Abstract
Development of multiple colorectal cancers (CRCs), synchronously or metachronously, is associated with hereditary predisposition for cancer and accurate risk estimates of multiple tumour development are relevant to recommend rational surveillance programs. A cross-sectional study design was used to estimate the risks of synchronous CRC (SCRC) and metachronous CRC (MCRC) based on data from the National Danish Hereditary Nonpolyposis Register. In total, 7100 individuals from families within the subgroups Lynch syndrome, familial CRC (FCC) and moderate risk were used with estimates relative to a non-hereditary population control cohort. SCRC was diagnosed in 7.4% of the Lynch syndrome cases, in 4.2% of FCC cases and 2.5% of the moderate risk cases, which translated to relative risks of 1.9–5.6. The risk of MCRC was distinctively linked to Lynch syndrome with a life-time risk up to 70% and an incidence rate ratio of 5.0. The risk of SCRC was significantly increased in all subgroups of FCC and hereditary CRC, whereas the risk of MCRC was specifically linked to Lynch syndrome. These observations suggest that individuals with FCC or hereditary CRC should be carefully screened for second primary CRC at the time of diagnosis, whereas intensified surveillance for second primary CRC is motivated in Lynch syndrome with lower-intensity programs in families with yet unidentified genetic causes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genetic factors are estimated to contribute to 20–25% of colorectal cancer (CRC) development [1]. The genetic landscape consists of high-penetrant germline genomic alterations that cause polyposis syndromes (e.g. APC and MUTYH) and genomic maintenance deficiency syndromes such as Lynch syndrome with mismatch repair (MMR) gene variants in MLH1, MSH2, MSH6, PMS2 and the rarer variants in POLE, POLD1 and NTHL1 [2]. The genetically defined syndromes account for approximately 5% of the cases [3]. This implies that in the majority of cases with a pedigree suggestive of familial aggregation of CRC, no disease-predisposing variant can be identified and in this group unidentified major genes are estimated to cause one-third to half of the currently unexplained cases [4].
Multiple primary CRC can develop at the same time (synchronously) or over time (metachronously). Synchronous CRC (SCRC) is important to diagnose prior to surgery to define relevant resection margins, whereas the risk of metachronous CRC (MCRC) will influence recommendations for surveillance and may define populations suitable for prevention initiatives such as chemoprevention or extended primary surgery in addition to colonoscopy. Genetic predisposition, inflammatory bowel disease and environmental influences constitute the main causes of multiple primary CRC [5]. First-degree relatives of patients with CRC have been estimated to be at a 1.68–2.34 fold risk of CRC, which may suggest a familial predisposition beyond the rare hereditary cancer syndromes [6, 7]. Data on the risk of SCRC and MCRC in families without an identified genetic cause are scarce and recommendations for surveillance in these subgroups vary between centres. Based on the link between multiple CRC and familial predisposition and demonstration of multiple adenomas in 1.9% and high-risk adenomas in 8.7% of individuals with familial CRC (FCC), 5-yearly colonoscopies have been suggested to be relevant [5, 6, 8].
SCRC is diagnosed in 1–4% of patients with CRC, and development of synchronous colorectal neoplasia is a hallmark of inflammatory bowel disease and FCC and hereditary CRC [9,10,11]. SCRC has been associated with higher age, male sex, precursor adenomas, microsatellite instability and proximal location and also tend to be located in the same bowel segment [11,12,13]. Polyposis syndromes such as sessile serrated polyposis and familial adenomatous polyposis are characterized by synchronous neoplasia and among patients with SCRC 2–21% has been estimated to carry disease-predisposing genetic variants linked to familial adenomatous polyposis [9, 14].
MCRC has been described to develop in 1.5-9% of patients with CRC with estimates around 3% after 10 years of follow-up [6, 10, 15, 16]. A high frequency of MCRC has been documented in Lynch syndrome with cumulative risks of 15–20% after 5–10 years of follow-up and up to 69% at 30 years of follow-up [17, 18]. The risk of MCRC depends on current age with an estimated cumulative risk of 36% from age 40 to 70 years, 31% from age 50 to 70 years, and 19% from age 60 to 70 years [19]. In individuals with Lynch syndrome, subtotal colectomy at the first CRC has been reported to be associated with significantly decreased risk of MCRC at 0–10% after 8–25 years of follow-up [18, 20, 21].
