Abstract
Hematological malignancies (HM) developed on underlying primary immunodeficiencies (PID) are rare and of unusual features. Differentiating between malignant and non-malignant lymphoproliferation in cases of pediatric hematology and oncology and revealing their molecular predisposition demonstrate the complex interplay between PID and HM. We retrospectively studied a case series of seven pediatric patients, all with PID with manifestations raising suspicion for HM or hypereosinophilic syndrome (HES) or confirmed HM of lymphoid origin. Combined immunodeficiency (CID) without detection of a known mutated gene or with ataxia-telangiectasia (AT), STAT3 gain of function (GOF), DOCK8 deficiency, and CTLA4 deficiency were diagnosed in three, one, one, one, and one patient, respectively. Acute lymphoblastic leukemia and Hodgkin lymphoma followed by second primary Burkitt lymphoma were diagnosed in one patient with CID each, while lymphomatoid granulomatosis in one patient with AT. Lymphoproliferative disease occurred in STAT3 GOF, CTLA4 deficiency and CID, one patient each, and idiopathic HES in DOCK8 deficiency (median age at presentation of PID or any hematological manifestation: four years). Four patients underwent hematopoietic cell transplantation (HCT) for STAT3 GOF, DOCK8 deficiency and CID in one, one, and two cases, respectively (median age: 10 years). At the last follow-up, all transplanted patients were alive. Reporting on patients’ phenotype, genotype and course of disease shed light on the prevalence, characteristics, and pathophysiology of HM complicating PID. Discriminating the non-yet malignant lymphoproliferation from its malignant equivalent on the same pathophysiology background proved of additional value. Outcomes of PID after HCT, herein reported, are favorable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary immune deficiencies (PID) have gained interest in hematology and oncology, as their spectrum expanded and patients age limits extended as a consequence of increased life expectancy and recognition of possible presentations at an adult age. Malignancies with germline predisposition to cancer are part of the pathogenic spectrum of PID. Good (1973) described the association between PID and tumors, particularly ‘lymphoreticular tumors’ and leukemias in the immunodeficiency-cancer registry [1]. Since then, other registries have confirmed an excess of lymphomas in children and adults with PID mostly due to common variable immunodeficiency (CVID) [2,3,4,5]. Within the rapidly evolving indexed PID, including more than 400 single-gene inborn errors of immunity [6], the association of immunodeficiencies and immune dysregulation disorders with lymphoid malignancies is increasingly recognized and inventoried [7,8,9]. Mechanisms of carcinogenesis in PID include germline mutations in oncogenes or tumor-suppressor genes, disruption of the equilibrium of the immune system, and defective immune surveillance to malignant clones and oncogenic viruses (EBV, human papillomavirus) [10,11,12].
Hematological malignancies (HM) driven by PID represent enormous challenges in pediatric hematology and oncology because of rarity, incomplete understanding and presentation with unusual clinical and pathological manifestations. Diagnosis poses several problems like discrimination between lymphoma, benign lymphoproliferation, and inflammation, evaluation of the significance of abnormal immunological laboratory values at diagnosis of HM and of the clinical relevance of molecular findings.
The most frequent HM in PID are lymphoproliferative disorders (LPD), whereas myeloproliferative disorders (myelodysplastic syndromes and acute myeloid leukemia) complicate inherited bone marrow failure syndromes like Fanconi anemia, GATA2 syndrome and SAMD9/SAMD9L syndrome, which are also included in the International Union of Immunological Societies Phenotypical Classification of Inborn Errors of Immunity [6].
LPD in children with PID comprise non-malignant lymphoproliferation, Hodgkin and non-Hodgkin lymphomas and, less often, acute lymphoblastic leukemia (ALL). PID-associated Hodgkin and non-Hodgkin lymphoma occur in general at a younger age than their counteparts in immunocompetent children, are more often associated with EBV, and present as disseminated disease with frequent extranodal localisations [7, 13,14,15,16,17,18]. LPD may follow or, less often, precede diagnosis of PID.
Prognosis of children with lymphoid HM with PID is poorer than in children without PID [7, 13,14,15,16,17,18]. To improve outcomes, it is important to accurately diagnose LPD, achieve cure, treat infectious complications, and prevent HM. In selected patients, consolidation and HM prevention, as well as other aspects of PID like autoimmunity and immune dysregulation, can be confronted with allogeneic hematopoietic stem cell transplantation (HCT).
Taken the above into consideration, we present this case series comprising pediatric patients with (a) immunodeficiency of proven or suspected genetic etiology with or without lymphoproliferation and (b) a proven HM or an initially suspected HM on a ground of immunodeficiency, with the aim to discuss their clinical presentation, course of disease, eventual development of HM, and the role, indications and timing of allogeneic HCT.
Patients and methods
Patients
We retrospectively studied all patients with an established or subsequent diagnosis of PID and referral to the Department of Pediatric Hematology-Oncology of “Aghia Sophia” Childrens’ Hospital during the years 1995–2015 for manifestations suggesting a lymphoid hematological malignancy or a lymphoproliferative disorder or an idiopathic hypereosinophilic syndrome. We excluded patients with PID due to inherited bone marrow failure syndromes. We defined PID entities on the basis of the International Union of Immunological Societies classification [6]. The parents or legal guardians of every child gave informed consent for participation in clinical research, and a separate consent for genetic testing. The study was conducted in compliance with the principles of the Declaration of Helsinki.
Immunological studies
Immunological studies were performed by means of peripheral blood flow cytometry for T-, B- and NK-cell lymphocyte populations subsets; T-cell lymphocyte proliferation after stimulation with mitogens and antigens; serum immunoglobulins levels; vaccine antibody titers. The minimal lymphocyte subsets analyzed were: CD4 + and CD8 + T cells, CD3 + HLADR + activated T cells, CD3 + TCRαβ + , CD3 + TCRγδ + , CD3 + CD4 + CD54RA + naive helper T cells, CD3 + CD4 + CD54R0 + memory helper T cells, CD3 + CD4 + CD25 + CD127- regulatory T cells, CD19 + CD27- naive non switched B cells, CD19 + CD27 + memory switched and non switched B cells, and CD21low CD38- B cells. Adenosine deaminase-2 (ADA-2) activity in the plasma was measured in the Laboratory of Clinical Biochemistry and Metabolism, University Hospital of Freiburg, Germany.
Genetic testing
Genetic testing was performed in patients with suspected or confirmed PID. According to the patient’s clinical and immunological phenotype, sequencing was performed at the single gene level or with targeted next generation sequencing (NGS) of a panel of genes known to be associated with a given phenotype or, in case of failure to identify a genetic cause with the previous methods, with whole exome sequencing (WES). Variant annotation and interpretation in terms of clinical relevance were reported.
Targeted NGS panel included genes associated with PID such as CVID, chronic mucocutaneous candidiasis, hyper-IgE syndrome or inflammatory bowel disease: AICDA, AIRE, BBX, BTK, CARD9, CARD11, CD274, CD28, CECR1, CR2, CTLA4, DKC1, DOCK8, FCHO1, FOXP3, ICOS, IKZF1, IL10RA, IL10RB, IL17A, IL17RA, ITSN2, LRBA, MICALL2, MYH9, MYO5B, NCF2, NFKB1, NFKB2, NFKBIA, NOD2, PDCD1, PIK3CD, PIK3C2A, PIK3R1, P2RX7, PGM3, PIK3R4, PTEN, RAG1, RAG2, REL, RELA, RELB, RLTPR, SEC61A1, SH2D1A, SPINK5, STAT1, STAT3, STXBP2, TNFSF10, TNFSF13, TNFSF13B, TNFRSF13B, TNFRSF13C, TNFRSF17, TYK2, WAS, XIAP, ZNF341.
The combined immunodeficiency (CID) targeted panel included: ADA, AICDA, AIRE, ATM, BLK, BLNK, BTK, CARD9, CARD11, CD40, CD40LG, CD79A, CD79B, CFTR, CR2, CXCR4, DKC1, DOCK8, FASLG, FCGR3B, GATA2, ICOS, IFIH1, IKBKB, IKZF1, IKZF3, IL12A, IL17A, IL17F, IL17RA, IL17RC, IL21, IL21R, IL23A, IL2RG, IL6, IRAK4, IRF2BP2, IRF8, LRBA, MBL2, MCM4, MRE11A, MS4A1, NFKB1, NFKB2, NFKBIA, NHEJ1, NLRC4, NLRP12, NLRP3, ORAI1, PIK3R1, PLCG2, PMS2, PRKCD, PRKDC, RNASEH2A, RNASEH2B, RNASEH2C, RTEL1, SAMHD1, SATB1, SEC61A1, SEC61A2, SEC61G, SH2D1A, SKIV2L, SPINK5, STAT3, STIM1, TAP2, TCF3, TINF2, TLR3, TNFAIP3, TNFRSF13B, TNFRSF13C, TNCAMLG, FANCA, FANCE, MDC1, NEIL1, TWIST1, ADA2, INPP5B, SEC61B, TNFRSF11B.
WES filtering was based upon inheritance mode, zygosity, coding effect segregation and significance as defined in ClinVar database. Candidate variants that accounted for ≥ 20% of total reads with a minimum coverage of × 10 were considered. Common variants were discarded.
