Abstract
This paper assesses the economic efficiency of Brazilian general hospitals that provide inpatient care for the Unified Health System (SUS). We combined data envelopment analysis (DEA) and spatial analysis to identify predominant clusters, measure hospital inefficiency and analyze the spatial pattern of inefficiency throughout the country. Our findings pointed to a high level of hospital inefficiency, mostly associated with small size and distributed across all Brazilian states. Many of these hospitals could increase production and reduce inputs to achieve higher efficiency standards. These findings suggest room for optimization, but inequalities in access and the matching of demand and supply must be carefully considered in any attempt to reorganize the hospital system in Brazil.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hospital expenditure represents a large share of total health expenses in almost all countries. The Organization for Economic Cooperation and Development (OECD) estimates that hospital spending alone represented 38% of total health expenses in 2015 [39]. This share reflects a complex production function since inpatient care usually involves different types of health and nonhealth professionals, demands a network of diagnostic services, and is technology intensive. In Brazil, the share of hospital expenditure in total expenses is similar to the OECD average, at approximately 36% for 2012–2014 [36]. In part, this share is justified by the model of care provided in both the public and private sectors that is mostly centered in inpatient care [20, 23].
In this context, the study of hospital efficiency is crucial to achieving a sustainable health system. Efficiency depends on a multitude of factors, including the organization of healthcare services. Mosca [37] found that OECD countries with a more decentralized health system have higher levels of health expenditure than their counterparts. The Brazilian Unified Health System (“Sistema Único de Saúde” [SUS]) provides universal and free access to a comprehensive set of healthcare services to the population. Healthcare services delivery is decentralized and hierarchically arranged, with municipalities playing a central role in their provision. Even though decentralization can better match local needs, it sometimes fails to achieve scale and technical efficiency requirements. In Brazil, for instance, a large number of municipalities (45%) have less than 10,000 inhabitants and limited technical capacity to manage and provide all the levels of services and complexity required [12, 20]. As a result, a large number of small hospitals operate inefficiently, with low levels of occupancy [42, 50]. The socioeconomic heterogeneity in Brazil also translates to different management abilities among municipalities.
Additionally, there are different healthcare providers in Brazil: public, private and philanthropic. Most of the Brazilian public hospitals are owned and operated by federal, state, or municipal governments, with direct administration (47%). Concerning organizational functions, such as procurement and budget implementation, only a small portion is autonomous (less than 1%) or semiautonomous (5%), with indirect administration. Private hospitals (16%) are for-profit organizations, operating under competitive pressure and assuming responsibility for their own results. Philanthropic hospitals (32%) differ from private hospitals because they are nonprofit organizations. However, to be a philanthropic entity and consequently enjoy the benefits of financial and tax incentives, it is necessary to satisfy Ministry of Health requirements, such as agreeing to provide a minimum of 60% of services to SUS patients [40]. Therefore, organizational arrangements impact a hospital’s performance, varying the incentives according to payment mechanisms, contracts or regulations [23]. The very existence of a decentralized health system composed of diverse healthcare providers in a large and socioeconomically heterogeneous country brings the study of efficiency to the forefront of health economic analysis in developing countries.
To the best of our knowledge, hospital efficiency analysis at the national level has not yet been conducted in Brazil. The existing studies focus on particular states [10, 31, 46, 48], Brazilian capitals [19] or groups of hospitals [3, 24, 26, 30, 42]. Regardless of the level of aggregation, these studies find that the majority of hospitals in Brazil are inefficient ([19, 23, 26, 31, 42]). Inefficiency is particularly common among small hospitals. Rodrigues et al. [42] showed that 53.13% of small hospitals in Brazil were operating inefficiently in 2014. Using a very small share of Brazilian hospitals (8%), La Forgia and Couttolenc [23] found an average technical efficiency score of 0.34. This very low average score calls into question the validity of La Forgia and Couttolenc’s findings. This is a very low score when compared to the OECD average, which ranges from 0.77 to 0.82 [49]. For instance, Portugal, despite having an average score above 0.90 for hospitals’ technical and scale efficiencies, was revealed to have an excess of full-time equivalent doctors and nurses, pointing to opportunities to improve productivity with reductions in operational resources [18].
