Abstract
The rearranged during transfection (RET) gene is a proto-oncogene; active mutations frequently occur in medullary thyroid carcinoma (MTC). This study investigated the spectrum of germline RET mutations and clinical features in Chinese hereditary MTC patients. A total of 53 family members from 11 different hereditary MTC families were recruited for detection of RET exon 8, 10, 11, 13, 14, 15, and 16 mutations, in genomic DNA from peripheral blood leucocytes using polymerase chain reaction (PCR) and direct DNA sequencing. Of the 53 participants, eight different germline RET mutations were detected in 37 individuals. These RET mutations were distributed in exons 10, 11, 13, and 16. The most frequent RET mutation was localized at exon 11 codon 634 (67.6 %; 25/37) and the most prevalent mutation was C634R (37.8 %; 14/37). The most frequent phenotype was multiple endocrine neoplasia type 2A (MEN2A). The incidences of MTC, pheochromocytoma, and hyperparathyroidism in the MEN2A patients were 100, 36.4 and 18.2 %, respectively. The phenotype of families with Y606C or L790F mutation was categorized as familial medullary thyroid carcinoma. Moreover, one proband was identified with multiple endocrine neoplasia type 2B and carried a de novo mutation of M918T. Two families with C618S/Y mutation were categorized as unclassified multiple endocrine neoplasia type 2. Our results further substantiate that most germline mutations of the RET proto-oncogene were localized at codon 634 in Chinese hereditary MTC patients and carriers. RET mutation at codon 634 was always associated to the phenotype of MEN2A. Screening of RET mutations should be probably limited to exons 10, 11, 13 and 16 initially to be cost-effective in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medullary thyroid carcinoma (MTC) is a relatively rare malignant thyroid tumor, accounting for <10 % of all thyroid cancers. Approximately 25 % of MTC represents inherited disease, while the rest is as a sporadic tumor [1–4]. MTC originates from the parafollicular cells (C cells) and produces the hormone calcitonin. MTC is a consistent feature of multiple endocrine neoplasia type 2A (MEN2A) and multiple endocrine neoplasia type 2B (MEN2B), and familial medullary thyroid carcinoma (FMTC), all of which are inherited as autosomal dominant traits. MEN2A is a cancer syndrome characterized as MTC, pheochromocytoma (PHEO), and hyperparathyroidism (HPT), while FMTC is a clinical variant of MEN2A with the presence of MTC only. MEN2B is characterized by MTC, PHEO, mucosal neuromas, ganglioneuromatosis of the gut, and a Marfanoid habitus. Hereditary MTC occurring with nearly complete penetrance is multifocal and bilateral, and occurs at an earlier age than sporadic ones. Germline mutations of the RET proto-oncogene were found to be responsible for development of MEN2 syndromes [5, 6]. Afterwards, a large number of cases with inherited MTC have been investigated for RET defects. The RET proto-oncogene is localized at chromosome 10q 11.21 and contains 21 exons to encode a transmemebrane receptor tyrosine kinase protein that is important in transferring cell growth and differentiation signals [7]. The RET receptor is primarily expressed in neural crest and urogenital precursor cells during fetal development. A single activating RET mutation in one allele could be sufficient to cause neoplastic transformation. To date, several genotype–phenotype correlation studies have identified the association between RET mutations and different MEN2 syndrome variants [8–10]. To date, the most common RET germline mutations causing MEN2A and FMTC syndromes affect exons 8, 10, 11, 13, 14 and 15 of RET, while a single germline RET mutation in exon 16 has been found in more than 95 % of MEN2B cases [10]. Thus, a genetic test for RET germline mutations is now available for screening and early detection of MTC. In many countries, such a test is suggested for all patients with a family medical history of MTC or MEN2.
