apheresis production cost of product σ with type α at the blood center: pσ ∗ A0tασ ∗ βσ
Apheresis production cost of product σ with type α at hospital i: pσ ∗ Aitασ ∗ βσ
Apheresis production cost of product σ with type α at collection facility j: pσ ∗ Ajtασ ∗ βσ
-
Transportation costs on day t:
Transportation cost from collection facility j to the blood center for blood type α: Gj ∗ (Bjtα + ∑σAjtασ ∗ βσ)
Transportation cost from the blood center to hospital i for product σ aged n with type α under scenario ε: Pε ∗ Hi ∗ Ritnασε
-
Inventory holding costs on day t under scenario ε:
Holding cost of product σ aged n with type α at hospital i: Pε ∗ hσ ∗ Iitnασε
Holding cost of product σ aged n with type α at the blood center: Pε ∗ hσ ∗ I0tnασε
-
Wastage costs on day t under scenario ε:
Wastage cost of discarded whole blood derived PLTs with blood type α: Pε ∗ vσ ∗ (1 − w) ∗ Qtασ, σ = PLT
Wastage cost of outdated product σ at hospital i: Pε ∗ vσ ∗ Oitσε
Wastage cost of outdated product σ at the blood center: Pε ∗ vσ ∗ O0tσε
-
Other costs under scenario ε:
Initial inventory cost of product σ aged nwith type α: \({P}_{\varepsilon}\ast \left({I}_{01 n\alpha \sigma \varepsilon}+{\sum}_{i=1}^I{I}_{i1 n\alpha \sigma \varepsilon}\right)\ast \left(L+V+{h}_{\sigma}\right)\)
The cost for initial inventory is estimated to be production cost adds one-day holding cost.
Eq. (1) shows the final objective function for the multi-stage multi-product stochastic blood supply chain model.
The blood supply chain model contains the following constraints:
-
(1)
Supply limitations at collection facilities, the blood center, and hospitals
Blood can be supplied through whole blood donation and apheresis donation. Whole blood is mainly collected using bloodmobiles at different collection sites. Constraint (2) represents the number of whole blood donation does not exceed the available whole blood donors of each blood type at collection facilities on each day. Bloodmobiles can also collect apheresis derived RBCs. Constraint (3) put an upper limit on the number of apheresis donation for RBCs at each collection site. The blood center and hospitals mainly collect apheresis derived RBCs and PLTs. Constraints (4) and (5) indicate the number of apheresis donation cannot exceed the available apheresis donors at the blood center and hospitals, respectively.
-
(2)
Production ratio between whole blood and apheresis
Apheresis donation requires an apheresis machine to collect a particular blood component, such as RBCs or PLTs, and return the other components back to the donor. This process takes much longer compared to a whole blood donation. Hence, more donors tend to make a whole blood donation instead of an apheresis donation. In addition, the number of apheresis machines is limited at different facilities. Therefore, we set a maximum percentage (uσ) for apheresis donation for each blood product. Constraint (6) ensures that the number of whole blood donations takes a minimum percentage of (1 − uσ).
-
(3)
Capacity restrictions at the blood center and each hospital
Whole blood collected at each bloodmobile is used to produce RBCs and PLTs at the blood center. Constraint (7) ensures that the number of RBCs and PLTs derived from whole blood do not exceed capacity of the blood center for each product. Constraints (8) and (9) guarantee the number of remaining inventories for each blood product at the end of each day do not exceed the storage capacity of the blood center and hospitals, respectively.
-
(4)
Production loss constraint
Production loss is considered for whole blood extraction as some collected whole blood units may fail the test and some may not be rich enough to extract RBCs and PLTs. Usually, the blood center can determine an estimated fixed percentage for production loss (γ). It is noted that two days are need for collected whole blood to undergo infectious disease testing and component separation. Therefore, the number of RBCs/PLTs derived from whole blood for each blood type on each day is based on the percentage of production loss times the number of whole blood donation two days ago. Constraint (10) represents this relationship.
