Abstract
Early-onset breast cancer may be due to Li–Fraumeni Syndrome (LFS). Current national and international guidelines recommend that TP53 genetic testing should be considered for women with breast cancer diagnosed before the age of 31 years. However, large studies investigating TP53 mutation prevalence in this population are scarce. We collected nationwide laboratory records for all young breast cancer patients tested for TP53 mutations in the Netherlands. Between 2005 and 2016, 370 women diagnosed with breast cancer younger than 30 years of age were tested for TP53 germline mutations, and eight (2.2%) were found to carry a (likely) pathogenic TP53 sequence variant. Among BRCA1/BRCA2 mutation negative women without a family history suggestive of LFS or a personal history of multiple LFS-related tumours, the TP53 mutation frequency was < 1% (2/233). Taking into consideration that TP53 mutation prevalence was comparable or even higher in some studies selecting patients with breast cancer onset at older ages or HER2-positive breast cancers, raises the question of whether a very early age of onset is an appropriate single TP53 genetic testing criterion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women in the Netherlands, accounting for 28% of all newly diagnosed cancers in women in 2016 [1]. Although most cases of breast cancer are sporadic, an estimated 5–10% are attributable to inherited germline mutations in single genes, particularly the BRCA1 or BRCA2 genes [2, 3]. Since early onset of breast cancer is an indicator of genetic susceptibility [4], diagnostic BRCA1/BRCA2 DNA testing is offered to all women diagnosed with breast cancer before the age of 40 (in the Netherlands) or 46 (in the U.S.A.) [5, 6]. In addition, routine parallel genetic testing for CHEK2*1100delC mutations has been performed in the Netherlands since September 2014 [7]. However, there are some other cancer predisposition genes that are associated with early-onset breast cancer, including TP53, which has been linked to Li Fraumeni syndrome (LFS) [6].
LFS is a rare autosomal dominant inherited cancer syndrome [8]. This syndrome is characterized by a high risk for a wide variety of early-onset neoplasms [9]. The National Cancer Institute showed a cumulative cancer incidence of 50% by age 31 years among female TP53 germline mutation carriers and an incidence of nearly 100% by age 70 years [10]. Sarcoma, breast cancer, brain tumours and adrenocortical carcinoma are the most frequently observed tumours in patients with germline TP53 mutations [9, 11].
Over the years, several different sets of criteria have been established to identify individuals and families at risk for a germline TP53 mutation [11,12,13,14,15,16]. The strictest criteria are the clinical criteria for classical LFS and Li–Fraumeni-like syndrome (LFL) [12,13,14]. However, TP53 mutations were also identified in families who had not fulfilled these clinical criteria due to another tumour spectrum, age at diagnosis or sporadic occurrence of cancer [9, 11]. It is estimated that at least 14% of germline TP53 mutation carriers have a de novo mutation [17]. Therefore, lack of a positive family history does not exclude the possibility of a TP53 mutation. To cover the different clinical presentations of LFS, and to facilitate the identification of germline TP53 mutations, Chompret and colleagues have sequentially updated the testing criteria [11, 16]. Recent multigene panel studies suggest that LFS may have a broader phenotypic spectrum than previously reported because TP53 germline mutations have been identified in individuals who do not fulfill established clinical criteria recommended for LFS testing [18,19,20]. TP53 mutation carriers detected by multigene panel testing (MGPT) are notably older at breast cancer diagnosis [18].
Breast cancer is the most frequently observed cancer in women with TP53 germline mutations [21]. Several studies have described TP53 germline mutations in women with early-onset breast cancer (age of diagnosis ≤ 30 years). Reported mutation detection rates varied between 0% and 8.5%, but these numbers are largely based on small studies [9, 11, 22,23,24,25,26]. In 2015, the Chompret TP53 testing criteria were revised to include early-onset breast cancer [11]. In addition to an early age of onset, amplification of HER2 has been reported as more common in TP53-mutation-associated breast cancer [27,28,29].