Whereas current RET mutation data are primarily based on observations in Caucasian populations, studies are rare for other ethnicities, such as Chinese. Collection of such data is very important since the genetic background of Chinese populations is different and the natural course of various RET mutation carriers may also be different [11]. Thus, in this study, we performed a molecular analysis of MTC patients and their family members to collect such information that could be useful for early detection and screening of Chinese MTC patients by selected to assess RET mutations at exons 8, 10, 11, 13, 14, 15, and 16. Our selection of these mutation spots in this study was also cost-effectively considered although we will miss RET mutations in other spots.
Subjects and methods
Subjects
A consecutive series of 74 MTC patients were recruited from the Department of Head and Neck, Cancer Hospital (Beijing, China) between January 2011 and September 2014. MTC was diagnosed histologically according to previously published criteria [12]. Germline mutations of the RET proto-oncogene were assessed in all MTC patients. If germline mutations of RET were detected, the patient’s relatives were also invited for RET screening. The control group consisted of 60 healthy people without a history of thyroid cancer. Genetic counseling was provided for all participants. This study was approved by the Human Research Ethics Committee of the Cancer Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences and an informed consent form was obtained from all participants.
Methods
Genomic DNA was extracted from peripheral blood leucocytes and then subjected to PCR and detection of RET mutations. The primers of RET exon 8, 10, 11, 13, 14, 15, and 16 are shown in Table 1. PCR was performed in 40-µL mixtures of 100–200 ng of genomic DNA, 0.2–0.4 µM of each primer, 1 × PCR buffer with 1–2 mM of Mg2+, and 0.062 U of Taq polymerase (Takara Bio Inc., Dalian, China). The concentrations of Mg2+ (Takara Bio Inc.), dNTPs (Takara Bio Inc.) and template DNA were adjusted specifically for detection of each exon. PCR conditions were set for a pre-heating cycle of 95 °C for 5 min, followed by 35 cycles of 95 °C for 30 s, 58–65 °C for 30 s, and 72 °C for 60 s, and a final extension at 72 °C for 10 min. After that, 5 µL of each PCR product was separated on 1.5 % agarose using gel electrophoresis and a portion of PCR products from each case was sent to DNA sequence for both sense and antisense orientations using ABI 3730XL DNA Analyzer (Applied Biosystems, Foster City, CA, USA). DNA sequence data were analyzed using a mutation surveyor version 4.0 (SoftGenetics, State College, PA, USA) and visual inspection.Student’s t test was used to analyze differences in mean values.
Results
Characteristics of study population
According to clinical and molecular features, 63 out of 74 MTC patients were diagnosed as sporadic MTC and 11 patients as hereditary MTC; thus, we also collected data on 42 relatives of these 11 hereditary MTC patients.
Among all 53 family members of these 11 unrelated pedigrees (including 11 probands and 42 family members), RET mutations were detected in 37 (69.8 %). Among these carriers, only 30 were diagnosed as hereditary MTC; 7 of them were asymptomatic carriers of RET mutations. The mean age at diagnosis in the hereditary MTC patients was significantly higher than that of mutation carriers (34.7 ± 13.8 vs. 11.0 ± 5.7 years, p < 0.05), but lower than that of sporadic ones (34.7 ± 13.8 vs. 44.8 ± 10.9 years, p < 0.01).
RET mutations in the hereditary MTC families
In these 11 hereditary MTC families, there were eight different heterozygote missense germline point mutations identified in RET exons 10, 11, 13, and 16. We did not find any RET mutations in exons 8, 14, and 15. In addition, each of these mutation carriers harbored only a single point mutation in RET. We also did not have any evidence of double mutations or deletion/insertions in RET in this cohort of patients. The RET mutations identified were Y606C(Tyr-Cys), C618Y(Cys-Tyr), C618S(Cys-Ser), C634R(Cys-Arg), C634W(Cys-Trp), C634Y(Cys-Tyr), L790F(Leu-Phe), M918T(Met-Thr). Among mutation carriers, a total of 25/37 (67.6 %) individuals were detected with codon 634 mutations and the most prevalent mutation was C634R (37.8 %; 14/37). Meanwhile, there were no RET mutations detected in the control group.