The Danish Hereditary Nonpolyposis Cancer (HNPCC) Register has collected data on more than 7000 families with a suspected inherited increased risk of CRC and thus allows for robust estimates in various subgroups of FCC and hereditary CRC. Based on these data, we determined the frequencies and risks of SCRC and MCRC in various FCC and hereditary CRC subgroups with comparison to a sporadic control cohort from the general population.
Patients and methods
The Danish national HNPCC Register was established in 1991. Clinicians and laboratories report data on family history, diagnosis (adenomas and cancers), surgical procedures and genetic test results. Based on these data, the families are classified as Lynch syndrome (disease-predisposing MMR gene variants), FCC or moderate familial risk of CRC (MFR). FCC fulfils the Amsterdam I or II criteria [22] with or without defined modifications as previously described [23]. MFR are defined either by one individual in the family diagnosed with CRC before age 50 years or by two first-degree relatives diagnosed with CRC after age 50. Detailed data by family subgroup are available in Supplementary Table 1 and Supplementary Fig. 1. The data are based on reports from hospitals, general practitioners, private clinics, specialized care and pathologic and genetic diagnostic laboratories.
Based on unique individual Central Population Registry (CPR) numbers, available since 1968, data from various national registers can be linked to ensure completeness and information on e.g. death and emigration. In Denmark, surveillance for individuals with Lynch syndrome follows international guidelines with biennial colonoscopies. During the study period, biennial colonoscopies were recommended also to individuals in the FCC subgroup, whereas individuals in MFR families were recommended colonoscopy with 5-year intervals. Data were extracted from the HNPCC Register on 2nd June 2016 and merged with data on CRC diagnosed 1943–2014 from the Danish National Cancer Register and with data on surgical procedures since 1977 from the Danish National Patient Register. Eligible cancers were verified based on pathology reports and/or clinical records (Fig. 1). Data on birth, death and emigration were retrieved from the CPR (Fig. 1). Follow-up was censored at the time of emigration, proctocolectomy, age 90 years or end of study, whichever came first; and for the analyses regarding MCRC a follow-up time of minimum 1 year was required (Fig. 1). Extra-colonic cancer development was not considered in the analyses.
A sporadic cohort was generated for comparison of the frequencies and the risks of multiple CRCs. We retrieved data on all individuals in the Danish population in 2008–2012 from Statistics Denmark, stratified on sex and 1-year age intervals. All CRCs were collected from the Danish National Cancer Register. Individuals with inherited risk of CRC, which was defined as individuals registered in the Danish national HNPCC Register or in the Danish National Familial Adenomatous Polyposis Register and all individuals diagnosed with CRC before age 50, were subtracted to generate a population-based sporadic cohort that excluded familial and hereditary cases as far as possible.
Register-based studies in Denmark are not subject to ethical review, but the study database and the register linkage were approved by the Danish Data Protection Agency (AHH-2014-008).
Definitions
The study encompassed the time period 1968–2014 to allow for linkage between the HNPCC Register and other relevant Danish national registers, but data from the Danish Cancer Register was used from 1943 to classify CRCs in the study period as first or subsequent CRCs and to account for resected bowel segments. Cases where information on surgical procedures was missing were assigned as segmentally resected, motivated by this being the standard procedure. SCRC was defined as more than one CRC diagnosed within 1 year of a primary CRC. MCRC was defined as a new primary CRC diagnosed more than 1 year after a CRC. Segmental resection was defined as right hemicolectomy, transverse resection, left hemicolectomy, sigmoid resection or rectum resection. Extended surgery was defined as subtotal or total colectomy. Proximal and distal tumour localizations were defined in relation to the splenic flexure. Absolute risk of MCRC was defined as the risk of being diagnosed with MCRC before the age of 90 with death as competing risk and conditioned on the individual not dying from a previous CRC.
