Abstract
Neonatal, infant, and Under-five mortality remain high with a slight improvement over the decades in Nigeria. This paper identifies the effect of maternal and health care practices on under-five survival in Nigeria. This study considers the risk of dying for 0–60 months children with identification of the time period of survival to death across the six geopolitical regions in Nigeria. The study uses data from the Demographic and Health Survey 2018 being the latest in Nigeria to explain the underlying factors associated with under-five mortality. The Kaplan Meier analysis and the Cox proportional regression were used to estimate the time between the period of birth and the event of death. Findings revealed that up to 71% of death in under-five children occurred between 0 and 12 months with a decrease in risk found as age increase after 24 months. All death occurred in children with no intake of any vaccination, 69% in children not delivered at government or private health centres, and 74% in rural communities, Result of the Cox proportional hazard regression indicates that mother’s age 15–30, education, poor nutrition and unchecked breastfeeding practices after birth increases the hazard of child mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mothers, infants, and children's well-being remains an important public health goal for the attainment of the Sustainable Development Goal. Substantive progress in child survival across the world led to a 59% rapid drop of under-five mortality from 93 deaths per 1000 livebirths to 38 deaths per 1000 live births in 2019 (UN IGME 2020). Infant mortality reduced by 54% from 61deaths in 1994 to 28 deaths per 1000 live births in 2019 (UN 2020). Sub-Saharan Africa remains the region with the highest under-five mortality rate despite the 58% drop from 180 deaths per 1000 livebirths in 1990 to 76 deaths per 1000 live births in 2019; an indication of a child out of thirteen dying before reaching age five (UN IGME 2020).
The risk of dying is highest for children at early stage of life with majority of death occurring at the first week of birth and mostly within the first month (UN IGME 2017). Living for under-five children starts from their conception which is influenced by their environment and household structure (Evans 2004). In Nigeria, neonatal, infant, and under-five mortality are high, Nigeria Demographic and Health Survey (NDHS 2018) reported that from 2008 to 2018, neonatal mortality stagnated at 40 to 39 deaths in 1000 live births, infant mortality reduced from 75 to 67 deaths while under-five mortality reduced from 157 deaths per to 132 deaths per 1000 live births.
A growing body of literature identifies that the underlying factors of under-five children health may be inherent in the institutional norms and practices associated with their childbirth, based on the characteristics of the parents, family, and community of the child (Adedini et al. 2015; Shapiro and Tenikue 2017; Olawuwo et al. 2018). The preceding birth length to conception, mothers’ age at childbirth, and the birth order was considered important as fertility-related behaviour influencing under-five mortality (Rutstein and Winter 2014).
Regional differential in under-five mortality rates across the six geo-political regions in Nigeria, has been attributed to socio-economic factors, beliefs and norms (Adedini et al. 2014; Akinyemi et al. 2013). Attributes of individual, mother, and community level on the risk of mortality in under-five children were found in Sierra Leone with evidence of regional variations (Liwin and Houle 2019), and the suggestion of the incorporation of targeted interventions based on regional disparities. Some community attributes were found with the risks of dying before age-five over intermediate factors in 28 sub-Sahara African countries (Boco 2010).
Studies in Nigeria have generally concentrated on the significant relationship between child mortality and individual-level characteristics (Akinyemi et al. 2019; Fayeun and Omololu 2011) while few recently considered community-level characteristics on children's health outcomes at the national and aggregate base with historical data (Adedini et al. 2013; Adekanmbi et al. 2013). Accurate measures and estimates of mortality are important and crucial for assessing child survival and risk of dying. As a higher proportion of under-five mortality in Nigeria occurred during neonatal, this study investigates how the basic factors of child health at birth measured by child weight at birth, place of birth: in health facilities or not, baby postnatal check on breastfeeding, and vaccination received contributes to survival in children within 0–60 months in Nigeria.
This paper uses Demographic and Health Survey (DHS) 2018 dataset in Nigeria to observe factors associated with under-five death and what category of variables can explain such variations. We considered the Cox proportion regression model which takes care of correlation from the clustering associated with national representative survey. From the methodological point of view, statistical models that ignore this type of clustering can make the study results biased because they violate the assumption of independence of event times.
