Abstract
Lynch syndrome is the hereditary disorder that most frequently predisposes to colorectal cancer as well as predisposing to a number of extracolonic cancers, most prominently endometrial cancer. It is caused by germline mutations in the mismatch repair genes. Both its phenotype and genotype show marked heterogeneity. This review gives a historical overview of the syndrome, its heterogeneity, its genomic landscape, and its implications for complex diagnosis, genetic counseling and putative implications for immunotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lynch syndrome (LS) is the hereditary disorder that most frequently predisposes to colorectal cancer (CRC). An estimated one of every 35 cases of CRC is attributable to LS [1] and certain extracolonic cancers are also integral to the syndrome; endometrial cancer is the most predominant of these. It is estimated that one million individuals in the United States carry LS mutations, with only 5% of these being aware of their cancer predisposition [2].
History of Lynch syndrome
The history of LS begins in 1895 with Aldred Warthin, a pathologist, who documented three families that showed a pronounced excess of cancers, particularly involving the colorectum, stomach, and endometrium, with patterns consistent with autosomal dominant inheritance [3]. In 1962, Lynch encountered a patient from Nebraska with a similar family history. Shaw, of the University of Michigan, also had a family with strikingly similar clinical and pathology characteristics. The pedigrees from both families were published together in 1966 [4].
These early reports, along with identification of other families with similar histories, provided a more comprehensive picture of the LS phenotype and led to the establishment of clinical diagnostic criteria and management guidelines for affected families. During the 1990s, links between LS and mutations in DNA mismatch repair (MMR) genes were established [5,6,7,8,9]. In 2009, Ligtenberg et al. [10] demonstrated that germline deletions on the EPCAM gene resulted in silencing of the adjacent MSH2 gene.
In the late 1980s, criteria for Lynch syndrome began to emerge. The Amsterdam Criteria [11] were intended to be used to assure that collaborating researchers in different parts of the world were following common criteria in classifying research subjects rather than being intended to be used to diagnose the syndrome clinically. They were found to be rather limiting, and the less stringent Amsterdam Criteria II [12] were developed. Subsequently, an even wider approach to diagnosis of the syndrome was developed, referred to as the Bethesda Guidelines [13], which were meant to identify those who should receive microsatellite instability (MSI) testing. These were subsequently expanded by including pathology features, and since then have been known as the Revised Bethesda Guidelines [14]. However, these criteria for LS diagnosis harbor major limitations. Boland and Shike [15] determined that screening of all CRC patients meeting the Amsterdam Criteria would fail to detect half of the cases of LS, while screening all patients meeting Bethesda Guidelines for MSI testing would fail to detect about one-third of LS cases.
In 1981 [16], the Muir-Torre syndrome with sebaceous and other skin tumors was identified as a variant of LS. In 1994 [17], LS was found to include significantly increased frequencies of cancers of the stomach, small bowel, hepatobiliary system, upper urologic tract, and ovary. A follow-up study in 2008 [18] added glioblastomas to the list and found that trials of diagnostic and preventive measures could be justified for urologic tract and ovarian cancers in some LS subgroups, especially MSH2 mutation carriers and individuals over a certain age (approaching or over age 50 for urologic tract and over 40 for ovarian cancer). More recently, cancers of the pancreas [19], breast [20], prostate [21], and the rare adrenocortical [22] tumors have been considered to be overrepresented in patients with LS. See the National Comprehensive Cancer Network Guidelines for Genetic/Familial High-Risk Assessment: colorectal cancer, page LS-B [23] for a table giving a detailed risk overview of those cancers integral to LS.
Genomic basis of Lynch syndrome
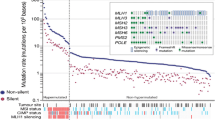
LS is inherited in an autosomal dominant pattern, which is caused by heterozygous germline mutations in the DNA MMR genes [24]: MLH1 [25], located on chromosome 3p21.3; MSH2 [26] and MSH6 [9], both located on 2p21; and PMS2 [8], located on 7p22. Mutations in MMR genes decrease an individual’s ability to repair base pair mismatches that occur during cell division, thereby predisposing carriers to high lifetime risks of developing MMR-deficient cancer(s). A proportion of patients without an identified genetic mutation within a MMR gene have a germline deletion spanning the 3′ end of the epithelial cell adhesion molecule (EPCAM) gene that is located immediately 5′ of MSH2 [27] and which silences the MSH2 gene in epithelial cells [10, 28]. Approximately one-third of suspected LS cases have no identifiable pathogenic mutation. An alternative mechanism in a portion of these cases is constitutional epimutation of MLH1 or MSH2 [29] which is characterized by methylation and transcriptional inactivation of an allele. MSH2 and some MLH1 epimutations have been linked to genetic alterations and show a dominant inheritance pattern; other MLH1 epimutations are reversible between generations and show non-Mendelian inheritance patterns [29].
MSI is a consequence and a characteristic of MMR-deficient tumors. MSI involves the accumulation of length variations in repetitive DNA sequences referred to as microsatellites. MSI indicates a defect in MMR which can be characterized by a hypermutable phenotype with a high mutational load.
The identification of MSI in LS-associated tumors and the use of immunohistochemistry to detect losses of expression of the MMR proteins have revolutionized the diagnosis of LS and enabled the possibility of testing all CRC and endometrial cancers to determine the probability of LS being present in the patient [1, 30, 31]. MSI and/or MMR protein expression status are now used as the first step in so-called “universal testing” schemes to identify patients with an increased risk of having LS.
Win et al. [32] estimated population carrier frequency of pathogenic MMR mutations to be 1/714 for PMS2, 1/758 for MSH6, 1/1,946 for MLH1, and 1/2,841 for MSH2. These authors calculated that these figures would lead to a population estimate of 1/279 for any MMR gene (note: they found no EPCAM mutation carriers in their cohort).
It has usually been reported that an estimated 80–90% of LS involves mutations in MLH1 or MSH2, while mutations in MSH6 or PMS2 account for 10–20% [27]. Up to 3% of LS is caused by an EPCAM mutation. However, these frequencies have been reported in patients ascertained via fulfillment of the Amsterdam or Bethesda clinical criteria for a presentation of CRC or endometrial cancer, which may have been biased against the identification of MSH6 and PMS2 mutations [33, 34].
Soares et al. [35] have found next-generation sequencing to be an efficient strategy that reduces time and expense in identifying mutations in MMR genes.
Differential diagnosis
Hereditary nonpolyposis colorectal cancer (HNPCC) was historically synonymous with LS, but it is now possible to differentiate among familial nonpolyposis CRC syndromes on the basis of a mutated gene [36]. Differentiation of HNPCC disorders can be aided by molecular analysis of tumors and germline mutation testing, and has implications for their diagnosis and management [36] (see Table 1). Conditions associated with defective DNA MMR include LS (germline MMR mutation), constitutional MMR deficiency syndrome (biallelic germline MMR mutations) [37], Lynch-like syndrome (some cases caused by biallelic somatic MMR mutations, some due to unknown causes) [38], and sporadic CRC with MSI (somatic biallelic methylation of MLH1) [39]. An HNPCC condition with proficient DNA MMR is known as familial CRC type X [40], which is familial nonpolyposis CRC that meets the Amsterdam criteria for HNPCC but is microsatellite stable (MSS) as well as MMR proficient.