Statistical analysis
Age at diagnosis was compared with the general linear model procedure in SAS 9.4. Distribution of all other demography variables was compared by the Pearson chi-squared test excluding unknowns. The proportion of SCRC at the first and subsequent CRC events was compared between subsets by the Pearson chi-squared test and exact confidence limits calculated. The proportion of SCRC per CRC event within a subset was analysed by the Cochran–Armitage trend test in SAS 9.4. Relative risk (RR) of SCRC was calculated by dividing the proportion of SCRC in this study with the proportion found in the sporadic cohort. Person years at risk of MCRC were calculated from 1 year after the first CRC or April 1968 whichever came last. IRs of MCRC were calculated in age intervals by sex and family subgroup. Incidence rate ratios (IRRs) adjusted for age and sex were calculated per family subset using Poisson regression and including time at risk for each stratum as an offset by comparison with the age- and sex-specific IRs of MCRC in the sporadic cohort. Absolute risk of MCRC up to age 90 was estimated by sex and attained age with death as a competing risk. Age specific mortality rates for the general population in 2008–2012 were retrieved from Statistics Denmark and probabilities for each of the three outcomes death, MCRC or entering the next age group without an event were calculated for each age group from 25 to 89 years of age. Probabilities were calculated from incidence and mortality rates using standard formulas for the Poisson distribution. The absolute risks for attained ages were calculated backwards through age using actuarial principles to estimate the risk of MCRC before age 90 or death, and cumulative incidence of MCRC at age 70 was calculated as time from first CRC to first MCRC with death as a competing event. These statistical analyses were performed in R-3.3.3 [24]. The level of statistical significance was set at p < 0.05.
Results
In the study population, 7100 individuals from 3174 families developed at least one primary CRC (Table 1; Supplementary Table 1). The median age at onset of the first CRC was significantly lower in Lynch syndrome (median age 50.5 years) than in the other subgroups (65.3 in FCC and 61.3 in MFR, p < 0.0001). Tumour location was more often in the proximal colon in the Lynch syndrome subset (50.1%) compared to FCC and MFR (25.1 and 26.8%, p < 0.0001). Extended colonic resection was more often performed in cases with Lynch syndrome (13.3%) than in the other subgroups (2.8–3.3%, p < 0.0001). Also the 1-year overall survival rate was more favourable in the Lynch syndrome subgroup (87.0%) compared to FCC (74.6%) and MFR cases (76.4%) though these figures were not adjusted for stage (p < 0.0001; Table 1; Supplementary Table 1).
SCRC was diagnosed in 7.4% of the Lynch syndrome cases, in 4.2% of FCC and in 2.5% of MFR families, which implies a significantly higher rate in the former subgroup (p < 0.0001). Compared to the sporadic cohort, all three hereditary and familial subgroups showed significantly increased risks for SCRC with RRs of 5.6, 3.2 and 1.9 respectively (Table 2). The frequencies of SCRC increased with the number of MCRC events and was observed in 4.1% at the first CRC, 8.3% at the second primary CRC and 20.4% at the third/fourth primary CRC (p < 0.0001, Table 2).
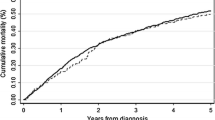
Among the 7100 patients with primary CRC, 5304 patients were eligible for analyses of the risk of MCRC. No patients were lost to follow-up, but 2 (0.04%) patients were censored at the date of emigration. In total, 471 MCRCs developed in 383 individuals. The proportion of patients with MCRC was 24.1% in Lynch syndrome, 5.0% in FCC and 4.3% in MFR. The age- and sex-adjusted IRRs compared to the sporadic cohort were 5.0 in Lynch syndrome, 1.1 in FCC and 1.2 in MFR. The IRR was only significantly increased in the Lynch syndrome subgroup (Table 3). In Lynch syndrome, the risk was further analysed in relation to disease-predisposing genes with IRRs of 5.0 for MLH1, 5.8 for MSH2 and 2.5 for MSH6 mutation carriers (Table 3). We did also analyse the risk in relation to surgical treatment of the first CRC and found an IRR of 5.5 after segmental resection and 0.9 after total/subtotal colectomy, corresponding to an IRR between the two treatments of 5.9 (2.5–19.1) (Table 3). In order to estimate the absolute risk of MCRC in the age span 25–90 years with death as competing risk, IRs and mortality rates were summarized within each age interval (Fig. 2; Supplementary Table 2). The IRs of MCRC relative to the sporadic cohort was significantly increased only in the Lynch syndrome subgroup and applied for both sexes and below age 80 (Supplementary Table 2). The absolute risk up to age 90 or death was 67.7% for men and 70.5% for women who developed their first primary CRC before age 29. With increasing age the absolute risk of MCRC decreases due to less time left until age 90 or death, leaving a risk of MCRC at 41.0% for men and 46.5% for women with Lynch syndrome and a first CRC at or before age 60. Increased absolute risks applied to all MMR genes except for PMS2. The risk was lower for carriers of disease predisposing variants in MSH6 than in MLH1 and MSH2 before age 60–70, but after that age the risks were at similar level (Fig. 3). Extended surgical resection as treatment for the first CRC gave the largest absolute risk reduction in the youngest patients (from 74.7 to 11.2% in men and from 74.9 to 34.0% in women) with decreasing relative benefit at higher age (Fig. 3). Cumulative incidence of MCRC until age 70 was 43.0% (95% CI 9.6–76.5%) in Lynch syndrome, 5.2% (95% CI 3.2–11.5%) in FCC, and 4.1 (95% CI 2.3–8.6%) in MFR.
