Abstract
Cardiovascular disease (CVD) risk factors, incidence and death increases from around the time of menopause comparing to women in reproductive age. A healthy lifestyle can prevent CVD, but it is unclear which lifestyle factors may help maintain and improve cardiovascular health for women after menopausal transition. We conducted a systematic review and meta-analysis of prospective cohort studies to evaluate the association between modifiable lifestyle factors (specifically smoking, physical activity, alcohol intake, and obesity), with CVD and mortality in middle-aged and elderly women. Pubmed, Embase, among other databases and reference lists were searched until February 29th, 2016. Study specific relative risks (RR) were meta-analyzed using random effect models. We included 59 studies involving 5,358,902 women. Comparing current versus never smokers, pooled RR were 3.12 (95% CI 2.15–4.52) for CHD incidence, 2.09 (95% CI 1.51–2.89) for stroke incidence, 2.76 (95% CI 1.62–4.71) for CVD mortality and 2.22 (95% CI 1.92–2.57) for all-cause mortality. Physical activity was associated with a decreased risk of 0.74 (95% CI 0.67–0.80) for overall CVD, 0.71 (95% CI 0.67–0.75) for CHD, 0.77 (95% CI 0.70–0.85) for stroke, 0.70 (95% CI 0.58–0.84) for CVD mortality and 0.71 (95% CI 0.65–0.78) for all-cause mortality. Comparing moderate drinkers versus non-drinkers, the RR was 0.72 (95% CI 0.56–0.91) for CHD, 0.63 (95% CI 0.57–0.71) for CVD mortality and 0.80 (95% CI 0.76–0.84) for all-cause mortality. For women with BMI 30–35 kg/m2 the risk was 1.67 (95% CI 1.24–2.25) for CHD and 2.3 (95% CI 1.56–3.40) for CVD mortality, compared to normal weight. Each 5 kg/m2 increase in BMI was associated with 24% (95% CI 16–33%) higher risk for all-cause mortality. This meta-analysis suggests that physical activity and moderate alcohol intake were associated with a reduced risk for CVD and mortality. Smoking and higher BMI were associated with an increased risk of these endpoints. Adherence to a healthy lifestyle may substantially lower the burden of CVD and reduce the risk of mortality among middle-aged and elderly women. However, this review highlights important gaps, as lack of standardized methods in assessing lifestyle factors and lack of accurate information on menopause status, which should be addressed by future studies in order to understand the role of menopause on the association between lifestyle factors and cardiovascular events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As women age and reach menopause around the age of 50 years old, estrogen levels decline and there is a deterioration of cardiovascular risk factors and increased risk of CVD and mortality [1,2,3,4,5,6]. Therefore, menopause marks an important period on women’s life to introduce preventive strategies in reducing women’s risk of CVD and mortality.
Adequate changes in lifestyle such as healthy diet, smoking cessation, ideal levels of physical activity, reductions of harmful alcohol intake and keeping a lean body have shown to play a role in CVD prevention [7,8,9,10,11,12], but the evidence is based mainly on men’s populations [13]. Lifestyle factors affect the risk of CVD in both men and women; however, the prevalence and physiological effects may differ between sexes [14]. For instance, prolonged smoking is significantly more hazardous for women than for men [14]. Also, emerging evidence indicates that the amount of alcohol associated with cardiovascular benefits is lower among women than it is among men, meaning that the threshold where drinking becomes harmful is lower in females than males [15]. Further, there is little information on the association between lifestyle factors, CVD and mortality in middle-aged and elderly women, which face the highest burden of CVD [16]. Estrogen has multiple protective cardiovascular effects in women before menopause, but with increasing age the decline in estrogen levels may be harmful [17]. Several lifestyle factors, such as obesity, alcohol intake and physical activity can affect health outcomes and modify the levels of endogenous sex hormones in women, including sex hormone levels [18,19,20]. Also, as women age and go into menopause there is a shift in women towards an increasing prevalence of adverse lifestyle risk factors, including an increase in body weight and higher frequency of alcohol consumption [15]. Previous systematic reviews and meta-analysis examining the association between lifestyle factors and CVD pooled the results for both men and women, included women of different ages, and did not look specifically at middle-aged and elderly women, being a barrier for specific lifestyle recommendations in this susceptible population.
We conducted a systematic review and meta-analysis to examine the association between modifiable lifestyle factors (specifically smoking, physical activity, alcohol intake and BMI) with CVD and mortality in middle-aged and elderly women.