Garre et al. [41] compared familial CRC type X (which they refer to as MSS-HNPCC), LS, and sporadic CRC. Similar to previous studies, they found MSS-HNPCC to have earlier age at CRC diagnosis and increased CRC incidence in relatives when compared with sporadic CRC, as well as distal tumor preference and more frequent presence of tumors when compared with LS. New findings were increased extracolonic cancers and improved overall survival in MSS-HNPCC when compared with sporadic CRC. In MSS-HNPCC families, incidences of CRC and endometrial cancer were higher than in sporadic CRC relatives but lower than in LS families; kidney and stomach cancers were higher than in sporadic CRC and similar to LS.
The majority of MSI is found in a subset of sporadic tumors, where it is caused by methylation of MLH1. Testing for BRAF mutation is often used to rule out LS in these cases, since BRAF V600E is closely associated with somatic MLH1 methylation. However, Adar et al. [42] have proposed a hybrid approach utilizing both BRAF genotyping and testing for MLH1 methylation, which could significantly reduce the number of methylation assays performed and reduce the referral rate for genetic testing.
Boulagnon et al. [43] have discussed the application of immunohistochemistry and molecular morphology relevant to their importance in the detection of BRAF mutation in CRC to enable the discrimination between sporadic and LS-related CRC. Therein, BRAF-specific antibody can be used effectively on tissue microarray in order to screen BRAF-mutated CRCs [42].
Heterogeneity
According to Vogelstein et al. [44], four types of genetic heterogeneity can be involved in tumorigenesis: (1) intratumoral: heterogeneity among the cells of one tumor; (2) intermetastatic: heterogeneity among different metastasized lesions in the same individual; (3) intrametastatic: heterogeneity among the cells of an individual metastasis; and (4) interpatient: heterogeneity among the tumors of different individuals. Interpatient heterogeneity accounts for no two cancer patients having identical clinical courses. Some of the difference could be attributable to host factors such as germline mutations, some to nongenetic factors, and some to variation of somatic mutations occurring within tumors. This interpatient heterogeneity makes development of uniform cancer treatments difficult and drives research into individualized treatments through genome-based medicine. Because of intrametastatic heterogeneity, most patients will need to be treated with at least two drugs which target different pathways.
Significant inter-patient heterogeneity exists among patients with LS and this poses challenges for diagnosis and clinical management. Some of this heterogeneity may be attributed to which of the MMR genes is mutated. Lifetime risk of CRC for MLH1 or MSH2 mutation carriers is estimated to be 52–85%, while that for MSH6 mutation carriers is 10–22% and that for PMS2 mutation carriers is 15–20%. Lifetime risk of endometrial cancer for MLH1 or MSH2 mutation carriers is 25–60%, while this risk is 16–26% for MSH6 and 15% for PMS2. (It is essential to observe that even these lower risks are substantially higher than those for the general population, which are 4.5% for CRC and 2.7% for endometrial cancer.) [23]. For patients with an EPCAM deletion, the lifetime risk for CRC is equivalent to patients with an MSH2 mutation, but the lifetime risks for extracolonic cancers is lower (~12% for endometrial cancer), unless the deletion extends into MSH2 [45, 46]. This difference has been attributed to the tissue-specific effects of the EPCAM deletion on downstream inactivation of MSH2, whereby MSH2 inactivation occurs predominantly in epithelial cells including the colonic mucosa [10]. The mean age of onset for the major LS cancers also differs by gene mutated, with cancer diagnoses occurring at a younger age in carriers of MLH1 and MSH2 mutations. The phenotypic heterogeneity by gene mutated has led to recommendations for a new classification for LS, whereby the gene mutated is now designated, as well as tailored clinical management of the varied cancer risks. Patients with MLH1- or MSH2-LS are advised to undergo colonoscopy every 1–2 years from age 20–25 and have additional surveillance of endometrium, ovaries and urinary tract, whereas carriers of mutations in MSH6 or PMS2 are advised to have a colonoscopy every 1–2 years from age 25–30 and additional surveillance of the endometrium and ovaries [47].
Møller et al. [48], used an observational international multi-center study with the objective of determining prospectively observed incidences of cancers and survival in pathogenic MMR mutation carriers up to 75 years of age. The conclusion was that as carriers of different pathologic MMR variants aged, they showed distinct patterns of cancer risk and survival. Therein, estimates for counseling and planning of surveillance strategies should be tailored to each patient from the perspectives of age, gender, and the pathologic MMR variant.
There is heterogeneity even among family members sharing the same mutation. Clearly the MMR mutation is not the whole story and other factors, such as environmental or polygenic factors, may influence phenotypic expression.
Watson et al. [49] found an association between tobacco use and CRC in LS, but did not find a phenotypic association involving alcohol use. Burn et al. [50] identified a long-term reduction of cancer associated with aspirin use. Donald et al. [51] noted that LS has a variable phenotypic expression that remains largely unexplained and suggest that more investigation is warranted. They concluded that currently there is no consistent evidence of low penetrance genetic modifiers that affect the LS phenotype.
In terms of diagnosis, Yamano et al. [34] note that patients with LS may be overlooked as a result of the syndrome’s heterogeneity. Historically, MSH6 and PMS2 cases may have been underdiagnosed because they did not fulfill the clinical criteria of the Amsterdam or Bethesda guidelines due to their lower penetrance and later age of cancer onset. It is also pointed out by ten Broeke et al. [52] that technical difficulties have possibly led to underreporting of PMS2 mutations, although new strategies have reduced this difficulty; these authors found significantly raised standardized incidence ratios for cancers of the small bowel, ovaries, breast, and renal pelvis in carriers of PMS2 mutations, with lower rates of CRC and endometrial cancer when compared with carriers of other MMR mutations. In an earlier study, Senter et al. [53] found PMS2 mutations to have lower penetrance than other MMR genes, although they determined that the incidence of CRC among PMS2 mutation carriers was 5.2-fold higher than the general population and the incidence of endometrial cancer was 7.5-fold higher.
A recent study by Espenschied et al. [33] presented data that led them to suggest that some MSH6 and PMS2 mutation carriers may present with a hereditary breast-ovarian cancer (HBOC)-like phenotype and are more likely to be missed by current LS screening and testing, which tends to concentrate on occurrences of CRC and endometrial cancer. Espenschied et al. [33] reviewed the clinical histories of patients who had undergone multigene panel testing for a diagnosis of CRC and/or endometrial cancer, and/or breast cancer, and/or ovarian cancer. Of their 528 MMR mutation carriers identified, 22.2% met BRCA1 and BRCA2 (BRCA1/2) testing criteria but not LS criteria while 5.1% met neither BRCA1/2 nor LS testing criteria. MSH6 and PMS2 mutations were more frequent than MLH1 and MSH2 mutations among patients who met BRCA1/2 testing criteria but did not meet LS testing criteria (P = 4.3 × 10−7). It was noted that 11.9% (63) of the 528 MMR mutation carriers had breast cancer only, while 27.3% (144) had CRC only, and 27.5% presented with breast or ovarian cancer as their first primary cancer. Of further interest, mutations of MSH6 or PMS2 were significantly more frequent than mutations of MLH1 or MSH2 in patients with breast cancer only compared with patients with CRC only (P = 2.3 × 10−5) [33]. A similar trend was found for ovarian cancer only, but this did not reach statistical significance. The authors noted that patients with HBOC were over-represented in this high-risk cohort, which may have incurred some bias in the mutation frequencies detected by multigene panel testing. Furthermore, the rates of MSH6 and PMS2 mutations detected in their cancer cohort were only marginally higher than the population-based rates estimated by Win et al. [32]. Nevertheless, Espenschied et al. note that their data may give insight into why MSH6 and PMS2 mutations have been under-represented in previous reports and suggest they may be under-identified in general [33].