According to the third (2005) and fourth (2010) edition of the Dutch national consensus-based guideline for genetics professionals (STOET/VKGN), TP53 germline mutation testing could be considered in women with breast cancer diagnosed before the age of 30 [30, 31]. The latest guideline (2017) recommends TP53 genetic testing in all breast cancer patients diagnosed before the age of 31, following the 2015 version of the Chompret criteria [32]. We conducted a nationwide retrospective laboratory records review in order to evaluate the prevalence of TP53 germline mutations among early-onset breast cancer patients in the Netherlands. We also examined genetics professionals’ experiences and attitudes regarding the timing and content of genetic counselling for LFS. The results of this survey have been published [33]. Our overall aim is to gain insight into the genetic counselling and testing of young breast cancer patients for LFS in order to make clinical recommendations regarding the most appropriate counselling strategy for these women.
Methods
Subjects
We retrospectively reviewed the laboratory records of all women diagnosed with invasive breast cancer or carcinoma in situ before the age of 30 who had been tested for TP53 germline mutations in the Netherlands between January 2005 and December 2016. Patients were referred for TP53 genetic testing on the basis of eligibility criteria that were part of the national guidelines of that time [30, 31]. In the Netherlands, TP53 mutation analysis is performed in six DNA-diagnostics laboratories. Early-onset breast cancer patients were identified by checking the TP53 DNA testing application forms of all six laboratories for personal clinical history of cancer and age at diagnosis. These data were provided by genetics professionals at the time of testing. If information about clinical history of cancer was not available on the application forms, medical records from the genetics departments were evaluated.
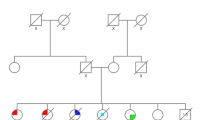
Additional data extracted from the TP53 DNA testing application forms or medical records from the genetics departments included the requested timing of DNA test results (i.e. treatment-focused DNA testing, which is used when decisions about primary breast cancer treatment could be impacted by genetic test results [34], or regular DNA testing), BRCA status (i.e. whether BRCA 1/BRCA2 testing was performed, including the results) and family history. Information about the family history was coded into three categories: (1) ‘family history suggestive of LFS’: first-degree relative (FDR) and/or second-degree relative (SDR) with a sarcoma, brain tumour or adrenocortical carcinoma (core LFS cancers); (2) ‘family history non-suggestive of LFS’: no FDR and/or SDR with a sarcoma, brain tumour or adrenocortical carcinoma (based on the family pedigree provided by the genetic professional or the notification ‘family history is non-contributory’); (3) ‘no information’: no information available about the family history of cancer. For TP53 mutation carriers, additional information was obtained regarding the histological type of breast cancer and the oestrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2) status. The Medical Research Ethics Committee of the University Medical Center Utrecht concluded that the Medical Research Human Subject Acts (WMO) does not apply.
Mutation analysis
Sanger sequence analysis of all coding exons (2–11) and exon/intron boundaries was performed for TP53 (NM_000546.5) to identify small nucleotide changes and for the identification of larger rearrangement. Multiplex ligation-dependent probe amplification (MLPA) was undertaken using the SALSA MLPA kit P056 (MRC-Holland, Amsterdam, the Netherlands). Sequence variants were classified into five categories based on the degree of likelihood of pathogenicity: (1) ‘benign’, (2) ‘likely benign’, (3) ‘uncertain significance’, (4) ‘likely pathogenic’, (5) ‘pathogenic’ [35]. Classes 3–5 were reported to the genetic professional involved.
Results
In total, 370 women diagnosed with breast cancer before the age of 30 years were tested for TP53 germline mutations in the Netherlands between 2005 and 2016, of whom 32% (119) had a treatment-focused genetic test. Since 2011, there has been a notably steep increase in the number of women tested (Fig. 1). Characteristics of the patients tested are described in Table 1. Mean age at breast cancer diagnosis was 26 years (range 15–29 years). Information about BRCA status was available for 356 patients (96%), of whom 15 were found to carry a BRCA1 pathogenic mutation and four a BRCA2 pathogenic mutation. Information about family history was available for 284 patients (77%), of whom the majority had a family history non-suggestive of LFS (255/284; 90%). Five patients had a history of LFS-spectrum cancers in addition to young onset breast cancer.
Mutation prevalence
Of the 370 early-onset breast cancer patients analysed for TP53 germline mutations, test results were available for 364 women. In six women, DNA analysis could not be performed due to insufficient quality of DNA. In eight women (2.2%), a (likely) pathogenic TP53 germline sequence variant was identified.