Clinical characteristics of patients and association between the phenotype and genotype
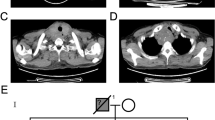
The clinical features and molecular data of these 11 hereditary MTC pedigrees are summarized in Table 2. In brief, 25 familial members from I to VI pedigrees carried a RET proto-oncogene mutation at codon 634. Among them, 22 showed the clinical MEN2A phenotype and had MTC, while 8 (36.4 %) with PHEO and 4 (18.2 %) had HPT. To date, the other three carriers had no obvious clinical symptoms and were diagnosed as carriers of RET proto-oncogene mutation.
Among the 22 MEN2A patients, only one patient (4.5 %) had MTC in combination with PHEO and HPT, and similarly, only one patient (4.5 %) had MTC solely, 20 other patients (91.0 %) had MTC with PHEO or HPT. Among these MTC patients, the mean age at diagnosis was 30.8 ± 9.1 years, 19 (86.4 %) cases were multifocal and 12 (54.5 %) cases had lymph node metastasis at initial diagnosis. Among the eight patients with PHEO, three (37.5 %) were bilateral, and five (62.5 %) were unilateral. Two patients who had bilateral involvement were among the four patients with HPT.
Furthermore, family VII and VIII had RET Y606C and L790F mutations, respectively. Each of these two families had three MTC patients in two generations, and they did not show other endocrine disorders. Based on clinical data and the less rigid definition of FMTC of the American Thyroid Association (ATA) [15], these patients were categorized as FMTC. Although the mutations were different, there is something in common among the patients. The age of all of these MTC patients at diagnosis was over 40 years, and none of them had lymph node metastasis.
In family IX, the proband was a 13-year-old female who had bilateral MTC in combination with evident mucosal neuromas on the lip and tongue, eyelid neuromas, reduced eyesight, and marfanoid habitus. This female was diagnosed histologically with Hirschsprung’s disease at the age of 3 years. There was no evidence of adrenal abnormality. The patient carries the RET M918T germline mutation; however, the same mutation was not detected in her parents. This patient had the very aggressive tumor and had multifocal MTC with extensive lymph node metastasis.
In addition, we also found other types of RET germline mutations that were clearly associated with MEN2. For example, in families X and XI the index cases harbored the codon 618 mutation. In the two MTC patients, there was no evidence of adrenal or parathyroid abnormality. Moreover, their relatives undergoing genetic screening were not found to have any RET mutations. Therefore, these two families were categorized as unclassified MEN2. The two patients had multifocal MTC with lymph node metastasis at initial diagnosis.
Discussion
In this study, we analyzed RET mutations in 116 participants (74 MTC patients and 42 family members) and observed 37 individuals from 11 families with eight different RET mutations. These 37 RET mutations were distributed in RET exons 10, 11, 13, and 16. Most frequent RET mutations were at codon 634 in MTC patients and the most prevalent mutation was C634R among the carriers. The mutation at codon 634 was always associated to MEN2A phenotype. Moreover, one proband identified with MEN2B syndrome showed the characteristic phenotype and de novo mutation of M918T with very aggressive tumor. The phenotype of families with RET L790F or Y606C mutation was categorized as FMTC. The family with RET C618S/Y was categorized as unclassified MEN2. Hereditary MTC patients were diagnosed at an earlier age than the sporadic ones. These data clearly indicate that RET mutations, especially at codon 634, are useful in screening and early detection of Chinese hereditary MTC.