The paper proceeds as follows: Sect. “Under-five survival and healthcare in Nigeria” presents literature on factors of under-five child survival and healthcare in Nigeria; Sect. “Data and Methods” focuses on the data, and methods; Sect. “Results”, presents the results, and findings; Sect. “Discussion”, discusses the implications of the findings and Sect. “Conclusions” draws out the conclusion of the study.
Under-five survival and healthcare in Nigeria
Regional inequalities in under-five survival in Nigeria
Variation in under-five mortality abounds with causal factors attributed to inequalities in parents’ education, and household wealth index. Regional differences abound in quality and pattern of life due to circumstances of childbirths (Garcia 2020; Oris and Fariñas 2016) which affect children's health outcomes as most of the children live in rural areas in many countries. In Nigeria, under-five mortality in rural areas is higher (157 deaths per 1000 livebirths) than urban areas (92 deaths per 1000 live births) and the national aggregates of 132 deaths per 1000 livebirths (NDHS 2018).
Dahiru (2015) found significant variations in neonatal mortality in Nigeria based on geographical settings with the risk of dying higher in the rural than in urban areas. Similar substantial levels of infant death clustering in Nigeria, are prevalent in North East, North West, and North Central, but common in all the other three southern regions; southeast, South-South, and South West (Akinyemi et al. 2019). Children survival has been linked to childbearing pace and age of mothers (Yaya et al. 2017). Childbirth in Nigeria is associated with low spacing between births, median birth interval gaps is 30.9 months with no difference recorded in past 18 years (NDHS 2018). The acceptable minimum of 36 months has not been attained in decades in Nigeria, thus making it possible for women to have many children at a short pace of years. Under-five mortality with mothers having more than six childbirths stood highest at 190 deaths per 1000 live births in 2018. Specifically, women who have too many births and those with births that often occur too close together have the unpleasant experiences of child survival.
Studies have shown that education is important in maternal reproductive decisions. Women who attain a higher level of education are more likely to marry later, play significant roles on issues pertaining to themselves and their children, be well informed on reproductive care and practices and their children are therefore likely to be well nurtured and enjoy better health (Gayawan et al. 2016), generally, non-educated mothers have more child deaths than others (Grepin and Bharadwaj 2015).
Childbirths and poor healthcare factors in Nigeria
About a third of all neonatal deaths tend to occur on the day of birth and close to three quarters die in the first week of life in developing countries (Sankar and Jeeva 2016), thus suggesting that the periods of birth and the following birth period is essential for the survival of new-born lives. Although coverage of vaccination for children has improved in Nigeria in the past 10 years, basic vaccination and immunization remain low with 19% of children age 12–23 months receives no-form of vaccination while only 31% receive all the basic vaccinations of Bacille Calmette-Guerin (BCG), Diphtheria-Pertussis-Tetanus (DPT), Haemophilus influenzae type b (B-Hib) and Polio (NDHS 2018).
Regional disparity is seen in intake of vaccination and immunisation routine in Nigeria. NDHS 2018 reported that vaccination coverage among children age 12–23 months is highest in Anambra state (76%) in the Southeast region and lowest in Sokoto state (5%) in the Northwest region of Nigeria. Across region, Bacille Calmette-Guerin (BCG) vaccination intake has the highest record in Southeast (93.4%), Southwest (90.6%), Southsouth (83.9%), Northcentral (74.4%), Northeast (57%) and least in Northwest (47%). Urban children have a higher chance of meeting all basic vaccination coverage than rural children (44% versus 23%) in 2018. Basic vaccination coverage also increases with the mother's level of education, and household wealth.
The weight of a new-born is seen as a measure of public health problems on maternal health, and malnutrition during pregnancy. The development and growth of babies during pregnancy is reflected by the weight at birth. Foetal and neonatal morbidity is closely related with low weight at birth which inhibited the cognitive development and growth of neonates making them prone to chronic diseases in early and later life (Negrato and Gomes 2013). Breastfeeding duration and early initiative is an important factor of growth and development in neonates. Breastfeeding patterns, time of initiation, and nature of practice have a significant relationship with infant mortality in Nigeria (Bankole and Adetutu 2015).