Kloor et al. [54] gave emphasis to CRC being a heterogeneous tumor type with regard to molecular pathogenesis and genetic instability. Therein, the majority of CRCs display chromosomal instability which follows the classical adenoma-carcinoma sequence of tumor progression. The authors note that a subset of approximately 15% of CRCs display DNA MMR deficiency and a high level of MSI (MSI-H). Therein, MSI-H CRCs can be either sporadic tumors or LS-related CRCs. These observations harbor important clinical relevance. Specifically, the MSI-H phenotype poses a hallmark of LS-associated cancers which is of diagnostic relevance with respect to the identification of LS mutation carriers. MSI-H CRCs are characterized by distinct clinical behavior which may result from their particular molecular pathogenesis and therefore gives rise to MSI testing for its clinical significance wherein the MSI-H phenotype shows association with “…proximal tumor localization, a dense local lymphocyte infiltration, and a low frequency of distant organ metastasis. Moreover, MSI-H colorectal cancers have a better prognosis than their microsatellite-stable counterparts.” Furthermore, these authors concluded that “…the clinical characteristics of MSI-H cancers are closely linked to their molecular pathogenesis and research on the molecular alteration characteristic of MSI-H cancers may provide a basis for novel diagnostic or therapeutic approaches.” [54].
Management
Surveillance for CRC in MMR mutation carriers has the potential to be effective and considerably more cost effective than foregoing surveillance [55,56,57]. Because of the early age of CRC onset in LS and the predominance of proximal colon involvement, full colonoscopy should be initiated by age 20–25. Because of accelerated carcinogenesis compared to non-MMR CRCs (CRC in 2–3 years compared with 8–10 years for non-MMR CRCs) [58], colonoscopy should be performed at least every 1–2 years. The early age of onset, right-sided predominance, and accelerated carcinogenesis lead to the conclusion stated by Kravochuck and Church [59] that, with respect to colonoscopy in LS patients, there is “no room for error.”
Haanstra et al. [60] have reviewed studies of new techniques for identifying carcinoma and precancer in the colorectum in LS patients, inclusive of narrow-band imaging [61], chromoendoscopy (topical application of stains during endoscopy to improve polyp detection) [62,63,64,65], autofluorescence endoscopy [66], and I-SCAN (digital enhancement of surfaces and contrast) and endomicroscopy. At the time of their review, none of these new techniques had been found to have clear and convincing superiority over conventional colonoscopy, although chromoendoscopy has advantages as the equipment is inexpensive and the procedure is easily performed.
Rahmi et al. [67] in a multicenter trial compared standard colonoscopy with standard colonoscopy followed by chromoscopy while screening 78 LS patients. Significantly more patients with at least one adenoma were identified by chromocolonoscopy (32/78 [41%]) than by standard colonoscopy (18/78 [23%]; P < 0.001). However, it is difficult to ascertain if improved adenoma detection was due to chromoendoscopy, or was merely the result of a “second pass” of the colonoscope.
Bisschops et al. [68] accounted for the second pass effect while comparing I-SCAN with standard colonoscopy. LS patients were randomized to either standard colonoscopy followed by I-SCAN (n = 31) or I-SCAN first followed by standard colonoscopy (n = 30). When standard colonoscopy was performed first, five adenomas were detected and removed and a second pass with I-SCAN detected a further eight adenomas. When I-SCAN was used first, 15 adenomas were removed and subsequent standard colonoscopy detected two additional adenomas. The adenoma miss rate was significantly higher for standard colonoscopy (62%) compared with I-SCAN (12%; RR 0.44, 95% confidence interval 0.21–0.87; P = 0.007).
Subtotal colectomy in LS patients at the time of first CRC has been shown to decrease incidence of metachronous CRCs [69] and the need for subsequent abdominal surgery when compared with more limited surgery [70].
Lynch et al.[71] have strongly advocated offering prophylactic subtotal colectomy to patients who have tested positive for a germline mutation for LS, or who are obligate mutation carriers. They cite the limitations of colonoscopy, the potential for the rapid rate of cancer progression, and the high penetrance of the germline mutation. Subtotal colectomy as a prophylactic measure among LS patients remains controversial because the risk of metachronous CRCs must be considered against the possible negative consequences of the more extensive surgery [72]. It must involve genetic counseling, as well as input from the surgeon, to aid patients in assessing various management strategies. Using a decision analysis model for Lynch patients at age 25 years, Syngal et al. [73] calculated life expectancy improvements of 13.5 years for colonoscopy, and 15.6 years for prophylactic proctocolectomy (compared with no intervention). Prophylactic colectomy has been suggested [74, 75] as an option for patients likely to show poor compliance with colonoscopy.
Liska and Kalady [76] point out that there are no prospective clinical studies evaluating the potential survival benefit of prophylactic colectomy in LS and should only be offered in special circumstances: patients who have a colon that is technically difficult to examine endoscopically, those with poor compliance with screening recommendations, and those who have severe psychological fear of developing colorectal cancer, and it is also to be considered for patients in families with severe penetrance of disease or early-age onset of CRC.
Clinical practice guidelines for LS from the US Multi-Society Task Force on Colorectal Cancer guidelines [77] include colectomy with ileorectal anastomosis as the primary treatment for LS patients with CRC or colon neoplasia not removable by endoscopy. They note that less-extensive surgery could be considered in patients older than 60–65 years of age and those with underlying sphincter dysfunction. Church [78] notes that in cases where genotype, phenotype, and family history increase CRC risk, earlier and more aggressive surgery is appropriate; a balance of cancer prevention with lifestyle considerations should be maintained.
Endometrial cancer is the most frequently occurring extracolonic cancer in LS and women with a LS germline mutation have an increased incidence rate for ovarian cancer. Because of limited effectiveness of surveillance for endometrial [79] and, especially, ovarian cancer, prophylactic hysterectomy and bilateral salpingo-oophorectomy can be considered after childbearing is completed in germline MMR mutation carriers [80]. Such surgery has been shown to effect a significant reduction in endometrial and ovarian cancer among LS patients [81]. Clinical practice guidelines from the US Multi-Society Task Force on Colorectal Cancer guidelines [77] recommend prophylactic hysterectomy and bilateral salpingo-oophorectomy for women with LS who have finished childbearing, or at 40 years of age. In a recent study involving 1942 LS mutation carriers, the Mallorca Group found good survival of endometrial and ovarian cancer, but it is not clear whether this was due to surveillance or to more favorable tumor characteristics in LS-associated cancers when compared with sporadic disease [82]. Each of LS’s integral cancers may harbor significant attributes for early detection and prevention which will affect genetic counseling, surveillance and management [23]. Møller et al. [83] studied subsequent cancers in patients with LS and found that favorable survival validated the importance of continuous follow-up after subsequent cancers, with the primary mission of cancer prevention and decrease of death from cancer.
Immunotherapy
A promising avenue of research is linking cancer genetics to immunotherapy. Approximately 15% of sporadic CRCs and most LS-associated CRCs show MSI. Llosa et al. [84] examined the immune microenvironment of CRCs. They found that a subset, virtually all of which had MSI, showed high infiltration with activated CD8+ cytotoxic T lymphocyte (CTL) and activated Th1 cells. This is the first link described between a genetically defined subset of cancer and the corresponding expression of immune checkpoints; MSI-H tumors showed expression of at least five checkpoint molecules (PD-1, PD-L1, CTLA-4, LAG-3, and IDO) that are targeted by inhibitors that are currently being clinically tested.