Methods
Search strategy and selection criteria
This review was conducted in accordance with the MOOSE and PRISMA guidelines [21, 22]. Medical databases were systematically searched (i.e. Pubmed, Embase, Medline, Medline, WoS, Lilacs, Scielo, PsycInfo, Popline and Google Scholar databases) up to February 29th, 2016 to identify studies eligible (Supplementary Methods). Studies were eligible for inclusion if the following criteria were met: (1) cohort studies; (2) studies evaluating the effect of at least one of the following lifestyle factors: smoking, physical activity, alcohol intake, and obesity (BMI); (3) studies with at least 2 months of follow-up; (4) studies involving perimenopausal (period immediate prior to the menopause and the first year after menopause) or postmenopausal (12 consecutive months of spontaneous amenorrhea with no obvious pathologic cause (natural menopause)) women and/or mean age of the study population > 40 (menopause occurs between 40 and 60 years), derived from the general population [23,24,25,26]; (5) studies among women without CVD at baseline; (6) studies reporting the following outcomes: overall CVD, fatal and non-fatal CHD, stroke, CVD mortality and/or all-cause mortality. Given the heterogeneity of how diet is measured (e.g. micronutrients, macronutrients, and dietary patterns), it was not included in the current review and would warrant separate investigation.
Two independent reviewers undertook title/abstract and full text selection. Data extraction was undertaken using pre-defined data collection forms (Supplementary Methods). Leisure time physical activity (LPA) and walking were separated as they are very common forms of physical activity among women [27, 28]. Physical activity assessment and the methodological quality of the studies [29] are described in Supplementary Table 3.
Statistical methods
Findings are presented as mean ± standard deviation (SD), proportions and relative risks (RR). Hazard ratios and incidence density ratios were directly considered as relative risks. Log RR’s of the most adjusted estimate in each study were calculated. Standard errors (SE) of the log RR’s were calculated using published confidence intervals.
Estimates were not included in the pooled results when the reported reference categories were not comparable to the other studies or cut-off values were not described, as this prevented the assumption of a normal distribution within that category. Given that studies lack standardization describing physical activity levels, the relative risk was calculated comparing the highest to lower exposure categories in each study (Supplementary Methods).
Heterogeneity of findings across individual studies was assessed by the I2 statistic and the Cochrane X2 statistic. Summary log RR’s were calculated by pooling the study-specific estimates using a random-effects model, in order the minimize effects of between-study heterogeneity. Meta-regression analyses were done to investigate how different BMI categories [30] relate to outcomes (Supplementary Methods). When possible, subgroup analyses were conducted to investigate the major sources of study heterogeneity, by characteristics such as duration of follow-up, geographical region and age. A subgroup analysis was restricted to women aged 50 and above as the majority of women experience menopause after the age of 50 [25, 26].
Publication bias and small studies effect across studies was evaluated by using funnel plots and Egger tests [31]. Additionally, harvest plots were built to summarize the evidence on the effect of combined lifestyle factors on CVD, CHD, stroke and mortality [32].
All analyses were undertaken in Stata, version 11 (StataCorp, College Station, Texas). p < 0.05 was used to determine statistical significance.
Further methodological details are described in the Supplementary Methods.
Results
Study characteristics
Of 6912 unique citations, 59 studies met the inclusion criteria (Fig. 1, Table 1 and Supplementary References). The studies comprised 5,358,902 women of which 10,519 experienced overall CVD, 27,943 CHD (fatal and non-fatal), 15,323 strokes, 19,588 CVD mortality and 194,362 all-cause mortality. Of the 30 different prospective cohort studies, 15 were from North America, 1 from South America, 11 from Europe, and 3 from the Western Pacific region.
Included studies had a follow-up ranging from 3.2 to 32 years. Most studies were well designed and defined cohorts and therefore scored a high methodological quality grading, with only three [33,34,35] scoring moderate quality.
Most of the studies were adjusted for confounders such as age, smoking, physical activity, alcohol intake, hormone replacement therapy and BMI. Few studies adjusted for potential confounders such as education, menopausal status and cardiovascular risk factors (Supplementary Table 3).
Smoking
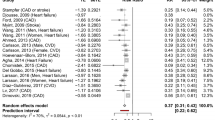
Twenty articles evaluated smoking, comprising 2,828,086 women (Table 1a and e). Only one study reported overall CVD, reporting that CVD risk was at least two times higher for current compared to never smokers (Supplementary Table 3) [36]. Compared to women who never smoke, smokers had an increased risk of 3.12 (95% confidence interval CI, 2.15–4.52) for CHD incidence, 2.09 (95% CI 1.51–2.89) for stroke incidence, 2.76 (95% CI 1.62–4.71) for CVD mortality and 2.22 (95% CI 1.92–2.57) for all-cause mortality (Fig. 2a).
