Abstract
Background The associations between dietary indices and mortality have not been evaluated in populations from the Middle East, which have different dietary patterns compared to the US and Europe. In this study, we evaluated the association between six dietary indices and mortality in the Golestan Cohort Study (GCS) in Iran, which is the largest prospective study in the Middle East with 50,045 participants. Methods The six dietary indices, namely the Healthy Eating Index (HEI-2015), Alternative Healthy Eating Index (AHEI-2010), Alternative Mediterranean Diet (AMED), Dietary Approach to Stop Hypertension created by Fung (DASH-Fung) and Mellen (DASH-Mellen), and the World Cancer Research Fund (WCRF/AICR) index, were applied to data from a food frequency questionnaire, computed and divided into quintiles. Adjusted Cox models were used to estimate hazards ratio (HR) and 95% confidence intervals (CI) for overall and cause-specific mortality, using the lowest quintile as a reference group. Results Among 42,373 participants included in the current analyses, 4424 subjects died during 10.6 years of follow-up. Participants with the highest quintile dietary scores, compared with the lowest quintile dietary scores, had significantly decreased overall mortality in the AHEI-2010, AMED, DASH-Fung, and WCRF/AICR indices (HR 0.88, 95% CI = 0.80–0.97; 0.80, 0.70–0.91; 0.77, 0.70–0.86; and 0.79, 0.70–0.90, respectively). A reduced cardiovascular mortality was found for high AHEI-2010 and DASH-Fung scores (17% and 23%, respectively), and a reduced cancer mortality for high HEI-2015, AMED, and DASH-Fung scores (21, 37 and 25%, respectively). Conclusion Various indices of dietary quality are inversely associated with overall mortality, and selectively with cancer and cardiovascular mortality in the GCS, which contribute to the generalizability and validity of dietary guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association of specific food groups or food items and mortality has been reported in various populations [1,2,3,4]. Further, the complexity of diet and the correlation between food items which are consumed justify the use of dietary score to characterize potentially beneficial and harmful food patterns [5].
Several dietary scores have been defined to evaluate dietary quality. Commonly used indices include: the Healthy Eating Index (HEI), which was created and subsequently updated to evaluate how diets follow federal dietary guidance in the United States [6, 7]; the Alternative Healthy Eating Index (AHEI), which was developed by Harvard University to decrease the risk of chronic diseases based on previous findings [8, 9]; the Alternative Mediterranean Diet (AMED), which is a model of eating based on Mediterranean Diet, the traditional foods and drinks of the countries surrounding the Mediterranean Sea, and has been proposed as one of the healthiest dietary patterns [10]; the Dietary Approach to Stop Hypertension (DASH), which was developed to prevent hypertension [11]; and The World Cancer Research Fund and the American Institute for Cancer Research (WCRF/AICR) index, which was proposed to prevent cancer on the basis of the most comprehensive scientific findings [12]. Multiple DASH scores have been created, the most commonly used of which are those based on food groups developed by Fung et al. (DASH-Fung) [13] and those based on nutrients developed by (DASH-Mellen) Mellen et al. [11].
The HEI, AHEI, AMED, DASH, and WCRF indices are frequently reported to be associated with a reduced risk of chronic diseases, such as cardiovascular diseases (CVD) and cancer, and overall mortality [14, 15]. However, the association of dietary indices has not been widely evaluated in the populations from the Middle East which have different dietary patterns from those from North America and Europe where the scores were originally developed. In this study, we use these six dietary indices (HEI-2015, AHEI-2010, AMED, DASH-Fung, DASH-Mellen, and WCRF/AICR) to evaluate the association between diet quality and mortality in the Golestan Cohort Study, the largest prospective population study of chronic diseases in the Middle East. We also compare the scores with each other to see the magnitude and significance of the associations in an Iranian population. To enable a rigorous comparison, we used the same scores as the Dietary Patterns Methods Project, which was created to conduct standard analyses of the association between dietary indices and mortality in three large prospective studies in the United States [16].