-
(5)
Inventory balance constraints at the blood center
Constraints (11)–(15) are balance constraints that update the inventory status of blood products at the blood center for each age group and blood type at the start of each day under each scenario. Constraint (11) states that the inventory level of blood products more than four days old equals the inventory level of the previous day minus the number of blood units transported to hospitals on the previous day. Constraints (12) and (13) update the inventory status of three-day-old RBCs and PLTs respectively. Blood products derived from whole blood are assigned to the three-day-old inventory on each day considering two days are required for processing and testing. The inventory level of three-day-old blood products equals the original two-day-old inventory of the previous day and newly produced whole blood derived products minus the number of two-day-old blood units transported to hospitals on the previous day. Apheresis derived blood products are assigned to the two-day-old inventory because one day is needed for testing apheresis derived blood products. In this regard, one-day-old blood products are not available. Therefore, at the start of each day, the inventory level of two-day-old blood products equals the quantity of blood products produced by apheresis on the previous day at the blood center and blood collection facilities as given by constraint (14). Constraint (15) enforces that the inventory level of two-day-old blood products on each day should be greater than the number of two-day-old blood products transported to hospitals on that day under all scenarios.
-
(6)
Inventory balance constraints at each hospital
Constraints (16) and (17) are balance constraints that update the inventory status of blood products at each hospital for each age group and blood type at the start of each day under each scenario. Constraint (16) shows that the inventory level of two-day-old blood products equals the quantity of blood products produced by apheresis at hospitals on the previous day. Note that those two-day-old blood products from the blood center have not arrived at hospitals at the point of status updating. They will be considered on the next day for updating inventory status of three-day-old products. Constraint (17) states that the inventory level of blood products more than two days old equals the previous inventory level and the quantity of blood products received from the blood center on the previous day minus the quantity of blood units used to satisfy demand on the previous day.
-
(7)
No shortage at hospitals
Constraint (18) ensures that no shortage occurs for each demand type and blood type at hospitals on each day under each scenario. \({\sum}_{\alpha^{\prime }}{\sum}_{n\in {D}_k}{U}_{itn{\alpha}^{\prime}\alpha \sigma \varepsilon}\) calculates the total number of blood product σ with different ages and blood types used to satisfy patient demand of type k and blood type α at hospital i on day t under scenario ε. All demand is fulfilled. Note that only PLTs need to consider different demand types. Fresh PLTs are permitted to be transfused to patients that require fresh, young, or old PLTs and young PLTs are suitable to be transfused to patients that require young or old PLTs.
-
(8)
Expired blood products at the blood center and each hospital
The leftover blood products with maximum age after fulfilling daily demand are outdated at the end of each day. Constraints (19) and (20) capture the outdated quantity for each blood product on each day at the blood center and each hospital, respectively.
-
(9)
Initial inventory at the blood center and each hospital
Constraints (21) and (22) put upper bounds for initial inventory of blood products at the blood center and hospitals, respectively. Constraint (23) ensures that the number of blood products derived from whole blood on the second day of planning horizon equals zero.
-
(10)
Non-negativity and binary constraints.
Constraints (24) and (25) define the domains of variables.
5 Computational study
5.1 Case description
In this section, a real-world multi-product blood supply chain with one blood center, three blood collection facilities, and five hospitals in the Fargo-Moorhead area is applied to test and evaluate the proposed model. This area mainly includes Fargo, North Dakota, Moorhead, Minnesota, and the surrounding communities in the United States as shown in Fig. 2, in which the geographical locations of collection sites, the blood center, and hospitals are also presented.
In accordance with the literature as shown in Ensafian and Yaghoubi [18] and Haijema et al. [24], we assume that daily demand for PLT units at each hospital follows a Poisson distribution and the mean values of daily demand at a regular hospital with around 100–150 beds are 12, 8, 16, 8, 12, 4 and 4 for Monday through Sunday respectively. For RBCs, the mean daily demand at a regular hospital are 100, 93, 56, 59, 44, 18, and 17 for Monday through Sunday respectively as mentioned in Gunpinar and Centeno [23]. The demand for each blood type of RBCs is estimated to be a proportion of total demand and the proportion equals the approximate distribution of each blood type in the US population [4]. To estimate mean daily demand of RBCs and PLTs at each considered hospital, a demand coefficient is assigned based on the number of beds at the relevant hospital. The upper bound for initial inventory of RBCs and PLTs at each hospital equals the mean daily demand of RBCs and PLTs at that hospital on Monday respectively.
Both RBCs and PLTs can be collected from apheresis donation at the blood center and hospitals as well as whole blood donation at collection facilities. In this study, one unit of whole blood is assumed to produce one unit of RBC and 1/5 unit of PLT. One apheresis production can obtain two units of RBCs or two units of PLTs. Apart from these approaches, RBCs can also come from apheresis donation at collection sites. Table 4 presents the number of available donors for different blood products on each day in these three sites. The uniform distribution is estimated based on real data collected at different locations for available appointments under a four-month period. The number of available donors at each facility is generated randomly using the corresponding uniform distribution. Not all whole blood units collected at collection facilities are suitable for producing RBCs and PLTs, thus we adopt the value of 98% for γ to represent the percentage of appropriate whole blood in accordance with Ensafian and Yaghoubi [18]. The pooling percentage is assumed to 1.