The association between lifestyle factors and overall CVD, coronary heart disease, stroke, CVD mortality and all-cause mortality in cohort studies. a Association of smoking habits and different outcomes in cohort studies. Heterogeneity for all-cause mortality I2 = 97.3%, p = 0.000; for CHD I2 = 98.4%, p = 0.000; CVD mortality I2 = 98.5%, p = 0.000; stroke I2 = 96.3%, p = 0.000. b Association of physical activity and different outcomes. Leisure time physical activity, heterogeneity for overall CVD I2 = 0%, p = 0.0; CHD I2 = 10.9%, p = 0.001; stroke I2 = 0%, p = 0.0; CVD mortality I2 = 59.3%, p = 0.016; for all-cause mortality I2 = 37.8%, p = 0.004. Walking, heterogeneity for overall CVD I2 = 0%, p = 0.94; CHD I2 39.3%, p = 0.008; stroke I2 = 20.2%, p = 0.286; CVD mortality I2 = 64.4%, p = 0.094; for all-cause mortality I2 = 66.8%, p = 0.049. c Association of alcohol intake categories and different outcomes. Moderate intake, less than 98 g/week of alcohol. Heterogeneity for all-cause mortality I2 = 0%, CVD mortality I2 = 56.9%, p = 0.098, CHD I2 = 44.1%; high intake, between 98 and 322 g/week of alcohol. Heterogeneity for all-cause mortality I2 = 0%, CVD mortality I2 = 0%, p = 0.83. d Association of BMI categories and different outcomes. Heterogeneity for all-cause mortality and 25–30 km/m2, I2 = 0%, p = 0.000; 30–35 km/m2, I2 = 84.4%, p = 0.000; 35–40 km/m2, I2 = 69.8%, p = 0.037; 40 km/m2, I2 = 0.0%, p = 0.345. CI, confidence interval; CHD, coronary heart disease; CVD, cardiovascular disease; N, number; RR, relative risk
Physical activity
Twenty-nine articles evaluated physical activity, comprising 1,145,462 women, (Table 1b and e). Studies analysing domains of physical activity other than LPA and walking (e.g. occupational and transport time) are described in Supplementary Table 3. Participants with the higher level of LPA had a risk reduction of 26% (95% CI 20–33%) for overall CVD incidence, 29% (95% CI 25–33%) for CHD incidence, 23% (95% CI 15–30%) for stroke incidence, 30% (95% CI 22–35%) for CVD mortality and 29% (95% CI 25–31%) for all-cause mortality, compared to participants with the lowest level in each study (Fig. 2b). Also in harvest plots, we observed an inverse association between LPA and all outcomes (Supplementary Fig. 4).
Participants with the higher level of walking had a risk reduction of 32% (95% CI 19–43%) for overall CVD incidence, 25% (95% CI 14–36%) for CHD incidence, 19% (95% CI 6–31%) for stroke incidence and 28% (95% CI 13–41%) for all-cause mortality, compared to the lowest level of walking in each study (Fig. 2b). There was no association between walking levels and CVD mortality. Harvest plots showed a significant inverse association between walking and the outcomes analyzed, except for CVD mortality (Supplementary Fig. 4).
Alcohol intake
Seventeen articles evaluated alcohol intake, comprising 880,834 women (Table 1c and e). One study found no association between moderate alcohol intake (< 98 g/weak, which corresponds to 1 dose of alcohol/day or 8–14 g of pure alcohol) and overall CVD [37]. Compared to non-drinking, moderate drinkers had a reduced risk of 0.72 (95% CI 0.56–0.91) for fatal and non-fatal CHD, 0.63 (95% CI 0.57–0.71) for CVD mortality and 0.80 (95% CI 0.76–0.84) for all-cause mortality (Fig. 2c). Three studies analysed the influence of alcohol intake on stroke, reporting no association with moderate intake (Supplementary Table 3) [38,39,40]. A higher alcohol intake (98–322 gr/wk) was not associated with CVD or all-cause mortality (Fig. 2c).
Body mass index
Twenty articles evaluated BMI, comprising 5,173,769 women (Table 1d and e). Pooled results indicated an increasing dose–response relation between weight gain with CHD incidence and CVD mortality (Fig. 2d). Compared to a BMI < 25 kg/m2, the risk increased from 1.47 (95% CI 1.20–1.81) for BMI 25–30 kg/m2 to 1.67 (95% CI 1.24–2.25) for BMI 30–35 kg/m2 for CHD; and from 1.46 (95% CI 1.31–1.63) for BMI 25–30 kg/m2 category, 2.3 (95% CI 1.56–3.40) for BMI 30–35 kg/m2 category for CVD mortality. For each 5 kg/m2 higher in BMI the risk of mortality increased by 1.24 (95% CI 1.16–1.33) (Supplementary Fig. 5). Two studies reported no relation between BMI and stroke incidence (per 1-unit increase RR: 1.01, 95% CI 0.99–1.03 and 1.02, 95% CI 0.99–1.05) [39, 41].