Since almost all tumors in patients with LS are deficient in MMR, those with metastatic disease can benefit from this therapy along with patients who have sporadic MMR deficiency. This therapy does not attempt to kill cancer cells directly but instead blocks a pathway that protects cancer cells from the body’s immune system which is able to fight cancer. One pathway includes the programmed death-1 (PD-1) protein which is expressed on the surface of immune cells and the programmed death ligand-1 (PD-L1) which is expressed on cancer cells. When PD-1 and PD-L1 join together, they protect tumor cells from being destroyed by the immune system by forming a shield that does not allow the immune system to recognize and attack the tumor cell. Therefore, blocking PD-1 or PD-L1 can interrupt that shield and allow the immune system to destroy the tumor [85]. See Fig. 1.
Binding of the TCR to the peptide:MHC complex alone is not sufficient to activate T cells. Costimulation is necessary from the binding of B7-1/B7-2 to CD28. Inhibitory receptors such as PD-1 and CTLA-4 have been discovered, which blunt costimulation, prevent T cell activation, and result in T cell anergy and/or apoptosis. TCR T cell receptor, MHC major histocompatibility, APC antigen presenting cell. Reprinted from Pharmacological Research. Vol. 120, pp. 1–9. Sweis and Luke [85], Mechanistic and pharmacologic insights on immune checkpoint inhibitors. Copyright 2017, with permission from Elsevier
“Both ligands are expressed in response to γ-chain cytokines, Type I interferons, and interferon-γ. GM-CSF and IL-4 can also induce expression of PD-L2. Expression of PD-L1 occurs not only on immune cells, but also epithelial cells including cancer cells. Binding of ligands to PD-1 inhibits T cell activation, and thus dampens the immune response.” [85].
The first clinical study of ipilimumab was published in 2003 and included 14 patients with metastatic melanoma. In that study, ipilimumab was administered by IV and was effective [86].
Le et al. [87] showed that MMR status in gastrointestinal cancers predicted whether immune checkpoint blockade with pembrolizumab would provide clinical benefit.
The majority of MMR-deficient endometrial tumors have been found to be PD-L1 positive in at least a subset of tumor cells [88]. Furthermore, it was found that tumoral PD-L1 expression is more common in LS-associated endometrial cancers relative to MLH1 hypermethylated and MMR-intact tumors, although sporadic cancers often show PD-L1 positive immune staining. These data suggest that MMR deficiency may be a better predictor of response to PD-1/PD-L1 inhibitor therapy than tumor grade in endometrial cancer and that the potential benefit may be based on the molecular mechanism of MMR defects [88].
Once CTLA-4 and PD-1/PD-L1 were determined to be negative regulators of anti-tumor immunity, clinical exploration of antibodies targeting these pathways ensued between 2011 and 2017 for immune checkpoint inhibitors were approved for six different diseases [85].
Within a tumor microenvironment, this requires uptake of peptide fragments by specialized antigen presenting cells (APCs) driven by Type I interferons which cross present them to T cells in the tumor draining lymph nodes [85].
Boland noted that previously it had been shown that MSI CRCs do not respond favorably to conventional cytotoxic adjuvant chemotherapy with 5-fluorouricil (5-FU) and that this treatment may even worsen outcome [89]. However, in a study by Bertagnolli et al. [90], MSI-H CRCs had improved outcomes when compared with MS-stable tumors when irinotecan was added to 5-fluorouracil/leucovorin in the adjuvant setting, suggesting that MSI-H/LS-associated CRCs may have improved response at least to irinotecan as a cytotoxic agent.
Boland [91] has developed a discussion of what he refers to as immunotherapy for LS dealing with a matter of speculation as to whether MMR-deficient crypts may be precursors of genuinely neoplastic tissues. However, investigators have demonstrated that the causal frameshift mutations give rise to immunogenic neoantigens [92] with neoantigenic peptides occurring in most MMR-defective neoplasms, and appearing repeatedly in an individual with LS. These neoantigens induce an antibody response [93] and tumor infiltrating lymphocyte (TIL) response typical of MMR-defective tumors [94]. Therein, these TILs are activated CD8+ T cells associated with early-stage tumors and the absence of lymph node metastases [95]. It has been proposed that immunizing LS patients with frameshift peptides may prevent cancer in such individuals [96]. Westdorp et al. [97] noted that neoantigen-based vaccination currently is being studied both in LS and in advanced-stage sporadic MSI CRC.
Predictive biomarkers are central to the concept of precision cancer medicine. Such validated predictive biomarkers such as BRCA1, BRCA2, and the MMR germline mutations in LS, among others, can often be effectively employed in the selection of individual patients for targeted treatment. For example, patients with BRCA mutations respond better to PARP inhibitors [98] and LS metastatic patients respond better to anti PD-1 [99]. On the other hand, a prognostic biomarker such as cancer stage or grade will be limited to providing statistical probability inclusive of survival estimates.
Conclusion
Precision medicine, which will include personalized medicine and genomic medicine as well as individualized medicine, is becoming a triumph for certain hereditary disorders inclusive of LS. With the continued advancements of immunotherapy and genomics, we should explore ways to combine various therapies to cure cancer. Significant challenges include research on predictive biomarkers as well as insight into the management of immune related toxicities and, finally, reversing mechanisms of primary and secondary resistance [85]. Full application of genomic and personalized medicine in health care will require dramatic changes in regulatory and reimbursement policies, as well as legislative protections for privacy for its system-wide adoption. Thus, there are challenges from both a scientific and a policy perspective, but they will be met with the certainty that the science behind genomic medicine is sound and the practice of medicine that it informs is evidence based [100]. Recognition of LS patients who can fully benefit from the personalized management and treatment options for these patients will have the potential of being lifesaving.