WES was performed in Centogene, Rostock, Germany, and in the Laboratory of the Division of Allergy/Immunology/Rheumatology/Dermatology, Boston Childrens Hospital, US, for two patients, one case each. Targeted NGS studies were performed in the Center for Chronic Immunodeficiency, University Hospital of Freiburg, Germany. Sequencing of SAP and WAS was performed in Unité INSERM U429, Hôpital Necker Enfants-Malades, Paris, France. Next-generation sequencing and Sanger sequencing of DOCK8 were performed in the Department of Laboratory Medicine DNA Sequencing Laboratory at the National Institute of Allergy and Infectious Diseases, Bethesda, US.
Results
PID and HM diagnoses of the patients and immunological, histological and genetic findings are presented in Table 1.
Cases with a proven hematological malignancy
Remote history of acute lymphoblastic leukemia and CID
A three-month-old Roma boy presented with B-cell precursor ALL without MLL rearrangement, treated with chemotherapy only. During maintenance treatment, he suffered abscesses in the vaccination sites. During a close follow-up period of eight years, his course was uneventful.
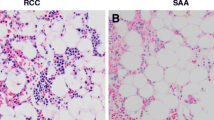
At the age of eight years, the patient presented with new-onset splenomegaly, lymphadenopathy, refractory immune cytopenias, hypogammaglobulinemia (IgG 568 mg/dl, IgA 73 mg/dl, IgM 74 mg/dl), a decrease of B cells (33/mm3) and T cells (481/mm3), and almost undetectable invariant NK/T cells. Because chemotherapy regimens for ALL would not cause long-term or late-onset immunodeficiency [31], CID was the most likely diagnosis. WES detected a homozygous mutation of NPAT (c.4274A > G, p.Lys1425Arg), a gene anecdotally involved in familial nodular lymphocyte-predominant Hodgkin lymphoma [19], as well as a homozygous mutation of BRMS1 (c.244C > T, p.Arg82Ter), a gene involved in anoikis, a cellular process defined as cell-detachment-induced apoptosis, and breast cancer metastases. Concomitant NGS with a panel of CID genes (not including NPAT or BRMS1) at another center detected a heterozygous MCM4 mutation (c.77G > A, p.Ser26Asn), a gene involved in autosomal recessive NK cell deficiency and chromosomal breakage syndrome [20, 21]. Despite intravenous immunoglobulin (IVIG) supplementation, he developed unremitting fever and lung infiltrates, posing concerns about lymphoid malignancy. However, an open lung biopsy revealed granulomatous-lymphocytic interstitial lung disease (GLILD) (Fig. 1). HCT from an unrelated fully matched donor for debilitating symptoms and prevention of lung function deterioration resulted in persistent remission of all PID manifestations without GVHD for two years.
CT scan of the chest showing areas of patchy consolidation and subpleural nodules in the boy with a remote history of acute lymphoblastic leukemia and combined immunodeficiency. Histology of an open-lung biopsy of the lesion located in the right lower lobe showed granulomatous-lymphocytic interstitial lung disease
A tale of two lymphomas: Hodgkin lymphoma (primary) and Burkitt lymphoma (second primary)
A three and a half-year-old Roma girl presented with pulmonary lesions suggesting pneumonia. However, a biopsy of a superficial lymph node revealed classical Hodgkin lymphoma of mixed cellularity type, stage IV, EBV positive. Moderate hypogammaglobulinemia (IgG 590 mg/dl, IgA 28 mg/dl, IgM 32 mg/dl), and low memory switched B cells (IgD- IgM- CD27 + : 0.5% of total B cells) without T-cell dysfunction, were all attributed to Hodgkin lymphoma. After chemotherapy according to the Euronet PHL C1 protocol, the patient achieved complete remission. After completion of chemotherapy, frequent upper respiratory infections and bronchiectases occurred. At a distance (nine months) from the end of chemotherapy, immunological workup showed severe hypogammaglobulinemia (IgG 201 mg/dl, IgA 7 mg/dl, IgM 19 mg/dl), persistently low memory and isotype switched B cells, decreased CD21 low B cells, low naive T cells, and decreased T-cell proliferation after stimulation with antigens and mitogens. Therefore, CID was diagnosed. Persistent immunodeficiency and immunoglobulin replacement needs three years after the end of chemotherapy strongly supported the primary character of immunodeficiency. Targeted NGS with a CID panel identified a heterozygous mutation of ZNF341 (c.544C > T, p.Pro182Ser), a gene linked to regulation of the JAK-STAT pathway, IL-6 immunity and autosomal recessive hyper IgE syndrome [22, 23], and of MYO5B (c.183C > G, p.Phe61Leu), a gene associated with autosomal recessive microvillous inclusion disease. Two of her three sisters were partially HLA-matched with the patient. Indication of HCT for CID was provisionally deferred because of improvement under IVIG supplementation. Three years later, she presented with enlarged mesenteric lymph nodes and ileus due to ileal wall thickening. Differential diagnosis included non-malignant lymphoproliferation and lymphoma. Histology obtained through an open biopsy showed Burkitt lymphoma of stage IV, with bone marrow infiltration. Bone marrow karyotype showed t(8;14)(q24;q32) with MYC rearrangement. The patient received intensive chemotherapy without rituximab according to BFM-NHL 2004 protocol, and, despite severe infections, including Giardia lamblia enterocolitis, reached complete remission for Burkitt lymphoma. Before treatment, EBV load in peripheral blood, measured by quantitative PCR, was 3,140 copies/mL and became undetectable within four weeks, after the first cycle of chemotherapy. Allogeneic HCT is scheduled.
Ataxia-telangiectasia and lymphomatoid granulomatosis
Ataxia-telangiectasia was diagnosed in a two and a half-year-old girl with ataxic gait and telangiectases of the conjunctivae, cutaneous granulomatous lesions, elevated alpha1-fetoprotein level, exquisite sensitivity to x-rays (10 chromatid breaks/cell after 1 Gy gamma-radiation in G2 phase), and absent ATM protein on Western blot. Immunological studies revealed low T cells (336/mm3), decreased T-cell proliferation after stimulation with mitogens (5% of the control), and low IgG (80 mg/dl) and IgA (7 mg/dl). B-cell lymphopenia eventually developed (35/mm3 vs. 330/mm3 two years earlier). The patient received regular IVIG replacement. At the age of five years, she presented with recalcitrant laryngitis with a laryngeal lesion. Three consecutive biopsies of the glottis with an interval of six weeks between the first and the third biopsy were necessary because of extensive necrosis. The third biopsy revealed lymphoproliferation with clusters of large B cells in the form of immunoblasts, Hodgkin-like and Reed-Sternberg-like cells, with an angiocentric and angioinvasive distribution. Immunophenotype of the large cells was CD79 + CD20 + BCL-2 + CD15- MUM1- LMP1 + . Lymphomatoid granulomatosis of grade 3 was diagnosed. EBV viral load by quantitative PCR in peripheral blood was 15,000 copies/mL. Rituximab 375 mg/m2, four doses, resulted in symptoms resolution and reduction to zero of EBV viral load in peripheral blood. However, central nervous system (CNS) aggressive lymphoma was eventually diagnosed. EBV viral load by quantitative PCR in cerebral tissue was 2.3 × 107 copies/mL. Severe concomitant infections (invasive aspergillosis and actinomycosis) and rapid neurological deterioration precluded administration of chemotherapy or HCT; the patient succumbed due to the CNS tumor.
Cases with an initially suspected hematological malignancy
STAT3 GOF mutation
A four-year old girl with short stature was admitted with suspicion of lymphoma because of a bulky mediastinal mass, fever, hepatosplenomegaly, pericardial, pleural, and peritoneal effusions, and skin lesions on the legs (Fig. 2). Multiple biopsies from the mediastinal mass and cytology of peritoneal fluid failed to demonstrate malignant lymphoproliferation. Histology consistently showed ill-defined granulomas. While fever continued, autoimmune hemolytic anemia developed and the patient progressively complained of arthralgia. Interferon gamma release assay for tuberculosis was non-reactive. Peripheral blood NK cells were low; other lymphocyte subsets and serum immunoglobulin levels were normal. However, decreased pro-inflammatory cytokine production after stimulation with lipopolysaccharide suggested suppression of the IFN gamma/IL-12 axis. WES revealed a de novo germline heterozygous STAT3 mutation (c.454C > T, p.Arg152Trp), a missense mutation resulting in increased transcriptional activity of STAT3 as compared to wild-type protein [24], and therefore defined as gain-of-function (GOF) mutation. A trial of interferon gamma + steroids yielded no response. The child was rapidly deteriorating with seizures and immune-mediated pancreatitis and cerebral vasculitis. After stabilization with steroids, initiation of tocilizumab, a humanized monoclonal antibody against the interleukin-6 receptor, with parallel steroid tapering, resulted in a partial response, followed by a relapse of the mediastinal mass and interstitial lung infiltrates. Also, vascular abnormalities of the lower limbs and optic neuritis appeared. After discussion with a clinician, expert on STAT3 GOF mutation, ruxolitinib, a Janus kinase inhibitor (JAK inhibitor) with selectivity for subtypes JAK1 and JAK2 was added and resulted in complete remission. After two years of tocilizumab and ruxolitinib, the patient, eight-year old then, successfully received HCT from her youngest HLA-identical brother. This donor was born during the last treatment of the patient, after a cancer-complicated pregnancy –the mother having Hodgkin lymphoma diagnosed before delivery. He was tested negative for the STAT3 GOF mutation. After HCT, the patient had a complete reversal of immunological phenotype and became independent from tocilizumab and ruxolitinib.