Combined lifestyle factors
Six studies analysed a combination of lifestyle factors combined and the risk for CVD mortality and overall mortality (Table 1E). Results could not be meta-analyzed due to heterogeneity of the studies with regard to definition of lifestyle combinations, measurement, outcomes and amount of clustered lifestyle categories (Supplementary Fig. 6). Women combining several healthy lifestyle factors had a lower risk of 78–83% for CHD [7, 42], 55% for stroke incidence [10], 75% for overall CVD incidence [42], between 58 and 88% for CVD mortality [43,44,45], and between 42 and 76% for all-cause mortality [44, 45] (Supplementary Table 3).
Time of follow-up (> 10 years of follow-up) did not explain the heterogeneity between groups (data not shown). The effects estimate remained similar when studies were grouped by region (USA and non-USA) and quality of evidence. For the associations between smoking and CHD, stroke and all-cause mortality, region did not explain the heterogeneity (CHD non-USA 95.9% vs. USA 98.5%; stroke non-USA 97.4% vs. USA 91.2%; all-cause non-USA 98.3% vs. USA 89.6%). The exception was CVD mortality, that did not shown heterogeneity among USA group (Supplementary Table 4). Findings did not alter when the analysis were restricted to women age 50 + (Table 2). As estimates were generally symmetric distributed in funnel plots, publication bias is unlikely (Supplementary Fig. 7). Visual analysis and Egger tests reported that the small studies effect is unlikely (p > 0.05 for all studies).
Discussion
Among middle-aged and elderly women, LPA, walking and moderate drinking were associated with a reduced risk of overall CVD incidence, CHD incidence, stroke incidence, CVD mortality and all-cause mortality. Current smoking (compared to never smoking) and higher BMI (compared to healthy BMI) were associated with an increased risk of these endpoints.
Our findings confirm smoking as an important risk factor for CVD and mortality in women [9]. Smoking has an antioestrogenic effect, which modulates bone mass, endometrium and breast tissue, affecting women`s all-cause mortality [46,47,48]. In smokers, low estrogen levels could cause an adverse impact on lipid profile, with elevations in cholesterol and triglyceride levels and reductions in high-density lipoprotein cholesterol levels, leading to endothelium dysfunction and atherosclerotic plaque formation [46, 48, 49]. Furthermore, studies have indicated that smoking could trigger premature menopause [14, 50]. Reducing smoking use, as well as, inciting early cessation to prevent CVD and mortality are important public health interventions that should be specifically tailed for women’s preferences, attitudes and detailed smoking habits.
In our study LPA and walking findings echo the results from previous meta-analyses up to 2010 which incorporated a broader age range (including women aged less than 40 years), reporting that LPA is associated with reduced risk of CHD incidence, stroke incidence and all-cause mortality [51, 52], and that walking is associated with a reduced risk of CVD incidence and all-cause mortality [53] in women. Our findings support the current guidelines stating that any level of physical activity is better than nothing and that engaging in more than 150 min/wk of moderate physical activity reduces the risk for adverse health outcomes [54,55,56]. Considering the health benefits of physical activity upon cardiovascular function and survival, it is paramount that women are encouraged to engage in physical activity of any level [50].
Our alcohol intake findings are in line with prior reviews comprising men and wider age ranges [20, 57]. Contradictory to our findings a 2010 meta-analysis reported an inverse association for moderate alcohol intake only for ischemic stroke, for both men and women [58]. The mechanisms linking alcohol intake with CVD and mortality in women are not well understood. Alcohol intake may have pro-estrogenic effects [59, 60]. The levels of dehydroepiandrosterone sulfate (DHEAS), a precursor of estrogen, are increased with alcohol intake as a consequence of adrenal secretion and can lead to increases in HDL cholesterol [59, 60]. For each 30 g alcohol/day (~ 2 doses of alcohol/day) there is an increase of 3.66 mg/dL of HDL and 8.67 mg/dL of apolipoprotein [61]. These factors support the hypothesis that indirect pathways, such as sex hormones and additional biomarkers, might explain the association between alcohol intake and CVD in women. It is also not clear whether wine provides a more protective effect than other alcoholic beverages [61,62,63]. Further research is required to examine different types of alcoholic beverages, and their specific components are associated with CVD outcomes.