Top: age-specific absolute risk estimates of MCRC up to age 90 for men and women with Lynch syndrome according to the 4 MMR genes MLH1 (blue), MSH2 (red), MSH6 (orange) and PMS2 (green) and the background population (black). Bottom: risk estimates in relation to type of surgical treatment for the first CRC with extended resection (green) and segmental resection (red). (Color figure online)
Discussion
Robust risk estimates provide a basis for development of precision medicine in FCC and hereditary CRC. Gene, age and gender-based surveillance programs would be beneficial to rationalize surveillance [25]. At genetic counselling, accurate risk estimates are especially challenging in individuals with a familial aggregation of CRC without an identified genetic variant. This led us to estimate the risks of SCRC and MCRC in the three major subgroups Lynch syndrome, FCC and MFR with comparison to a population-based sporadic cohort. Our data support the notion that a distinct risk profile with clearly increased risks for SCRC and MCRC apply to Lynch syndrome (Tables 2, 3) [26]. SCRC has been reported to occur in 5–25% of the first primary CRC in individuals with Lynch syndrome [27,28,29] and we support a risk in the lower range of this estimate with 7.1% SCRC diagnosed. The increased risk of multiple CRCs in Lynch syndrome applies predominantly to MCRC, which in the Danish cohort were found to develop in 24.1% of the patients after a mean follow-up time of 10.4 years with a cumulative incidence of 43% up to age 70. Our observations in the Lynch syndrome cohort support previous results with cumulative risks ranging from 6 to 22% after 10 years, 41 to 47% at 20 years and 62 to 69% at 30 years and up to 36% from age 40 to 70 years [15, 17, 19, 21, 28, 30, 31]. The somewhat higher risk estimates identified in our cohort could be explained by differences in selection criteria, variable definitions of follow-up times and differences in the statistical approaches. The age- and sex-adjusted IRR for MCRC relative to the sporadic cohort was 5.0. The life-time risks of MCRC in Lynch syndrome was 67.7% for men and 70.1% for women with their first CRC below age 29, which compares well to the 30-year cumulative incidences of 69% reported by Win et al. [17].
The choice of surgery for CRC in Lynch syndrome is debateable as there is no grade-1 evidence for performing extended resection versus segmental resection. Extended bowel resections have been linked to low (up to 10%) frequencies of MCRC [18,19,20, 27]. At the same time, total or subtotal colectomy has implications on functional outcome [19]. Current study data are not readily comparable since factors such as age at diagnosis and death as competing risk have been handled differently in the analyses. Our analyses have accounted for these factors and demonstrate decreased life-time risk of MCRC in both sexes to maximum 11.2 and 34.0% for men and women. The IRR of MCRC was 5.9 after segmental resection compared to extended resection, which corresponds well with reports of odds ratio at 4.0, hazard ratio at 5.0 and RR at 8.6 [18,19,20]. Patients with Lynch syndrome should thus be informed of a high risk of MCRC and the need for life-long surveillance.
The disease-predisposing MMR gene may also influence the risk of MCRC in Lynch syndrome and we demonstrate a two times higher life-time risk in patients with disease-predisposing variants in MLH1 or MSH2 compared to MSH6 due to a higher risk before the age of 60–70 years (Fig. 3). Previous studies on the impact from the different genes on the risk of MCRC have reached partly different conclusions, though a lower risk has been documented in MSH6, which is compatible with a lower penetrance and a higher age at onset of CRC in this subgroup [28, 32].