Table 5 summarizes the values of cost parameters used to demonstrate the proposed model. Most values are obtained from Ensafian and Yaghoubi [18], Barbee et al. [10], and Gunpinar and Centeno [23].
5.2 Numerical results
To better capture the variability of demand for both RBCs and PLTs and simulate a real blood supply chain, it is necessary to consider an appropriate number of demand scenarios and length of the planning horizon. Thus, we tested different numbers of demand scenarios including 5, 10, 15, and 20 based on a planning horizon of 60 days, and we assessed planning horizon of 50, 60, and 75 days based on 20 demand scenarios. We selected the average daily cost, which is calculated as total cost divided by the length of the planning horizon, as the performance measure for the proposed multi-product blood supply chain model under different situations. The demand dataset was generated using the R language and the experimental results were obtained using IBM ILOG CPLEX solver on a Dell XPS8940 desktop with 2.50 GHz CPU and 16 GB of RAM. To assess the variability of the outputs with different numbers of demand scenarios, the experiments were repeated ten times with different demand datasets that were randomly generated based on daily mean values for each day of the week. We use G i (i = 1, 2, . . , 10) to denote the group of demand datasets for the i th run of the experiments. In Appendix 1, Tables 12 and 13 present the computational results of average daily cost for the experiments.
Figures 3 and 4 show the average daily cost for the ten groups of datasets with different numbers of demand scenarios and different lengths of the planning horizon, respectively. From Fig. 3, the average daily cost increases as the number of scenarios increases from 5 to 15 for all groups, but the average daily costs for the 15 and 20 scenarios look similar. The convergence of decision variables was checked with 15 and 20 scenarios. When the number of scenarios increases from 15 to 20, average daily production of apheresis RBCs increases by 1.68%, average daily production of apheresis PLTs increases by 2.92%, whole blood donation decreases by 0.002%, average daily inventory of RBCs increases by 0.24%, and average daily inventory of PLTs increases by 1.01%. It is clear that decisions are converging with 15 and 20 scenarios. Based on Appendix 1, Table 12, the Bootstrapping method was used to calculate confidence intervals for the optimal average daily cost for different numbers of demand scenarios. The confidence intervals for 5, 10, 15, and 20 demand scenarios are ($52,428–$52,819), ($52,973–$53,222), ($53,169–$53,428), and ($53,296–$53,556), respectively. From Fig. 4, we can see that the average daily cost increases as the length of the planning horizon increases from 50 to 60 days for all the groups, but the average daily costs for the 60-day and 75-day planning horizon look similar. Based on Appendix 1, Table 13, the confidence intervals for 50-day, 60-day, and 75-day planning horizons are ($51,772–$52,001), ($53,296–$53,556), and ($53,331–$53,507), respectively. Therefore, it is enough to consider 15 demand scenarios and a planning horizon of 60 days for the proposed blood supply chain. In this research, we consider 20 demand scenarios within a 60-day planning horizon to perform the remaining analyses.
The proposed multi-product blood supply chain model considers production, inventory holding, transportation, and wastage costs for both RBCs and PLTs. To examine the specific daily cost within the 60-day planning horizon considering 20 demand scenarios, we use G1 dataset as an illustration. Table 6 summarizes the optimal daily cost that allows the model to satisfy both demand for RBCs and PLTs in all 20 scenarios within the 60-day planning period. Because daily cost during the third day to the fifty-eight day fluctuates up and down within a certain range, we use the average value to show the numerical results. In addition, the fluctuation of total cost from day 3 to day 58 is shown in Fig. 5. As can be seen in Fig. 5, total cost ranges from $42,680 to $63,463 with a mean value of $52,761 during these days. There is a weekly pattern with peaks on Tuesdays.