References
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, Clendenning M, Sotamaa K, Prior T, Westman JA, Panescu J, Fix D, Lockman J, LaJeunesse J, Comeras I, de la Chapelle A (2008) Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J Clin Oncol 26:5783–5788
Blue Ribbon Panel: Cancer Moonshot Blue Ribbon Panel Report (2016) Available at: https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative/blue-ribbon-panel/blue-ribbon-panel-report-2016.pdf. Accessed 9 Oct 2017
Warthin AS (1913) Heredity with reference to carcinoma as shown by the study of the cases examined in the pathological laboratory of the University of Michigan, 1895–1913. Arch Intern Med 12:546–555
Lynch HT, Shaw MW, Magnuson CW, Larsen AL, Krush AJ (1966) Hereditary factors in cancer: study of two large Midwestern kindreds. Arch Intern Med 117:206–212
Peltomäki P, Aaltonen L, Sistonen P, Pylkkänen L, Mecklin J-P, Järvinen H, Green JS, Jass JR, Weber JL, Leach FS, Petersen GM, Hamilton SR, de la Chapelle A, Vogelstein B (1993) Genetic mapping of a locus predisposing to human colorectal cancer. Science 260:810–812
Lindblom A, Tannergard P, Werelius B, Nordenskjold M (1993) Genetic mapping of a second locus predisposing to hereditary nonpolyposis colorectal cancer. Nat Genet 5:279–282
Leach FS, Nicolaides NC, Papadopoulos N, Liu B, Jen J, Parsons R, Peltomaki P, Sistonen P, Aaltonen LA, Nystrom-Lahti M, Guan X-Y, Zhang J, Metzler PS, Yu J-W, Kao F-T, Chen DJ, Cerosaletti KM, Fournier REK, Todd S, Lewis T, Leach RJ, Naylor SL, Weissenbach J, Mecklin J-P, Jarvinen H, Petersen GM, Hamilton SR, Green J, Jass J, Watson P, Lynch HT, Trent JM, de la Chapelle A, Kinzler KW, Vogelstein B (1993) Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell 75:1215–1225
Nicolaides NC, Papadopoulos N, Liu B, Wei Y-F, Carter KC, Ruben SM, Rosen CA, Haseltine WA, Fleischmann RD, Fraser CM, Adams MD, Venter JC, Dunlop MG, Hamilton SR, Petersen GM, de la Chapelle A, Vogelstein B, Kinzler KW (1994) Mutations of two PMS homologues in hereditary nonpolyposis colon cancer. Nature 371:75–80
Miyaki M, Konishi M, Tanaka K, Kikuchi-Yanoshita R, Muraoka M, Yasuno M, Igari T, Koike M, Chiba M, Mori T (1997) Germline mutation of MSH6 as the cause of hereditary nonpolyposis colorectal cancer. Nat Genet 17:271–272
Ligtenberg MJL, Kuiper RP, Chan TL, Goossens M, Hebeda KM, Voorendt M, Lee TYH, Bodmer D, Hoenselaar E, Hendriks-Cornelissen SJB, Tsui WY, Kong CK, Brunner HG, van Kessel AG, Yuen ST, van Krieken JHJM, Leung SY, Hoogerbrugge N (2009) Heritable somatic methylation and inactivation of MSH2 in families with Lynch syndrome due to deletion of the 3´ exons of TACSTD1. Nat Genet 41:112–117
Vasen HFA, Mecklin J-P, Khan PM, Lynch HAT (1991) The International Collaborative Group on hereditary nonpolyposis colorectal cancer (ICG-HNPCC). Dis Colon Rectum 34:424–425
Vasen HFA, Watson P, Mecklin J-P, Lynch HT, ICG-HNPCC (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative Group on HNPCC. Gastroenterology 116:1453–1456
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN, Srivastava S (1998) A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58:5248–5257
Laghi L, Bianchi P, Roncalli M, Malesci A (2004) Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 96:1402–1403
Boland CR, Shike M (2010) Report from the Jerusalem workshop on Lynch syndrome-hereditary nonpolyposis colorectal cancer. Gastroenterology 138:2197.e1–2197.e7
Lynch HT, Lynch PM, Pester J, Fusaro RM (1981) The cancer family syndrome: rare cutaneous phenotypic linkage of Torre’s syndrome. Arch Intern Med 141:607–611
Watson P, Lynch HT (1994) The tumor spectrum in HNPCC. Anticancer Res 14:1635–1640
Watson P, Vasen HFA, Mecklin J-P, Bernstein I, Aarnio M, Järvinen HJ, Myrhøj T, Sunde L, Wijnen JT, Lynch HT (2008) The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int J Cancer 123:444–449
Kastrinos F, Mukherjee B, Tayob N, Wang F, Sparr J, Raymond VM, Bandipalliam P, Stoffel EM, Gruber SB, Syngal S (2009) Risk of pancreatic cancer in families with Lynch syndrome. JAMA 302:1790–1795
Win AK, Young JP, Lindor NM, Tucker KM, Ahnen DJ, Young GP, Buchanan DD, Clendenning M, Giles GG, Winshiip I, Macrae FA, Goldblatt J, Southey MC, Arnold J, Thibodeau SN, Gunawardena SR, Bapat B, Baron JA, Casey G, Gallinger S, Le Marchand L, Newcomb PA, Haile RW, Hopper JL, Jenkins MA (2012) Colorectal and other cancer risks for carriers and noncarriers from families with a DNA mismatch repair gene mutation: a prospective cohort study. J Clin Oncol 30:958–964
Bauer CM, Ray AM, Halstead-Nussloch BA, Dekker RG, Raymond VM, Gruber SB, Cooney KA (2011) Hereditary prostate cancer as a feature of Lynch syndrome. Fam Cancer 10:37–42
Raymond VM, Everett JN, Furtado LV, Gustafson SL, Jungbluth CR, Gruber SB, Hammer GD, Stoffel EM, Greenson JK, Giordano TJ, Else T (2013) Adrenocortical carcinoma is a Lynch syndrome-associated cancer. J Clin Oncol 31:3012–3018
National Comprehensive Cancer Network (2017) NCCN guidelines version 1.2017, Lynch syndrome. Available at: http://www.nccn.org. Accessed 9 Oct 2017
Peltomäki P (2005) Lynch syndrome genes. Fam Cancer 4:227–232
Bronner CE, Baker SM, Morrison PT, Warren G, Smith LG, Lescoe MK, Kane M, Earabino C, Lipford J, Lindblom A, Tannergard P, Bollag RJ, Godwin AR, Ward DC, Nordenskjold M, Fishel R, Kolodner R, Liskay RM (1994) Mutation in the DNA mismatch repair gene homologue hMLH1 is associated with hereditary nonpolyposis colon cancer. Nature 368:258–261
Fishel R, Lescoe MK, Rao MRS, Copeland NG, Jenkins NA, Garber J, Kane M, Kolodner R (1993) The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 75:1027–1038
Carneiro da Silva F, Wernhoff P, Dominguez-Barrera C, Dominguez-Valentin M (2016) Update on hereditary colorectal cancer. Anticancer Res 36:4399–4406
Kovacs ME, Papp J, Szentirmay Z, Otto S, Olah E (2009) Deletions removing the last exon of TACSTD1 constitute a distinct class of mutations predisposing to Lynch syndrome. Hum Mutat 30:197–203
Hitchins MP (2013) The role of epigenetics in Lynch syndrome. Fam Cancer 12:189–205
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group (2009) Recommendations from the EGAPP Working Group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med 11:35–41
Hampel H, Frankel W, Panescu J, Lockman J, Sotamaa K, Fix D, Comeras I, La Jeunesse J, Nakagawa H, Westman JA, Prior TW, Clendenning M, Penzone P, Lombardi J, Dunn P, Cohn DE, Copeland L, Eaton L, Fowler J, Lewandowski G, Vaccarello L, Bell J, Reid G, de la Chapelle A (2006) Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res 66:7810–7817