In the FCC and MFR subgroups, SCRC occurred in 4.2 and 2.5% of patients with a first CRC compared to 1.3% in the sporadic cohort, which corresponds to RRs of 3.2 and 1.9, respectively. The significant difference between these groups and the general population, albeit limited in absolute numbers, may reflect the exclusion of familial and hereditary cases from the general population sample to which they contribute in most comparative studies. This is also reflected in general population estimates of SCRC that have generally been 3–4% [9,10,11, 33]. The higher frequency of SCRC linked to subsequent MCRC needs further investigation, but could reflect increased tendency for multiplicity with age, environmental exposure and influence from yet unidentified epigenetic/genetic defects. SCRC may also constitute a marker of MCRC development with a hazard rate of 2.7 and RR at 13.9 identified [10, 16]. Though an association between MCRC and SCRC exists, analyses of somatic alterations suggest that the tumorigenic pathways may differ with a strong concordance in MSI status and molecular alterations between SCRC, suggestive of a stronger influence from environmental factors herein [34,35,36]. In contrast, genetic factors may play a stronger role in MCRC, which is also supported by the high risk of MCRC in the Lynch syndrome subgroup in our study.
The risk of MCRC in FCC and MFR was not significantly different from the sporadic cohort with MCRC diagnosed in 5.0 and 4.3% of the patients, respectively. An overall lower cancer incidence has been documented in FCC families compared to Lynch syndrome [37]. The findings in the FCC and the MFR subgroups were similar; supporting that similar clinical guidelines can be applied in these groups. Similar frequencies of adenomas and outcome of colonoscopy in FCC Type X and in families with late onset CRC has previously been demonstrated, suggesting that these groups may benefit from common clinical guidelines [8].
Strengths of the study include use of population-based, complete, validated and enriched data, based on National Health Register linkage. The comparative general population cohort has been generated after exclusion of familial and hereditary cases, which is unique to our study. Herein, age-specific mortality rates from the same population were imported to provide unbiased and comparable estimates of the absolute risk of MCRC up to age 90 in the various subgroups. Long-term (47 years) follow-up also allow for robust risk estimates. Limitations include a retrospective study design and restricted sample sizes for the oldest age groups and for carriers of pathogenic PMS2 variants. Lack of data on adherence to surveillance and outcome of colonoscopies may also influence outcome. In principle, colonoscopic surveillance has since the mid-1990s been recommended with 2-year intervals in Lynch syndrome and FCC and with 5-year intervals in moderate risk families. Following CRC, a standardized surveillance program is initiated regardless of family history of CRC, so systematic differences that influence SCRC and MCRC are not expected. Further, data on inflammatory bowel disease were not available, though unlikely to have different impact in the various subgroups.
In summary, we demonstrate an increased prevalence of SCRC in all three subsets of hereditary CRC, and an increased risk of MCRC only in the Lynch syndrome subset. The increased incidence of SCRC serves as a reminder of careful evaluation of the entire colorectum prior to CRC surgery. The risk of MCRC was increased in Lynch syndrome, but not in the FCC and MFR subsets, which has implications for choice of surgery and follow-up strategies and intervals.