Of these variants, six were definitely pathogenic (c.503A > G, c.524G > A, c.637C > T, c.723delC, c.916C > T, and 376 − ?_(993 + ?)del; del exon5-exon9) and two were likely pathogenic (c.587G > A and c.749C > T). In addition, one woman was tested for a specific TP53 germline mutation that was already known to exist in her family. The majority of carriers of a (likely) pathogenic TP53 germline sequence variant (6/8) had been referred for treatment-focused genetic testing. The youngest TP53 mutation carrier was diagnosed with breast cancer at 19 years of age. Histology reports and information about family history of LFS-related cancer were available for seven carriers of a (likely) pathogenic TP53 germline mutation. Five breast cancers were identified as HER2 positive and two as triple positive (i.e. ER, PR and HER2 positive). Three carriers of a (likely) pathogenic TP53 germline sequence variant had a family history suggestive of LFS, and three carriers had developed another LFS-related tumour (2 rhabdomyosarcoma, 1 osteosarcoma) prior to their breast cancer diagnosis.
Discussion
This study was designed to evaluate the diagnostic yield of TP53 genetic testing in early-onset breast cancer patients. Our findings, the largest such study to date, show a steep increase in the number of TP53 DNA testing applications since 2011. We assume that this increase is the result of changes in national guidelines and the results of international studies [6, 21, 24, 32]. A family history suggestive of LFS was no longer required for TP53 genetic testing. Consequently, TP53 DNA genetic testing is now offered to women with early-onset breast cancer more often than it was previously. However, another possible explanation could be the increase of referrals for treatment-focused genetic counselling and testing.
Our results also show that the TP53 mutation prevalence among early-onset breast cancer patients was lower than most studies previously reported (Table 2) [9, 11, 22,23,24,25]. We found (likely) pathogenic TP53 germline mutations in 2.2% (8/370) of women diagnosed with breast cancer before the age of 30, unselected for family history. To evaluate the clinical utility of ‘early-onset breast cancer’ as a criterion for identifying TP53 carriers, it is necessary to investigate the likelihood of a germline TP53 mutation in young breast cancer patients who did not fulfil other established criteria for TP53 testing. McCuaig et al. reported the results of TP53 testing in a very small sample; they found a TP53 mutation was present in one of 13 (7.7%) cases of breast cancer diagnosed before age 30 who did not meet established criteria for TP53 testing [24]. More recently, Bougeard et al. reported on a larger series of 333 early-onset breast cancer patients (≤ 30 years) [11]. Patients had been selected for TP53 genetic testing on the basis of clinical criteria that corresponded, in most cases, with the Chompret criteria (version 2009). Of these women, 14% were found to have a TP53 mutation. Among the patients who did not fulfil the 2009 version of the Chompret criteria, the mutation detection rate was 6%. However, the exact number of women who did not fulfil these criteria was not reported. In our cohort, six of eight carriers of a (likely) pathogenic TP53 mutation did meet other established criteria for TP53 testing, in addition to ‘early-onset breast cancer’. The TP53 mutation prevalence was 0.9% (2/233) among early onset breast cancer BRCA1/BRCA2 mutation negative patients without additional features indicative of LFS (family history suggestive of LFS and/or a personal history of multiple LFS-related tumours).
Our study highlights the importance of critically reviewing established testing criteria. Women with breast cancer diagnosed before the age of 30 without additional features indicative of LFS can be reassured that they have a very low chance of being a TP53-mutation carrier. This raises the question of whether age of onset actually is an appropriate criterion for TP53 genetic testing.