DOCK8 deficiency
A three-year-old girl was admitted with chronically elevated absolute eosinophil count (30 G/L). Lymphoid and myeloid causes of chronic hypereosinophilia were excluded. Her parents were unrelated; three siblings were healthy. The patient's medical history included atopic dermatitis and food allergy. Serum IgE level was markedly elevated (15,000 IU/mL). Immunological studies were within the normal reference range initially. Therefore, she was diagnosed with idiopathic hypereosinophilic syndrome (HES). A trial of imatinib, indicated in HES, failed. Over the next three years, she received interferon α-1a, combined with steroids as needed, with partial remission of eosinophilia and symptoms and normal development and quality of life. However, with time, she became infection-prone at the age of seven years, recurrent mucocutaneous herpes zoster virus infections, pyogenic perianal lesions, relapsing fever, interstitial pneumonitis, and a life-threatening pericardial S. aureus infection occurred. T-cell (233/mm3 vs. 814/mm3 two years earlier) and NK-cell lymphopenia (64/mm3 vs. 814/mm3 two years earlier) and hypogammaglobulinemia (IgG 829 mg/dl vs. 1260 mg/dl two years earlier; IgM 19 mg/dl vs. 43 mg/dl two years earlier) became apparent. Because of hyper-IgE, hypereosinophilia, and combined immune deficiency, DOCK8 deficiency was considered. Targeted gene testing revealed a homozygous DOCK8 mutation (p.N1470Vfs*8). She received HCT from her HLA-identical brother, who was a DOCK8 mutation carrier in the heterozygous state. At the last follow-up, the patient was in complete remission for three years, with complete phenotype reversal.
CTLA4 deficiency and lymphoproliferative presentation
A seven-year old girl was admitted after a traffic accident in 1995: at that point, a diffuse lymphoid hyperplasia and splenomegaly –found incidentally– aroused suspicion for lymphoid malignancy. Over the next years, she underwent multiple biopsies to rule out lymphoma. Histology consistently showed granulomas. Diffuse granulomatosis of the lungs with large macronodules, kidneys, liver, and spleen progressed. Profound hypogammaglobulinemia (IgG 47 mg/dl, IgG1 29.9 mg/dl, IgG2 8.59 mg/dl, IgG4 1.73 mg/dl, IgA 6.9 mg/dl, IgM 14.1 mg/dl versus IgG 401 mg/dl, IgG1 242 mg/dl, IgG2 < 6 mg/dl, IgG4 3 mg/dl, IgA 11 mg/dl, IgM 63 mg/dl two years earlier) developed with time. Frequent infections poorly controlled by IVIG replacement developed. Immunophenotype by flow cytometry on peripheral blood showed low CD27 + IgM and class switched B cells and low naive T cells. The patient eventually died at the age of 21 years in the context of spontaneous bacterial peritonitis, underlying chronic kidney disease, and pulmonary hypertension. Postmortem genetic testing revealed a heterozygous mutation c.208C > T, p.R70W, establishing the diagnosis of cytotoxic T-lymphocyte antigen 4 (CTLA4) deficiency [25]. The patient and her sister, who had a much milder phenotype, probably inherited the CTLA4 germline mutation from their asymptomatic father.
Combined immune deficiency and thrombotic vasculitis
A four-year-old Roma girl, daughter of consanguineous healthy parents, was admitted with immune thrombocytopenia, vasculitis, and venous thrombosis. She also had frequent infections and café-au-lait macules. Antibody deficiency (IgG 395 mg/dl, IgA 7 mg/dl, IgM 14 mg/dl), low peripheral blood NK cells, high activated T cells, low memory switched B cells (IgD- IgM- CD27 + : 1.1% of total B cells), high CD21low CD38- B cells, and decreased T-cell proliferation after stimulation with antigens in comparison with the control, supported the diagnosis of CID with immune dysregulation. Her condition worsened over the years, despite IVIG supplementation, with debilitating symptoms (failure to thrive, cachexia), profound cytopenias, lymphoproliferation and opportunistic infection (episodes of severe gingivostomatitis and pneumonia). At the age of ten years, she developed protein-losing enteropathy with histology of inflammatory bowel disease. Immune replacement became less efficient, probably because of intestinal protein wasting. In particular, weight loss, lymphadenopathy and hepatosplenomegaly repeatedly aroused suspicion for lymphoma. A CID-oriented NGS genetic panel showed heterozygous mutations in CECR1 alias ADA2 (c.1173C > G, p.His391Gln), as well as in IL10R and another two PID candidate genes, FCHO1 (c.529C > T, p.Arg177Cys) and PIK3C2A (c.399 T > G, p.Phe133Leu). Adenosine deaminase-2 (ADA2) activity was measured, because biallelic CECR1 mutations cause ADA2 deficiency (DADA2) –an autoinflammatory disorder with hypogammaglobulinemia, vasculitis, and thrombosis, and also a phenocopy of Diamond-Blackfan anemia [32, 33]. ADA2 activity in plasma was 22.10 mU/mL or 492 mU/g protein [patients: 0.0–0.91 mU/mL (0.43 ± 0.38); controls: 2.7–10.6 mU/mL (5.62 ± 1.61)]. The patient underwent HCT from a fully HLA-matched unrelated donor for failure to thrive and cachexia. Her parents, newly baptized Jehovah’s Witnesses, which further complicated delivery of care, gave their informed consent for HCT. At the last follow-up, two years after HCT, the patient was free of disease manifestations and treatment-related complications.
Discussion
In this retrospective series involving rare pediatric patients with PID and suspected or proven lymphoid cancer, distinguishing inflammation from lymphoproliferation or clonal from non-clonal proliferation was often complex. Experience of an expert hematopathologist was essential in recognizing specific histopathological patterns like atypical granulomas (the girls with STAT3 GOF and CTLA4 deficiency and the boy with a remote history of ALL and CID), granulomatous-lymphocytic interstitial lung disease (the boy with a remote history of ALL and CID and possibly, in retrospect, the girl with CTLA4 deficiency), or inflammatory bowel disease in the context of PID (the girl with CID and history of thrombotic vasculitis. A pathology classification system, defines immunodeficiency-associated LPD by incorporating the name of the lesion, associated virus, and specific immunodeficiency [34]. Monomorphic vs. polymorphic cell infiltration, monoclonal vs. polyclonal cell population and polytypic vs. monotypic immunoglobulin expression mark the extremes of the spectrum of B-cell lymphoproliferation between hyperplasia and lymphoma [34].
Studies on HM in children with PID are presented in Table 2. Hodgkin and non-Hodgkin lymphoma are the more common HM among patients with PID [5, 7, 13,14,15,16,17,18]. Age at occurrence of HM, distribution of histological types, EBV status and outcomes differ as compared with children without PID. Young age, polymorphic, atypical and extranodal EBV-positive forms and worst outcomes are features characterizing PID-driven lymphoid HM. Except for the classical lymphoid malignancies, we described here a case of lymphomatoid granulomatosis, which has not been associated previously with AT [35, 36].
A second complexity in diagnosing PID and predisposition to HM, resides in interpreting genetic results (Table 1). The situation where PID cannot be proven on the genetic level is illustrated by the case of the boy with remote history of ALL and CID, where WES revealed homozygous mutations in two genes, NPAT and BRMS1, associated with Hodgkin lymphoma and breast cancer, respectively, neither of which occurred in the patient, and a heterozygous mutation in MCM4, a recessive-trait CID gene with NK deficiency. Another example is that of the girl with two lymphomas who had a heterozygous mutation in two recessive-trait PID genes a priori irrelevant to her clinical condition. Similarly, in the girl with CID and thrombotic vasculitis, heterozygous mutations in four recessive-trait PID genes were found. Among them, ADA2 mutation was of particular interest because deficiency of ADA2 (DADA2) is a complex systemic inflammatory disorder with vasculopathy, childhood-onset polyarteritis nodosa hypogammaglobulinemia [37, 38]. A familial case with two affected brothers carrying a single mutated allele has been reported in large cohort of affected children with polyarteritis nodosa, livedo reticularis or stroke and DADA2 [38]. The two patients had undetectable ADA2 enzymatic activity whereas the patient described here had elevated ADA2 activity. Inconclusive genetic findings should be reported and revisited periodically. Genetic epistasis could explain PID and predisposition to HM in these patients with multiple mutated genes. Of interest, all three patients were of Roma origin. From a genetic point of view, communities with high rates of endogamy may be at higher risk of familial cancer, like Fanconi anemia in Roma populations. Furthermore, the high frequency of variants in these populations poses problems of donor choice for HCT.