Recently, Lins et al. [25] and the World Bank [50] studied Brazilian municipalities’ health performance. Lins et al. [25] analyzed municipal efficiency in health provision. The World Bank report found a high level of inefficiency in the provision of secondary healthcare services, suggesting that improvements in high- and medium-complexity healthcare are feasible and would allow the reallocation of financial resources to primary healthcare [50]. Municipalities with a large expenditure on medium-complexity hospital services are those with the highest levels of inefficiency [50]. These studies are different from ours as they used the municipality instead of hospitals as the unit of analysis. The approach of using local municipalities as the production unit of hospitalizations is not adequate because it hides the intramunicipal heterogeneity in terms of scale and efficiency. Moreover, the studies also used the aggregate level of healthcare expenditure [50] or specific health indicators [25] as inputs instead of production factors directly measured at the hospital level. As a consequence, there is no clear guidance in terms of public intervention at the hospital level.
In contrast to previous studies, we assessed hospital efficiency by taking into account all Brazilian general hospitals that provided healthcare services for the SUS in 2015. Combining efficiency estimation and spatial analysis, we found a high proportion of inefficiency associated with small and public hospitals. Despite some level of spatial clustering, inefficiency is widespread in the national territory. This is the first nationwide study to estimate inefficiency at the hospital level and the first to explore the spatial distribution of such inefficiency.
2 Methods
2.1 Data
We used two official cross-sectional databases: the National Registry of Health Facilities (CNES) [34] and the Hospital Information System of the Unified Health System (SIH/SUS) [35]. CNES is a national registry of mandatory completion that gathers monthly information on all health facilities, including their infrastructure and human resources. The SIH/SUS is an administrative database that contains information regarding all hospitalizations financed by the SUS, including characteristics of patients and medical procedures. We merged these databases using the CNES code as a unique identifier. In this analysis, we considered July 2015 as the temporal reference (midyear) for the CNES database and compiled all hospitalizations that occurred during the year from the SIH/SUS database. We excluded long-term hospitalizations since they refer to treatments that require long-term recovery, such as psychiatric or tuberculosis care. Excluded cases represented only 2.5% of total inpatient care delivered in that year.
From a total of 6154 general and specialized hospitals, 5120 are general hospitals. One limitation of the data used in this study is that available information concerns only hospitalizations financed by the SUS, regardless of whether they are provided by a private or by a public health facility. As private hospitals may be hired by the SUS but also provide inpatient care to the private sector, their production would be underestimated if we considered only hospitalizations financed by the SUS. To take into account this data limitation, we included only general hospitals that had at least 50% of beds allocated to the SUS and registered more than 50 hospitalizations throughout the year. Three hospitals that registered zero doctors were also excluded. In total, 1616 general hospitals were excluded and 3504 general hospitals included in the study.
2.2 Analysis
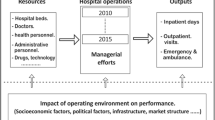
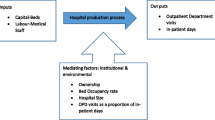
We performed data envelopment analysis (DEA) [14] to assess hospital efficiency. DEA is a linear programming approximation that estimates decision making unit (DMU) efficiency comparing each unit to best practice [11]. It is a nonparametric model that identifies best performers and builds a production frontier under which the other DMUs are evaluated. The efficiency score is estimated as the distance of a DMU to the production frontier [11, 44]. One advantage of using DEA is that it allows the estimation of efficiency by considering multiple inputs and outputs and decomposing total efficiency into technical and scale efficiencies [14, 15]. Technical inefficiency is observed when the mix of inputs does not reach the maximum feasible production [6]. Scale efficiency is obtained as the ratio between the total efficiency score estimated assuming constant returns of scale and variable returns to scale. We chose the input-oriented model [45] since the increase in the public health budget is probably not a feasible scenario. Brazil has experienced public deficits in recent decades, and the federal government has recently implemented strict measures to contain public expenditures. We chose the variable returns to scale (VRS) model since it accepts a more varied technology set. We also conducted a DEA slack analysis to check for the existence of DMUs that are considered Farrell efficient (weakly efficient). When the production function presents some flat regions, the efficiency of the DMUs projected onto these regions (Farrell efficient) may be improved by reducing the level of inputs; depending on the shape of the curve, output variations are also feasible [6].