Several studies have reported the frequency of TP53 mutations in different cohorts of breast cancer patients [16, 20, 26, 36,37,38,39]. For women unselected by family history, with a personal history of breast cancer up to age 36 years of age and who are BRCA1/BRCA2 mutation negative, the proportion of TP53 germline mutation carriers ranged between 2.3% and 4.2% [16, 36,37,38]. Sample size varied from 30 to 128. Two studies explored TP53 genetic testing in patients with HER2-amplified breast cancer, unselected for family history suggestive of LFS [26, 39]. Eccles and colleagues reported a TP53 mutation prevalence of 3% (9/304) among women diagnosed with HER2+ breast cancer (ER/PR status was not uniform) under the age of 41, and 8.5% (5/71) for women diagnosed before 31 years [26]. In a cohort of women with HER2+ breast cancer diagnosed ≤ 50 years without a known family history, consistent with Chompret criteria, TP53 mutations were identified in 1/195 (0.5%) [39]. In a review of 37 multigene panel studies (including mainly patients who were referred due to personal or family history of breast cancer), the overall TP53 mutation prevalence ranged from 0 to 4.4% [20]. For BRCA1/BRCA2 mutation negative patients of European ancestry undergoing breast cancer multigene panel testing (MGPT), the weighted frequency of TP53 mutation carriers was 0.3%. Although patients were diverse in age of onset and family history, it is noteworthy that approximately half of the TP53 mutation carriers detected by MGPT did not meet NCCN criteria for LFS testing (e.g. classic LFS criteria or Chompret 2015 criteria) [6]. The findings of these studies suggest that it may be beneficial to consider an expanding age of onset or HER2-positive tumour status for LFS testing criteria. However, larger studies are needed to provide more precise estimates of TP53 germline mutations in different cohorts of breast cancer patients.
An evaluation of the benefits and concerns raised by offering TP53 genetic testing is also warranted. The most reported justifications for the utility of TP53 genetic testing in patients with a low a priori probability of carrying a pathogenic TP53 variant, concerns potential clinical implications [20, 24, 40, 41]. First, there are important consequences for primary breast cancer treatment. If a woman is proven to be a TP53 mutation carrier, she may opt for bilateral mastectomy to reduce the risk of a second primary breast cancer. In addition, radiotherapy should be avoided if possible because radiation therapy may increase future cancer risks [42]. Patients without a genetic predisposition can be reassured that their risk of a secondary breast cancer is not substantially increased. There are also important potential implications for family planning and the use of prenatal diagnostics (e.g. pre-implantation genetic testing (PGD)). Lammens and colleagues evaluated the attitudes towards PGD among high risk family members from LFS and Von-Hippel Lindau families [43]. Approximately half of those contemplating a future pregnancy (23/48) would consider the use of PGD. Of note, over a period of 9 years (2009–2017), 12 couples were referred for counselling on PGD for LFS in the Netherlands, of whom 50% (6/12) started with PGD-treatment [44].
In contrast, there are other issues that complicate genetic testing for TP53 in clinical practice. Although TP53 mutation carriers may participate in a comprehensive screening protocol [10, 45,46,47], determining the optimal risk management is complex because of the wide range of cancer predisposition involved [6, 48].This applies especially to TP53 mutation carriers identified in non-classic LFS-families due to lack of information about actual phenotypic spectrum and cancer risks in these families [18]. The benefits of intensive annual screening programs must be weighed against the possibility of false positive findings that require additional diagnostic procedures [45, 49]. In addition, a few studies have reported that a substantial proportion of the individuals in families with TP53 mutations exhibit psychological distress [50,51,52]. Another relevant aspect, which was highlighted by Azzolini and colleagues, concerns patients who willingly decline TP53 DNA-analysis following genetic counselling [53]. Almost one-fourth (23.4%; 11/47) of patients decided not to undergo TP53 testing. Also, in newly diagnosed breast cancer patients who needed to define treatment options, 13% (2/23) consented to BRCA1/BRCA2 genetic testing but declined TP53 analysis.
In one genetic department in the Netherlands, we have kept records about declined testing. Here we find that 40% (16/39) of early-onset breast cancer patients who were offered TP53 genetic testing declined to be tested, and of these a considerable proportion (28%; 7/25) occurred in a setting of treatment-focused genetic counselling. These findings emphasize the necessity of thorough genetic counselling and confirm the importance of the recommendations we have made previously about the ten information items about LFS that should be discussed during pre-test counselling [33].