A more straightforward genetic diagnosis of PID and predisposition to cancer could be established in the patients with STAT3 GOF mutation, DOCK8 deficiency and CTLA4 deficiency. Germline STAT3 GOF mutations in humans cause a multisystem, infantile-onset autoimmune disease with recurrent infections, lymphadenopathy, hepatosplenomegaly and various autoimmune phenomena, including autoimmune hemolytic anemia and vasculitis; all the above were observed in our patient [24]. Germline STAT3 GOF mutations are not classically associated with malignancy [24, 39]. However, somatic STAT3 GOF mutations occur in large granular lymphocyte (LGL) leukemia although with a different distribution than germline STAT3 GOF mutations associated with PID [40]. LGL leukemia was reported in a patient with germline STAT3 GOF [41] and Hodgkin lymphoma developed in a patient with SOCS1 haploinsufficiency, a recently described PID, which also results in STAT activation [42]. On the opposite sides of human disease with impaired interleukin-6 immunity, DOCK8 deficiency is a cause of hyperIgE syndrome, viral infections and significant susceptibility to neoplasia. Severe hypereosinophilia may be a prominent sign and hypereosinophilic syndrome might be the presenting diagnosis, as in the patient described here. [5, 43,44,45,46,47]. Finally, autoimmune lymphoproliferative syndrome due to CTLA4 haploinsufficiency manifests with autoimmune cytopenias, lymphoproliferation and abnormal lymphocytic and granulomatous infiltration of nonlymphoid organs, as in the patient described who suffered from diffuse granulomatosis, organ failure and fatal infection [25, 48,49,50]. CTLA4 deficiency is associated with increased risk for malignancies, especially lymphomas and gastric cancer [50].
Published studies on HCT studies in children with PID and malignant disease are presented in Table 3. In general, RIC HCT is feasible and effective in children with PID and lymphoma. Every effort should be made to achieve complete or partial response of lymphoma before HCT. Early HCT before end-organ damage was associated with improved outcomes. In general, development of autoimmunity and inflammation negatively impact outcomes after HCT in patients with PID [57].
Although identification of a genetic cause of PID does not prevail over clinical decision for HCT, some recommendations about specific genetic causes can be formulated. DOCK8 deficiency is one of the few PID (with the exception of severe combined immunodeficiency) where HCT indication is straightforward [55, 58, 59]. Reported outcomes are excellent [55]. In our case with DOCK8 deficiency, HCT completely reversed immune phenotype: hypereosinophilia completely subsided after six months, B and T-cell numbers normalized, and the patient remained asymptomatic for infections and allergy. Children with AT are less often offered HCT, because of non-hematopoietic, essentially neurologic, comorbidities, concerns about transplant-related toxicity. Nevertheless, HCT not only corrects propensity to infection in AT, but also may prevent from other malignancies by restoring immune surveillance [60, 61]. Increased naive T cells after HCT for AT could act as a shield against leukemia and lymphoma [62]. Similarly, HCT may alter the course of CTLA4 deficiency [56]. Early HCT with less complex autoimmunity could lead to less alloreactivity and GVHD. Our patient with CTLA4 deficiency would probably have benefitted from early HCT to prevent fatal infection, organ failure due to extensive granulomatous-lymphocytic infiltration, or lymphoma.
For most PID and PID-driven HM indications, timing and modalities of HCT are neither clear nor consensual. One illustrative example is that of the girl diagnosed with CID and two EBV-related lymphomas in a three-year span. The arguments for HCT, pro and con, are immunity restoration but with an incompressible, although low, risk of treatment-related mortality and morbidity with the potential to affect long-term quality of life. Other important aspects of HCT in PID, like immunological and genetic evaluation of candidate sibling donors, are not yet standardized. Therefore, until the results of large clinical trials are published, critical decisions about indications and modalities of HCT in PID with cancer predisposition or PID-driven malignancies are largely based on clinical judgment. Clinical indications of HCT in our patients included chronic debilitating symptoms (the girl with CID and thrombotic vasculitis with failure to thrive), need for organ function preservation (the boy with a history of ALL and CID, diagnosed with GLILD, the girl with CTLA4 deficiency and diffuse granulomatosis), avoiding lifelong treatment (the girl with STAT3 GOF mutation). On the contrary, HCT could not be offered to the girl with AT and lymphomatoid granulomatosis because of comorbidities and poor performance status. In this series, all patients who underwent HCT survived with full restoration of immunological phenotype and resolution of immune dysregulation, and none developed extensive GVHD.
New targeted treatments for PID may constitute alternative or bridge therapies to HCT. Ruxolitinib, a Janus kinase inhibitor, which downregulates JAK-STAT signaling, and tocilizumab, an anti-IL-6 receptor, were used in our patient with STAT3 GOF mutation [63]. Although HCT was the only curative treatment, a matched donor was initially lacking. In this case, ruxolitinib and tocilizumab helped implement the initial treatment plan in optimal conditions. This example highlights the role of targeted treatments for stabilizing the patient –not to replace but to prepare for HCT. Another targeted treatment, abatacept, a fusion protein composed of the Fc region of IgG1 fused to the extracellular domain of CTLA4, with or without an mTOR inhibitor, may alleviate symptoms in CTLA4 deficiency [64,65,66]. However, long-term treatment with abatacept or ruxolitinib may predispose to malignancies [67], and long-term treatment with ruxolitinib is associated with infections [68]. In addition, there are no data on the impact of targeted treatment on cumulative incidence of HM in PID. Taking the above into consideration, HCT should be systematically discussed for children with PID and severe lymphoproliferation or end-organ involvement. Shared decision-making with the parents is essential in this setting.
Conclusion
In conclusion, cancer predisposition lies at the intersection between PID, hematological malignancies and non-malignant lymphoproliferation. In the era of wide access to genomic testing, genetic findings can document a cancer predisposition syndrome if they are clearly pathogenic, but must be interpreted with caution if not. Inconclusive genetic findings should not impact clinical decisions. In cases with a suggestive personal history or a genetically defined cancer predisposition syndrome, HCT might suppress the vicious circle of PID and cancer predisposition.
Malignant and non-malignant lymphoproliferation in a child may be a warning sign for underlying PID. The first step is to refer to the immunologist and perform a functional workup of the immune system. If immunodeficiency is documented, referral to a clinical geneticist should be considered [69]. Multiple mailgnancies should also raise suspicion for underlying PID, as well as for other causes of genetic predisposition. In the setting of genetic predisposition, eligibility of sibling donors must be checked with a careful clinical, immunological and genetic evaluation.