In the current review, overweight and obesity were associated with CHD incidence, CVD mortality and all-cause mortality. We found no evidence that higher BMI would be associated with a higher incidence of overall CVD incidence or stroke incidence. Comparable associations were found in The Prospective Studies Collaboration, where each 5 kg/m2 increase of BMI was associated with a 26% higher risk for all-cause mortality among women [64]. In the National Cancer Institute Cohort Consortium, healthy women aged 19–84 years old had a 13% higher risk for all-cause mortality if they were overweight and 44% if they were obesity class I [65]. Obesity might induce a pro-inflammatory status, which subsequently might lead to increasing CVD risk. Also, adipose tissue is an endocrine organ and affects levels of estradiol, which is altered with menopause transition and suggesting a vicious circle among higher weight, menopause and aging [66]. Obesity is affected by demographic, socioeconomic status and behavior, and as most studies adjusted for these factors (including physical activity and diet) our findings may be an underestimate of the full effects of obesity on cardiovascular risk [66].
On one hand, we found consistent evidence that combine lifestyle factors are associated with CHD incidence, CVD mortality and all-cause mortality. On the other hand, we found limited evidence that combine lifestyle factors are associated with overall CVD incidence and stroke incidence. Previous meta-analyses have reported that four healthy lifestyle factors combined reduced the risk of all-cause mortality by 66% in a general population [67]. While there have been efforts to define cardiovascular health [68], there is still no consensus of the definition of a healthy lifestyle, especially according to age and menopausal status for women [69].
Compared with the most recent previous quantitative reviews [9, 11, 12, 51, 52, 58, 70], our study had greater precision including several larger and higher quality cohort studies for various exposure-outcome associations (effect of smoking, alcohol, LPA, walking and BMI on overall CVD incidence, fatal and non-fatal CHD incidence, stroke incidence, CVD mortality and all-cause mortality). Also, previous analyses have not specifically evaluated these associations among middle-aged and elderly women. Providing the correct health promotion information at each life stage is an important aspect of public health and it was not clear if the effect of lifestyle upon cardiovascular disease outcomes differs by age for women. In addition, since most studies did not report the estimates by menopausal status, in our study we restricted a subgroup analysis among women aged 50+, providing more information on the association between lifestyle factors and risk of CVD and mortality in postmenopausal women. Our analyses included a larger sample (more than 5 million) and a longer follow-up than prior reviews.
However, some limitations merit consideration. Most studies were conducted in the United States and Western Europe, hence, the results may be not generalizable. To limit the risk of reverse-causation (especially in women of older age since they are more prone of suffering from a disease which can lead to changes in lifestyle factors), we excluded studies among women with chronic disease at baseline and this may limit generalizability. Few studies evaluated changes of lifestyle factors over time, which may lead to potential misclassification of the exposures (i.e. as part of treatment for chronic diseases). Many studies failed to measure the use of hormone therapy or did not report estimates by menopausal status. We followed the SWAN study’s methodology, that reported using a cutoff age of 50 to distinguish premenopausal from postmenopausal women offered the highest specificity and the lowest false positivity compared to menstrual history-based definitions [71], to examine a proxy of menopause status. However, taking age as a proxy for menopause status can introduce misclassification. For instance, among 227,700 women, 25% aged 50–54 were classified as premenopausal, and 10% of women aged 40–49 were classified as postmenopausal [72]. Thus, future studies, with accurate information on menopause status, are needed to address this issue.
Most studies that were identified adjusted for a range of relevant confounders. However, some studies did not examine the impact of traditional cardiovascular risk factors (serum lipids, diabetes, blood pressure and smoking) as well as other factors (e.g. education). Therefore, the risk of unmeasured confounding cannot be entirely ruled out.
We were unable to identify the reason for some of our analyses having high heterogeneity. Heterogeneity among studies may have derived in part from inherent bias of the original studies but we were not able to explain it in our subgroup analyses. Sources of heterogeneity are likely to include population differences, including sample size, ethnicity and menopausal status [24]. Further, the included studies in the review used different methodology to assess lifestyle factors; did not consider duration of smoking; type, frequency and cut-off units of alcohol intake and physical activity; or changes during the follow-up, which might have contributed to the heterogeneity in effects observed in our analyses. The number of available studies in some analyses was small, precluding our ability to quantitatively investigate the sources of the observed heterogeneity. Typical to any literature-based review, despite the conventional funnel plots and Egger test estimates indicating minimal publication bias, we cannot exclude the possibility of publication bias coming from underreporting of negative findings.
Our risk estimates for the relation of several lifestyle factors with CVD and mortality for middle-aged and elderly women, are an essential motivation tool when implementing preventive measures. Governments and health care agencies require such scientific evidence to direct their efforts in promoting primary prevention programs among middle-aged and elderly women, which may also facilitate passive and active measures resulting in the adoption of a healthy behavior among a population who are at an increasing risk of CVD and mortality during and after their transition to menopause.