Win AK, Jenkins MA, Dowty JG, Antoniou AC, Lee A, Giles GG, Buchanan DD, Clendenning M, Rosty C, Ahnen DJ, Thibodeau SN, Casey G, Gallinger S, Le Marchand L, Haile RW, Potter JD, Zheng Y, Lindor NM, Newcomb PA, Hopper JL, Macinnis RJ (2017) Prevalence and penetrance of major genes and polygenes for colorectal cancer. Cancer Epidemiol Biomarkers Prev 26:404–412
Espenschied CR, LaDuca H, Li S, McFarland R, Gau C-L, Hampel H (2017) Multigene panel testing provides a new perspective on Lynch syndrome. J Clin Oncol 35:2568–2575
Yamano T, Hamanaka M, Babaya A, Kimura K, Kobayashi M, Fukumoto M, Tsukamoto K et al (2017) Management strategies in Lynch syndrome and familial adenomatous polyposis: a national healthcare survey in Japan. Cancer Sci 108:243–249
Soares BL, Brant AC, Gomes R, Pastor T, Schneider NB, Ribeiro-dos-Santos Â, Pimentel de Assumpção P, Achatz MIW, Ashton-Prolla P, Moreira MAM (2017) Screening for germline mutations in mismatch repair genes in patients with Lynch syndrome by next generation sequencing. Fam Cancer. doi:10.1007/s10689-017-0043-5 (in press)
Carethers JM, Stoffel EM (2015) Lynch syndrome and Lynch syndrome mimics: the growing complex landscape of hereditary colon cancer. World J Gastroenterol 21:9253–9261
Wimmer K, Etzler J (2008) Constitutional mismatch repair-deficiency syndrome: have we so far seen only the tip of the iceberg? Hum Genet 124:105–122
Mensenkamp AR, Vogelaar IP, van Zelst-Stams WAG, Goossens M, Ouchene H, Hendriks-Cornelissen SJB, Kwint MP, Hoogerbrugge N, Nagtegaal ID, Ligtenberg MJL (2014) Somatic mutations in MLH1 and MSH2 are a frequent cause of mismatch-repair deficiency in Lynch syndrome-like tumors. Gastroenterology 146:643–646
Bettstetter M, Dechant S, Ruemmele P, Grabowski M, Keller G, Holinski-Feder E, Hartmann A, Hofstaedter F, Dietmaier W (2007) Distinction of hereditary nonpolyposis colorectal cancer and sporadic microsatellite-unstable colorectal cancer through quantification of MLH1 methylation by real-time PCR. Clin Cancer Res 13:3221–3228
Sánchez-Tomé E, Rivera B, Perea J, Pita G, Rueda D, Mercadillo F, Canal A, Gonzalez-Neira A, Benitez J, Urioste M (2015) Genome-wide linkage analysis and tumoral characterization reveal heterogeneity in familial colorectal cancer type X. J Gastroenterol 50:657–666
Garre P, Martín L, Bando I, Tosar A, Llovet P, Sanz J, Romero A, de la Hoya M, Díaz-Rubio E, Caldés T (2014) Cancer risk and overall survival in mismatch repair proficient hereditary non-polyposis colorectal cancer, Lynch syndrome and sporadic colorectal cancer. Fam Cancer 13:109–119
Adar T, Rodgers LH, Shannon KM, Yoshida M, Ma T, Mattia A, Lauwers GY, Iafrate AJ, Chung DC (2017) A tailored approach to BRAF and MLH1 methylation testing in a universal screening program for Lynch syndrome. Mod Pathol 30:440–447
Boulagnon C, Dudez O, Beaudoux O, Dalstein V, Kianmanesh R, Bouché O, Diebold M-D (2016) BRAFV600E gene mutation in colonic adenocarcinomas. Immunohistochemical detection using tissue microarray and clinicopathologic characteristics: an 86 case series. Appl Immunohistochem Mol Morphol 24:88–96
Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA Jr, Kinzler KW (2013) Cancer genome landscapes. Science 339:1546–1558
Kempers MJE, Kuiper RP, Ockeloen CW, Chappuis PO, Hutter P, Rahner N, Schackert HK, Steinke V, Holinski-Feder E, Morak M, Kloor M, Büttner R, Verwiel ETP, van Krieken JH, Nagtegaal ID, Goossens M, van der Post RS, Niessen RC, Sijmons RH, Kluijt I, Hogervorst FBL, Leter EM, Gille JJP, Aalfs CM, Redeker EJW, Hes FJ, Tops CMJ, van Nesselrooij BPM, van Gijn ME, Gómez Garcia EBG, Eccles DM, Bunyan DJ, Syngal S, Stoffel EM, Culver JO, Palomares MR, Graham T, Velsher L, Papp J, Oláh E, Chan TL, Leung SY, van Kessel AG, Kiemeney LALM, Hoogerbrugge N, Ligtenberg MJL (2011) Risk of colorectal and endometrial cancers in EPCAM deletion-positive Lynch syndrome: a cohort study. Lancet Oncol 12:49–55
Lynch H, Riegert-Johnson D, Snyder C, Lynch J, Hagenkord J, Boland CR, Rhees J, Thibodeau S, Boardman L, Davies J, Kuiper RP, Hoogerbrugge N, Ligtenberg M (2011) Lynch syndrome associated extracolonic tumors are rare in two extended families with the same EPCAM deletion. Am J Gastroenterol 106:1829–1836
Vasen HF, Tomlinson I, Castells A (2015) Clinical management of hereditary colorectal cancer syndromes. Nat Rev Gastroenterol Hepatol 12:88–97
Moller P, Seppala TT, Bernstein I, Holinski-Feder E, Sala P, Gareth ED, Lindblom A, Macrae F, Blanco I, Sijmons RH, Jeffries J, Vasen HFA, Burn J, Nakken S, Hovig E, Rodland EA, Tharmaratnam K, de Vos Tot Nederveen Cappel WH, Hill J, Wijnen JT, Jenkins MA, Green K, Lalloo F, Sunde L, Mints M, Bertario L, Pineda M, Navarro M, Morak M, Renkonen-Sinisalo L, Valentin MD, Frayling IM, Plazzer JP, Pylvanainen K, Genuardi M, Mecklin JP, Moeslein G, Sampson JR, Capella G. (2017) Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective Lynch syndrome database. Gut. doi:10.1136/gutjni-2017-314057 (in press)
Watson P, Ashwathnarayan R, Lynch HT, Roy HK (2004) Tobacco use and increased colorectal cancer risk in patients with hereditary nonpolyposis colorectal cancer (Lynch syndrome). Arch Intern Med 164:2429–2431
Burn J, Gerdes A-M, Macrae F, Mecklin J-P, Moeslein G, Olschwang S, Eccles D, Evans G, Maher ER, Bertario L, Bisgaard M-L, Dunlop MG, Ho JWC, Hodgson SV, Lindblom A, Lubinski J, Morrison PJ, Murday V, Ramesar R, Side L, Scott RJ, Thomas HJW, Vasen HF, Barker G, Crawford G, Elliott F, Movahedi M, Pylvanainen K, Wijnen JT, Fodde R, Lynch HT, Mathers JC, Bishop T, on behalf of the CAPP2 investigators (2011) Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. The Lancet 378:2081–2087
Donald N, Malik S, McGuire JL, Monahan KJ. (2017) The association of low penetrance genetic risk modifiers with colorectal cancer in lynch syndrome patients: a systematic review and meta-analysis. Fam Cancer. doi:10.1007/s10689-017-9995-8. (in press)
ten Broeke SW, Brohet RM, Tops CM, van der Klift HM, Velthuizen ME, Bernstein I, Munar GC, Garcia EG, Hoogerbrugge N, Letteboer TGW, Menko FH, Lindblom A, Mensenkamp AR, Moller P, van Os TA, Rahner N, Redeker BJW, Sijmons RH, Spruijt L, Suerink M, Vos YJ, Wagner A, Hes FJ, Vasen HF, Nielsen M, Wijnen JT (2015) Lynch syndrome caused by germline PMS2 mutations: delineating the cancer risk. J Clin Oncol 33:319–325