Another important aspect of efficiency analysis is to consider minimally homogenous DMUs in terms of inputs and outputs. We classified hospitals into three groups based on a previous work of Botega et al. [7] that applied latent cluster class analysis to identify similar hospitals in terms of indicators and technology settings. The latent cluster class analysis identified three clusters of hospitals: small (less than 50 beds), medium (from 51 to 150 beds) and large hospitals (over 150 beds). Therefore, in our DEA specification, we ran separate models for each of these three groups. We also compared efficiency scores among type of healthcare providers (public, private, and philanthropic).
We included as inputs: (i) human resources working for the SUS (doctors, nurses, nursing assistants, and technicians), (ii) infrastructure dedicated to the SUS (number of beds, number of pieces of medium- and high-tech medical equipment). The numbers of doctors, nurses, and nurse assistants working were standardized by workload hours to allow for hospital comparisons. The output variables are the number of hospitalizations according to five groups of ICD-10 (circulatory, respiratory, pregnancy, childbirth/puerperium procedures, and others) and two age groups (younger than 60 and over 60 years old). These first three ICD-10 groups were responsible for 42% of all hospitalizations delivered in 2015 by the SUS. This disaggregation intends to control for differences in hospitals’ service composition and patients’ risk attributes. For instance, childbirth and puerperium procedures usually require short stays compared to circulatory procedures. Additionally, age is the only available variable that allows adjustments for risk attributes.
Density curves for the efficiency scores were represented by Epanechnikov kernel estimators. We performed a multivariate analysis of variance (MANOVA) to compare and test mean differences in efficiency scores by hospital size and type of healthcare providers. All analyses were estimated using R (version 3.3.3): for DEA with the benchmarking library and for MANOVA with the stats library.
To identify hospitals’ efficiency patterns throughout the country, we estimated a continuous efficiency surface from hospitals’ efficiency score. The spatial interpolation used the inverse distance weighting (IDW) method, which estimates the missing values using the sum of the weights of existent sample points in the neighborhood. As the weights are inversely associated with the distances between the predicted and the sampled points, this method more heavily weights the nearest sampled locality and is usually applied when certain locations attributes are unknown or inexistent [28]. In our study, for example, there are some municipalities with one or more hospitals and others with none. The estimated values are a linear combination of the weights and the observed values [28]. This analysis was performed using QGIS (3.10).
While surface analysis only identifies hot spots of hospital efficiency, it does not test whether these local spatial patterns are statistically significant. The statistical test of local clustering was performed using local spatial autocorrelation (LISA) analysis [1]. Departing from the point data representing hospital units, we generated Voronoi polygons in QGIS and imported this shapefile into GeoDa (version 1.14.0) to perform the global spatial autocorrelation (Moran I) and LISA tests. We used a queen matrix of order one as spatial weights and 99,999 permutations for bootstrapping hypothesis testing of spatial autocorrelation.
3 Results
3.1 Hospital size and healthcare service provider assessment
Figure 1 presents the main characteristics of Brazilian general hospitals. The majority of hospitals in Brazil are small and predominantly public. On average, the proportion of beds allocated to the SUS is 90%, indicating that the general hospitals included in this study are mostly dedicated to the public health system. Large hospitals represent only 13% of hospital units but have a significant role in meeting inpatient care demand: they are responsible for 86% of the highest-complexity treatments and almost 50% of all SUS hospitalizations and receive a higher proportion of nonresident patients compared to smaller hospitals. Large hospitals are also intensive in human, physical, and financial resources and have an average occupancy rate (68%) close to the National Health Agency (ANS) recommendation – 75% to 85% [2]. Small hospitals present a lower ratio of health professionals and average spending per bed and a significantly lower occupancy rate (21.86%), indicating that small hospitals have an excess of beds.