Materials and methods
Study population and design
The Golestan Cohort study enrolled 50,045 participants aged 40–75 years in 2004–2008 in Golestan Province, located in the northeastern part of Iran. In urban areas, the participants were selected randomly by systematic clustering using household number. In rural areas, all eligible residents were invited to participate. Participation rates were between 50 and 84% in urban and rural areas [17]. About 57% of the population were women, and 81% were rural. The baseline questionnaire on demographic and lifestyle variables and the Food Frequency Questionnaire (FFQ) were completed by trained interviewers. The study protocol has been described before [18] and was approved by the Institutional Review Boards of the U.S. National Cancer Institute (NCI), the International Agency for Research on Cancer (IARC), and the Digestive Disease Research Institute of the Tehran University of Medical Sciences (DDRI). All participants provided a written informed consent at baseline.
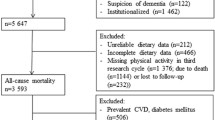
We excluded participants who had ≥ 30 missing responses on the baseline FFQ (n = 872); participants whose energy intake was more than twice the interquartile range above the 75th percentile (3690 kcal/day for women and 4145 kcal/day for men) or less than twice the interquartile range below the 25th percentile of energy intake (300 kcal/day for women and 525 kcal/day for men) (n = 599); and participants with a self-reported history of cancer, heart disease or diabetes at baseline (n = 6201). The final cohort included 42,373 participants (18,272 men and 24,101 women) (Supplemental Fig. 1). We also examined excluding the participants within the lowest and highest 1% of the cohort distribution of the ratio of reported total energy intake to energy requirements, which has been used by Romaguera et al. [14] for WCRF score, and the results were largely identical.
Outcome measures
The participants were followed up annually by phone; fewer than 1% were lost to follow-up during the study period [18]. Deaths were reported by health workers, family or friends. Any report was followed by a visit in order to collect all medical reports and undertake a verbal autopsy, the validity of which has been previously confirmed [19]. All medical records, pathology reports, radiographs, and hospital documents were used to identify the cause of death, based on the International Classification of Disease. Two internists reviewed the documents, and in case of a disagreement on the cause of death, a third expert internist made the final diagnosis. If a final diagnosis could not be determined due to insufficient documents, it was classified as “unknown” [2]. In this analysis, we classified cause-specific mortality as death from CVD, including ischemic heart disease (ICD-10 codes I20–I25), stroke (ICD-10 codes I60–I69), and other disease of circulatory system (ICD-10 codes I00–I99); and cancer (ICD-10 codes C00–C97, excluding C44 and C46.0). Follow-up time was calculated from the date of the completion of the FFQ until death, loss to follow up, or June 30, 2017, whichever came first.
Exposure measures
A 116-item FFQ was developed for this population inquiring about the frequency of consumption of a typical portion size of each food item based on daily, weekly, monthly or yearly intake. These were converted to provide estimates of mean daily intakes. The reproducibility and validity of the questionnaire was assessed using four repetitions of the FFQ and twelve 24-h dietary recalls during one year [20]. Pearson’s correlation coefficients were 0.75 for total energy, 0.75 for carbohydrates, 0.76 for proteins and 0.65 for fat based on the mean of the four FFQs and the mean of the twelve 24-h diet recalls [20]. To calculate energy and nutrient intake, we multiplied the daily intake (grams/day) by the energy or nutrient content of each food item according to the Iranian food composition tables [21] or the United State Department of Agriculture reports (release 23), if the food items were not available in the Iranian tables [22].
To create components of the HEI-2015 and AHEI-2010 scores, we converted the daily intakes from grams to cup and ounce equivalents using the Food Patterns Equivalents Database (FPED) 2013–2014 [23]. The FPED units are ounce and cup equivalents and can be converted to standard units as follows: 1 oz = 28.35 g and 1 cup = 225 ml. For fruits and vegetables, we used an extensive list of one cup equivalent weights for fruits and vegetables in the FPED [23]. For example, for canned fruit in light syrup, 65% fruit was assumed. For grain products such as bread, dough and cake, made with flour, each 16 g of flour present in a food was used as the basis for defining a 1-oz grain equivalent, the rationale being that one standard slice of bread has been defined as equal to 1-oz grain equivalent, which will contain 16 g of flour [23]. For intact grains such as rice and pasta, cooked grains were converted to the uncooked forms with conversion factors 0.36 and 0.37, respectively [24], and 1-oz equivalent of grains was defined as 28.35 g [23]. In the FFQ, multi-ingredient foods such as pizza were not asked, so we did not have to disaggregate the foods. However, protein foods were further disaggregated to lean fraction and fat as follows: meat and poultry were disaggregated to lean meat and solid fat fractions; and seafood and nuts were disaggregated to lean protein and oil fractions. Similarly, dairy foods were further disaggregated to a low fat dairy fraction, similar to skim milk, and a solid fat fraction [23].