In the past, only certain aspects of PID were of concern for hematologists, like impaired neutrophil function, gene therapy for severe combined immune deficiency and immune defects in hemophagocytic lymphohistiocytosis. This field is rapidly changing, especially in pediatric hematology, where the need for a consensus on HCT indications and modalities for these patients is strongly felt.
References
Kersey JH, Spector BD, Good RA (1973) Primary immunodeficiency diseases and cancer: the immunodeficiency-cancer registry. Int J Cancer 12(2):333–347. https://doi.org/10.1002/ijc.2910120204
Mayor PC, Eng KH, Singel KL, Abrams SI, Odunsi K, Moysich KB, Fuleihan R, Garabedian E, Lugar P, Ochs HD, Bonilla FA, Buckley RH, Sullivan KE, Ballas ZK, Cunningham-Rundles C, Segal BH (2018) Cancer in primary immunodeficiency diseases: cancer incidence in the United States immune deficiency network registry. J Allergy Clin Immunol 141(3):1028–1035. https://doi.org/10.1016/j.jaci.2017.05.024
Yakaboski E, Fuleihan RL, Sullivan KE, Cunningham-Rundles C, Feuille E (2020) Lymphoproliferative disease in CVID: a report of types and frequencies from a US patient registry. J Clin Immunol 40(3):524–530. https://doi.org/10.1007/s10875-020-00769-8
Maffeis M, Notarangelo LD, Schumacher RF, Soncini E, Soresina A, Lanfranchi A, Porta F (2019) Primary immunodeficiencies and oncological risk: the experience of the children’s hospital of Brescia. Front Pediatr 7:232. https://doi.org/10.3389/fped.2019.00232
Cekic S, Metin A, Aytekin C, Edeer Karaca N, Baris S, Karali Y, Kiykim A, Karakoc Aydıner E, Ozen A, Aslan T, Sevinir B, Aksu G, Kutukculer N, Kilic SS (2020) The evaluation of malignancies in Turkish primary immunodeficiency patients; a multicenter study. Pediatr Allergy Immunol 31(5):528–536. https://doi.org/10.1111/pai.13231
Bousfiha A, Jeddane L, Picard C, Al-Herz W, Ailal F, Chatila T, Cunningham-Rundles C, Etzioni A, Franco JL, Holland SM, Klein C, Morio T, Ochs HD, Oksenhendler E, Puck J, Torgerson TR, Casanova JL, Sullivan KE, Tangye SG (2020) Human inborn errors of immunity: 2019 update of the IUIS phenotypical classification. J Clin Immunol 40(1):66–81. https://doi.org/10.1007/s10875-020-00758-x
Attarbaschi A, Carraro E, Abla O, Barzilai-Birenboim S, Bomken S, Brugieres L, Bubanska E, Burkhardt B, Chiang AK, Csoka M, Fedorova A, Jazbec J, Kabickova E, Krenova Z, Lazic J, Loeffen J, Mann G, Niggli F, Miakova N, Osumi T, Ronceray L, Uyttebroeck A, Williams D, Woessmann W, Wrobel G, Pillon M, European Intergroup for Childhood Non-Hodgkin Lymphoma (EICNHL) and the International Berlin-Frankfurt-Münster (i-BFM) Study Group (2016) Non-Hodgkin lymphoma and pre-existing conditions: spectrum, clinical characteristics and outcome in 213 children and adolescents. Haematologica 101(12):1581–1591. https://doi.org/10.3324/haematol.2016.147116
Notarangelo LD, Uzel G, Rao VK (2019) Primary immunodeficiencies: novel genes and unusual presentations. Hematol Am Soc Hematol Educ Program 1:443–448. https://doi.org/10.1182/hematology.2019000051
Bomken S, van der WerffTenBosch J, Attarbaschi A, Bacon CM, Borkhardt A, Boztug K, Fischer U, Hauck F, Kuiper RP, Lammens T, Loeffen J, Neven B, Pan-Hammarström Q, Quinti I, Seidel MG, Warnatz K, Wehr C, Lankester AC, Gennery AR (2018) Current understanding and future research priorities in malignancy associated with inborn errors of immunity and DNA repair disorders: the perspective of an interdisciplinary working group. Front Immunol 9:2912. https://doi.org/10.3389/fimmu.2018.02912
Shapiro RS (2011) Malignancies in the setting of primary immunodeficiency: Implications for hematologists/oncologists. Am J Hematol 86(1):48–55. https://doi.org/10.1002/ajh.21903
Renzi S, Langenberg-Ververgaert KPS, Waespe N, Ali S, Bartram J, Michaeli O, Upton J, Cada M (2020) Primary immunodeficiencies and their associated risk of malignancies in children: an overview. Eur J Pediatr 179(5):689–97. https://doi.org/10.1007/s00431-020-03619-2
Hauck F, Voss R, Urban C, Seidel MG (2018) Intrinsic and extrinsic causes of malignancies in patients with primary immunodeficiency disorders. J Allergy Clin Immunol 141(1):59-68.e4. https://doi.org/10.1016/j.jaci.2017.06.009
Frizzera G, Rosai J, Dehner LP, Spector BD, Kersey JH (1980) Lymphoreticular disorders in primary immunodeficiencies: new findings based on an up-to-date histologic classification of 35 cases (180). Cancer 46(4):692–9
Seidemann K, Tiemann M, Henze G, Sauerbrey A, Müller S, Reiter A (1999) Therapy for non-Hodgkin lymphoma in children with primary immunodeficiency: analysis of 19 patients from the BFM trials (1999). Med Pediatr Oncol 33(6):536–544
Canioni D, Jabado N, MacIntyre E, Patey N, Emile JF, Brousse N (2001) Lymphoproliferative disorders in children with primary immunodeficiencies: immunological status may be more predictive of the outcome than other criteria. Histopathology 38(2):146–159. https://doi.org/10.1046/j.1365-2559.2001.01039.x
Kiykim A, Eker N, Surekli O, Nain E, Kasap N, Aktürk H, Dogru O, Canbolat A, Somer A, Koc A, Tokuc G, Bozkurt S, Turkoz K, Karakoc-Aydiner E, Ozen A, Baris S (2020) Malignancy and lymphoid proliferation in primary immune deficiencies; hard to define, hard to treat. Pediatr Blood Cancer 67(2):e28091. https://doi.org/10.1002/pbc.28091
Suarez F, Mahlaoui N, Canioni D, Andriamanga C, Dubois d’Enghien C, Brousse N, Jais JP, Fischer A, Hermine O, Stoppa-Lyonnet D (2015) Incidence, presentation, and prognosis of malignancies in ataxia-telangiectasia: a report from the French national registry of primary immune deficiencies. J Clin Oncol 33(2):202–208. https://doi.org/10.1200/JCO.2014.56.5101
Cheminant M, Mahlaoui N, Desconclois C, Canioni D, Ysebaert L, Dupré L, Vasconcelos Z, Malphettes M, Moshous D, Neven B, Rohrlich PS, Bernard M, Bertrand Y, Fischer A, Suarez F (2019) Lymphoproliferative disease in patients with Wiskott-Aldrich syndrome: analysis of the French registry of primary immunodeficiencies. J Allergy Clin Immunol 143(6):2311-2315.e7. https://doi.org/10.1016/j.jaci.2019.01.046
Saarinen S, Aavikko M, Aittomäki K, Launonen V, Lehtonen R, Franssila K, Lehtonen HJ, Kaasinen E, Broderick P, Tarkkanen J, Bain BJ, Bauduer F, Ünal A, Swerdlow AJ, Cooke R, Mäkinen MJ, Houlston R, Vahteristo P, Aaltonen LA (2011) Exome sequencing reveals germline NPAT mutation as a candidate risk factor for Hodgkin lymphoma. Blood 118(3):493–498. https://doi.org/10.1182/blood-2011-03-341560
Casey JP, Nobbs M, McGettigan P, Lynch S, Ennis S (2012) Recessive mutations in MCM4/PRKDC cause a novel syndrome involving a primary immunodeficiency and a disorder of DNA repair. J Med Genet 49(4):242–245. https://doi.org/10.1136/jmedgenet-2012-100803
Hughes CR, Guasti L, Meimaridou E, Chuang CH, Schimenti JC, King PJ, Costigan C, Clark AJ, Metherell LA (2012) MCM4 mutation causes adrenal failure, short stature, and natural killer cell deficiency in humans. J Clin Invest 122(3):814–820. https://doi.org/10.1172/JCI60224
Frey-Jakobs S, Hartberger JM, Fliegauf M, Bossen C, Wehmeyer ML, Neubauer JC, Bulashevska A, Proietti M, Fröbel P, Nöltner C, Yang L, Rojas-Restrepo J, Langer N, Winzer S, Engelhardt KR, Glocker C, Pfeifer D, Klein A, Schäffer AA, Lagovsky I, Lachover-Roth I, Béziat V, Puel A, Casanova JL, Fleckenstein B, Weidinger S, Kilic SS, Garty BZ, Etzioni A, Grimbacher B (2018) ZNF341 controls STAT3 expression and thereby immunocompetence. Sci Immunol. https://doi.org/10.1126/sciimmunol.aat4941
Béziat V, Li J, Lin JX, Ma CS, Li P, Bousfiha A, Pellier I, Zoghi S, Baris S, Keles S, Gray P, Du N, Wang Y, Zerbib Y, Lévy R, Leclercq T, About F, Lim AI, Rao G, Payne K, Pelham SJ, Avery DT, Deenick EK, Pillay B, Chou J, Guery R, Belkadi A, Guérin A, Migaud M, Rattina V, Ailal F, Benhsaien I, Bouaziz M, Habib T, Chaussabel D, Marr N, El-Benna J, Grimbacher B, Wargon O, Bustamante J, Boisson B, Müller-Fleckenstein I, Fleckenstein B, Chandesris MO, Titeux M, Fraitag S, Alyanakian MA, Leruez-Ville M, Picard C, Meyts I, Di Santo JP, Hovnanian A, Somer A, Ozen A, Rezaei N, Chatila TA, Abel L, Leonard WJ, Tangye SG, Puel A, Casanova JL (2018) A recessive form of hyper-IgE syndrome by disruption of ZNF341-dependent STAT3 transcription and activity. Sci Immunol. https://doi.org/10.1126/sciimmunol.aat4956