There are some limitations to be reported. First, this is not a population-based series of cases, but rather a nationwide clinical testing cohort. Only young breast cancer patients who were referred for genetic counselling and testing and who had chosen TP53 mutation testing were included. Between 2005 and 2016, 965 women were diagnosed with breast cancer before the age of 30 in the Netherlands [1]. Our findings show that 370 early-onset breast cancer patients were tested for TP53 germline mutations during this 12-year period. This selection might have increased the likelihood of a suggestive family history or personal history of multiple LFS-related tumours. In that case, the actual TP53 mutation prevalence among early onset breast-cancer patients may be even lower than we report. Furthermore, the degree to which information about family history was mentioned in the DNA-testing application forms differed. These data were provided by genetics professionals at the time of testing and are based on the patient’s own knowledge of their family history. Particularly in the case of treatment-focused testing, family cancer history will not be verified by pathology reports. Therefore, we may have missed information regarding family history. Another issue concerns mosaic TP53 mutations. High-coverage NGS provides new opportunities to identify germline or somatic mosaicism that was undetectable or nearly undetectable with Sanger sequencing [17]. Since we have performed Sanger sequence analysis, we may have missed mosaic TP53 mutations. However, as mosaicism in TP53 is probably very rare [54], additional NGS-results are unlikely to have a large impact on the overall TP53 mutation prevalence among early-onset breast cancer patients.
In conclusion, for early-onset breast cancer patients without additional features indicative of LFS (i.e. family history suggestive of LFS or a personal history of multiple LFS-related tumours) the probability of finding a germline TP53 mutation is exceedingly low. This is useful information for genetic counselling. However, since TP53 mutation prevalence was comparable or even higher in some studies selecting patients with breast cancer at an older age or HER2-positive breast cancers, the question is raised whether very early age of onset is an appropriate LFS testing criterion. Further research is warranted to determine the most appropriate TP53 testing strategy for women diagnosed with breast cancer. In the interim, a careful approach to genetic counselling for LFS is needed as we have noted that a substantial number of breast cancer patients who were offered TP53 DNA-analysis following genetic counselling declined to be tested.
References
Netherlands Comprehensive Cancer Organisation (IKNL) (2016) Dutch cancer Figs. 2016 [Internet]. http://www.cijfersoverkanker.nl/. Accessed May 21 2018
Turnbull C, Rahman N (2008) Genetic predisposition to breast cancer: past, present, and future. Annu Rev Genomics Hum Genet 9:321–345
Tung N, Lin NU, Kidd J et al (2016) Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol 34(13):1460–1468
Claus EB, Risch NJ, Thompson D (1990) Age at onset as an indicator of familial risk of breast cancer. Am J Epidemiol 131(6):961–972
NABON (2017) Breast Cancer, Dutch Guideline [Internet]. http://www.oncoline.nl/borstkanker. Accessed May 25 2018
National Comprehensive Cancer Network (2018) NCCN Clinical Practice Guidelines in Oncology: genetic/familial high risk assessment: breast and ovarian (Version 2.2019) [internet]. https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf (registration required). Accessed 7 Nov 2018
Adank MA, Hes FJ, van Zelst-Stams WAG et al (2015) CHEK2-mutation in Dutch breast cancer families: expanding genetic testing for breast cancer (in Dutch). Ned Tijdschr Geneeskd 159:A8910
Schneider K, Zelley K, Nichols KE et al (1999) Li–Fraumeni syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al (eds) GeneReviews [Internet]. University of Washington, Seattle, WA
Gonzalez KD, Noltner KA, Buzin CH et al (2009) Beyond Li Fraumeni Syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 27(8):1250–1256