Food items were assigned to food groups according to Supplemental Table 1. The dietary scores were calculated as follows and were categorized into quintiles. Note that the number of participants were not always equal in each quintile.
The HEI-2015 The HEI-2015 includes 13 components for a total of 100 points based on the 2015 Dietary Guidelines for Americans [7], including 9 adequacy components: total fruit (include fruit juice); whole fruit; total vegetables; greens and beans (includes dark green vegetables and legumes); whole grains; dairy; total protein foods [includes meat and poultry (lean fraction), eggs, seafood, nuts, seeds, soy and legumes]; seafood and plant proteins [includes seafood, nuts, seeds, soy and legumes]; fatty acids [ratio of polyunsaturated fatty acids (PUFAs) and monounsaturated fatty acids (MUFAs) to saturated fatty acids (SFAs)] (Supplemental Table 2); and four moderation components: SFAs, refined grains, sodium, and added sugars (Supplemental Table 2). The components were calculated per 1000 kcal/d (energy density model).
The AHEI-2010 The AHEI-2010 includes 11 components for a total of 110 points [5, 8, 9]. The AHEI-2010 includes fruits, vegetables, whole grains, red and processed meat, nuts and legumes, trans fats, omega-3 fatty acids, PUFAs, sugary sweetened beverages (SSB) and fruit juice, sodium, and alcohol (Supplementary Table 2). The AHEI-2010 is similar to HEI-2015, however, potatoes are not included in the vegetable group in this score. Also, the AHEI-2010 uses an absolute intake method instead of a nutrient density method [8]. SSBs were defined as any beverages containing a caloric sweetener, even if added after purchase [25]. Therefore, we included sweet tea if it contained approximately one half (or more) of the sugar and calories of regular sodas [25].
The AMED The AMED includes nine components for a total of nine points, based on the Mediterranean diet [26]: all vegetables (excluding potatoes), all fruits (including juice), nuts, legumes, fish, whole grains, MUFA to SFA ratio, red and processed meat, and alcohol. We applied one point where reported red and processed meat consumption was less than the sex-specific median. For other components, intakes above the sex-specific median of the study subjects received one point. All other intakes received 0 points (Supplementary Table 2).
The DASH-Fung score The DASH score created by Fung includes eight components for a total of 40 points: seven food groups and one nutrient [13]. Scores are based on sex-specific quintiles in the population. The highest quintile of intake for fruits, vegetables, low-fat dairy, whole grains, nuts and legumes each received five points, and the highest quintile of intake for red and processed meat, SSBs, and sodium each received one point (Supplementary Table 2).
The DASH-Mellen score The DASH score created by Mellen [11] includes nine components, all nutrients, for a total of 45 points. The highest quintile of intake for protein, fiber, magnesium, calcium, and potassium each received five points, and the highest quintile of intake for cholesterol, total fat, saturated fat, and sodium each received one point. The total scores were created by summing all points [11] (Supplementary Table 2). We created scores based on quintiles in the Iranian population, because when we used the cut-points based on the American population, the categorization of participants was not appropriate. For example, 88, 85, 89, 90, and 98% of the participants in this study had a score of 0 for protein, calcium, potassium, saturated fat, and sodium, respectively. For example, 98% of the participants consumed more than 1286 mg/1000 kcal of sodium.
The WCRF/AICR score The WCRF/AICR score includes seven dietary components: energy dense foods which cause weight gain [27], fruits and vegetables, red and processed meat, alcohol, sugary drinks, fiber, and sodium; plus nondietary components associated with cancer risk including physical activity, body fatness, and breastfeeding [14]. However, we only calculated the dietary components in this study, to allow for comparability with the other diet-only scores. Energy density was calculated as energy from all solid and semi-solid foods divided by the weights (g) of these foods. Drinks (including water, tea, green tea, juice, soft drinks, alcoholic drinks and milk) were not included in the calculation of energy density [27]. For each component, participants who met the official recommendation received one point, those who met an intermediate recommendation received one-half of a point, and those who met neither recommendation received zero points [14] (Supplementary Table 2).