Milner JD, Vogel TP, Forbes L, Ma CA, Stray-Pedersen A, Niemela JE, Lyons JJ, Engelhardt KR, Zhang Y, Topcagic N, Roberson ED, Matthews H, Verbsky JW, Dasu T, Vargas-Hernandez A, Varghese N, McClain KL, Karam LB, Nahmod K, Makedonas G, Mace EM, Sorte HS, Perminow G, Rao VK, O’Connell MP, Price S, Su HC, Butrick M, McElwee J, Hughes JD, Willet J, Swan D, Xu Y, Santibanez-Koref M, Slowik V, Dinwiddie DL, Ciaccio CE, Saunders CJ, Septer S, Kingsmore SF, White AJ, Cant AJ, Hambleton S, Cooper MA (2015) Early-onset lymphoproliferation and autoimmunity caused by germline STAT3 gain-of-function mutations. Blood 125(4):591–599. https://doi.org/10.1182/blood-2014-09-602763
Schwab C, Gabrysch A, Olbrich P, Patiño V, Warnatz K, Wolff D, Hoshino A, Kobayashi M, Imai K, Takagi M, Dybedal I, Haddock JA, Sansom DM, Lucena JM, Seidl M, Schmitt-Graeff A, Reiser V, Emmerich F, Frede N, Bulashevska A, Salzer U, Schubert D, Hayakawa S, Okada S, Kanariou M, Kucuk ZY, Chapdelaine H, Petruzelkova L, Sumnik Z, Sediva A, Slatter M, Arkwright PD, Cant A, Lorenz HM, Giese T, Lougaris V, Plebani A, Price C, Sullivan KE, Moutschen M, Litzman J, Freiberger T, van de Veerdonk FL, Recher M, Albert MH, Hauck F, Seneviratne S, Pachlopnik Schmid J, Kolios A, Unglik G, Klemann C, Speckmann C, Ehl S, Leichtner A, Blumberg R, Franke A, Snapper S, Zeissig S, Cunningham-Rundles C, Giulino-Roth L, Elemento O, Dückers G, Niehues T, Fronkova E, Kanderová V, Platt CD, Chou J, Chatila TA, Geha R, McDermott E, Bunn S, Kurzai M, Schulz A, Alsina L, Casals F, Deyà-Martinez A, Hambleton S, Kanegane H, Taskén K, Neth O, Grimbacher B (2018) Phenotype, penetrance, and treatment of 133 cytotoxic T-lymphocyte antigen 4-insufficient subjects. J Allergy Clin Immunol 142(6):1932–1946. https://doi.org/10.1016/j.jaci.2018.02.055
Łyszkiewicz M, Ziętara N, Frey L, Pannicke U, Stern M, Liu Y, Fan Y, Puchałka J, Hollizeck S, Somekh I, Rohlfs M, Yilmaz T, Ünal E, Karakukcu M, Patiroğlu T, Kellerer C, Karasu E, Sykora KW, Lev A, Simon A, Somech R, Roesler J, Hoenig M, Keppler OT, Schwarz K, Klein C (2020) Human FCHO1 deficiency reveals role for clathrin-mediated endocytosis in development and function of T cells. Nat Commun 11(1):1031. https://doi.org/10.1038/s41467-020-14809-9
Calzoni E, Platt CD, Keles S, Kuehn HS, Beaussant-Cohen S, Zhang Y, Pazmandi J, Lanzi G, Pala F, Tahiat A, Artac H, Heredia RJ, Dmytrus J, Reisli I, Uygun V, Uygun D, Bingol A, Basaran E, Djenouhat K, Benhalla N, Bendahmane C, Emiroglu M, Kirchhausen T, Pasham M, Jones J, Wallace JG, Zheng L, Boisson B, Porta F, Rosenzweig SD, Su H, Giliani S, Lenardo M, Geha RS, Boztug K, Chou J, Notarangelo LD (2019) F-BAR domain only protein 1 (FCHO1) deficiency is a novel cause of combined immune deficiency in human subjects. J Allergy Clin Immunol 143(6):2317-2321.e12. https://doi.org/10.1016/j.jaci.2019.02.014
Tiosano D, Baris HN, Chen A, Hitzert MM, Schueler M, Gulluni F, Wiesener A, Bergua A, Mory A, Copeland B, Gleeson JG, Rump P, van Meer H, Sival DA, Haucke V, Kriwinsky J, Knaup KX, Reis A, Hauer NN, Hirsch E, Roepman R, Pfundt R, Thiel CT, Wiesener MS, Aslanyan MG, Buchner DA (2019) Mutations in PIK3C2A cause syndromic short stature, skeletal abnormalities, and cataracts associated with ciliary dysfunction. PLoS Genet 15(4):e1008088. https://doi.org/10.1371/journal.pgen.1008088
Glocker EO, Kotlarz D, Boztug K, Gertz EM, Schäffer AA, Noyan F, Perro M, Diestelhorst J, Allroth A, Murugan D, Hätscher N, Pfeifer D, Sykora KW, Sauer M, Kreipe H, Lacher M, Nustede R, Woellner C, Baumann U, Salzer U, Koletzko S, Shah N, Segal AW, Sauerbrey A, Buderus S, Snapper SB, Grimbacher B, Klein C (2009) Inflammatory bowel disease and mutations affecting the interleukin-10 receptor. N Engl J Med 361(21):2033–2045. https://doi.org/10.1056/NEJMoa0907206
Meyts I, Aksentijevich I (2018) Deficiency of adenosine deaminase 2 (DADA2): updates on the phenotype, genetics, pathogenesis, and treatment. J Clin Immunol 38(5):569–578. https://doi.org/10.1007/s10875-018-0525-8
Williams A, Bate J, Brooks R, Clarke S, Dixon E, Faust S, Chisholm JC, Galanopoulou A, Heath P, Maishman T, Mapstone S, Patel SR, Vora A, Wilding S, Gray J (2020) Immune reconstitution in children following chemotherapy for acute lymphoblastic leukaemia. eJHaem. https://doi.org/10.1002/jha2.27
Claassen D, Boals M, Bowling KM, Cooper GM, Cox J, Hershfield M, Lewis S, Wlodarski M, Weiss MJ, Estepp JH (2018) Complexities of genetic diagnosis illustrated by an atypical case of congenital hypoplastic anemia. Cold Spring Harb Mol Case Stud 4(6):a003384. https://doi.org/10.1101/mcs.a003384
Ulirsch JC, Verboon JM, Kazerounian S, Guo MH, Yuan D, Ludwig LS, Handsaker RE, Abdulhay NJ, Fiorini C, Genovese G, Lim ET, Cheng A, Cummings BB, Chao KR, Beggs AH, Genetti CA, Sieff CA, Newburger PE, Niewiadomska E, Matysiak M, Vlachos A, Lipton JM, Atsidaftos E, Glader B, Narla A, Gleizes PE, O’Donohue MF, Montel-Lehry N, Amor DJ, McCarroll SA, O’Donnell-Luria AH, Gupta N, Gabriel SB, MacArthur DG, Lander ES, Lek M, Da Costa L, Nathan DG, Korostelev AA, Do R, Sankaran VG, Gazda HT (2018) The genetic landscape of Diamond-Blackfan anemia. Am J Hum Genet 103(6):930–947. https://doi.org/10.1016/j.ajhg.2018.10.027
Natkunam Y, Gratzinger D, Chadburn A, Goodlad JR, Chan JKC, Said J, Jaffe ES, de Jong D (2018) Immunodeficiency-associated lymphoproliferative disorders: time for reappraisal? Blood 132(18):1871–1878. https://doi.org/10.1182/blood-2018-04-842559
Walsh MF, Chang VY, Kohlmann WK, Scott HS, Cunniff C, Bourdeaut F, Molenaar JJ, Porter CC, Sandlund JT, Plon SE, Wang LL, Savage SA (2017) Recommendations for childhood cancer screening and surveillance in DNA repair disorders. Clin Cancer Res 23(11):e23–e31. https://doi.org/10.1158/1078-0432.CCR-17-0465
Melani C, Jaffe ES, Wilson WH (2020) Pathobiology and treatment of lymphomatoid granulomatosis, a rare EBV-driven disorder. Blood 135(16):1344–1352. https://doi.org/10.1182/blood.2019000933
Schepp J, Proietti M, Frede N, Buchta M, Hübscher K, Rojas Restrepo J, Goldacker S, Warnatz K, Pachlopnik Schmid J, Duppenthaler A, Lougaris V, Uriarte I, Kelly S, Hershfield M, Grimbacher B (2017) Screening of 181 patients with antibody deficiency for deficiency of adenosine deaminase 2 sheds new light on the disease in adulthood. Arthritis Rheumatol 69(8):1689–1700. https://doi.org/10.1002/art.40147
Caorsi R, Penco F, Grossi A, Insalaco A, Omenetti A, Alessio M, Conti G, Marchetti F, Picco P, Tommasini A, Martino S, Malattia C, Gallizzi R, Podda RA, Salis A, Falcini F, Schena F, Garbarino F, Morreale A, Pardeo M, Ventrici C, Passarelli C, Zhou Q, Severino M, Gandolfo C, Damonte G, Martini A, Ravelli A, Aksentijevich I, Ceccherini I, Gattorno M (2017) ADA2 deficiency (DADA2) as an unrecognised cause of early onset polyarteritis nodosa and stroke: a multicentre national study. Ann Rheum Dis 76(10):1648–1656. https://doi.org/10.1136/annrheumdis-2016-210802
Flanagan SE, Haapaniemi E, Russell MA, Caswell R, Allen HL, De Franco E, McDonald TJ, Rajala H, Ramelius A, Barton J, Heiskanen K, Heiskanen-Kosma T, Kajosaari M, Murphy NP, Milenkovic T, Seppänen M, Lernmark Å, Mustjoki S, Otonkoski T, Kere J, Morgan NG, Ellard S, Hattersley AT (2014) Activating germline mutations in STAT3 cause early-onset multi-organ autoimmune disease. Nat Genet 46(8):812–814. https://doi.org/10.1038/ng.3040