Future studies looking at lifestyle factors should include standardized measures, as MET/wk (metabolic equivalent per week) and minutes/wk, to facilitate the pooling effects analysis. Combined lifestyle factors following guidelines would be of great value and there are gaps in the literature regarding lifestyle recommendations, specifically by menopausal status.
A recent study, quantifying the risk of myocardial infarction between men and women suggested that it is unlikely that the risk when moving from pre to postmenopause is due to hormone changes, and the risk increase steadily with age [73]. Since the literature still presents divergent results regarding menopause, age and CVD risks, we believe it is important to improve the methodological rigor of standardizing the results by menopausal status.
Conclusion
Healthy lifestyle factors are associated with a reduced risk of CVD and mortality in middle-aged and elderly women. While engaging in physical activity and moderate alcohol intake had a significant impact in reducing overall CVD incidence, CHD incidence, stroke incidence, CVD mortality or all-cause mortality, smoking and excessive adiposity were related to an increased risk of these endpoints. These findings are an essential motivation tool for implementation of preventive strategies and to encourage women to improve their lifestyles. Changes in sex hormones levels have been suggested to mediate these effects, but the evidence is not clear [73]. Therefore, future studies are required to explore the mechanisms behind these associations.
References
Agrinier N, Cournot M, Dallongeville J, et al. Menopause and modifiable coronary heart disease risk factors: a population based study. Maturitas. 2010;65(3):237–43. https://doi.org/10.1016/j.maturitas.2009.11.023.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–292. https://doi.org/10.1161/01.cir.0000441139.02102.80.
Matthews KA, Crawford SL, Chae CU, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009;54(25):2366–73. https://doi.org/10.1016/j.jacc.2009.10.009.
van der Graaf Y, de Kleijn MJ, van der Schouw YT. Menopause and cardiovascular disease. J Psychosom Obstet Gynaecol. 1997;18(2):113–20.
Muka T, Asllanaj E, Avazverdi N, et al. Age at natural menopause and risk of type 2 diabetes: a prospective cohort study. LID https://doi.org/10.1007/s00125-017-4346-8.
Muka T, Oliver-Williams C, Kunutsor S, et al. Association of age at onset of menopause and time since onset of menopause with cardiovascular outcomes, intermediate vascular traits, and all-cause mortality: a systematic review and meta-analysis. JAMA Cardiology. 2016;1(7):767–76.
Akesson A, Weismayer C, Newby PK, Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch Intern Med. 2007;167(19):2122–7.
Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health. 2011;101(10):1922–9. https://doi.org/10.2105//ajph.2011.300167.
Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378(9799):1297–305.
Kurth T, Moore SC, Gaziano JM, et al. Healthy lifestyle and the risk of stroke in women. Arch Intern Med. 2006;166(13):1403–9.
Peters SA, Huxley RR, Woodward M. Smoking as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 81 cohorts, including 3,980,359 individuals and 42,401 strokes. Stroke. 2013;44(10):2821–8.
Sattelmair JR, Kurth T, Buring JE, Lee IM. Physical activity and risk of stroke in women. Stroke. 2010;41(6):1243–50.
Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–602.
Appelman Y, van Rijn BB, Ten Haaf ME, Boersma E, Peters SA. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis. 2015;241(1):211–8. https://doi.org/10.1016/j.atherosclerosis.2015.01.027.
Taneri PE, Kiefte-de Jong JC, Bramer WM, Daan NM, Franco OH, Muka T. Association of alcohol consumption with the onset of natural menopause: a systematic review and meta-analysis. Hum Reprod Update. 2016;22(4):516–28. https://doi.org/10.1093/humupd/dmw013.
Moller-Leimkuhler AM. Gender differences in cardiovascular disease and comorbid depression. Dialogues Clin Neurosci. 2007;9(1):71–83.
Muka T, Vargas KG, Jaspers L, et al. Estrogen receptor beta actions in the female cardiovascular system: a systematic review of animal and human studies. Maturitas. 2016;86:28–43. https://doi.org/10.1016/j.maturitas.2016.01.009.
Ennour-Idrissi K, Maunsell E, Diorio C. Effect of physical activity on sex hormones in women: a systematic review and meta-analysis of randomized controlled trials. BCR. 2015;17(1):139. https://doi.org/10.1186/s13058-015-0647-3.
Bjornerem A, Straume B, Midtby M, et al. Endogenous sex hormones in relation to age, sex, lifestyle factors, and chronic diseases in a general population: the Tromso Study. J Clin Endocrinol Metab. 2004;89(12):6039–47. https://doi.org/10.1210/jc.2004-0735.