From Table 6, we can see that the minimum total cost for the multi-product blood supply chain is $3,217,189 during the planning horizon. This mainly comes from production cost which takes a proportion of approximately 98.58%. The production cost involves both whole blood and apheresis blood production costs of RBCs and PLTs and production cost for initial inventory. The average initial inventory is about 686 units for RBCs and 90 units for PLTs in all 20 demand scenarios. The number of RBCs produced on average is 16,079 units with 92.77% from whole blood production. The total production of PLTs on average is 3696 units with 80.71% being derived from whole blood. There are more than four times as many RBCs being produced as PLTs. For both products, there are no outdates which suggests that all the units produced are used for fulfilling demand. All the platelets derived from whole blood are assumed to be pooled together and put into inventory in the blood center. As one unit of whole blood can produce one unit of RBC and 1/5 unit of PLT at the same time, the amount of whole blood derived RBCs will equal the amount of whole blood derived PLTs times 1/5. On one hand, if this quantity is too small, there may not be enough RBCs to satisfy demand and shortage occurs. On the other hand, if this quantity is too big, PLTs maybe overproduced because of the big demand difference between RBCs and PLTs. As shortage is not allowed, the optimal production is a tradeoff between whole blood production and apheresis production for RBCs and PLTs to minimize overproduction and wastage. Transportation cost is the second largest at 0.74%. The inventory holding cost is the third largest, about 0.68% of the total. This includes an additional one day holding cost for initial inventory of RBCs and PLTs. Wastage costs are zero and are thus not shown in the table.
5.3 Comparing the multi-product model to an uncoordinated model
In this section, the proposed multi-product supply chain model is compared with an uncoordinated model which handles the RBC and PLT supply chains separately. The uncoordinated model includes two single product models: the RBC model and the PLT model. The objective of the RBC model is to minimize total cost in the RBC supply chain and the objective of the PLT model is to minimize total cost in the PLT supply chain. For the uncoordinated model, there are several assumptions:
-
Whole blood donors and apheresis RBC donors are both considered in the RBC supply chain. According to the AABB and National Blood Collection and Utilization surveys, around 85% of RBCs collected are derived from whole blood in the US, but only 8% of PLTs transfused are derived from whole blood [10]. Thus, whole blood is an important source for RBC supply.
-
Most of the PLTs, which are produced when producing RBCs through whole blood, will be discarded directly instead of being pooled together to create a transfusable PLT unit. This is reasonable considering the real situation in the US blood supply chain as only 8% of PLTs transfused are derived from whole blood despite the large amount of whole blood collected and separated.
-
The PLT supply chain only considers apheresis PLT donors, but PLT supply also includes pooled PLTs that are produced in the RBC supply chain. Whole blood derived PLTs that are pooled will be put into inventory in the blood center and can be used for PLT transfusion. The pooling percentage is assigned to be 0.25 according to Barbee et al. [10].
The multi-product model is used to run the RBC and PLT supply chains, respectively. First, the RBC supply chain is considered. Demand for RBCs is the same as the multi-product model but demand for PLTs is set to zero. The remaining parameters are the same as the multi-product model. Total cost for the RBC supply chain only includes the different types of costs for RBCs. Though PLTs are also produced through whole blood, any cost regarding PLTs such as pooling cost, holding cost, and wastage cost will not be considered in the RBC supply chain. Instead, these costs will be considered in the PLT supply chain. Further, we add the quantity of whole blood derived PLTs from the RBC supply chain to the inventory of the PLT supply chain on the corresponding days. For the PLT supply chain, demand for PLTs is the same as the multi-product model while demand for RBCs is set to be zero. In addition, available whole blood donors are also set to zero. Total cost for the PLT supply chain only includes the different types of costs for PLTs.
Tables 7 and 8 show results of daily cost for the RBC supply chain and corresponding PLT supply chain, respectively. The total cost is on average $2,813,332 for the RBC supply chain and $1,432,196 for the PLT supply chain. The two single product models have similar cost distributions as the multi-product model where production cost takes over 75% of total cost. For the RBC supply chain, 16,079 units of RBCs are produced and around 92.77% are derived from whole blood. At the same time, approximately 2983 units of PLTs are produced. For these whole blood derived PLTs, around 2237 units are discarded as whole blood is primarily used for producing RBCs in the US, and the remaining units are put into inventory for the PLT supply chain. For the PLT model, an additional 2006 units of PLTs are produced through apheresis to satisfy demand.
To examine the differences between the multi-product model and the uncoordinated model, it is necessary to sum up the results for the RBC and the PLT supply chains and compare it to the multi-product model under different realized demand within the 60-day planning horizon. Therefore, we select production cost, holding cost, wastage cost, transportation cost, and total cost as performance measures, and run the models on all ten groups of demand datasets. The value of each cost measure under each group for the RBC supply chain is added with the corresponding value for the PLT supply chain to constitute a new data table. As a representation, we select and compare the total costs from the multi-product model and the total costs for the sum of the two single product models using a paired sample T-test. The mean and standard deviation are $3,205,563 and $3438, respectively, for the multi-product model and $4,240,063 and $6016, respectively, for the sum of the single product models. The mean difference is $1,034,500 and its 95% confidence interval is between $1,022,751 and $1,046,249. In addition, the p-value equals 0.000, which is less than 0.05. Thus, we conclude that there is a statistically significant difference between the means of total cost for the multi-product model and the sum of the single product models.