Alcohol was asked on the demographic baseline questionnaire. Since alcohol intake is not common in this population (4%), all participants received a zero for it in each dietary score. Also, no item in the FFQ was a whole grain, because they are not consumed by this population, so all respondents received a zero for whole grains. We did not modify the scores and did not delete these components, so that we could compare the scores from this population with others.
Covariables were extracted from the baseline questionnaire, which contained questions about demographics, wealth, physical activity at work (irregular or regular; intense or non-intense), and self-reported history of diseases. Ever users of opium or tobacco were defined as those who had used opium or tobacco at least once a week for more than 6 months. Ever tobacco users were also categorized into former and current users [18]. Wealth scores were calculated based on household appliances, vehicles, and other variables associated with wealth, using multiples correspondence analyses [28]. The tertiles of this composite score were used to create low, medium, and high wealth status. Height and weight were measured by trained staff at baseline and then entered into the questionnaire by the staff. We calculated body mass index (BMI) based on weight and height using the formula, weight (kg)/height square (m2). This BMI was then used in statistical analysis as a covariable.
Statistical analysis
Descriptive values of variables were expressed as means ± SD and percentages. The correlations between dietary scores were determined using the Spearman test. Multivariable Cox proportional hazards regression models were used to model the hazard ratios of overall, cardiovascular and cancer mortality for each dietary index. Age (years) was used as the underlying time metric. Multivariable models were adjusted for age (years, continuous), sex, body mass index (BMI) (< 18.5, 18.5 to < 25, 25 to < 30, ≥ 30 kg/m2), formal education (yes, no), place of residence (rural, urban), ethnicity (Turkmen, non-Turkmen), smoking status (never, former, current), opium use (never, ever), physical activity (irregular non-intense, regular non-intense, irregular or regular intense) [29], wealth score (tertile) [30], marital status (married, other), self-reported history of hypertension (yes, no), and total energy intake (kcal/d). We replaced missing covariables with median values, which included 8 participants for history of hypertension and 5 participants for BMI. The substitution of continuous BMI for categorical BMI did not produce meaningfully different results regarding the confounding effect of BMI on the dietary score estimates. In an additional analysis, we took BMI and hypertension out of the models, because they could be considered as mediators.
Potential interaction was assessed for age, gender, smoking status, and BMI (continuous) using the likelihood ratio test, by multiplying each dietary score by each potential effect modifier.
In a sensitivity analysis, participants who were followed less than 2 years were excluded to address potential reverse causality.
All statistical analyses were performed with STATA software (version 14, STATA Corp, College Station, TX, USA). Reported P values are two-sided. All P values < 0.05 were considered to indicate statistical significance.
Results
Of the 42,373 participants included in this study, 4424 were reported to have died during a median (interquartile range) follow-up of 10.6 (9.7 to 11.4) years, including 1598 deaths due to cardiovascular diseases, 976 deaths due to cancer, 1194 deaths due to other causes such as trauma, and 656 due to unknown causes of death.
The median dietary index scores in this population, in comparison with the total possible scores, were as follows: the HEI-2015 = 33 of 100; the AHEI-2010 = 37 of 110; the AMED = 3 of 9; the DASH-Fung = 22 of 40; the DASH-Mellen = 27 of 45; and the WCRF/AICR = 2.5 of 7. The baseline characteristics of the participants are listed in Table 1. The persons with the highest quintile of dietary scores, compared with those with the lowest quintile, for each dietary score had a higher BMI and were more likely to live in urban areas, to be non-Turkmen, to be educated, and to have a higher intake of fruits and vegetables, calcium, and potassium. Other characteristics were not consistent among the six dietary scores; for example, participants with higher scores in the HEI-2015, AHEI-2010, DASH-Fung, and DASH-Mellen were older, while in the AMED and WCRF/AICR, those with the higher scores were younger.
Significant positive correlation was found among the different dietary scores (Table 2). The highest correlation was between the DASH-Fung and AHEI-2010 (r = 0.67), and the lowest correlation was between the AMED and DASH-Mellen (r = 0.18). Four of the five correlations < 0.30 were between DASH-Mellen (nutrient-based) and other dietary scores.