Currently data on the distribution and rate of RET mutations are very limited in the Chinese population. A previous cross-sectional study that evaluated 119 family members from MEN2A pedigrees showed that RET mutations were restricted to codon 634 in Chinese families with MEN2A [13]. In our current study, the most common clinical subtype of MEN2 is MEN2A. Indeed, RET mutations in all of MEN2A patients were localized at codon 634, which is consistent with the previous study. The most frequent substitution at the codon 634 is to replace a cysteine with arginine change, followed by Cys634Tyr and Cys634Trp. This phenomenon was similar to studies on RET mutations in other races, such as Caucasian populations where Cys634Arg is the most prevalent [14, 15]. The typical age of onset of MEN2A is in the third or fourth decade of life [12], the risk of developing unilateral or bilateral PHEO is as high as 57, and 15–30 % of RET mutation carriers will develop HPT [16]. In this study, incidence of PHEO and HPT were similar to the previous reports. In addition, according to previous reports, individuals with RET mutation in codon 634 were at high risk of developing PHEO, but not related to any specific base mutation. The development of HPT was closely related to RET mutation in codon 634, but not to in codon 609, 611, 618, 620, 790 or 791 [17, 18]. The findings of this study are in agreement with these reports, i.e., PHEO occurred with RET codon 634 mutation in different genotypes and two patients with HPT carried the C634R or C634W mutation.
Furthermore, FMTC is characterized as a simple MTC without other endocrine neoplasms. MTC in these patients tends to be the least aggressive, with a later age of onset and earlier stage at diagnosis. Genetically, FMTC is most commonly associated with RET mutations in exon 10 codon 618, and 620 or exon 13 codon 768 [10]. In the cohort used for this study, the germline RET mutations affecting codons 606 and 790 were associated with FMTC; the RET Y606C mutation affected six members of family VII. Among them, the index patient and her mother and sister suffered from MTC but they all lacked other endocrine neoplasms. The mean age at diagnosis of these patients was 50 years (range 47–53 years) and the tumors were at early stage without regional lymph node metastasis. To date, RET codon 606 mutation has been rarely reported. The RET Y606C mutation has been reported in only a single patient with MTC and this mutation was not found in any relatives of the patient [19]. Y606C variant was able to lead to an increase in activation of the downstream signaling of RET receptor and thus should be the cause of MTC development [19, 20]. However, although we classified the family as FMTC, persistent follow-up will be needed to evaluate the risk of PHEO in the patients and other family members. In family VIII, the mean age at diagnosis of these patients was 46 years (range 43–50 years) and the tumors were early stage without regional lymph node metastasis. RET codon 790 mutations differs from other common RET mutations, such as exon 10 and 11, as they do not affect the extracellular domain of the protein but, rather, the intracellular tyrosine kinase 1 domain, mutation of which increases the transforming activity, possibly by altering the substrate specificity or the ATP-binding capacity of RET to modify the kinase activity [21]. RET mutations in codon 790 and 791 have been described in 5 of 181 German MEN2A/FMTC families as rare spots leading to hereditary MTC and PHEO [21]. After the analysis of the phenotypic expression, Fitze [22] suggested that RET codon 790/791 mutations might be associated with low penetrance and might generate a mild thyroid disease phenotype compared to that of the more common MEN2 mutations.
Approximately 95 % of MEN2B cases were associated with RET exon 16 codon 918 (M918T) mutation that affects the intracellular domain of RET protein [10]. We found this mutation in a 13-year-old female from family IX, and this young patient had already been characterized as MEN2B and had the very aggressive tumor, but the same mutation was not detected in her parents, suggesting that this mutation occurred de novo. Indeed, approximately 75 % of MEN2B patients have de novo RET mutations and 95 % of them have germline M918T mutation [23]. Previously, Zhou et al. [13] also reported five Chinese probands identified in MEN2B and all of them showed de novo mutation of M918T.