Table 9 shows the comparisons of different costs for the multi-product model and sum of the single product models, where the results are the averages on ten groups of demand data. The total cost for the multi-product model is $3,205,563, while it is $4,240,063 for the uncoordinated model, an increase of 32.27%. A coordinated multi-product model can save $1,034,500 in 60 days, that is about $6.29 million annual savings. The cost difference between both models mainly comes from differences in production cost. As demand is the same for both models, this suggests that average unit production cost is lower for the multi-product model. Both RBCs and PLTs can be produced through whole blood and apheresis. Using cost parameters stated in Table 5, we find that unit apheresis production cost is $219 for RBCs, and $538 for PLTs, but the unit production cost is around $125 (150/1.2) since one unit of whole blood can produce 1.2 units of blood products. Therefore, whole blood production is a preferred approach for both models. However, for the uncoordinated model, PLTs are mainly produced through apheresis. The ratio of whole blood derived PLTs to total produced PLTs is 80.89% for the multi-product model and 59.74% for the PLT supply chain. This explains why average unit production cost for the multi-product model is lower than the uncoordinated model. In addition to production cost, increases in wastage cost also play an important role in the total cost difference between the multi-product model and the uncoordinated model. A large amount of whole blood derived PLTs are wasted for the uncoordinated model as the pooling percentage is set at 0.25 to simulate the current PLT supply chain. From these results, we can conclude that considering a coordinated multi-product model is important in reducing production and wastage costs for the blood supply chain.
5.4 Sensitivity Analysis
In this section, we perform sensitivity analyses to explore the impacts of donors and pooling percentage on system performance with total cost as the performance indicator.
5.4.1 Impact of donors on total cost
As demand for RBCs is much larger than PLTs, changing the supply of RBCs should significantly influence the performance of both the coordinated and uncoordinated blood supply chains. We consider three different situations to evaluate the impact of donors on total cost: decreasing supply of RBCs by multiplying by 0.8, the base case, and increasing supply by multiplying by 1.2.
We firstly evaluate the impact of changing both whole blood and apheresis RBC donors on total cost. Table 10 shows the average total cost for the multi-product model and two single product models under three situations with ten groups of demand data. When the supply of RBCs decreases from 1 to 0.8, total cost for the multi-product model increases by 4.92%. However, total cost for the RBC supply chain increases by 5.43% and increases by 0.70% for the PLT supply chain, which leads to an increase of 3.83% in total cost for the uncoordinated model. The increases on total cost mainly come from higher unit production cost for both models, and the cost difference between the two models decreases to 30.89%. When the supply of RBCs increases from 1 to 1.2, total cost for the multi-product model decreases by 1.97%, and total cost for the uncoordinated model decreases by 1.55%. The cost difference between the multi-product model and the uncoordinated model enlarges to 32.84%. These results suggest that a coordinated multi-product blood supply chain performs much better than an uncoordinated single product supply chain as the number of donors increases.
As RBCs can be obtained from both whole blood donors and apheresis RBC donors, it is useful to identify which type of donor has a higher impact on system performance. Therefore, we evaluate the impact of whole blood donors and apheresis donors on total cost respectively. The impact of whole blood donors on total cost is examined through multiplying the number of whole blood donors by 0.8, 1, and, 1.2 respectively. Similarly, the impact of available apheresis donors of RBCs on total cost is examined through multiplying the number of total apheresis RBC donors by 0.8, 1, and, 1.2 respectively. The corresponding average result of total cost for the multi-product model and two single product models under ten groups of demand data is shown in Table 11. The result for whole blood donors is quite similar to the previous analysis on both whole blood and apheresis RBC donors, but the impact of apheresis donors on total cost for both the multi-product model and sum of the single product models are negligible. This indicates that whole blood donors have a major influence on the cost efficiency of the blood supply chain and changes in apheresis donors do not have much impact on total cost.