Characteristics of Brazilian general hospitals according to hospital size and healthcare provider, 2015 Source: CNES and SIH/SUS, 2015 [34, 35]. [1] As long as only one small hospital is classified as a syndicate, it is analyzed as an isolated case and not detailed in the table. * VRS = variable returns to scale model assumption; CRS = constant returns to scale model assumption. [2] Mean exchange rate of 2015 according to Brazilian Central Bank [5]
Concerning organizational structure, public and philanthropic hospitals are more intensive in human and physical resources, while private hospitals are more intensive in financial resources. Public large hospitals show higher averages for occupancy rate (73.05%), length of stay (7.30 days) and patients’ distance traveled (377.04 km). Private large hospitals receive more than 50% of nonresident patients. All mean differences are statistically significant across group sizes and healthcare providers (Fig. 1).
The DEA estimation pointed to average technical and scale efficiency scores of 0.59 and 0.75, respectively. A bootstrap analysis was conducted, resulting in a 0.43 average score for technical efficiency. However, the bootstrap analysis is preferable when the distribution is symmetric [6]. Instead, our efficiency score distribution was skewed; most of the hospitals are inefficient. The bootstrap method pushed the average scores down as the most efficient hospitals were not entirely included in the resampling. Therefore, we chose to advance with our study without the bootstrap estimation, which enabled us to proceed with the slack and returns to scale investigation as well.
The density curves for technical and scale scores revealed a very distinctive pattern according to hospital size (Fig. 2). The small hospitals distribution is left-skewed, with a median of approximately 0.46 and a higher concentration at lower levels of technical efficiency. In contrast, large hospitals had a median of 0.75, with a peak around 1. Concerning scale efficiency, large and medium hospitals had a right-skewed distribution, while the density curve for small hospitals was approximately flat, suggesting that large hospitals are more able to achieve economies of scale. A considerable difference in median scale efficiency scores by hospital size was also observed: 0.76 for small hospitals in contrast to 0.83 and 0.93 for medium and large hospitals.
Efficiency also varies by type of healthcare provider (Fig. 2). Public hospitals showed the worst performance for both technical and scale efficiency. The comparison of the density curves for the efficiency scores revealed that these differences are pronounced mainly for technical efficiency. Private hospitals presented a left-skewed distribution with a peak around 1 and a median score of 0.69, suggesting that those are the most efficient hospitals in the country (Fig. 2C). The median scale efficiency score was also higher for private hospitals (0.88). Public hospitals presented a median technical efficiency score of 0.51 and a scale efficiency score of 0.78, while philanthropic hospitals had median scores of 0.62 and 0.86, respectively. Figure 2e to j show the density curves disaggregated by size and type of health provider. For technical efficiency, the curves for private hospitals are right-skewed independently of hospital size, evidencing again that this group comprises the most efficient hospitals.
Regardless of size and healthcare provider, most hospitals in Brazil have increasing returns to scale (87%), suggesting that the majority of Brazilian hospitals were operating below the optimal scale size (Fig. 3). This percentage decreases monotonically with hospital size, underlining that some large hospitals, such as most large public hospitals, have already achieved scale efficiency.
The slack analysis showed potential savings of beds and human and technological resources as well as output expansion opportunities according to hospital size (Fig. 4). This analysis revealed that there is room to reduce beds, human resources and amounts of equipment, regardless of hospital size. Differences in output expansion by size reinforce the presence of available beds in small Brazilian hospitals. To achieve efficiency, small hospitals should increase hospitalizations by 26% on average, followed by 16% among medium hospitals and 9% among large hospitals. This increase corresponds to 16, 38, and 74 more hospitalizations per month for small, medium, and large hospitals, respectively.
Source: CNES and SIH/SUS, 2015 [34, 35].
3.2 Spatial pattern assessment
The spatial analysis shows that technical and scale efficiencies are heterogeneously distributed throughout the country, with hot spots of efficiency (Fig. 5). Areas in light gray represent the hospital neighborhoods with the lowest scores, while the darkest black ones correspond to scores above the Brazilian average. The totally efficient hospitals (scores equal to 1), in terms of both scale and technical efficiency, are displayed as black dots.
Technical and scale inefficiency are widespread across the country, reflecting the presence of small hospitals in a greater number of localities. The concentration of technical and scale inefficiency is mainly observed in less developed regions, including Amazonas State and the Northeast and Midwest regions.