Hunger and malnutrition also affect child health. An estimated 2.5 million under-five Nigerian children suffer severe acute malnutrition (SAM) yearly (UNICEF 2015). The nutritional status of under-five children in Nigeria is poor with, 37% stunted, 7% wasted and 22% underweight (NDHS 2018). 68% of children age 6–59 months is anaemic with 73% and 62% from rural and urban areas respectively. Regional differences exist with stunted children higher in the Northwest region with 57% while Southeast recorded 18%. Across the state, stunting is lowest in Anambra (14%) and highest in Kebbi (66%).
Data and methods
Data source
The Demographic and Health Survey (DHS) database in Nigeria, which sourced data from a cross-sectional study with information on nationally selected samples serving as a representative of a nation in rural, urban, and regional zones is used. DHS dataset is presented in different groups recode files and this study concentrate on the children recode file on mothers with births in the past five years which provides information on children within age 0–60 months born in the 5 years prior to the surveys. Implementation of six surveys of the Nigeria DHS has been conducted by the National Population Commission and this study uses NDHS 2018 dataset to estimate our analysis with 33924 observations with a record of 3211 mortality in all the six geopolitical regions of Nigeria.
Description of variables
Outcome variable: The dataset considered those children who were born within the preceding five years from the survey year 2018. The outcome is the hazard of dying before reaching 56 months. Among the children, those who died before reaching their 5th birthday were treated as failure cases and classified as the dependent variable of analysis.
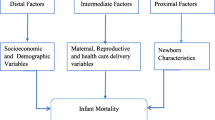
Explanatory variables: Our key explanatory variables focus on child health at birth measured by child weight/size at birth, whether child health was checked after discharge, baby postnatal check on breastfeeding within 2 days of delivery, and hospital discharged and vaccination and immunization received at birth. Other control variables comprise maternal and household characteristics comprising of mothers place of residence, region, education, religion, wealth status, place of delivery, and the preceding birth interval.
Ethical considerations
The demographic and health survey program has ethical approval for the survey and obtained informed consent from each respondent. Approval to use the NDHS datasets for this research was obtained by the author from the DHS.
Method of analysis
Descriptive statistics were computed with the use of frequency and percentage distribution. The measure of association between the outcome variable and its explanatory factors were established with survival analysis measured by Cox proportion hazard regression and the Kaplan Meier graph in the Stata software 13.0 version. The survival analysis help analyze the length of time between the time of birth and the event of death. The probability of the endpoint occurring (death,) is called the hazard. The duration of survival in months was used as the risk of death in childhood which was a time-to-event data; an indication of the length of survival of the child before death. The Cox proportional regression analysis considers the history of an event in examining the factors of death risk. The main advantage of this model is that it accounts for the problem of censoring data.
The hazard is modelled as: \(H_{t }\) = \(H_{0} \left( t \right) \times {\text{exp}}(b_{1} X_{1} + b_{2} X_{2}\) + …\(b_{n} X_{n} )\).
By dividing both sides of the above equation by H0(t) and taking logarithms, we obtain:
where \(t\) is the survival time; \(H\left( t \right)\) is the hazard function determined by a set of covariates (\(X_{1} ,X_{2} ,...,X_{n}\)). The coefficients (\(b_{1} ,b_{2} ,...,b_{n}\)) measure the size/impact of covariates and \(H_{0}\) is the baseline hazard. Time \(t\) indicates the hazard may vary over time.
The quantities \(exp\left( {b_{i} } \right)\) are called hazard ratios (HR). A hazard ratio greater than zero, or equivalent to one, indicates that as the value of the \(ith\) covariate increases, the event hazard increases and thus the length of survival decreases.
Results
Descriptive analysis
A total of 3211 deaths out of 33,924 under-five births were captured by this study and reported in Table1 and 2. About 61% (1947 out of 3211) of this mortality is associated with mothers within age 15–30 and 39% (1264 out of 3211) is within ages 31–49. 58% (1864 out of 3211) child death is found in mothers with no form of education, 22% (710 out of 3211) had secondary, 15.6% (498 out of the 3211) had primary education and only 4.3% (139 out of 3211) had higher education. About 80% (2573 out of 3211) occurred in the north (1371 in Northwest, 730 in North east, 472 in the North central). Rural place of residence has 74% (2368 out of 3211), households practising Islam had 72% death (2299 out of 3211), household classified as poorest and poorer wealth status captures 30% (985 out of the 3211) and 28% (904 out of 3211) respectively.