5.4.2 Impact of pooling percentage on total cost
To capture the impact of pooling percentages on system performance, we introduce pooling percentage w, which measures the percentage of whole blood derived PLTs used for pooling and transfusion. This parameter directly affects the production of PLTs and the production costs of the entire blood supply chain. The impact of pooling percentage on total cost is evaluated by assigning values of 0.25, 0.5, 0.75, and 1 to the pooling percentage. Figure 6 shows the corresponding average result of total cost for the multi-product model and sum of total costs for the two single product models with ten groups of demand data. When the pooling percentage increases, the total costs for both the multi-product model and sum of the single product models decrease. With the same pooling percentage, the multi-product model always performs better than the sum of the single product models, and the cost difference increases as the pooling percentage decreases. This indicates that increasing pooling percentage and applying the multi-product model are effective ways to improve system performance for the blood supply chain.
6 Conclusion
This paper presents a multi-product multi-period stochastic program for an integrated blood supply chain which includes two perishable blood products. The blood supply chain consists of one regional blood center, several blood collection facilities, and hospitals with consideration of demand uncertainty, blood age information, blood type substitution of RBCs, three demand types of PLTs, and centralized operational decisions. The aim of the model is to minimize the total cost incurred during the collection, production, inventory, and distribution by making optimal decisions on the quantity of collected whole blood and apheresis derived RBCs and PLTs, the quantity of whole blood separation, and the quantity of blood distribution to different hospitals. In the multi-product system, the RBC and PLT supply chains intertwine at the collection and production stages as whole blood donated can be separated into RBCs and PLTs at the same time. The sharing of a production process and the demand differences between RBCs and PLTs may result in excess PLTs that can’t be absorbed by the current supply chain system.
The formulated model was applied to a real case study from the Fargo-Moorhead area, North Dakota and Minnesota, USA. The results were analyzed and compared with that of an uncoordinated model where the RBC and PLT supply chains were considered separately. Our numerical result for the multi-product model indicated that production cost takes over 90% of overall cost and optimal decision on production is a tradeoff between whole blood production and apheresis production for RBCs and PLTs. We also found that a coordinated multi-product model outperforms an uncoordinated model, and coordinating decisions can save $1,034,500 in 60 days, that is about $6.29 million annual savings. Furthermore, sensitivity analyses were implemented to explore the impacts of donors and pooling percentage on system performance of both coordinated and uncoordinated supply chains. The analyses showed that the coordinated multi-product model performs much better than an uncoordinated model as the number of donors increases and these cost savings mainly come from changes in the number of whole blood donors. In addition, increasing pooling percentage can positively affect the system performance of both models.
It is important for administrators and decision makers to make optimal tactical and operational decisions in the blood supply chain that account for cost efficiency along with controlling shortage and wastage. Therefore, we provide the following managerial insights:
-
Considering a multi-product supply chain for RBCs and PLTs is an effective strategy to save total operational cost along with reducing wastage for the blood supply chain network. We encourage decision makers in charge of RBC and PLT supply chains at blood centers to coordinate production plans of blood products.
-
Whole blood production is a more cost-effective way on producing both RBCs and PLTs. If recruiting donors is a necessity, then recruiting whole blood donors is a better choice.
-
Despite the advantages of apheresis PLTs, increasing the use of pooled PLTs through whole blood donation is an effective way to save total cost and reduce wastage of the blood supply chain. It is better for decision makers to take use of as many PLTs that is produced while producing whole blood derived RBCs for PLT transfusions.
However, this study still exhibits some limitations. First, though stochastic demand was considered, the proposed multi-product model only works for normal situations in the blood supply chain, but it doesn’t work for a disaster situation when demand increases dramatically and lasts for a period of time. Second, the model was considered for a centralized system. This requires that hospitals and the blood center maintain mutual trust and information transparency and make decisions regarding production and distribution with a system-wide perspective.
There are several future research directions. First, developing efficient solution algorithms to solve a large-scale problem within a reasonable time. The computational complexity of the problem increases dramatically if considering more facilities sites and hospitals. Second, the consideration of a larger blood supply chain with more blood centers, collection sites, and hospitals. It is normal to have multiple blood centers in large cities such as New York and it is necessary to consider the interactions among these blood centers. Third, considering weekends and holidays when normal blood collection and production activities are not conducted. Finally, the consideration of supply uncertainty with respect to the number of different types of donors at different facilities.
Data Availability
Not applicable.