Globally, efficiency scores show low levels of spatial correlation: the global Moran indexes for technical and scale efficiency are 0.126 and 0.152, respectively. Both are pseudostatistically significant at 0.001. Local efficiency scores also suggest a few pockets of significant spatial hospital inefficiency autocorrelation (Fig. 6). Negative spatial autocorrelation is scarce, and different patterns are observed for positive autocorrelation. Even though inefficiency is widespread in almost all Brazilian states, clusters of technical and scale inefficiency (low-low in light gray) are found mainly in Amazonas State and the Midwest region. On the other hand, some clusters of technical efficiency are observed, in particular for the Southeast region and the southern parts of Pará and Maranhão (Fig. 6).
4 Discussion
This is the first study to evaluate hospital efficiency while taking into account all Brazilian general hospitals. We found two main results. First, inpatient care is provided with a high level of inefficiency. Second, this inefficiency is not a regional phenomenon and is distributed across all Brazilian states.
Since the SUS was created, the Brazilian health system has experienced several changes, improvements and challenges: for instance, an imbalance between income and expenses, a lack of human resources specialized in hospital management, and increasing costs as a function of technological, demographic and epidemiological changes [9]. There is a lack of studies concerning hospital efficiency for Brazil as a whole. The literature concerning access to and utilization of hospitalization is scarce compared to research on outpatient services [9]. La Forgia and Couttolenc [23] found an average technical efficiency score of 0.34 for Brazilian hospitals in 2002. This very low average score casts doubt on the validity of their findings. Our paper shows that Brazilian hospital efficiency (0.59) is below the average OECD score, which ranges from 0.77 to 0.82 [49]. Hospital inefficiency arises mainly from barriers to achieving scale and implementing management best practices. A large number of hospitals are local, public, and small as a likely consequence of the decentralization principle of the Unified Health System. Even though decentralization can better match local needs, it sometimes fails to achieve scale and technical efficiency requirements [4, 8, 21, 43], implying a scenario where persistent inefficiency is likely to be observed [13]. Local governments are responsible for the provision of access to all healthcare services, either directly or by contracting inpatient care from other municipalities. The mayors’ decisions depend on political incentives, which are not always aligned with principles of economic efficiency or with the local population’s wellbeing in the long run [21]. The autonomy to control the opening of new local hospitals translates into powerful political capital for local governments ([17, 23, 32]). By neglecting the presence of externalities and scale and scope economies, mayors create barriers to the development of a healthcare services network. The size of the Brazilian territory is another aspect to consider when assessing hospital efficiency. Brazil is a continental country with a large number of small municipalities with low levels of population density. The combination of political incentives with the particular geographical setting of the country results in an excessive number of small hospitals with low levels of effective healthcare provision throughout the territory [42].
The federal government has already made some effort to counterbalance SUS decentralization by trying to organize healthcare supply into micro and macro health regions [29]. These initiatives failed to organize healthcare delivery in a hierarchical and integrated network, mainly because of financing constraints [38]. The Federal government is allowed to transfer money only to states or municipalities, which discourages local authorities from building healthcare networks by region or even by consortia. Decentralization, therefore, is still a challenge to the achievement of efficient provision of inpatient care within the Unified Health System.
Brazilian hospital performance also varies according to the type of healthcare provider. Private hospitals showed the highest technical efficiency scores, while public hospitals showed the lowest. These findings are in tandem with La Forgia and Couttolenc [23], who found that public hospitals administered by Health Social Organizations, called OSSs, were the most efficient group, followed by for-profit hospitals. OSSs are characterized by having an autonomous administrative arrangement, suggesting that higher autonomy can lead to better hospital management. Management autonomy is common among private hospitals, which are free to introduce payment based on performance, thus favoring efficiency [23, 33, 51]. In addition, private hospitals do not have to account for local political interests and constraints and can make decisions more rapidly and develop network configurations with other hospitals, thus exploiting economies of scale, knowledge exchange or centralization of input purchases [16, 21]. Therefore, cooperation across hospitals seems to have greater effects on hospital quality and efficiency than local policy intervention [27]. Large public hospitals play an important social role. These hospitals, despite presenting lower levels of technical efficiency than private and philanthropic hospitals, have an important role in providing high-complexity services, receiving a large proportion of SUS patients from other municipalities and dedicated mainly to the most socioeconomically vulnerable population [47]. Thus, these reasons, associated with specific medical choices, such as waiting for complementary tests, results of tests performed, or medical decisions regarding treatment, might be among the obstacles causing delay to hospital discharge in large public hospitals [47]. These discharge delays and the consequent high occupancy rates are especially frequent for nonresidents, who usually travel long distances and have difficulties in finding a place to stay. In these situations, doctors avoid authorizing hospital discharges.