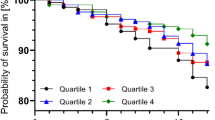
In multivariable models, participants with the highest versus the lowest quintile of dietary scores had a significantly decreased risk of overall mortality in the AHEI-2010 (HRC5 vs. C1 = 0.88, 95% CI = 0.80 to 0.97, P trend = 0.013), AMED (HRC5 vs. C1 = 0.80, 95% CI = 0.70 to 0.91, P trend < 0.0001), DASH-Fung (HRC5 vs. C1 = 0.77, 95% CI = 0.70 to 0.86, P trend < 0.0001), and WCRF/AICR indices (HRC5 vs. C1 = 0.79, 95% CI = 0.70 to 0.90, P trend = 0.0010). However, for the HEI-2015 (HRC5 vs. C1 = 0.92, 95% CI = 0.83 to 1.01, P trend = 0.051), and DASH-Mellen indices (HRC5 vs. C1 = 0.95, 95% CI = 0.86 to 1.05, P trend = 0.26), there was no significant effect on the risk of overall mortality for participants with the highest versus lowest quintile of dietary scores (Table 3).
In multivariable models, participants with the highest compared to the lowest dietary scores had a significantly decreased risk of cardiovascular mortality in the AHEI-2010 (HRC5 vs. C1 = 0.83, 95% CI = 0.70 to 0.97, P trend = 0.080) and DASH-Fung indices (HRC5 vs. C1 = 0.77, 95% CI = 0.64 to 0.92, P trend = 0.0040) (Table 4). However, in the HEI-2015 (HRC5 vs. C1 = 1.00, 95% CI = 0.86 to 1.17, P trend = 0.69), AMED (HRC5 vs. C1 = 0.93, 95% CI = 0.75 to 1.09, P trend = 0.23), DASH-Mellen (HRC5 vs. C1 = 1.11, 95% CI = 0.94 to 1.30, P trend = 0.14) and WCRF/AICR indices (HRC5 vs. C1 = 0.84, 95% CI = 0.68 to 1.04, P trend = 0.080), there was no significant effect on the risk of cardiovascular mortality for participants with the highest versus lowest quintile of dietary scores (Table 4).
In multivariable models, participants with the highest compared to the lowest dietary scores had a significantly decreased risk of cancer mortality in the HEI-2015 (HRC5 vs. C1 = 0.79, 95% CI = 0.64 to 0.98, P trend = 0.058), AMED (HRC5 vs. C1 = 0.63, 95% CI = 0.46 to 0.85, P trend = 0.0010), and DASH-Fung indices (HRC5 vs. C1 = 0.75, 95% CI = 0.60 to 0.93, P trend = 0.0040) (Table 5). However, in the AHEI-2010 (HRC5 vs. C1 = 0.85, 95% CI = 0.68 to 1.05, P trend = 0.10), DASH-Mellen (HRC5 vs. C1 = 0.88, 95% CI = 0.70 to 1.10, P trend = 0.36), and WCRF/AICR indices (HRC5 vs. C1 = 0.87, 95% CI = 0.65 to 1.16, P trend = 0.27), there was no significant effect on the risk of cancer mortality for participants with the highest versus lowest quintile of dietary scores (Table 5).
We tested removing BMI and hypertension from the models because they may be in the causal pathway between diet and mortality, but this change did not alter our results. There were no statistically significant interactions between risk associations and gender, age, smoking status, or BMI for any of the dietary indices.
We also restricted the analysis to the participants with more than 2 years of follow-up, and the results remained largely unchanged (data not shown).
Discussion
This study demonstrates that participants with the highest compared to the lowest dietary scores according to federal US dietary guidelines, the Mediterranean diet, the DASH diet, or WCRF/AICR recommendations had a 12–23% decrease in overall mortality in this largely rural Iranian population. Among the six indices, the DASH-Fung score showed the most consistent relation with overall and cause-specific mortality. To our knowledge this is the first study which compares these six dietary scores in the Middle East, where populations have different cultures and different constraints and excesses in their food systems compared to the US and European populations where the scores were developed.