Koskela HL, Eldfors S, Ellonen P, van Adrichem AJ, Kuusanmäki H, Andersson EI, Lagström S, Clemente MJ, Olson T, Jalkanen SE, Majumder MM, Almusa H, Edgren H, Lepistö M, Mattila P, Guinta K, Koistinen P, Kuittinen T, Penttinen K, Parsons A, Knowles J, Saarela J, Wennerberg K, Kallioniemi O, Porkka K, Loughran TP Jr, Heckman CA, Maciejewski JP, Mustjoki S (2012) Somatic STAT3 mutations in large granular lymphocytic leukemia. N Engl J Med 366(20):1905–1913. https://doi.org/10.1056/NEJMoa1114885
Haapaniemi EM, Kaustio M, Rajala HL, van Adrichem AJ, Kainulainen L, Glumoff V, Doffinger R, Kuusanmäki H, Heiskanen-Kosma T, Trotta L, Chiang S, Kulmala P, Eldfors S, Katainen R, Siitonen S, Karjalainen-Lindsberg ML, Kovanen PE, Otonkoski T, Porkka K, Heiskanen K, Hänninen A, Bryceson YT, Uusitalo-Seppälä R, Saarela J, Seppänen M, Mustjoki S, Kere J (2015) Autoimmunity, hypogammaglobulinemia, lymphoproliferation, and mycobacterial disease in patients with activating mutations in STAT3. Blood 125(4):639–648. https://doi.org/10.1182/blood-2014-04-570101
Hadjadj J, Castro CN, Tusseau M, Stolzenberg MC, Mazerolles F, Aladjidi N, Armstrong M, Ashrafian H, Cutcutache I, Ebetsberger-Dachs G, Elliott KS, Durieu I, Fabien N, Fusaro M, Heeg M, Schmitt Y, Bras M, Knight JC, Lega JC, Lesca G, Mathieu AL, Moreews M, Moreira B, Nosbaum A, Page M, Picard C, Ronan Leahy T, Rouvet I, Ryan E, Sanlaville D, Schwarz K, Skelton A, Viallard JF, Viel S, Villard M, Callebaut I, Picard C, Walzer T, Ehl S, Fischer A, Neven B, Belot A, Rieux-Laucat F (2020) Early-onset autoimmunity associated with SOCS1 haploinsufficiency. Nat Commun 11(1):5341. https://doi.org/10.1038/s41467-020-18925-4
Puel A, Casanova JL (2019) The nature of human IL-6. J Exp Med 216(9):1969–1971. https://doi.org/10.1084/jem.20191002
Aydin SE, Kilic SS, Aytekin C, Kumar A, Porras O, Kainulainen L, Kostyuchenko L, Genel F, Kütükcüler N, Karaca N, Gonzalez-Granado L, Abbott J, Al-Zahrani D, Rezaei N, Baz Z, Thiel J, Ehl S, Marodi L, Orange JS, Sawalle-Belohradsky J, Keles S, Holland SM, Sanal Ö, Ayvaz DC, Tezcan I, Al-Mousa H, Alsum Z, Hawwari A, Metin A, Matthes-Martin S, Hönig M, Schulz A, Picard C, Barlogis V, Gennery A, Ifversen M, van Montfrans J, Kuijpers T, Bredius R, Dückers G, Al-Herz W, Pai SY, Geha R, Notheis G, Schwarze CP, Tavil B, Azik F, Bienemann K, Grimbacher B, Heinz V, Gaspar HB, Aydin R, Hagl B, Gathmann B, Belohradsky BH, Ochs HD, Chatila T, Renner ED, Su H, Freeman AF, Engelhardt K, Albert MH, Inborn Errors Working Party of EBMT (2015) DOCK8 deficiency: clinical and immunological phenotype and treatment options—a review of 136 patients. J Clin Immunol 35(2):189–198. https://doi.org/10.1007/s10875-014-0126-0
Dimitriades VR, Devlin V, Pittaluga S, Su HC, Holland SM, Wilson W, Dunleavy K, Shah NN, Freeman AF (2017) DOCK 8 deficiency, EBV+ lymphomatoid granulomatosis, and intrafamilial variation in presentation. Front Pediatr. https://doi.org/10.3389/fped.2017.00038
Kuşkonmaz B, Ayvaz D, Barış S, Ünal Ş, Tezcan İ, Uçkan D (2017) Acute myeloid leukemia in a child with dedicator of cytokinesis 8 (DOCK8) deficiency. Pediatr Blood Cancer. https://doi.org/10.1002/pbc.26695
Sanal O, Jing H, Ozgur T, Ayvaz D, Strauss-Albee DM, Ersoy-Evans S, Tezcan I, Turkkani G, Matthews HF, Haliloglu G, Yuce A, Yalcin B, Gokoz O, Oguz KK, Su HC (2012) Additional diverse findings expand the clinical presentation of DOCK8 deficiency. J Clin Immunol 32(4):698–708. https://doi.org/10.1007/s10875-012-9664-5
Schubert D, Bode C, Kenefeck R, Hou TZ, Wing JB, Kennedy A, Bulashevska A, Petersen BS, Schäffer AA, Grüning BA, Unger S, Frede N, Baumann U, Witte T, Schmidt RE, Dueckers G, Niehues T, Seneviratne S, Kanariou M, Speckmann C, Ehl S, Rensing-Ehl A, Warnatz K, Rakhmanov M, Thimme R, Hasselblatt P, Emmerich F, Cathomen T, Backofen R, Fisch P, Seidl M, May A, Schmitt-Graeff A, Ikemizu S, Salzer U, Franke A, Sakaguchi S, Walker LSK, Sansom DM, Grimbacher B (2014) Autosomal dominant immune dysregulation syndrome in humans with CTLA4 mutations. Nat Med 20(12):1410–1416. https://doi.org/10.1038/nm.3746
Kuehn HS, Ouyang W, Lo B, Deenick EK, Niemela JE, Avery DT, Schickel JN, Tran DQ, Stoddard J, Zhang Y, Frucht DM, Dumitriu B, Scheinberg P, Folio LR, Frein CA, Price S, Koh C, Heller T, Seroogy CM, Huttenlocher A, Rao VK, Su HC, Kleiner D, Notarangelo LD, Rampertaap Y, Olivier KN, McElwee J, Hughes J, Pittaluga S, Oliveira JB, Meffre E, Fleisher TA, Holland SM, Lenardo MJ, Tangye SG, Uzel G (2014) Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science 345(6204):1623–1627. https://doi.org/10.1126/science.1255904
Egg D, Schwab C, Gabrysch A, Arkwright PD, Cheesman E, Giulino-Roth L, Neth O, Snapper S, Okada S, Moutschen M, Delvenne P, Pecher AC, Wolff D, Kim YJ, Seneviratne S, Kim KM, Kang JM, Ojaimi S, McLean C, Warnatz K, Seidl M, Grimbacher B (2018) Increased risk for malignancies in 131 affected CTLA4 mutation carriers. Front Immunol 9:2012. https://doi.org/10.3389/fimmu.2018.02012
Wehr C, Gennery AR, Lindemans C, Schulz A, Hoenig M, Marks R, Recher M, Gruhn B, Holbro A, Heijnen I, Meyer D, Grigoleit G, Einsele H, Baumann U, Witte T, Sykora KW, Goldacker S, Regairaz L, Aksoylar S, Ardeniz Ö, Zecca M, Zdziarski P, Meyts I, Matthes-Martin S, Imai K, Kamae C, Fielding A, Seneviratne S, Mahlaoui N, Slatter MA, Güngör T, Arkwright PD, van Montfrans J, Sullivan KE, Grimbacher B, Cant A, Peter HH, Finke J, Gaspar HB, Warnatz K, Rizzi M, Inborn Errors Working Party of the European Society for Blood and Marrow Transplantation and the European Society for Immunodeficiency (2015) Multicenter experience in hematopoietic stem cell transplantation for serious complications of common variable immunodeficiency. J Allergy Clin Immunol 135(4):988–97.e6. https://doi.org/10.1016/j.jaci.2014.11.029
Robison LL, Stoker V, Frizzera G, Heinitz K, Meadows AT, Filipovich AH (1987) Hodgkin’s disease in pediatric patients with naturally occurring immunodeficiency. Am J Pediatr Hematol Oncol 9(2):189–192. https://doi.org/10.1097/00043426-198722000-00019
Prunotto G, Offor UT, Samarasinghe S, Wynn R, Vora A, Carpenter B, Gowdy C, McHugh K, Windebank KP, Rovelli AM, Slatter MA, Gennery AR, Veys P, Bacon CM, Bomken S, Lucchini G (2020) HSCT provides effective treatment for lymphoproliferative disorders in children with primary immunodeficiency. J Allergy Clin Immunol 146(2):447–450. https://doi.org/10.1016/j.jaci.2020.03.043
Chan AY, Leiding JW, Liu X, Logan BR, Burroughs LM, Allenspach EJ, Skoda-Smith S, Uzel G, Notarangelo LD, Slatter M, Gennery AR, Smith AR, Pai SY, Jordan MB, Marsh RA, Cowan MJ, Dvorak CC, Craddock JA, Prockop SE, Chandrakasan S, Kapoor N, Buckley RH, Parikh S, Chellapandian D, Oshrine BR, Bednarski JJ, Cooper MA, Shenoy S, Davila Saldana BJ, Forbes LR, Martinez C, Haddad E, Shyr DC, Chen K, Sullivan KE, Heimall J, Wright N, Bhatia M, Cuvelier GDE, Goldman FD, Meyts I, Miller HK, Seidel MG, Vander Lugt MT, Bacchetta R, Weinacht KG, Andolina JR, Caywood E, Chong H, de la Morena MT, Aquino VM, Shereck E, Walter JE, Dorsey MJ, Seroogy CM, Griffith LM, Kohn DB, Puck JM, Pulsipher MA, Torgerson TR (2020) Hematopoietic cell transplantation in patients with primary immune regulatory disorders (PIRD): a primary immune deficiency treatment consortium (PIDTC) survey. Front Immunol. https://doi.org/10.3389/fimmu.2020.00239