In addition, our current data showed a RET mutation in exon 10 codon 618 affecting cysteine-rich extracellular domain. RET codon 618 mutation is usually described in the literature as the cause of MEN2A [24], but in the Netherlands, the highest rate of RET mutation in FMTC has been related to codon 618 [25]. The penetrance of PHEO and HPT to RET codon 618 mutation carriers is significantly lower than RET codon 634 mutations carriers [24]. However, in family X and XI, the only two index patients with MTC showed to have RET codon 618 mutation but without other mutations. Two daughters of the proband in family X and the father of the proband in family XI did not carry the same mutation. The small number in the current study does not allow us to draw a conclusion on phenotype/genotype correlations. But our present study showed that clinical characteristics of patients with RET codon 618 mutation did not show any “less aggressiveness”, although a previous study demonstrated that MTC caused by RET codon 618 mutation is generally less aggressive than RET codon 634 mutation [12].
Clinically, to date, surgery is still the curable therapy for MTC patients; thus, genetic testing could diagnose the disease early for thyroidectomy to prevent or cure MTC. In our current study, a total of 6 asymptomatic carriers were detected by genetic screening. Combined with clinical examination, three were suspected to be MTC (two for positive neck ultrasound and one for increased calcitonin), and they were all confirmed by postoperative pathology. However, three other asymptomatic carriers did not accept further clinical examination, because their parents worried that the result might bring a spiritual and psychological burden to the families. As a result, prophylactic thyroidectomy was not carried out during the period of our study. In China, prophylactic surgery still faces difficulties.
Although the exome sequencing of RET is feasible technically, it may not be financially cost-effective. Based on our current data and other previous studies, in Chinese HMTC families, the germline mutation spectrum of the RET proto-oncogene is limited. Screening of RET mutations should be probably limited to exons 10, 11, 13 and 16 initially and could be cost-effective, and then extended to the other hotspot exons if necessary, such as 8 and 15 exons and beyond.
Although MEN2 is an autosomal dominant hereditary syndrome with low prevalence, China is a country of diversity with a large population, and thus the number of MEN2 patients may be relatively higher than other countries [13]. However, reports for the genetic characteristics of RET in Chinese MEN2 patients are rare. This study is an example for comprehensive survey of patients with MTC in China. Further studies using a larger sample size are needed to comprehensively identify RET mutations in MTC patients and their families. More importantly, we have to plan to pursue the goal of prophylactic surgery for MTC patients and RET mutation carriers in the near future with the launching of genetic counseling and health education in China.
References
Pelizzo MR, Boschin IM, Bernante P et al (2007) Natural history, diagnosis, treatment and outcome of medullary thyroid cancer: 37 years experience on 157 patients. Eur J Surg Oncol 33:493–497
Baloch ZW, LiVolsi VA (2001) Prognostic factors in well-differentiated follicular-derived carcinoma and medullary thyroid carcinoma. Thyroid 11:637–645
Paszko Z, Sromek M, Czetwertynska M et al (2007) The occurrence and the type of germline mutations in the RET gene in patients with medullary thyroid carcinoma and their unaffected kindred’s from central Poland. Cancer Investig 25:742–749
Bergant D, Hocevar M, Besic N et al (2006) Hereditary medullary thyroid cancer in Slovenia–genotype–phenotype correlations. Wien Klin Wochenschr 118:411–416
McKusick VA, Amberger JS (1993) The morbid anatomy of the human genome: chromosomal location of mutations causing disease. J Med Genet 30:1–26
McKusick VA, Amberger JS (1994) The morbid anatomy of the human genome: chromosomal location of mutations causing disease (update 1 December 1993). J Med Genet 31:265–279