Up to 78% (2501 out of 3211) had less than the recommended 36 months gap in births preceding their birth. On place of delivery; only 992 out of 3321 (31%) births were delivered at any government or private hospital and health clinic while other delivery of 2219 out of 3321 (69%) were at respondent home and other homes. 595 out of 3321 (19%) had small weight at birth, 1551 of 3321 (48%) were recorded as an average weight while those with baby weight classified as large were 982 out of 3321 (30.1%) responses with don’t know is 83 out of 3321 (2.6%), NDHS 2018 classified weight of baby at birth into five groups and for this study; “very small and smaller” was classified as small and “very large and larger than” classified as large and those in average group remains. On breastfeeding; only 117 out of 3211 death (3.6%) had record of breast-feeding checked within two days of delivery by medical practitioner. No form of vaccination (BCG, DPT and Hepatitis B) was received by all the 3211 deaths.
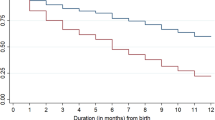
From these descriptive statistics; U-5 deaths were predominant in the Northern region than the South, common among Islamist and dominant in the rural areas. On health factors, child mortality is associated with non-delivery of child at hospital and health centres, common with under-weight babies and closely associated with babies whose breastfeeding were not adequately monitored within 2 days of delivery. All under-five mortality had no record of received immunization (BCG, DPT and Hepatitis B). Statistics in Table 2 also indicates that 2266 of 3211 children (71%) death occurred within 0-12 months of delivery; thus signifying the presence of high infant mortality in Nigeria. Although the northwest had the highest percentage of under-five mortality, 62% (844 out of 1371) of these deaths occurred in 0–12 months of births while the south-south has about 82% deaths (149 out of 181) in 0–12 months. The Kaplan–Meier function presented in Fig. 1 indicates the time period of death from 0–60 months. This result shows a low survival probability among new-born babies in early stage of life with a quick drop in the function till about 24 months; an indication that mortality risk was highest for 0–24 month’s children and decrease in risk is found in increase in ages after 24 months.
Cox proportion hazard result
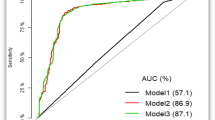
This section presents the result of the cox proportional regression on time of survival of childbirth 0–60 months in NDHS 2018.
The result presented in Table 3 revealed that the entire six regions has a high risk of mortality with significant risk highest in southsouth(HR = 1.51, p < 0.01), southeast(HR = 1.48, p < 0.01) and in the northeast(HR = 1.42, p < 0.05); an indication that these regions have increased risk of death compared to the southwest. The risk of dying is higher among children with mothers within age 15–30(HR = 1.11, p < 0.05) and with mothers with secondary school education (HR = 1.26, p < 0.05), thus signifying that children associated with these factors have a lower survival rate between 0-60 months, with their death occurring in infancy. Children whose breastfeeding was not checked within two days of delivery have a higher ratio of dying (HR = 1.2, p < 0.001); an indication that such children have lower months of survival. We can deduce that it is not only the time breastfeeding start that is important to the survival of a child but adequate breastfeeding should be given with proper care.
Other factors of rural residence, household wealth status and small weight of the baby at birth has high hazard ratio with dying although these results are not significant with their confidence interval passing through 1, and the hazard ratios decline gradually when a child is of an average or large size at birth. Further clarification of the association of mothers and household characteristics on child mortality with the total population (33,924) women with children of 0-60 months in the last five years in NDHS 2018 presented in Table 4 revealed that the northwest, northeast, and the southeast have a high odd ratio greater than one than the southwest and the south-south. Mothers with higher, secondary education have a lower odd ratio of child mortality than those with no education. Religion (other church and Islam) have a higher odds ratio with child mortality but their effect on the time of survival is not significant; thus religion has no significant effect on the space and timing of the death of under-five in most regions. The effect of household wealth also has an effect on child mortality in Nigeria with the richest, richer, and middle class having a lower odd ratio than the poorest group.