Aydin SE, Freeman AF, Al-Herz W, Al-Mousa HA, Arnaout RK, Aydin RC, Barlogis V, Belohradsky BH, Bonfim C, Bredius RG, Chu JI, Ciocarlie OC, Doğu F, Gaspar HB, Geha RS, Gennery AR, Hauck F, Hawwari A, Hickstein DD, Hoenig M, Ikinciogullari A, Klein C, Kumar A, Ifversen MRS, Matthes S, Metin A, Neven B, Pai SY, Parikh SH, Picard C, Renner ED, Sanal Ö, Schulz AS, Schuster F, Shah NN, Shereck EB, Slatter MA, Su HC, van Montfrans J, Woessmann W, Ziegler JB, Albert MH, Inborn Errors Working Party of the European Group for Blood and Marrow Transplantation and the European Society for Primary Immunodeficiencies (2019) Hematopoietic stem cell transplantation as treatment for patients with DOCK8 deficiency. J Allergy Clin Immunol Pract 7(3):848–55. https://doi.org/10.1016/j.jaip.2018.10.035
Slatter MA, Engelhardt KR, Burroughs LM, Arkwright PD, Nademi Z, Skoda-Smith S, Hagin D, Kennedy A, Barge D, Flood T, Abinun M, Wynn RF, Gennery AR, Cant AJ, Sansom D, Hambleton S, Torgerson TR (2016) Hematopoietic stem cell transplantation for CTLA4 deficiency. J Allergy Clin Immunol 138(2):615-619.e1. https://doi.org/10.1016/j.jaci.2016.01.045
Fischer A, Provot J, Jais JP, Alcais A, Mahlaoui N, Members of the CEREDIH French PID study group (2017) Autoimmune and inflammatory manifestations occur frequently in patients with primary immunodeficiencies. J Allergy Clin Immunol. https://doi.org/10.1016/j.jaci.2016.12.978
Cuellar-Rodriguez J, Freeman AF, Grossman J, Su H, Parta M, Murdock H, Shah N, Bollard C, Kong HH, Moutsopoulos N, Stone K, Gea-Banacloche J, Holland SM, Hickstein DD (2015) Matched related and unrelated donor hematopoietic stem cell transplantation for DOCK8 deficiency. Biol Blood Marrow Transplant 21(6):1037–1045. https://doi.org/10.1016/j.bbmt.2015.01.022
Pillay BA, Avery DT, Smart JM, Cole T, Choo S, Chan D, Gray PE, Frith K, Mitchell R, Phan TG, Wong M, Campbell DE, Hsu P, Ziegler JB, Peake J, Alvaro F, Picard C, Bustamante J, Neven B, Cant AJ, Uzel G, Arkwright PD, Casanova JL, Su HC, Freeman AF, Shah N, Hickstein DD, Tangye SG, Ma CS (2019) Hematopoietic stem cell transplant effectively rescues lymphocyte differentiation and function in DOCK8-deficient patients. JCI Insight 5(11):e127527. https://doi.org/10.1172/jci.insight.127527
Bakhtiar S, Woelke S, Huenecke S, Kieslich M, Taylor AM, Schubert R, Zielen S, Bader P (2018) Pre-emptive allogeneic hematopoietic stem cell transplantation in ataxia telangiectasia. Front Immunol. https://doi.org/10.3389/fimmu.2018.02495
Beier R, Sykora KW, Woessmann W, Maecker-Kolhoff B, Sauer M, Kreipe HH, Dörk-Bousset T, Kratz C, Lauten M (2016) Allogeneic-matched sibling stem cell transplantation in a 13-year-old boy with ataxia telangiectasia and EBV-positive non-Hodgkin lymphoma. Bone Marrow Transplant 51(9):1271–1274. https://doi.org/10.1038/bmt.2016.93
Duecker R, Baer PC, Buecker A, Huenecke S, Pfeffermann LM, Modlich U, Bakhtiar S, Bader P, Zielen S, Schubert R (2019) Hematopoietic stem cell transplantation restores naive T-cell populations in Atm-deficient mice and in preemptively treated patients with ataxia-telangiectasia. Front Immunol. https://doi.org/10.3389/fimmu.2019.02785
Forbes LR, Vogel TP, Cooper MA, Castro-Wagner J, Schussler E, Weinacht KG, Plant AS, Su HC, Allenspach EJ, Slatter M, Abinun M, Lilic D, Cunningham-Rundles C, Eckstein O, Olbrich P, Guillerman RP, Patel NC, Demirdag YY, Zerbe C, Freeman AF, Holland SM, Szabolcs P, Gennery A, Torgerson TR, Milner JD, Leiding JW (2018) Jakinibs for the treatment of immune dysregulation in patients with gain-of-function signal transducer and activator of transcription 1 (STAT1) or STAT3 mutations. J Allergy Clin Immunol 142(5):1665–1669. https://doi.org/10.1016/j.jaci.2018.07.020
van Leeuwen EM, Cuadrado E, Gerrits AM, Witteveen E, de Bree GJ (2018) Treatment of intracerebral lesions with abatacept in a CTLA4-haploinsufficient patient. J Clin Immunol 38(4):464–467. https://doi.org/10.1007/s10875-018-0511-1
Lee S, Moon JS, Lee CR, Kim HE, Baek SM, Hwang S, Kang GH, Seo JK, Shin CH, Kang HJ, Ko JS, Park SG, Choi M (2016) Abatacept alleviates severe autoimmune symptoms in a patient carrying a de novo variant in CTLA-4. J Allergy Clin Immunol 137(1):327–330. https://doi.org/10.1016/j.jaci.2015.08.036
Lo B, Zhang K, Lu W, Zheng L, Zhang Q, Kanellopoulou C, Zhang Y, Liu Z, Fritz JM, Marsh R, Husami A, Kissell D, Nortman S, Chaturvedi V, Haines H, Young LR, Mo J, Filipovich AH, Bleesing JJ, Mustillo P, Stephens M, Rueda CM, Chougnet CA, Hoebe K, McElwee J, Hughes JD, Karakoc-Aydiner E, Matthews HF, Price S, Su HC, Rao VK, Lenardo MJ, Jordan MB (2015) AUTOIMMUNE DISEASE. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science 349(6246):436–440. https://doi.org/10.1126/science.aaa1663
Porpaczy E, Tripolt S, Hoelbl-Kovacic A, Gisslinger B, Bago-Horvath Z, Casanova-Hevia E, Clappier E, Decker T, Fajmann S, Fux DA, Greiner G, Gueltekin S, Heller G, Herkner H, Hoermann G, Kiladjian JJ, Kolbe T, Kornauth C, Krauth MT, Kralovics R, Muellauer L, Mueller M, Prchal-Murphy M, Putz EM, Raffoux E, Schiefer AI, Schmetterer K, Schneckenleithner C, Simonitsch-Klupp I, Skrabs C, Sperr WR, Staber PB, Strobl B, Valent P, Jaeger U, Gisslinger H, Sexl V (2018) Aggressive B-cell lymphomas in patients with myelofibrosis receiving JAK1/2 inhibitor therapy. Blood 132(7):694–706. https://doi.org/10.1182/blood-2017-10-810739
Lussana F, Cattaneo M, Rambaldi A, Squizzato A (2018) Ruxolitinib-associated infections: a systematic review and meta-analysis. Am J Hematol 93(3):339–347. https://doi.org/10.1002/ajh.24976
Jongmans MC, Loeffen JL, Waanders E, Hoogerbrugge PM, Ligtenberg MJ, Kuiper RP, Hoogerbrugge N (2016) Recognition of genetic predisposition in pediatric cancer patients: an easy-to-use selection tool. Eur J Med Genet 59(3):116–125. https://doi.org/10.1016/j.ejmg.2016.01.008
Acknowledgements
The authors would like to thank Dr. Kalliopi Stefanaki, Department of Pathology, “Aghia Sophia” Children’s Hospital, Athens, Greece, for expert diagnostics; Prof. Bodo Grimbacher at the Center for Chronic Immunodeficiency (CCI), Medical Center—University of Freiburg, Germany, Prof. Raif Geha, at the Division of Allergy/ Immunology/Rheumatology/ Dermatology, Children’s Hospital, Boston, US, Dr. Lisa Forbes, Department of Pediatrics, Immunology, Allergy and Rheumatology, Texas Children’s Hospital Infusion Center, Houston, US, and Dr. Alexandra Freeman at the National Institute of Allergy and Infectious Diseases, Bethesda, US, for input in diagnostics and clinical management of the patients; Dr. Kosmas Kotsonis and Dr. Maria Tsinti, Department of Pediatrics, Dr. Vasiliki Kitra, Dr. Ioulia Peristeri and Dr. Evgenios Goussetis, Bone Marrow Transplantation Unit, Dr. Marianna Tzanoudaki, Department of Immunology and Histocompatibility, Dr. Maria Ampatzidou, Dr. Vassilios Papadakis, Dr. Kondilia Antoniadi, Dr. Sophia Papargyri, Dr. Loizos Petrikkos, Dr. Konstantinos Tsitsikas, Department of Pediatric Hematology and Oncology, Dr. Maria Hasiotou, Dr. Maria Gavra, Dr. Georgios Pitsoulakis, Department of Radiology, all in “Aghia Sophia” Children’s Hospital, Athens, Greece; Dr. Georgios Paterakis, Laboratory of Flow Cytometry, Dr. Stefanos I. Papadhimitriou, Hematology Laboratory, Georgios Gennimatas Hospital, Dr. Lina Florentin, AlfaLab Molecular Biology and Cytogenetics Center, Dr. Kalliopi Manola, Cytogenetics, IPTA Demokritos, Dr. Maria Roumelioti, Hematology Research Laboratory, University of Athens, all in Athens, Greece, for clinical collaboration and expert diagnostics.
Funding
None.
Author information
Authors and Affiliations
Contributions
CK, VT, SP conceived and wrote the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kelaidi, C., Tzotzola, V. & Polychronopoulou, S. The paradigm of hematological malignant versus non-malignant manifestations, driven by primary immunodeficiencies: a complex interplay. Familial Cancer 20, 363–380 (2021). https://doi.org/10.1007/s10689-021-00266-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-021-00266-w