Reedy et al. [5] compared four indices, the HEI-2010, the AHEI-2010, the AMED (as defined by Fung et al. for an American population), and the DASH-Fung in the NIH-AARP study, and showed that higher scores in all four indices were consistently associated with lower risk of overall, cardiovascular and cancer mortality. Harmon et al. [31]. showed the same results in the Multiethnic Cohort Study. George et al. [32] compared the same four indices in the Women’s Health Initiative’s Observational Study and found similar results except that the AHEI-2010 was not associated with cancer mortality in their study. Our results are consistent with these three studies in the U.S. population for overall mortality; however, for cause-specific mortality, only the AHEI-2010, and DASH-Fung scores were inversely associated with cardiovascular mortality and only the HEI-2015, AMED, and DASH-Fung scores were inversely associated with cancer mortality. Also, the median scores in this study were lower than these three U.S. studies [16]. In a recent study in the Singapore Chinese Health Study, higher scores in the AHEI-2010, AMED and DASH-Fung indices were associated with lower risk of overall and cardiovascular mortality; however, only AMED and DASH-Fung scores were inversely associated with cancer mortality [33], consistent with our results. The WCRF/AICR score has been associated with lower overall and cancer mortality, but not with cardiovascular mortality, in the United States [34]. In this study the WCRF/AICR score was associated only with overall mortality, and not with cardiovascular or cancer mortality. As noted above, we did not include nondietary components of the WCRF/AICR score in this study, which may explain why the WCRF/AICR was not associated with cancer mortality in this study, but this change allowed us to focus on the dietary components of the score.
All the US-based dietary indices include components for fruits, vegetables, and whole grains. However, some components vary among dietary indices. For example, AMED does not have sodium or added sugar or sugary drinks, DASH and WCRF/AICR do not have fatty acids, and only WCRF/AICR has energy density. Also, the AHEI-2010, AMED, and WCRF/AICR indices ignore dairy products. In addition to the components that are included, the weight of each component is important, too. For example, AHEI-2010 assigns more value to fatty acids (three components are related to fat), which may explain why it was significantly associated with CVD, and DASH-Fung assigns an equal value to each component, which may explain the consistency of its associations in this population. Another reason for discrepancies among different indices’ associations could be how the scores are constructed. According to dietary scores using rankings of intake, people who are in the fifth quintile of intake for each food group or nutrient will achieve a high score in that population, even if they do not meet the recommended intake for that food or nutrient. For example, in this study a person who consumed 3400 mg/day of sodium received the highest score in the DASH-Fung index, because they were in the lowest quintile of sodium intake in this population, even though this is a very large intake of sodium, and they received zero points in their HEI-2015 and WCRF/AICR scores. Therefore, differences in how the dietary scores are calculated affect the ability of the scores to predict mortality in different populations.
The DASH score created by Mellen et al., which uses only nutrients, was not associated with risk of mortality in this population; however, we observed consistent and protective results with DASH-Fung scores, which are determined by food groups, and a low correlation between these two scores (0.19). In contrast to this study, Miller et al. [35] compared four DASH scores and found a Spearman correlation coefficient of 0.6 between DASH-Fung and DASH-Mellen in the NIH-AARP study. This discrepancy in correlation results could be due to several reasons. First, minerals often come from different food sources in this population compared to the American population, which could make the DASH-Mellen components not reflect the food groups in the DASH-Fung diet in this population. For example, magnesium intake reflects grain intake rather than nut or soybean intake in Golestan, because grains are an extremely common food in this population. Second, using the United State Department of Agriculture reports database may not be accurate for calculating micronutrients in the Golestan population. Third, DASH-Mellen emphasizes fat and minerals, and although a low saturated fat diet has been reported to be associated with lower risk of mortality [36], the associations of low cholesterol and mineral intake with mortality are equivocal [37,38,39,40,41,42,43,44,45,46]. Fourth, DASH-Mellen was different from the other indices in its relationship with some covariables. For example, in this study all indices’ scores were positively associated with the GCS wealth score except for the DASH-Mellen score, for which a higher score was associated with a lower wealth score. The DASH-Mellen index was also the only one in which a higher score was associated with higher opium use, which is associated with increased risk of mortality in this population [47]. Consistent with our results, high dietary scores in indices based on food groups were consistently associated with lower risk of mortality in the Singapore Chinese Health Study, but the associations were weak and less consistent using a nutrient-based score [33].
Table 1 shows that for HEI-2015, there was a higher intake of red and process meat, which is usually associated with increased total mortality, in C5 than in C1, while in AHEI-2010 the opposite trend was evident. Such differences in the characteristics of participants may, for example, have contributed to why HEI-2015 was not significantly associated with overall mortality in this population, but AHEI-2010 was.