Mai PL, Best AF, Peters JA et al (2016) Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li–Fraumeni syndrome cohort. Cancer 122(23):3673–3681
Bougeard G, Renaux-Petel M, Flaman JM et al (2015) Revisiting Li–Fraumeni Syndrome from TP53 mutation carriers. J Clin Oncol 33(21):2345–2352
Li FP, Fraumeni JF Jr, Mulvihill JJ et al (1988) A cancer family syndrome in twenty-four kindreds. Cancer Res 48(18):5358–5362
Birch JM, Hartley AL, Tricker KJ et al (1994) Prevalence and diversity of constitutional mutations in the P53 gene among 21 Li–Fraumeni families. Cancer Res 54(5):1298–1304
Eeles RA (1995) Germline mutations in the TP53 gene. Cancer Surv 25:101–124
Chompret A, Abel A, Stoppa-Lyonnet D et al (2001) Sensitivity and predictive value of criteria for p53 germline mutation screening. J Med Genet 38(1):43–47
Tinat J, Bougeard G, Baert-Desurmont S et al (2009) 2009 version of the Chompret criteria for Li Fraumeni syndrome. J Clin Oncol 27(26):e108-9
Renaux-Petel M, Charbonnier F, Thery JC et al (2018) Contribution of de novo and mosaic TP53 mutations to Li–Fraumeni syndrome. J Med Genet 55(3):173–180
Rana HQ, Gelman R, LaDuca H et al (2018) Differences in TP53 mutation carrier phenotypes emerge from panel-based testing. J Natl Cancer Inst 110(8):863–870
Amadou A, Waddington Achatz MI, Hainaut P (2018) Revisiting tumor patterns and penetrance in germline TP53 mutation carriers: temporal phases of Li–Fraumeni syndrome. Curr Opin Oncol 30(1):23–29
Fortuno C, James PA, Spurdle AB (2018) Current review of TP53 pathogenic germline variants in breast cancer patients outside Li–Fraumeni syndrome. Hum Mutat 39:1764–1773
Bouaoun L, Sonkin D, Ardin M et al (2016) TP53 variations in human cancers: new lessons from the IARC TP53 database and genomics data. Hum Mutat 37(9):865–876
Lalloo F, Varley J, Moran A et al (2006) BRCA1, BRCA2 and TP53 mutations in very early-onset breast cancer with associated risks to relatives. Eur J Cancer 42(8):1143–1150
Mouchawar J, Korch C, Byers T et al (2010) Population-based estimate of the contribution of TP53 mutations to subgroups of early-onset breast cancer: Australian Breast Cancer Family Study. Cancer Res 70(12):4795–4800
McCuaig JM, Armel SR, Novokmet A et al (2012) Routine TP53 testing for breast cancer under age 30: ready for prime time? Fam Cancer 11(4):607–613
Ginsburg OM, Akbari MR, Aziz Z et al (2009) The prevalence of germline TP53 mutations in women diagnosed with breast cancer before age 30. Fam Cancer 8(4):563–567
Eccles DM, Li N, Handwerker R et al (2016) Genetic testing in a cohort of young patients with HER2-amplified breast cancer. Ann Oncol 27(3):467–473
Wilson JR, Bateman AC, Hanson H et al (2010) A novel HER2-positive breast cancer phenotype arising from germline TP53 mutations. J Med Genet 47(11):771–774
Masciari S, Dillon DA, Rath M et al (2012) Breast cancer phenotype in women with TP53 germline mutations: a Li–Fraumeni syndrome consortium effort. Breast Cancer Res Treat 133(3):1125–1130
Melhem-Bertrandt A, Bojadzieva J, Ready KJ et al (2012) Early onset HER2-positive breast cancer is associated with germline TP53 mutations. Cancer 118(4):908–913
Netherlands Foundation for the Detection of Hereditary Tumours (STOET) and the Dutch Society of Clinical Genetics (VKGN) (2005) Guidelines for the diagnosis and prevention of hereditary cancer predisposition syndromes (in Dutch). Edition 2005
Netherlands Foundation for the Detection of Hereditary Tumours (STOET) and the Dutch Society of Clinical Genetics (VKGN) (2010) Guidelines for the diagnosis and prevention of hereditary cancer predisposition syndromes (in Dutch). Edition 2010
Netherlands Foundation for the Detection of Hereditary Tumours (STOET) and the Dutch Society of Clinical Genetics (VKGN) (2017) Guidelines for the diagnosis and prevention of hereditary cancer predisposition syndromes (in Dutch). Edition 2017
Bakhuizen JJ, Velthuizen ME, Stehouwer S et al (2018) Genetic counselling of young women with breast cancer for Li–Fraumeni syndrome: a nationwide survey on the experiences and attitudes of genetics professionals. Fam Cancer. https://doi.org/10.1007/s10689-018-0103-5