Muller M, den Tonkelaar I, Thijssen JH, Grobbee DE, van der Schouw YT. Endogenous sex hormones in men aged 40–80 years. Eur J Endocrinol. 2003;149(6):583–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop +10: addressing the unfinished agenda of staging reproductive aging. Climacteric. 2012;15(2):105–14. https://doi.org/10.3109/13697137.2011.650656.
Jaspers L, Daan NM, van Dijk GM, et al. Health in middle-aged and elderly women: a conceptual framework for healthy menopause. Maturitas. 2015;81(1):93–8. https://doi.org/10.1016/j.maturitas.2015.02.010.
Henderson KD, Bernstein L, Henderson B, Kolonel L, Pike MC. Predictors of the timing of natural menopause in the Multiethnic Cohort Study. Am J Epidemiol. 2008;167(11):1287–94. https://doi.org/10.1093/aje/kwn046.
NAMS: North American Menopause Society. https://www.menopause.org. Accessed March 2017.
Hu FB, Stampfer MJ, Colditz GA, Ascherio A. Physical activity and risk of stroke in women. JAMA. 2000;283(22):2961–7. https://doi.org/10.1001/jama.283.22.2961.
Kawachi I, Colditz GA, Stampfer MJ, et al. Smoking cessation and time course of decreased risks of coronary heart disease in middle-aged women. Arch Intern Med. 1994;154(2):169–75. https://doi.org/10.1001/archinte.1994.00420020075009.
Wells G, Shea B, O’Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed January, 21 2016.
WHO. Global database on body mass index. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed January, 22 2015.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Ogilvie D, Fayter D, Petticrew M, et al. The harvest plot: a method for synthesising evidence about the differential effects of interventions. BMC Med Res Methodol. 2008;8:8. https://doi.org/10.1186/1471-2288-8-8.
Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. JAMA. 1998;280(21):1843–8.
Salonen JT, Puska P, Tuomilehto J. Physical activity and risk of myocardial infarction, cerebral stroke and death: a longitudinal study in Eastern Finland. Am J Epidemiol. 1982;115(4):526–37.
Sesso HD, Paffenbarger RS, Ha T, Lee IM. Physical activity and cardiovascular disease risk in middle-aged and older women. Am J Epidemiol. 1999;150(4):408–16.
Gellert C, Schottker B, Muller H, Holleczek B, Brenner H. Impact of smoking and quitting on cardiovascular outcomes and risk advancement periods among older adults. Eur J Epidemiol. 2013;28(8):649–58.
Djousse L, Lee IM, Buring JE, Gaziano JM. Alcohol consumption and risk of cardiovascular disease and death in women potential mediating mechanisms. Circulation. 2009;120(3):237–44.
Ikehara S, Iso H, Toyoshima H, et al. Alcohol consumption and mortality from stroke and coronary heart disease among Japanese men and women: the Japan collaborative cohort study. Stroke. 2008;39(11):2936–42.
Lindenstrom E, Boysen G, Nyboe J. Lifestyle factors and risk of cerebrovascular disease in women: the Copenhagen City Heart Study. Stroke. 1993;24(10):1468–72.
Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997;337(24):1705–14.
Kurth T, Buring JE. Body mass index and risk of stroke in women. Cardiol Rev. 2006;23(3):29–32.
Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. New Engl J Med. 2000;343(1):16–22.
Chiuve SE, Fung TT, Rexrode KM, et al. Adherence to a low-risk, healthy lifestyle and risk of sudden cardiac death among women. JAMA. 2011;306(1):62–9.
McCullough ML, Patel AV, Kushi LH, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(6):1089–97.
van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. Bmj-Brit Med J. 2008;337:1440.
Erhardt L. Cigarette smoking: an undertreated risk factor for cardiovascular disease. Atherosclerosis. 2009;205(1):23–32.
Michnovicz JJ, Hershcopf RJ, Naganuma H, Bradlow HL, Fishman J. Increased 2-hydroxylation of estradiol as a possible mechanism for the anti-estrogenic effect of cigarette smoking. N Engl J Med. 1986;315(21):1305–9. https://doi.org/10.1056/NEJM198611203152101.
Reichert VC, Seltzer V, Efferen LS, Kohn N. Women and tobacco dependence. Med Clin North Am. 2004;88(6):1467–81. https://doi.org/10.1016/j.mcna.2004.07.009.
Willett WC, Stampfer MJ, Manson JE, et al. Intake of trans fatty acids and risk of coronary heart disease among women. Lancet. 1993;341(8845):581–5.
Gold EB, Crawford SL, Avis NE, et al. Factors related to age at natural menopause: longitudinal analyses from SWAN. Am J Epidemiol. 2013;178(1):70–83. https://doi.org/10.1093/aje/kws421.
Li J, Siegrist J. Physical activity and risk of cardiovascular disease–a meta-analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9(2):391–407. https://doi.org/10.3390/ijerph9020391.
Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011;40(5):1382–400. https://doi.org/10.1093/ije/dyr112.
Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med. 2008;42(4):238–43. https://doi.org/10.1136/bjsm.2007.039974.
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. https://doi.org/10.1161/CIR.0000000000000152.
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(11):815–40. https://doi.org/10.1093/jnci/djs207.
Dickie K, Micklesfield LK, Chantler S, Lambert EV, Goedecke JH. Meeting physical activity guidelines is associated with reduced risk for cardiovascular disease in black South African women; a 5.5-year follow-up study. BMC Public Health. 2014;14:498. https://doi.org/10.1186/1471-2458-14-498.
Bellavia A, Bottai M, Wolk A, Orsini N. Alcohol consumption and mortality: a dose-response analysis in terms of time. Ann Epidemiol. 2014;24(4):291–6. https://doi.org/10.1016/j.annepidem.2013.12.012.
Patra J, Taylor B, Irving H, et al. Alcohol consumption and the risk of morbidity and mortality for different stroke types–a systematic review and meta-analysis. BMC Public Health. 2010;10:258.
Rohwer RD, Liu S, You NC, Buring JE, Manson JE, Song Y. Interrelationship Between Alcohol Intake and Endogenous Sex-Steroid Hormones on Diabetes Risk in Postmenopausal Women. J Am Coll Nutr. 2015. https://doi.org/10.1080/07315724.2014.926163.
Sierksma A, Sarkola T, Eriksson CJ, van der Gaag MS, Grobbee DE, Hendriks HF. Effect of moderate alcohol consumption on plasma dehydroepiandrosterone sulfate, testosterone, and estradiol levels in middle-aged men and postmenopausal women: a diet-controlled intervention study. Alcohol Clin Exp Res. 2004;28(5):780–5.
Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. https://doi.org/10.1136/bmj.d636.
Gronbaek M, Becker U, Johansen D, et al. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med. 2000;133(6):411–9.
Rimm EB, Klatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ. 1996;312(7033):731–6.
Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. https://doi.org/10.1016/S0140-6736(09)60318-4.
Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–9. https://doi.org/10.1056/NEJMoa1000367.
Davis SR, Castelo-Branco C, Chedraui P, et al. Understanding weight gain at menopause. Climacteric. 2012;15(5):419–29. https://doi.org/10.3109/13697137.2012.707385.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med. 2012;55(3):163–70. https://doi.org/10.1016/j.ypmed.2012.06.017.
Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. https://doi.org/10.1161/circulationaha.109.192703.
van Dijk GM, Kavousi M, Troup J, Franco OH. Health issues for menopausal women: the top 11 conditions have common solutions. Maturitas. 2015;80(1):24–30. https://doi.org/10.1016/j.maturitas.2014.09.013.
Oguma Y, Shinoda-Tagawa T. Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med. 2004;26(5):407–18. https://doi.org/10.1016/j.amepre.2004.02.007.
Morabia A, Flandre P. Misclassification bias related to definition of menopausal status in case-control studies of breast cancer. Int J Epidemiol. 1992;21(2):222–8.
Phipps AI, Ichikawa L, Bowles EJ, et al. Defining menopausal status in epidemiologic studies: a comparison of multiple approaches and their effects on breast cancer rates. Maturitas. 2010;67(1):60–6. https://doi.org/10.1016/j.maturitas.2010.04.015.
Albrektsen G, Heuch I, Lochen ML, et al. Lifelong gender gap in risk of incident myocardial infarction: the Tromso Study. JAMA Intern Med. 2016;176(11):1673–9. https://doi.org/10.1001/jamainternmed.2016.5451.
Funding
LJ, GMVD, TM, KD, MT and OHF work in ErasmusAGE, a center for aging research across the life course funded by Nestlé Nutrition (Nestec Ltd.), Metagenics Inc. and AXA. VC and GGVV were supported by Coordination of Improvement of Higher Education Personal (CAPES) and The National Council for Scientific and Technological Development (CNPQ). MK is supported by VENI grant from The Netherlands Organization for Health Research and Development (ZonMw VENI, 91616079). The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
VC and OHF had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. VC and CPV contributed equally. Concept and design: VC, LJ, OHF. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: all authors. Critical revision of the manuscript for important intellectual content: All Authors. Statistical analysis: VC, CPB, RC. Obtaining funding: OHF. Study supervision: OHF.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Cristina P. Baena, Loes Jaspers, Gabriella M. van Dijk, Taulant Muka, and Oscar H. Franco have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Colpani, V., Baena, C.P., Jaspers, L. et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol 33, 831–845 (2018). https://doi.org/10.1007/s10654-018-0374-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-018-0374-z