This paper is a step forward in the assessment of hospital performance in Brazil. In contrast to many previous studies that focused on restricted samples ([3, 10, 19, 23, 24, 26, 30, 31, 46, 48]) or a particular hospital size [42], our analysis encompasses all general hospitals in the country. The only exception that provides a nationwide estimate of efficiency in healthcare expenditure is the study conducted by the World Bank [50]. The study measures inefficiency at the municipal level for health units offering medium- and high-complexity procedures, which makes the analysis not directly comparable with ours. Both studies, however, found an overall level of inefficiency, implying that there is room for optimization. Although the report suggests a reallocation of financial resources to primary healthcare, we contend that other forms of reallocation may be equally efficient and meet equity concerns [4, 8, 43]. Inequalities in access and the matching of demand and supply must thus be carefully considered in any attempt to reorganize the hospital system in Brazil.
This study presents some limitations. First, variables from the CNES only account for the quantitative dimension of healthcare. Measures of the quality of care, such as the level of technology used and the quality of services provided by health professionals – including their expertise – are all key aspects of healthcare supply but are not available in the data used in this study. Second, data regarding expenses do not consider outpatient care and complementary public financial transfers to hospitals, limiting analysis using this variable. Thus, the expense variable was not used in our DEA model. Third, health professionals, despite being mostly dedicated to inpatient care, can sometimes perform outpatient care, but the information available does not allow us to make this identification precisely. Fourth, despite the recognized reliability of the CNES [41], the database has not been systematically audited. As a consequence, contemporary changes in the structure of healthcare provision may be underreported. Fifth, the analysis of efficiency for hospitals detailed by OSSs was not possible using CNES data. The administrative records provide no reliable identification of OSS units for two reasons: this type of organization is relatively new in Brazil, and contracts are constantly renewed, making it difficult for the administrative records to track these updates. Since some studies found that OSSs were the most efficient healthcare units [23] and given the increasingly favorable environment towards public-private partnerships, future studies should pay more attention to the performance of this type of initiative. Despite these limitations, the results are timely, measured at the most appropriate unit of analysis, and based on a method that is widely used in the efficiency literature.
References
Anselin L. (2016). Local spatial autocorrelation clusters. The Center for Spatial Data Science. The University of Chicago. https://spatial.uchicago.edu/sites/spacial-data.uchicago.edu/files/6a_local_SA_r.pdf, accessed 15 February 2019
ANS. (2013). Ministério da Saúde. Brasil: National Agency of Suplementary health (ANS). Essential Hospital Indicators Datasheets. http://www.ans.gov.br/texto_lei_pdf.php?id=1575, accessed May 2018
Araújo C, Barros CP, Wanke P (2014) Efficiency determinants and capacity issues in Brazilian for-profit hospitals. Health Care Manag Sci 17(2):126–138
Avdic D (2016) Improving efficiency or impairing access? Health care consolidation and quality of care: evidence from emergency hospital closures in Sweden. J Health Econ 48:44–60
Banco Central do Brasil (2015). Exchange rate - R$/US$. Brasília. https://www3.bcb.gov.br/expectativas/publico/en/serieestatisticas, accessed January 2018
Bogetoft P, Otto L. (2010). Benchmarking with DEA, SFA, and R (Vol. 157).Springer Science & Business Media
Botega LA, Andrade MV, Guedes GR. 2020. Perfil dos Hospitais do Sistema Único de Saúde. Revista de Saúde Pública
Capps C, Dranove D, Lindrooth RC (2010) Hospital closure and economic efficiency. J Health Econ 29(1):87–109