Wevers MR, Aaronson NK, Verhoef S et al (2014) Impact of rapid genetic counselling and testing on the decision to undergo immediate or delayed prophylactic mastectomy in newly diagnosed breast cancer patients: findings from a randomised controlled trial. Br J Cancer 110(4):1081–1087
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424
Lee DS, Yoon SY, Looi LM et al (2012) Comparable frequency of BRCA1, BRCA2 and TP53 germline mutations in a multi-ethnic Asian cohort suggests TP53 screening should be offered together with BRCA1/2 screening to early-onset breast cancer patients. Breast Cancer Res 14(2):R66. https://doi.org/10.1186/bcr3172
Ang P, Lim IH, Yong RY, Lee AS (2009) A molecular approach for identifying individuals with Li–Fraumeni syndrome who have a limited family history. Clin Genet 75(3):294–297
Carraro DM, Koike Folgueira MA, Garcia Lisboa BC et al (2013) Comprehensive analysis of BRCA1, BRCA2 and TP53 germline mutation and tumor characterization: a portrait of early-onset breast cancer in Brazil. PLoS ONE 8(3):e57581
Rath MG, Masciari S, Gelman R et al (2013) Prevalence of germline TP53 mutations in HER2+ breast cancer patients. Breast Cancer Res Treat 139(1):193–198
O’Shea R, Clarke R, Berkley E et al (2017) Next generation sequencing is informing phenotype: a TP53 example. Fam Cancer 17(1):123–128
Schon K, Tischkowitz M (2018) Clinical implications of germline mutations in breast cancer: TP53. Breast Cancer Res Treat 167(2):417–423
Heymann S, Delaloge S, Rahal A et al (2010) Radio-induced malignancies after breast cancer postoperative radiotherapy in patients with Li–Fraumeni syndrome. Radiat Oncol 5:104
Lammens C, Bleiker E, Aaronson N et al (2009) Attitude towards pre-implantation genetic diagnosis for hereditary cancer. Fam Cancer 8(4):457–464
PGD Netherlands (2017) Annual report 2017 [Internet]. https://www.pgdnederland.nl/en/annual-reports. Accessed 7 Nov 2018
Ballinger ML, Best A, Mai PL et al (2017) Baseline surveillance in Li–Fraumeni Syndrome using whole-body magnetic sesonance imaging: a meta-analysis. JAMA Oncol 3(12):1634–1639
Villani A, Tabori U, Schiffman J et al (2011) Biochemical and imaging surveillance in germline TP53 mutation carriers with Li–Fraumeni syndrome: a prospective observational study. Lancet Oncol 12(6):559–567
Villani A, Shore A, Wasserman JD et al (2016) Biochemical and imaging surveillance in germline TP53 mutation carriers with Li–Fraumeni syndrome: 11 year follow-up of a prospective observational study. Lancet Oncol 17(9):1295–1305
McBride KA, Ballinger ML, Killick E et al (2014) Li–Fraumeni syndrome: cancer risk assessment and clinical management. Nat Rev Clin Oncol 11(5):260–271
Ruijs MWG, Loo CE, van Buchem CAJM, Bleiker EMA, Sonke GS (2017) Surveillance of Dutch patients with Li–Fraumeni syndrome: the LiFe-Guard Study. JAMA Oncol 3(12):1733–1734
Peterson SK, Pentz RD, Marani SK et al (2008) Psychological functioning in persons considering genetic counseling and testing for Li–Fraumeni syndrome. Psychooncology 17(8):783–789
Lammens CR, Aaronson NK, Wagner A et al (2010) Genetic testing in Li–Fraumeni syndrome: uptake and psychosocial consequences. J Clin Oncol 28(18):3008–3014
Lammens CR, Bleiker EM, Verhoef S et al (2011) Distress in partners of individuals diagnosed with or at high risk of developing tumors due to rare hereditary cancer syndromes. Psychooncology 20(6):631–638
Azzollini J, Mariani M, Peissel B, Manoukian S (2018) Increased access to TP53 analysis through breast cancer multi-gene panels: clinical considerations. Fam Cancer 17(3):317–319
MacFarland SP, Maxwell KN (2018) The differential diagnosis of a TP53 genetic testing result. Genet Med 20(8):806–808
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Medical Research Ethical Committee concluded that the Medical Research Human Subject Acts (WMO) does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bakhuizen, J.J., Hogervorst, F.B., Velthuizen, M.E. et al. TP53 germline mutation testing in early-onset breast cancer: findings from a nationwide cohort. Familial Cancer 18, 273–280 (2019). https://doi.org/10.1007/s10689-018-00118-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-018-00118-0