Senter L, Clendenning M, Sotamaa K, Hampel H, Green J, Potter JD, Lindblom A, Lagerstedt K, Thibodeau SN, Lindor NM, Young J, Winship I, Dowty JG, White DM, Hopper JL, Baglietto L, Jenkins MA, de la Chapelle A (2008) The clinical phenotype of Lynch syndrome due to germ-line PMS2 mutations. Gastroenterology 135:419–428
Kloor M, Staffa L, Ahadova A, von Knebel Doeberitz M (2014) Clinical significance of microsatellite instability in colorectal cancer. Langenbecks Arch Surg 399:23–31
Järvinen HJ, Aarnio M, Mustonen H, Aktan-Collan K, Aaltonen LA, Peltomäki P, de la Chapelle A, Mecklin J-P (2000) Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 118:829–834
Dove-Edwin I, Sasieni P, Adams J, Thomas HJW (2005) Prevention of colorectal cancer by colonoscopic surveillance in individuals with a family history of colorectal cancer: 16 year, prospective, follow-up study. BMJ 331:1047
Ladabaum U, Wang G, Terdiman J, Blanco A, Kuppermann M, Boland CR, Ford J, Elkin E, Phillips KA (2011) Strategies to identify the Lynch syndrome among patients with colorectal cancer: a cost-effectiveness analysis. Ann Intern Med 155:69–79
Lynch HT, Smyrk T, Jass JR (1995) Hereditary nonpolyposis colorectal cancer and colonic adenomas: aggressive adenomas? Semin Surg Oncol 11:406–410
Kravochuck SE, Church JM (2017) Colonoscopy in patients with Lynch syndrome: no room for error. ANZ J Surg 87:204–205
Haanstra JF, Kleibeuker JH, Koornstra JJ (2013) Role of new endoscopic techniques in Lynch syndrome. Fam Cancer 12:267–272
East JE, Suzuki N, Stavrinidis M, Guenther T, Thomas HJW, Saunders BP (2008) Narrow band imaging for colonoscopic surveillance in hereditary non-polyposis colorectal cancer. Gut 57:65–70
Stoffel EM, Turgeon DK, Stockwell DH, Zhao L, Normolle DP, Tuck MK, Bresalier RS, Marcon NE, Baron JA, Ruffin MT, Brenner DE, Syngal S, for Great Lakes-New England Clinical Epidemiology and Validation Center of the Early Detection Research Network (2008) Missed adenomas during colonoscopic surveillance in individuals with Lynch syndrome (hereditary nonpolyposis colorectal cancer). Cancer Prev Res 1:470–475
Lecomte T, Cellier C, Meatchi T, Barbier JP, Cugnenc PH, Jian R, Laurent-Puig P, Landi B (2005) Chromoendoscopic colonoscopy for detecting preneoplastic lesions in hereditary nonpolyposis colorectal cancer syndrome. Clin Gastroenterol Hepatol 3:897–902
Hurlstone DP, Karajeh M, Cross SS, McAlindon ME, Brown S, Hunter MD, Sanders DS (2005) The role of high-magnification-chromoscopic colonoscopy in hereditary nonpolyposis colorectal cancer screening: a prospective “back-to-back” endoscopic study. Am J Gastroenterol 100:2167–2173
Hüneburg R, Lammert F, Rabe C, Rahner N, Kahl P, Büttner R, Propping P, Sauerbruch T, Lamberti C (2009) Chromocolonoscopy detects more adenomas than white light colonoscopy or narrow band imaging colonoscopy in hereditary nonpolyposis colorectal cancer screening. Endoscopy 41:316–322
Ramsoekh D, Haringsma J, Poley JW, van Putten P, van Dekken H, Steyerberg EW, van Leerdam ME, Kuipers EJ (2010) A back-to-back comparison of white light video endoscopy with autofluorescence endoscopy for adenoma detection in high-risk subjects. Gut 59:785–793
Rahmi G, Lecomte T, Malka D, Maniere T, Le Rhun M, Guimbaud R, Lapalus M-G, Le Sidaner A, Moussata D, Caron O, Barbieux J-P, Gaudric M, Coron E, Barange K, Ponchon T, Sautereau D, Samaha E, Saurin J-C, Chaussade S, Laurent-Piug P, Chatellier G, Cellier C (2015) Impact of chromoendoscopy on adenoma detection in patients with Lynch syndrome: a prospective, multicenter, blinded, tandem colonoscopy study. Am J Gastroenterol 110:288–298
Bisschops R, Tejpar S, Willekens H, De Hertogh G, Van Cutsem E (2017) Virtual chromoendoscopy (I-SCAN) detects more polyps in patients with Lynch syndrome: a randomized controlled crossover trial. Endoscopy 49:342–350
Anele CC, Adegbola SO, Askari A, Rajendran A, Clark SK (2017) Risk of metachronous colorectal cancer following colectomy in Lynch syndrome: a systematic review and meta-analysis. Colorectal Dis 19:528–536
Natarajan N, Watson P, Silva-Lopez E, Lynch HT (2010) Comparison of extended colectomy and limited resection in patients with Lynch syndrome. Dis Colon Rectum 53:77–82
Lynch HT, Lynch JF, Fitzgibbons R (2003) Role of prophylactic colectomy in Lynch syndrome. Clin Colorectal Cancer 3:99–101
Parry S, Win AK, Parry B, Macrae FA, Gurrin LC, Church JM, Baron JA, Giles GG, Leggett BA, Winship I, Lipton L, Young GP, Young JP, Lodge CJ, Southey MC, Newcomb PA, Le ML, Haile RW, Lindor NM, Gallinger S, Hopper JL, Jenkins MA (2011) Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 60:950–957
Syngal S, Weeks JC, Schrag D, Garber JE, Kuntz KM (1998) Benefits of colonoscopic surveillance and prophylactic colectomy in patients with hereditary nonpolyposis colorectal cancer mutations. Ann Intern Med 129:787–796
Church JM (1996) Prophylactic colectomy in patients with hereditary nonpolyposis colorectal cancer. Ann Med 28:479–482
Lynch HT (1996) Is there a role for prophylactic subtotal colectomy among hereditary nonpolyposis colorectal cancer germline mutation carriers? Dis Colon Rectum 39:109–110
Liska D, Kalady MF (2015) Colorectal surgery in Lynch syndrome patients: when and how? Curr Colorectal Cancer Rep 11:45–53
Herzig DO, Buie WD, Weiser MR, You YN, Rafferty JF, Feingold D, Steele SR (2017) Clinical practice guidelines for the surgical treatment of patients with Lynch syndrome. Dis Colon Rectum 60:137–143
Church JM (2016) Controversies in the surgery of patients with familial adenomatous polyposis and Lynch syndrome. Fam Cancer 15:447–451
Lu KH, Daniels M (2013) Endometrial and ovarian cancer in women with Lynch syndrome: update in screening and prevention. Fam Cancer 12:273–277
Ryan NAJ, Evans DG, Green K, Crosbie EJ (2017) Pathological features and clinical behavior of Lynch syndrome-associated ovarian cancer. Gynecol Oncol 144:491–495
Schmeler KM, Lynch HT, Chen L-M, Munsell MF, Soliman PT, Clark MB, Daniels MS, White KG, Boyd-Rogers SG, Conrad PG, Yang KY, Rubin MM, Sun CC, Slomovitz BM, Gershenson DM, Lu KH (2006) Prophylactic surgery to reduce the risk of gynecologic cancers in the Lynch syndrome. N Engl J Med 354:261–269
Moller P, Seppala T, Bernstein I, Holinski-Feder E, Sala P, Evans DG, Lindblom A, Macrae F, Blanco I, Sijmons R, Jeffries J, Vasen H, Burn J, Nakken S, Hovig E, Rodland EA, de Tharmaratnam K, Hill J, Wijnen J, Green K, Lalloo F, Sunde L, Mints M, Bertario L, Pineda M, Navarro M, Morak M, Renkonen-Sinisalo L, Frayling IM, Plazzer JP, Pylvanainen K, Sampson JR, Capella G, Mecklin JP, Moslein G, Vos Tot Nederveen Cappel WH (2017). Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. Gut 66:464–472