Castro MSMD (2006) Desigualdades sociais no uso de internações hospitalares no Brasil: o que mudou entre 1998 e 2003. Ciência & Saúde Coletiva 11:987–998
Cesconetto A, Lapa JDS, Calvo MCM (2008) Avaliação da eficiência produtiva de hospitais do SUS de Santa Catarina, Brasil. Cadernos de Saúde Pública 24:2407–2417
Chen A, Hwang Y, Shao B (2005) Measurement and sources of overall and input inefficiencies: evidences and implications in hospital services. Eur J Oper Res 161(2):447–468
Collins C, Araujo J, Barbosa J (2000) Decentralising the health sector: issues in Brazil. Health Policy 52(2):113–127
Colombi R, Martini G, Vittadini G (2017) Determinants of transient and persistent hospital efficiency: the case of Italy. Health Econ 26:5–22
Cooper WW, Seiford LM, Zhu J. (2004). Data envelopment analysis.In handbook on data envelopment analysis (pp. 1–39). Springer, Boston, MA
Cooper WW, SeifordLM TK et al (2007) Some models and measures for evaluating performances with DEA: past accomplishments and future prospects. J Prod Anal 28(3):151–163
Czypionka T, Kraus M, Mayer S, Röhrling G (2014) Efficiency, ownership, and financing of hospitals: the case of Austria. Health Care Manag Sci 17(4):331–347
Ferraz C and Finan F. (2005). Reelection incentives and political corruption: evidence from Brazil’s municipal audit reports.University of California, Berkeley
Ferreira DC, Nunes AM, Marques RC (2018) Doctors, nurses, and the optimal scale size in the Portuguese public hospitals. Health Policy 122(10):1093–1100
Gonçalves AC, Noronha CP, Lins MP, Almeida RM (2007) Análise Envoltória de Dados na avaliação de hospitais públicos nas capitais brasileiras. Rev Saude Publica 41:427–435
Gragnolati M, Lindelow M, Couttolenc B. (2013). Twenty years of health system reform in Brazil: an assessment of the Sistema Único de Saúde. The World Bank
Herr A, Schmitz H, Augurzky B (2011) Profit efficiency and ownership of German hospitals. Health Econ 20(6):660–674
IBGE. (2015). Bases Cartográficas. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística (IBGE)https://mapas.ibge.gov.br/bases-e-referenciais/bases-cartograficas/malhas-digitais, accessed March 2019
La Forgia GM, Couttolenc BF. Hospital performance in Brazil: the search for excellence (English). Washington, DC: World Bank. 2008. Disponível em: http://documents.worldbank.org/curated/en/815061468015870054/Hospital-performance-in-Brazil-the-search-for-excellence
Lins ME, Lobo MSDC, Silva ACMD et al (2007) O uso da Análise Envoltória de Dados (DEA) para avaliação de hospitais universitários brasileiros. Ciência & Saúde Coletiva 12:985–998
Lins MPE, Netto SOA, Lobo MCS (2019) Multimethodology applied to the evaluation of healthcare in Brazilian municipalities. Health Care Manag Sci 22(2):197–214
Lobo MSC, Rodrigues HC, André ECG et al (2016) Análise envoltória de dados dinâmica em redes na avaliação de hospitais universitários. Rev Saude Publica 50:22–22
Longo F, Siciliani L, Gravelle H et al (2017) Do hospitals respond to rivals' quality and efficiency? A spatial panel econometric analysis. Health Econ 26:38–62
Lu GY, Wong DW (2008) An adaptive inverse-distance weighting spatial interpolation technique. Comput Geosci 34(9):1044–1055
Malachias I, Leles FAG, Pinto MAS et al. (2011). Plano Diretor de Regionalização da Saúde de Minas Gerais (PDR-MG). Belo Horizonte
Marinho A (2001) Estudo de eficiência em alguns hospitais públicos e privados com a geração de rankings. In: Texto para Discussão, (794). Econômica e Aplicada, Instituto de Pesquisa
Marinho A (2003) Avaliação da eficiência técnica nos serviços de saúde nos municípios do Estado do Rio de Janeiro. Rev Bras Econ 57(3):515–534
Mello L, Lago-Peñas S. (2013). Local government cooperation for joint provision: the experiences of Brazil and Spain with inter-municipal consortia. The challenge of local government size. Theoretical perspectives, international experience, and policy reform. Edward Elgar, Cheltenham, 221-241
Miller G and Babiarz KS. (2013). Pay-for-performance incentives in low-and middle-income country health programs (no. w18932). National Bureau of Economic Research