Discussion
Evidence of variation in under-five survival is established in Nigeria with the 2018 DHS dataset of 0-60 months children recode file. Results across regions suggest that the Northern region has high under-five risk factors which can be attributed to maternal and household factors considered as socioeconomic factors (Akinyemi et al. 2013). The time survival analysis revealed that child mortality in south-south, southeast, and northeast has a shorter lifespan than in north-central and southwest. Mothers within age 15–30 have a higher hazard ratio with the time of child mortality; this signifies the need to control teenage pregnancy as indicated by the previous study with earlier DHS datasets in Nigeria (Adedini et al. 2014; Yaya et al. 2017). The Cox proportional hazard model revealed that women’s education has no significant effect on the time of death of under-five children but evidence of higher, secondary, and primary education was found in association with child mortality in the logistic regression result. Previous studies (Adedini et al. 2015; Akinyemi et al. 2013) have suggested there is a need to improve education in northern Nigeria towards correcting regional disparities and imbalance in Nigeria. This result is also in line with the previous study (Shapiro and Tenikue 2017) on sub-Saharan Africa which suggests that an increase in women’s education is essential to reduce infant and child mortality which will rapidly reduce the fertility rate. No record of immunization routine was found in all the cases with child mortality; a reflection of poor immunization and vaccination coverage in Nigeria. A notable effect of breastfeeding is seen on the unchecked pattern of breastfeeding in the first two days of birth having a high hazard ratio with mortality. This result indicates that adequate monitoring and check-up on breastfeeding within 2 days of delivery is essential for the development of neonates.
Conclusions
To accelerate under-five death reduction, greater attention is needed on the lives of a new-born. With a high level of under-five deaths occurring during the neonatal period, there is a need to place a critical focus on the healthy start of neonates (UN IGME 2019). Nigeria needs to improve the survival and health of new-borns through increased attention on coverage of quality antenatal care, use of skilled care at birth, postnatal care for mother and baby, and promotion of vaccination at birth for new-borns. Health care practices that promote healthy births and the survival of children should consider regional disparities. Providing essential care for new-born must be done in rural and urban areas and the management of high-risk new-borns must incorporate monitoring and at the grassroots level. Issue of teenage pregnancy is also to be discouraged with the abolishment of practices that encourage early motherhood.
Availability of data and materials
The dataset for this study is available in the online DHS archive [https://dhsprogram.com/data/available-datasets.cfm]. Permission from the DHS program is required to access the data. The principal author has obtained permission to use the dataset and anybody in need can request from DHS.
References
Adedini, S. A., Odimegwu, C., Imasiku, E. N., & Ononokpono, D. N. (2015). Ethnic differentials in under-five mortality in Nigeria. Ethnicity and Health, 20(2), 145–162.
Adedini, S.A, Odimegwu, C., Imasiku, E.N, Ononokpono, D.N, & Ibisomi, L. (2014). Regional variations in infant and child mortality in Nigeria: a multilevel analysis. Journal of Biosocial Science, 47(2):1–23.
Adedini, S. A., Odimegwu, C., Imasiku, E. N., Ononokpono, D. N., & Ibisomi, L. (2013). Regional variations in infant and child mortality in Nigeria: A multilevel analysis. Journal of Biosocial Science, 10, 1–23.
Adekanmbi, V. T., Kayode, G. A., & Uthman, O. A. (2013). Individual and contextual factors associated with childhood stunting in Nigeria: A multilevel analysis. Maternal Child Nutrition, 9(2), 244–259.
Akinyemi, J. O., Odimegwu, C. O., Banjo, O. O., & Gbadebo, B. M. (2019). Clustering of infant deaths among Nigerian women: investigation of temporal patterns using dynamic random effects model. Genus, 75, 12.
Akinyemi, J. O., Bamigboye, F. A., & Ayeni, O. (2013). New trends in under-five mortality determinants and their effects on child survival in Nigeria: A review of childhood mortality data from 1990–2008. Africa Population Studies, 2(1), 25–42.
Bankole, O. T., & Adetutu, O. (2015). Exclusive breastfeeding practice and infant survival in Northern Nigeria. Journal of Demography and Social Statistics, 2(1 & 2), 28–36.
Boco, A. G. (2010). Individual and community level effects on child mortality: An analysis of 28 Demographic and Health Surveys in Sub-Saharan Africa. DHS Working Papers No. 73. Calverton, Maryland, USA: ICF Macro.