Elisei R, Romei C, Cosci B et al (2007) RET genetic screening in patients with medullary thyroid cancer and their relatives: experience with 807 individuals at one center. J Clin Endocrinol Metab 92:4725–4729
Mulligan LM, Kwok JB, Healey CS et al (1993) Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 363:458–460
Machens A, Gimm O, Hinze R et al (2001) Genotype–phenotype correlations in hereditary medullary thyroid carcinoma: oncological features and biochemical properties. J Clin Endocrinol Metab 86:1104–1109
Eng C, Clayton D, Schuffenecker I et al (1996) The relationship between specific RET proto-oncogene mutations and disease phenotype in multiple endocrine neoplasia type 2. Int RET Mutat Consort Anal JAMA 276:1575–1579
Chang CF, Yang WS, Su YN et al (2009) Mutational spectrum of multiple endocrine neoplasia type 2 and sporadic medullary thyroid carcinoma in taiwan. J Formos Med Assoc 108:402–408
American Thyroid Association Guidelines Task F, Kloos RT, Eng C et al (2009) Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 19:565–612
Zhou Y, Zhao Y, Cui B et al (2007) RET proto-oncogene mutations are restricted to codons 634 and 918 in mainland Chinese families with MEN2A and MEN2B. Clin Endocrinol (Oxf) 67:570–576
Mulligan LM, Eng C, Healey CS et al (1994) Specific mutations of the RET proto-oncogene are related to disease phenotype in MEN 2A and FMTC. Nat Genet 6:70–74
Punales MK, Graf H, Gross JL et al (2003) RET codon 634 mutations in multiple endocrine neoplasia type 2: variable clinical features and clinical outcome. J Clin Endocrinol Metab 88:2644–2649
Brandi ML, Gagel RF, Angeli A et al (2001) Guidelines for diagnosis and therapy of MEN type 1 and type 2. J Clin Endocrinol Metab 86:5658–5671
Karga HJ, Karayianni MK, Linos DA et al (1998) Germ line mutation analysis in families with multiple endocrine neoplasia type 2A or familial medullary thyroid carcinoma. Eur J Endocrinol 139:410–415
Magalhaes PKR, Antonini SRR, de Paula FJA et al (2011) Primary hyperparathyroidism as the first clinical manifestation of multiple endocrine neoplasia type 2A in a 5-year-old child. Thyroid 21:547–550
Ahmed SA, Snow-Bailey K, Highsmith WE et al (2005) Nine novel germline gene variants in the RET proto-oncogene identified in twelve unrelated cases. J Mol Diagn 7:283–288
Ercolino T, Lombardi A, Becherini L et al (2008) The Y606C RET mutation causes a receptor gain of function. Clin Endocrinol (Oxf) 69:253–258
Berndt I, Reuter M, Saller B et al (1998) A new hot spot for mutations in the ret protooncogene causing familial medullary thyroid carcinoma and multiple endocrine neoplasia type 2A. J Clin Endocrinol Metab 83:770–774
Fitze G, Schierz M, Bredow J et al (2002) Various penetrance of familial medullary thyroid carcinoma in patients with RET protooncogene codon 790/791 germline mutations. Ann Surg 236:570–575
American Thyroid Association Guidelines Task F, Wells SA, Asa SL et al (2015) Revised american thyroid association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567–610
Quayle FJ, Fialkowski EA, Benveniste R et al (2007) Pheochromocytoma penetrance varies by RET mutation in MEN 2A. Surgery 142:800–805
Landsvater RM, Jansen RP, Hofstra RM et al (1996) Mutation analysis of the RET proto-oncogene in Dutch families with MEN 2A, MEN 2B and FMTC: two novel mutations and one de novo mutation for MEN 2A. Hum Genet 97:11–14
Acknowledgments
This research was supported by Grants from Research Fund for the Doctoral Program of Higher Education of China (20101106110016) and Graduate Innovation Foundation of Peking Union Medical College (20101002016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest in this work.
Ethical approval
Ethical approval was given by the Human Research Ethics Committee of the Cancer Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, with the following Approval Number: 11-05/440.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wang, J., Zhang, B., Liu, W. et al. Screening of RET gene mutations in Chinese patients with medullary thyroid carcinoma and their relatives. Familial Cancer 15, 99–104 (2016). https://doi.org/10.1007/s10689-015-9828-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-015-9828-6