Moller P, Seppala T, Bernstein I, Holinski-Feder E, Sala P, Evans DG, Lindblom A, Macrae F, Blanco I, Sijmons R, Jeffries J, Vasen H, Burn J, Nakken S, Hovig E, Rodland EA, de Tharmaratnam K, Hill J, Wijnen J, Jenkins M, Green K, Lalloo F, Sunde L, Mints M, Bertario L, Pineda M, Navarro M, Morak M, Renkonen-Sinisalo L, Frayling IM, Plazzer JP, Pylvanainen K, Genuardi M, Mecklin JP, Moslein G, Sampson JR, Capella G, Vos Tot Nederveen Cappel WH (2017) Incidence of and survival after subsequent cancers in carriers of pathogenic MMR variants with previous cancer: a report from the prospective Lynch syndrome database. Gut 66:1657–1664
Llosa NJ, Cruise M, Tam A, Wicks EC, Hechenbleikner EM, Taube JM, Blosser RL, Fan H, Wang H, Luber BS, Zhang M, Papadopoulos N, Kinzler KW, Vogelstein B, Sears CL, Anders RA, Pardoll DM, Housseau F (2015) The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov 5:43–51
Sweis RF, Luke JJ (2017) Mechanistic and pharmacologic insights on immune checkpoint inhibitors. Pharmacol Res 120:1–9
Phan GQ, Yang JC, Sherry RM, Hwu P, Topalian SL, Schwartzentruber DJ, Restifo NP, Haworth LR, Seipp CA, Freezer LJ, Morton KE, Mavroukakis SA, Duray PH, Steinberg SM, Allison JP, Davis TA, Rosenberg SA (2003) Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc Natl Acad Sci USA 100:8372–8377
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, Biedrzycki B, Donehower RC, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Duffy SM, Goldberg RM, de la Chapelle A, Koshiji M, Bhaijee F, Huebner T, Hruban RH, Wood LD, Cuka N, Pardoll DM, Papadopoulos N, Kinzler KW, Zhou S, Cornish TC, Taube JM, Anders RA, Eshleman JR, Vogelstein B, Diaz LA, (2015) PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 372:2509–2520
Sloan EA, Ring KL, Willis BC, Modesitt SC, Mills AM (2017) PD-L1 expression in mismatch repair-deficient endometrial carcinomas, incuding Lynch syndrome-associated and MLH1 promoter hypermethylated tumors. Am J Surg Pathol 41:326–333
Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French AJ, Goldberg RM, Hamilton SR, Laurent-Puig P, Gryfe R, Shepherd LE, Tu D, Redston M, Gallinger S (2003) Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 349:247–257
Bertagnolli MM, Niedzwiecki D, Compton CC, Hahn HP, Hall M, Damas B, Jewell SD, Mayer RJ, Goldberg RM, Saltz LB, Warren RS, Redston M (2009) Microsatellite instability predicts improved response to adjuvant therapy with irinotecan, fluorouracil, and leucovorin in stage III colon cancer: Cancer and Leukemia Group Protocol 89803. J Clin Oncol 27:1814–1821
Boland CR (2016) Recent discoveries in the molecular genetics of Lynch syndrome. Fam Cancer 15:395–403
Schwitalle Y, Kloor M, Eiermann S, Linnebacher M, Kienle P, Knaebel HP, Taraverdian M, Benner A, von Knebel Doeberitz M (2008) Immune response against frameshift-induced neopeptides in HNPCC patients and healthy HNPCC mutation carriers. Gastroenterology 134:988–997
Reuschenbach M, Kloor M, Morak M, Wentzensen N, Germann A, Garbe Y, Tariverdian M, Findelsen P, Neumaier M, Holinski-Feder E, von Knebel-Doeberitz M (2010) Serum antibodies against frameshift peptides in microsatellite unstable colorectal cancer patients with Lynch syndrome. Fam Cancer 9:173–179
Bauer K, Michel S, Reuschenbach M, Nelius N, von Knebel Doeberitz M, Kloor M (2011) Dendritic cell and macrophage infiltration in microsatellite-unstable and microsatellite-stable colorectal cancer. Fam Cancer 10:557–565
de Miranda NF, Goudkade D, Jordanova ES, Tops CM, Hes FJ, Vasen HF, van Wezel T, Morreau H (2012) Infiltration of Lynch syndrome colorectal cancers by activated immune cells associates with early staging of the primary tumor and absence of lymph node metastases. Clin Cancer Res 18:1237–1245
von Knebel Doeberitz M, Kloor M (2013) Towards a vaccine to prevent cancer in Lynch syndrome patients. Fam Cancer 12:307–312
Westdorp H, Fennemann FL, Weren RD, Bisseling TM, Ligtenberg MJ, Figdor CG, Schreibelt G, Hoogerbrugge N, Wimmers F, de Vries IJ (2016) Opportunities for immunotherapy in microsatellite instable colorectal cancer. Cancer Immunol Immunother 65:1249–1259
Lee J-M, Ledermann JA, Kohn EC (2014) PARP inhibitors for BRCA1/2 mutation-associated and BRCA-like malignancies. Ann Oncol 25:32–40
Link JT, Overman MJ (2016) Immunotherapy progress in mismatch repair-deficient colorectal cancer and future therapeutic challenges. Cancer J 22:190–195
Ginsburg GS, Willard HF (2009) Genomic and personalized medicine: foundations and applications. Transl Res 154:277–287
Kravochuck SE, Kalady MF, Burke CA, Heald B, Church JM (2014) Defining HNPCC and Lynch syndrome: what’s in a name? Gut 63:1525–1526
Fusaro RM, Lemon SJ, Lynch HT (1996) The Muir-Torre syndrome: a variant of hereditary nonpolyposis colorectal cancer syndrome. J Tumor Marker Oncol 11:19–31
Shiovitz S, Copeland WK, Passarelli MN, Burnett-Hartman AN, Grady WM, Potter JD, Gallinger S, Buchanan DD, Rosty C, Win AK, Jenkins M, Thibodeau SN, Haile R, Baron JA, Marchand LL, Newcomb PA, Lindor NM, Colon Cancer Family Registry (2014) Characterisation of familial colorectal cancer type X, Lynch syndrome, and non-familial colorectal cancer. Br J Cancer 111:598–602
MedicineNet (2017) Familial colorectal cancer. Available at: http://www.medicinenet.com/script/main/art.asp?articlekey=38753. Accessed 9 Oct 2017
Westdorp H, Kolders S, Hoogerbrugge N, de Vries IJM, Jongmans MCJ, Schreibelt G (2017) Immunotherapy holds the key to cancer treatment and prevention in constitutional mismatch repair deficiency (CMMRD) syndrome. Cancer Lett 403:159–164
Acknowledgements
We thank Peter Silberstein, M.D., for technical assistance.
Funding
This work was supported by revenue from Nebraska’s excise tax on cigarettes awarded to Creighton University by the Nebraska Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the State of Nebraska or the Nebraska Department of Health and Human Services. Funding was also received from the Liz’s Legacy fund through Kicks for a Cure. Dr. Henry Lynch’s work is partially funded through the Charles F. and Mary C. Heider Chair in Cancer Research, which he holds at Creighton University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lynch, H.T., Lanspa, S., Shaw, T. et al. Phenotypic and genotypic heterogeneity of Lynch syndrome: a complex diagnostic challenge. Familial Cancer 17, 403–414 (2018). https://doi.org/10.1007/s10689-017-0053-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-017-0053-3