Dahiru, T. (2015). Determinants of early neonatal mortality in Nigeria: Results from 2013 Nigeria DHS. Journal of Pediatrics and Neonatal Care, 2(5), 00089. https://doi.org/10.15406/jpnc.2015.02.00089.
Evans, G. W. (2004). The environment of childhood poverty. American Psychologist, 59(2), 77–92.
Fayeun, O., & Omololu, O. (2011). Ethnicity and child survival in Nigeria. Africa Population Studies, 25(1), 92–112.
Garcia, J. (2020). Urban-rural differentials in Latin American infant mortality. Demographic Research, 42(8), 203–244.
Gayawan, E., Adarabioyo,M.I., Okewole, D.O., Fashoto, S.G. & Ukaegbu, J.C.(2016).Geographical variations in infant and child mortality in West Africa: A geo-additive discrete-time survival modelling. Genus 72:5.
Grépin, K. A., & Bharadwaj, P. (2015). Maternal education and child mortality in Zimbabwe. Journal of health economics, 44(6), 97-117.
Liwin, L., & Houle, B. (2019). The effects of household and community context on mortality among children under five in Sierra Leone: Evidence from the 2013 Demographic and Health Survey. Demographic Research, 40(11).
National Population Commission (NPC) [Nigeria] and ICF. (2019). Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
Negrato, C. A., & Gomes, M. B. (2013). Low birth weight: Causes and consequences. Diabetology & Metabolic Syndrome, 5(1), 49.
NDHS. (2018). National Population Commission (NPC) [Nigeria] and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
Olawuwo, S., Forcheh, N. & Setlhare, S. (2018). Individual, household and community-level effects of infant and child mortality in Nigeria: A logistic regression approach. Global Journal of Health Science 10(10). Published by Canadian Center of Scienceand Education.
Oris, M. & Fariñas, D.R. (2016). New approaches to death in cities during the health transition: An introduction. In Fariñas, D.R. &Oris, M. (eds.). New approaches to death in cities during the health transition (pp. 1–16). Cham: Springer International Publishing.
Rustein, S., & Winter, R. (2014). The effects of fertility behaviour on child survival and child nutritional status: Evidence from the Demographic and Heath Surveys, 2006 to 2012. DHS Analytical Studies, No.37. Rockville, Maryland, USA: ICF International.
Sankar, M. & Jeeva, .A.,(2016). When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries’, Journal of Perinatology, 36 (Suppl 1: S1-S11).
Shapiro, D., & Tenikue, M. (2017): Women’s education, infant and child mortality, and fertility decline in urban and rural sub-Saharan Africa. Demographic Research 37(21) Research Article.
UNICEF. (2015). Nigeria Humanitarian Situation Report. New York: United Nations Children’s Fund.
United Nations Inter-agency Group for Child Mortality Estimation. (2017). Levels & Trends in Child Mortality: Report 2017, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’. (p. 2017). United Nations Children’s Fund.
United Nations Inter-agency Group for Child Mortality Estimation. (2020). Levels & Trends in Child Mortality: Report 2020, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’. (p. 2020). United Nations Children’s Fund.
UN. Department of Economic and Social Affairs, Population Division. World population prospects: The. (2019). revision. . United Nations.
Yaya, S., Ekholuenetale, M., Tudeme, G., Vaibhav, S., Bishwajit, G. & Kadio, B. (2017). Prevalence and determinants of childhood mortality in Nigeria. BMC Public Health. 17(1):485–492.
Acknowledgment
Not applicable
Funding
No fund was received from any source for this study.
Author information
Authors and Affiliations
Contributions
KFA conceptualize the topic and prepares the background, KFA and LIJ prepared the literature, the Dataset was extracted by KFA and analysed. All authors discussed the findings and approve the paper.
Corresponding author
Ethics declarations
Competing Interest
The paper has no competing interest with any work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akeju, K.F., Jegede, L.I., Oluyemo, C.A. et al. Explaining regional variations in child survival in Nigeria: Evidence from demographic and health survey. GeoJournal 87, 3091–3100 (2022). https://doi.org/10.1007/s10708-021-10420-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-021-10420-7