One limitation of this study was using a FFQ to estimate dietary intake, which may result in misclassification and attenuate results; however, in the GCS, four repetitions of the FFQ and twelve 24 h recalls were implemented to validate the FFQ, which should have minimized this problem. Another limitation was collecting data on dietary intake only at baseline, which may not reflect long-term patterns and changes in these exposures over the course of follow-up. Higher dietary scores may be associated with a healthier lifestyle and reflect a higher socioeconomic status, which raises a concern about residual confounding. However, to minimize this concern, we adjusted for many potential confounders in our multivariable models. Reverse casualty could be another possible explanation for inverse association of diet quality with mortality; however, results were similar after excluding the first 2 years of follow-up, thus reducing the opportunity for reverse causation. Opium use is not legal in Golestan; however, opium is widely used and culturally acceptable in Golestan especially among older people, and we previously demonstrated that opium use is accurately reported in this population [48].For the WCRF/AICR score, we only included the dietary components in order to make this score comparable to the other diet-only scores. Our results may not be generalizable to other populations. This study also had several strengths, including the large size of the cohort, its prospective design, long follow-up, and low (< 1%) lost to follow-up rate.
In conclusion, our results demonstrate that in this population, most indices of diet quality based on food groups (The HEI-2015, AHEI-2010, AMED, DASH-Fung, and WCRF/AICR) were inversely associated with overall mortality, similar to the associations reported in Western populations. However, this study suggests that nutrient-based dietary indices (such as DASH-Mellen) designed for Western populations may not be suitable to apply to other populations and should probably first be validated in the populations in which they are intended for use. The objective of this study was not to find a superior index, but rather to clarify the differences between the indices and their influence on evaluating populations with different dietary patterns. Our finding of associations between higher diet quality, defined by these indices, and lower mortality in Golestan, Iran contributes to our understanding of the generalizability and validity of western Dietary Guidelines for other countries. Similar studies in other populations with different dietary patterns are warranted.
References
Micha R, et al. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–24.
Eslamparast T, et al. Nut consumption and total and cause-specific mortality: results from the Golestan Cohort Study. Int J Epidemiol. 2017;46(1):75–85.
Schwingshackl L, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2017;105(6):1462–73.
Ilic M, et al. Association of the consumption of common food groups and beverages with mortality from cancer, ischaemic heart disease and diabetes mellitus in Serbia, 1991–2010: an ecological study. BMJ Open. 2016;6(1):e008742.
Reedy J, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6):881–9.
Kennedy ET, et al. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–8.
National Cancer Institute; National Institutes of Health. Dietary Patterns Methods Project. https://epi.grants.cancer.gov/hei/hei-2015-table1.html.
McCullough ML, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–71.
Chiuve SE, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–18.
Dinu M, et al. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2017;27(1):e21.
Mellen PB, et al. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168(3):308–14.
World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC: AICR; 2007.
Fung TT, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20.
Romaguera D, et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr. 2012;96(1):150–63.
Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780–800.
Liese AD, et al. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393–402.
Sheikh M, et al. Individual and combined effects of environmental risk factors for esophageal cancer based on results from the Golestan Cohort Study. Gastroenterology. 2019. https://doi.org/10.1053/j.gastro.2018.12.024.
Pourshams A, et al. Cohort profile: the Golestan Cohort Study–a prospective study of oesophageal cancer in northern Iran. Int J Epidemiol. 2010;39(1):52–9.
Khademi H, et al. Verbal autopsy: reliability and validity estimates for causes of death in the Golestan Cohort Study in Iran. PLoS ONE. 2010;5(6):e11183.
Malekshah AF, et al. Validity and reliability of a new food frequency questionnaire compared to 24 h recalls and biochemical measurements: pilot phase of Golestan cohort study of esophageal cancer. Eur J Clin Nutr. 2006;60(8):971–7.
Azar M, Sarkisian E. Food composition table of Iran. Tehran: National Nutrition and Food Technology Research Institute of Iran; 1981.
U.S. Department of Agriculture, A.R.S., USDA National Nutrient Database for Standard Reference. Release 23, Nutrient Data Laboratory. http://www.ars.usda.gov/ba/bhnrc/ndl.
Bowman SA, C.J., Friday JE, Lynch KL, and Moshfegh AJ, Food patterns equivalents database 2013–14: Methodology and User Guide. Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture, Beltsville, Maryland. http://www.ars.usda.gov/nea/bhnrc/fsrg.