References
Abbasi B, Hosseinifard SZ (2014) On the Issuing Policies for Perishable Items such as Red Blood Cells and Platelets in Blood Service. Decis Sci 45(5):995–1020
Abdulwahab U, Wahab MIM (2014) Approximate dynamic programming modeling for a typical blood platelet bank. Comput Ind Eng 78:259–270. https://doi.org/10.1016/j.cie.2014.07.017
Altiparmak F, Gen M, Lin L, Karaoglan I (2009) A steady-state genetic algorithm for multi-product supply chain network design. Comput Ind Eng 56(2):521–537. https://doi.org/10.1016/j.cie.2007.05.012
American Red Cross (2019) Know the facts about blood and blood types. https://www.redcrossblood.org/donate-blood/blood-types.html. Accessed 10 Oct 2019
American Red Cross (2021a) Blood components. https://www.redcrossblood.org/donate-blood/how-to-donate/types-of-blood-donations/blood-components.html. Accessed 25 Oct 2021
American Red Cross (2021b) Blood needs and blood supply. https://www.redcrossblood.org/donate-blood/how-to-donate/how-blood-donations-help/blood-needs-blood-supply.html. Accessed 25 Oct 2021
American Red Cross (2021c) Types of blood donations. https://www.redcrossblood.org/donate-blood/how-to-donate/types-of-blood-donations.html. Accessed 25 Oct 2021
Arvan M, Tavakoli-Moghadam R, Abdollahi M (2015) Designing a bi-objective and multi-product supply chain network for the supply of blood. Uncertain Supply Chain Management 3(1):57–68. https://doi.org/10.5267/j.uscm.2014.8.004
Barbee IW (2013) The 2011 National Blood Collection and Utilization Survey Report. https://www.hhs.gov/sites/default/files/ash/bloodsafety/2011-nbcus.pdf. Accessed 25 Mar 2022
Barbee IW, Srijana R, Andrea H (2015) The 2013 AABB Blood Collection, Utilization, and Patient Blood Management Survey Report. https://www.aabb.org/docs/default-source/default-document-library/resources/2013-aabb-blood-survey-report.pdf?sfvrsn=17317db0_0. Accessed 25 Mar 2022
Beliën J, Forcé H (2012) Supply chain management of blood products: A literature review. Eur J Oper Res 217(1):1–16. https://doi.org/10.1016/j.ejor.2011.05.026
Birge JR, Louveaux F (2011) Introduction to stochastic programming. Springer Science & Business Media. http://www.springer.com/series/3182. Accessed 10 Oct 2019
Civelek I, Karaesmen I, Scheller-Wolf A (2015) Blood platelet inventory management with protection levels. Eur J Oper Res 243(3):826–838. https://doi.org/10.1016/j.ejor.2015.01.023
Deuermeyer BL, Pierskalla WP (1978) A By-Product Production System with an Alternative. Manag Sci 24(13):1373–1383
Dillon M, Oliveira F, Abbasi B (2017) A two-stage stochastic programming model for inventory management in the blood supply chain. Int J Prod Econ 187:27–41. https://doi.org/10.1016/j.ijpe.2017.02.006
Duan Q, Liao TW (2013) A new age-based replenishment policy for supply chain inventory optimization of highly perishable products. Int J Prod Econ 145(2):658–671. https://doi.org/10.1016/j.ijpe.2013.05.020
Duan Q, Liao TW (2014) Optimization of blood supply chain with shortened shelf lives and ABO compatibility. Int J Prod Econ 153:113–129. https://doi.org/10.1016/j.ijpe.2014.02.012
Ensafian H, Yaghoubi S (2017) Robust optimization model for integrated procurement , production and distribution in platelet supply chain. Transp Res E 103:32–55. https://doi.org/10.1016/j.tre.2017.04.005
Ensafian H, Yaghoubi S, Modarres M (2017) Raising quality and safety of platelet transfusion services in a patient-based integrated supply chain under uncertainty. Comput Chem Eng 106:355–372. https://doi.org/10.1016/j.compchemeng.2017.06.015
Eskandari-Khanghahi M, Tavakkoli-Moghaddam R, Taleizadeh AA, Amin SH (2018) Designing and optimizing a sustainable supply chain network for a blood platelet bank under uncertainty. Eng Appl Artif Intell 71(March):236–250. https://doi.org/10.1016/j.engappai.2018.03.004
Fahimnia B, Jabbarzadeh A, Ghavamifar A, Bell M (2017) Supply chain design for efficient and effective blood supply in disasters. Int J Prod Econ 183:700–709. https://doi.org/10.1016/j.ijpe.2015.11.007
Govender P, Ezugwu AE (2019) A Symbiotic Organisms Search Algorithm for Optimal Allocation of Blood Products. IEEE Access 7:2567–2588. https://doi.org/10.1109/ACCESS.2018.2886408