Ministério da Saúde. (2015a). Cadastro Nacional dos Estabelecimentos de Saúde. Rio de Janeiro: Ministério da Saúde, DATASUS. http://datasus.saude.gov.br/informacoes-de-saude/servicos2/transferencia-de-arquivos, accessed 30 August 2018
Ministério da Saúde. (2015b). Sistema de Informações Hospitalares. Rio de Janeiro: Ministério da Saúde, DATASUS. http://datasus.saude.gov.br/informacoes-de-saude/servicos2/transferencia-de-arquivos, accessed 30 August2018
Ministério da Saúde. (2017). Contas do SUS na Perspectiva da Contabilidade Internacional – Brasil, 2010–2014
Mosca I (2007) Decentralization as a determinant of health care expenditure: empirical analysis for OECD countries. Appl Econ Lett 14(7):511–515
O'Dwyer G, Konder MT, Machado CV et al (2013) The current scenario of emergency care policies in Brazil. BMC Health Serv Res 13(1):70
OECD. (2015). Health at a glance 2011. OECD indicators, OECD publishing, Paris. https://doi.org/10.1787/health_glance-2015-en, accessed February, 15, 2016
Pires MBN, Oliveira R, Alcantara CCV, Abbas K (2017) A Relação entre a Remuneração do Sistema Único de Saúde, os Custos dos Procedimentos Hospitalares e o Resultado: Estudo nas Santas Casas de Misericórdia do Estado de São Paulo. RAHIS 14(3)
Rocha TAH, Silva NCD, Barbosa ACQ, Amaral PV, Thumé E, Rocha JV, Alvares V, Facchini LA (2018) National registry of health facilities: data reliability evidence. Ciencia & Saúde Coletiva 23(1):229–240
Rodrigues JM, Torres HOG, Barbosa ACQ et al. (2016). Gestão de Recursos Humanos e desempenho hospitalar na perspectiva da eficiência: um estudo em hospitais brasileiros de pequeno porte. Universidade Federal de Minas Gerais
Schmitt M (2017) Do hospital mergers reduce costs? J Health Econ 52:74–94
Sherman HD. (1984). Hospital efficiency measurement and evaluation: empirical test of a new technique. Med Care, 922–938
Sherman HD, Zhu J. (2006). Service productivity management: improving service performance using data envelopment analysis (DEA). Springer Science & Business Media
Souza IV, Nishijima M, Rocha F (2010) Eficiência do setor hospitalar nos municípios paulistas. Economia Aplicada 14(1):51–66
Silva SAD, Valácio RA, Botelho FC, Amaral CFS (2014) Reasons for discharge delays in teaching hospitals. Revista de saude publica 48(2):314–321
Souza PCD, Scatena JHG, Kehrig RT (2016) Aplicação da Análise Envoltória de Dados para avaliar a eficiência de hospitais do SUS em Mato Grosso. Physis: Revista de Saúde Coletiva 26:289–308
Varabyova Y, Schreyögg J (2013) International comparisons of the technical efficiency of the hospital sector: panel data analysis of OECD countries using parametric and non-parametric approaches. Health Policy 112(1–2):70–79
World Bank (2018) Propostas de Reformas do Sistema Único de Saúde Brasileiro – Uma nota de política econômica, working paper. World Bank, Brasília
Werner RM, Kolstad JT, Stuart EA, Polsky D (2011) The effect of pay-for-performance in hospitals: lessons for quality improvement. Health Aff 30(4):690–698
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• This is the first study to estimate technical and scale efficiency using Data Envelopment Analysis for all Brazilian general hospitals.
• Brazilian hospitals operate, on average, on low levels of technical and scale efficiency, but efficiency varies by hospital size and by healthcare provider.
• Most of the hospitals operate on increasing returns to scale, suggesting that there is room for resources optimization.
• Hospital inefficiency can be found in units across all Brazilian states.
• Municipalities with higher levels of human development concentrate a larger share of hospitals with higher technical efficiency.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
de Almeida Botega, L., Andrade, M.V. & Guedes, G.R. Brazilian hospitals’ performance: an assessment of the unified health system (SUS). Health Care Manag Sci 23, 443–452 (2020). https://doi.org/10.1007/s10729-020-09505-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-020-09505-5