References
Lichtenstein P, Holm NV, Verkasalo PK et al (2000) Environmental and heritable factors in the causation of cancer—analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 343:78–85. https://doi.org/10.1056/NEJM200007133430201
Valle L (2017) Recent discoveries in the genetics of familial colorectal cancer and polyposis. Clin Gastroenterol Hepatol 15:809–819. https://doi.org/10.1016/j.cgh.2016.09.148
Kanth P, Grimmett J, Champine M et al (2017) Hereditary colorectal polyposis and cancer syndromes: a primer on diagnosis and management. Am J Gastroenterol 112:1509–1525. https://doi.org/10.1038/ajg.2017.212
Win AK, Jenkins MA, Dowty JG et al (2017) Prevalence and penetrance of major genes and polygenes for colorectal cancer. Cancer Epidemiol Biomark Prev 26:404–412. https://doi.org/10.1158/1055-9965.EPI-16-0693
Pajares JA, Perea J (2015) Multiple primary colorectal cancer: individual or familial predisposition? World J Gastrointest Oncol 7:434–444. https://doi.org/10.4251/wjgo.v7.i12.434
Samadder NJ, Curtin K, Wong J et al (2014) Epidemiology and familial risk of synchronous and metachronous colorectal cancer: a population-based study in Utah. Clin Gastroenterol Hepatol 12:2078–2084.e2. https://doi.org/10.1016/j.cgh.2014.04.017
Lautrup CK, Mikkelsen EM, Lash TL et al (2015) Familial colorectal cancer risk may be lower than previously thought: a Danish cohort study. Cancer Epidemiol 39:714–719. https://doi.org/10.1016/j.canep.2015.07.004
Mesher D, Dove-Edwin I, Sasieni P et al (2014) A pooled analysis of the outcome of prospective colonoscopic surveillance for familial colorectal cancer. Int J Cancer 134:939–947. https://doi.org/10.1002/ijc.28397
Lam AK-Y, Carmichael R, Gertraud Buettner P et al (2011) Clinicopathological significance of synchronous carcinoma in colorectal cancer. Am J Surg 202:39–44. https://doi.org/10.1016/j.amjsurg.2010.05.012
Jayasekara H, Reece JC, Buchanan DD et al (2016) Risk factors for metachronous colorectal cancer following a primary colorectal cancer: a prospective cohort study. Int J Cancer 139:1081–1090. https://doi.org/10.1002/ijc.30153
Latournerie M, Jooste V, Cottet V et al (2008) Epidemiology and prognosis of synchronous colorectal cancers. Br J Surg 95:1528–1533. https://doi.org/10.1002/bjs.6382
Hu H, Chang DT, Nikiforova MN et al (2013) Clinicopathologic features of synchronous colorectal carcinoma: a distinct subset arising from multiple sessile serrated adenomas and associated with high levels of microsatellite instability and favorable prognosis. Am J Surg Pathol 37:1660–1670. https://doi.org/10.1097/PAS.0b013e31829623b8
Bos ACRK, Matthijsen RA, Erning FN van et al (2018) Treatment and outcome of synchronous colorectal carcinomas: a nationwide study. Ann Surg Oncol 25:414–421. https://doi.org/10.1245/s10434-017-6255-y
Greenstein AJ, Slater G, Heimann TM et al (1986) A comparison of multiple synchronous colorectal cancer in ulcerative colitis, familial polyposis coli, and de novo cancer. Ann Surg 203:123–128
Fante R, Roncucci L, Di Gregorio C et al (1996) Frequency and clinical features of multiple tumors of the large bowel in the general population and in patients with hereditary colorectal carcinoma. Cancer 77:2013–2021. https://doi.org/10.1002/(SICI)1097-0142(19960515)77:10%3C2013::AID-CNCR8%3E3.0.CO;2-R
Mulder SA, Kranse R, Damhuis RA et al (2012) The incidence and risk factors of metachronous colorectal cancer: an indication for follow-up. Dis Colon Rectum 55:522–531. https://doi.org/10.1097/DCR.0b013e318249db00
Win AK, Parry S, Parry B et al (2013) Risk of metachronous colon cancer following surgery for rectal cancer in mismatch repair gene mutation carriers. Ann Surg Oncol 20:1829–1836. https://doi.org/10.1245/s10434-012-2858-5
Anele CC, Adegbola SO, Askari A et al (2017) Risk of metachronous colorectal cancer following colectomy in Lynch syndrome: a systematic review and meta-analysis. Colorectal Dis 19:528–536. https://doi.org/10.1111/codi.13679
Møller P, Seppälä T, Bernstein I et al (2017) Incidence of and survival after subsequent cancers in carriers of pathogenic MMR variants with previous cancer: a report from the prospective Lynch syndrome database. Gut 66:1657–1664. https://doi.org/10.1136/gutjnl-2016-311403