Gunpinar S, Centeno G (2015) Stochastic integer programming models for reducing wastages and shortages of blood products at hospitals. Comput Oper Res 54:129–141. https://doi.org/10.1016/j.cor.2014.08.017
Haijema R, Van Der Wal J, Van Dijk NM (2007) Blood platelet production: Optimization by dynamic programming and simulation. Comput Oper Res 34(3):760–779. https://doi.org/10.1016/j.cor.2005.03.023
Hamdan B, Diabat A (2019) A two-stage multi-echelon stochastic blood supply chain problem. Comput Oper Res 101:130–143. https://doi.org/10.1016/j.cor.2018.09.001
Hosseinifard Z, Abbasi B, Fadaki M, Clay NM (2019) Postdisaster Volatility of Blood Donations in an Unsteady Blood Supply Chain. Decis Sci. https://doi.org/10.1111/deci.12381
Liang T-F (2008) Fuzzy multi-objective production/ distribution planning decisions with multi-product and multi-time period in a supply chain. Comput Ind Eng 55:676–694. https://doi.org/10.1016/j.cie.2008.02.008
Mirzapour Al-E-Hashem SMJ, Malekly H, Aryanezhad MB (2011) A multi-objective robust optimization model for multi-product multi-site aggregate production planning in a supply chain under uncertainty. Int J Prod Econ 134(1):28–42. https://doi.org/10.1016/j.ijpe.2011.01.027
Najafi M, Ahmadi A, Zolfagharinia H (2017) Blood inventory management in hospitals: Considering supply and demand uncertainty and blood transshipment possibility. Operations Research for Health Care 15:43–56. https://doi.org/10.1016/j.orhc.2017.08.006
Osorio AF, Brailsford SC, Smith HK (2015) A structured review of quantitative models in the blood supply chain: a taxonomic framework for decision-making. Int J Prod Res 1(1):1–22. https://doi.org/10.1080/00207543.2015.1005766
Osorio, A. F., Brailsford, S. C., Smith, H. K., Forero-Matiz, S. P., & Camacho-Rodríguez, B. A. (2016). Simulation-optimization model for production planning in the blood supply chain. Health Care Management Science, 122. https://doi.org/10.1007/s10729-016-9370-6
Paksoy T, Bektaş T, Özceylan E (2011) Operational and environmental performance measures in a multi-product closed-loop supply chain. Transportation Research Part E: Logistics and Transportation Review 47(4):532–546. https://doi.org/10.1016/j.tre.2010.12.001
Pirabán, A., Guerrero, W. J., & Labadie, N. (2019). Survey on blood supply chain management: Models and methods. Comput Oper Res, 112. https://doi.org/10.1016/j.cor.2019.07.014
Rajendran S, Ravindran AR (2019) Inventory management of platelets along blood supply chain to minimize wastage and shortage. Comput Ind Eng 130(July 2018):714–730. https://doi.org/10.1016/j.cie.2019.03.010
Rajendran S, Srinivas S (2020) Hybrid ordering policies for platelet inventory management under demand uncertainty. IISE Transactions on Healthcare Systems Engineering 10(2):113–126. https://doi.org/10.1080/24725579.2019.1686718
Van Dijk N, Haijema R, Van Der Wal J, Sibinga CS (2009) Blood platelet production: A novel approach for practical optimization. Transfusion 49(3):411–420. https://doi.org/10.1111/j.1537-2995.2008.01996.x
Wang K-M, Ma Z-J (2015) Age-based policy for blood transshipment during blood shortage. Transportation Research Part E: Logistics and Transportation Review 80:166–183. https://doi.org/10.1016/j.tre.2015.05.007
World Health Organization. (2020). 10 facts on blood transfusion. https://www.who.int/features/factfiles/blood_transfusion/blood_transfusion/en/. Accessed 15 June 2020
Zahiri B, Pishvaee MS (2017) Blood supply chain network design considering blood group compatibility under uncertainty. Int J Prod Res 55(5):2013–2033. https://doi.org/10.1080/00207543.2016.1262563
Code availability
No
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
Not applicable.
Ethics approval
was not needed, in accordance with the policies of my institution.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
Xu, Y., Szmerekovsky, J. A multi-product multi-period stochastic model for a blood supply chain considering blood substitution and demand uncertainty. Health Care Manag Sci 25, 441–459 (2022). https://doi.org/10.1007/s10729-022-09593-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-022-09593-5