Bowman SA, M.C., Carlson JL, Clemens JC, Lin B-H, and Moshfegh AJ, Food intakes converted to retail commodities databases: 2003–08: methodology and user guide, A.R.S. U.S. Department of Agriculture, Beltsville, MD, and U.S. Department of Agriculture, Economic Research Service, Editor. 2013: Washington, D.C. p. 48.
Miller PE, et al. Sugar-sweetened beverage consumption in the U.S.: novel assessment methodology. Am J Prev Med. 2013;45(4):416–21.
Fung TT, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–73.
Muller DC, et al. Modifiable causes of premature death in middle-age in Western Europe: results from the EPIC cohort study. BMC Med. 2016;14:87.
Islami F, et al. Socio-economic status and oesophageal cancer: results from a population-based case-control study in a high-risk area. Int J Epidemiol. 2009;38(4):978–88.
Hashemian M, et al. Dietary intake of minerals and risk of esophageal squamous cell carcinoma: results from the Golestan Cohort Study. Am J Clin Nutr. 2015;102(1):102–8.
Etemadi A, et al. Impact of body size and physical activity during adolescence and adult life on overall and cause-specific mortality in a large cohort study from Iran. Eur J Epidemiol. 2014;29(2):95–109.
Harmon BE, et al. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101(3):587–97.
George SM, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616–25.
Neelakantan N, et al. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among Chinese adults. J Nutr. 2018;148(8):1323–32.
Lohse T, et al. Adherence to the cancer prevention recommendations of the World Cancer Research Fund/American Institute for Cancer Research and mortality: a census-linked cohort. Am J Clin Nutr. 2016;104(3):678–85.
Miller PE, et al. Comparison of 4 established DASH diet indexes: examining associations of index scores and colorectal cancer. Am J Clin Nutr. 2013;98(3):794–803.
Baer HJ, et al. Risk factors for mortality in the nurses’ health study: a competing risks analysis. Am J Epidemiol. 2011;173(3):319–29.
Soliman GA. Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients. 2018;10(6):780.
Kanter MM, et al. Exploring the factors that affect blood cholesterol and heart disease risk: is dietary cholesterol as bad for you as history leads us to believe? Adv Nutr. 2012;3(5):711–7.
Macpherson H, Pipingas A, Pase MP. Multivitamin-multimineral supplementation and mortality: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2013;97(2):437–44.
Michaelsson K, et al. Long term calcium intake and rates of all cause and cardiovascular mortality: community based prospective longitudinal cohort study. BMJ. 2013;346:f228.
Li K, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012;98(12):920–5.
Xiao Q, et al. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639–46.
Fang X, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. 2016;14(1):210.
Hashemian M, et al. Systematic review of zinc biochemical indicators and risk of coronary heart disease. ARYA Atheroscler. 2015;11(6):357–65.
Eshak ES, et al. Associations between copper and zinc intakes from diet and mortality from cardiovascular disease in a large population-based prospective cohort study. J Nutr Biochem. 2018;56:126–32.
Hashemian M, et al. Systematic review of zinc biomarkers and esophageal cancer risk. Middle East J Dig Dis. 2014;6(4):177–85.
Khademi H, et al. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50,000 adults in Iran. BMJ. 2012;344:e2502.
Abnet CC, et al. Reliability and validity of opiate use self-report in a population at high risk for esophageal cancer in Golestan, Iran. Cancer Epidemiol Biomark Prev. 2004;13(6):1068–70.
Acknowledgements
We are grateful to all participants of the study, and the Golestan Cohort Study for expert help in collecting the data.
Funding
This work was supported by the World Cancer Research Fund International (Grant Number: WCRF 2016/1633), Tehran University of Medical Sciences (Grant Number: 81/15), Cancer Research UK (grant number: C20/A5860), the Intramural Research Program of the U.S. National Cancer Institute, National Institutes of Health, and the International Agency for Research on Cancer.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Review Boards of the U.S. National Cancer Institute (NCI), the International Agency for Research on Cancer (IARC), and the Digestive Disease Research Institute of the Tehran University of Medical Sciences (DDRI). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hashemian, M., Farvid, M.S., Poustchi, H. et al. The application of six dietary scores to a Middle Eastern population: a comparative analysis of mortality in a prospective study. Eur J Epidemiol 34, 371–382 (2019). https://doi.org/10.1007/s10654-019-00508-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-019-00508-3