Renkonen-sinisalo L, Seppälä TT, Järvinen HJ, Mecklin J (2017) Subtotal colectomy for colon cancer reduces the need for subsequent surgery in Lynch syndrome. Dis Colon Rectum 60:792–799. https://doi.org/10.1097/DCR.0000000000000802
Malik SS, Lythgoe MP, McPhail M, Monahan KJ (2017) Metachronous colorectal cancer following segmental or extended colectomy in Lynch syndrome: a systematic review and meta-analysis. Fam Cancer. https://doi.org/10.1007/s10689-017-0062-2
Vasen HFA, Watson P, Mecklin J, Lynch HT (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative Group on HNPCC. Gastroenterology 116:1453–1456. https://doi.org/10.1016/S0016-5085(99)70510-X
Lindberg LJ, Ladelund S, Frederiksen BL et al (2017) Outcome of 24 years national surveillance in different hereditary colorectal cancer subgroups leading to more individualised surveillance. J Med Genet 54:297–304. https://doi.org/10.1136/jmedgenet-2016-104284
R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Wilschut JA, Steyerberg EW, van Leerdam ME et al (2011) How much colonoscopy screening should be recommended to individuals with various degrees of family history of colorectal cancer? Cancer 117:4166–4174. https://doi.org/10.1002/cncr.26009
Shiovitz S, Copeland WK, Passarelli MN et al (2014) Characterisation of familial colorectal cancer type X, Lynch syndrome, and non-familial colorectal cancer. Br J Cancer 111:598–602. https://doi.org/10.1038/bjc.2014.309
Silva FC da, Oliveira Ferreira JR, de, Torrezan GT et al (2015) Clinical and molecular characterization of Brazilian patients suspected to have Lynch syndrome. PLoS ONE 10:e0139753. https://doi.org/10.1371/journal.pone.0139753
Parry S, Win AK, Parry B et al (2011) Metachronous colorectal cancer risk for mismatch repair gene mutation carriers—the advantage of more extensive colon surgery. Gut. https://doi.org/10.1136/gut.2010.228056
Box JC, Rodriguez-Bigas MA, Weber TK, Petrelli NJ (1999) Clinical implications of multiple colorectal carcinomas in hereditary nonpolyposis colorectal carcinoma. Dis Colon Rectum 42:717–721
Kalady MF, Lipman J, McGannon E, Church JM (2012) Risk of colonic neoplasia after proctectomy for rectal cancer in hereditary nonpolyposis colorectal cancer. Ann Surg 255:1121–1125. https://doi.org/10.1097/SLA.0b013e3182565c0b
Stupart DA, Goldberg PA, Baigrie RJ et al (2011) Surgery for colonic cancer in HNPCC: total vs segmental colectomy. Colorectal Dis 13:1395–1399. https://doi.org/10.1111/j.1463-1318.2010.02467.x
Vasen HFA, Abdirahman M, Brohet R et al (2010) One to 2-year surveillance intervals reduce risk of colorectal cancer in families with Lynch syndrome. Gastroenterology 138:2300–2306. https://doi.org/10.1053/j.gastro.2010.02.053
Mulder SA, Kranse R, Damhuis RA et al (2011) Prevalence and prognosis of synchronous colorectal cancer: a Dutch population-based study. Cancer Epidemiol 35:442–447. https://doi.org/10.1016/j.canep.2010.12.007
Zauber P, Huang J, Sabbath-Solitare M, Marotta S (2013) Similarities of molecular genetic changes in synchronous and metachronous colorectal cancers are limited and related to the cancers’ proximities to each other. J Mol Diagn 15:652–660. https://doi.org/10.1016/j.jmoldx.2013.03.009
Arriba M, Sánchez R, Rueda D et al (2017) Toward a molecular classification of synchronous colorectal cancer: clinical and molecular characterization. Clin Colorectal Cancer 16:31–37. https://doi.org/10.1016/j.clcc.2016.07.014
Dykes SL, Qui H, Rothenberger DA, García-Aguilar J (2003) Evidence of a preferred molecular pathway in patients with synchronous colorectal cancer. Cancer 98:48–54. https://doi.org/10.1002/cncr.11445
Lindor NM, Rabe K, Petersen GM et al (2005) Lower cancer incidence in Amsterdam-I criteria families without mismatch repair deficiency. JAMA 293:1979–1985. https://doi.org/10.1001/jama.293.16.1979
Acknowledgements
Financial support was granted from the Danish Cancer Society (Grant No. R90-A6150) and from the Swedish Cancer Society (Grant No. 2014/442). We would also like to thank all clinicians who have contributed with data to the Danish HNPCC Register.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lindberg, L.J., Wegen-Haitsma, W., Ladelund, S. et al. Risk of multiple colorectal cancer development depends on age and subgroup in individuals with hereditary predisposition. Familial Cancer 18, 183–191 (2019). https://doi.org/10.1007/s10689-018-0109-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-018-0109-z