Abstract
Despite a rapid increase in immigration from low-income countries, studies on immigrants’ mortality in Italy are scarce. We aimed to describe differences in all and cause-specific mortality among immigrants and Italians residing in Turin and Reggio Emilia (Northern Italy), two cities participating in the Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS). We used individual data from the municipal population registers linked to the cause of death registers. All people aged 1–64 years residing between 2001 and 2010 were enrolled (open cohort) and followed up until 2013. The mortality of citizens from high migratory pressure countries (as a whole, and for each macro-area group) was compared with that of Italians; differences were estimated by Poisson regression adjusted by age and calendar year mortality rate ratios (MRRs), and by age-standardized mortality ratios for the analysis of cause-specific mortality. Compared with Italians, immigrants had lower overall mortality (MRR for men: 0.82, 95 % CI: 0.75–0.90; for women: 0.71, 95 % CI: 0.63–0.81). Sub-Saharan Africans experienced a significant higher mortality than Italians (MRR for men 1.29, 95 % CI: 1.03–1.61; for women: 1.70, 95 % CI: 1.22–2.36). Higher mortality for immigrants compared to Italians was observed for infectious diseases, congenital anomalies, some site-specific tumours and homicide mortality. Our study showed heterogeneity in mortality across the macro-areas of origin, and in particular Sub-Saharan Africans seemed to be a vulnerable population. The extension to other cohorts of IN-LiMeS will allow the health status of immigrants and vulnerable groups to be studied and monitored in more depth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many studies carried out in Western countries have shown that immigrants have lower all-cause mortality rates than natives, or at least lower than expected for their socio-economic characteristics [1–3]. These findings are usually explained by the selective migration flows of healthy young people (the healthy-migrant effect [4–6]) and by the remigration of elder and unhealthy immigrants to native countries (salmon bias) [7, 8]. There is also concern about the reliability of demographic data on immigrants’ mortality. In particular the under-recorded emigration and deaths in the country of origin may lead to underestimate immigrants’ mortality [9].
With increasing length of stay in host countries, immigrants tend to lose their initial health advantage because of different mechanisms: the ageing of the first cohorts of immigrants, the cultural and linguistic barriers to access the health care and the acculturation process, which in most cases leads immigrants to experience life conditions and behaviours of people in the lower socioeconomic positions [10, 11].
A great variability in mortality by ethnic group, age, cause of death, place of destination and length of stay has been observed [10, 12–15], pointing out the need for country-specific studies analysing all these factors.
Italy started experiencing a net immigration flow in the last two decades of the twentieth century and, since then, the number of foreigners, especially those coming from high migratory pressure countries (HMPC), has constantly increased. At the beginning of 2015, immigrants accounted for 8.3 % of the total resident population [16]; they were extremely heterogeneous in terms of countries of origin and settlement patterns across the country.
A few studies on immigrants’ mortality have been published in Italy and most of them are descriptive and cross-sectional [17–19]. Two studies between 1997 and 2013 found higher mortality rates among Italians than immigrants and great variation in mortality by cause of death and area of origin among immigrants [18, 19]. To our knowledge, no study on mortality by immigration status in Italy has used a longitudinal approach.
The Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) includes cohorts of residents with individual socio-demographic and health information from 11 cities. To date, an open cohort design is available in two of the participating cities: Turin and Reggio Emilia.
This study aims to evaluate differences in all-cause and cause-specific mortality between Italians and immigrants in Turin (896,773 inhabitants in 2015) and Reggio Emilia (171,655 inhabitants in 2015).
Methods
Setting and data sources
The data sources are the longitudinal studies of Turin and Reggio Emilia. Thanks to an integrated dataset retrieved by the population register, the health information databases and census data, they provide the socio-demographic and clinical history of people residing in the cities at any time since 1971 (in Turin [20]) and 1991 (in Reggio Emilia [21]). This study uses data from 2001 onwards because it was only then that the immigrant population became significant enough.
Study design
We conducted an open cohort study (Fig. 1) including people who were resident in Turin and Reggio Emilia at the 2001 Census Day (21/10/2001) or were subsequently registered by birth or immigration until 31/12/2010. Individuals were followed up until 31/12/2013, allowing a minimum of 3 years of follow-up for everyone. Analyses were restricted to individuals aged 1–64 years during the follow-up time in order to: (a) exclude infant mortality, whose study merits a separate analysis, (b) exclude the older age classes where immigrants are strongly under-represented in Italy and (c) avoid potential un-registration of emigration, which was shown to be more frequent at older ages [22]. Person-years at risk were calculated from the date of enrolment until death or emigration or the end of the follow-up period.
Enrolment criteria of the Turin and Reggio Emilia cohorts and description of subjects, person year (PY) and events. *The record linkage process between the municipal population register and the death register follows a different methodology in the two cities, given the specific characteristics of the local administrative databases. The Turin study performs specific linkages with each health database (in this study the population register linked with the death register 97.9 % of all deaths); the Reggio Emilia study performs a preliminary record linkage with the regional health register (RHR), a database that records every contact made by the population with the regional heath system and contains the anonymous identifier code used for successive linkages with each health database (in this study 99.5 % of all selected residents have been linked to the RHR and 97.5 % of all deaths have been subsequently linked with the death register)
Exposure and other variables
The exposure was immigration status defined on the basis of citizenship: all the individuals residing in either Reggio Emilia or Turin with any citizenship of a HMPC (online supplementary Table I) were considered as immigrants and were analysed as a whole and according to the following macro-areas: Central-Eastern Europe, North Africa, Sub-Saharan Africa, Asia (except for Israel and Japan), and Central and South America. Stateless individuals were also included in the immigrants’ group. In Italy immigrants can obtain citizenship by marriage or, on demand, after a period ranging between 3 and 10 consecutive years of legal residence [23]. Moreover, children born in Italy to foreign parents can obtain citizenship after their 18th birthday. Therefore young people of the so-called “second generation” aged under 18 are also included in the immigrant population. Residents with citizenship of highly developed countries (HDC: other European countries, North America, Oceania, Israel and Japan) were excluded from the analyses, given that previous researches showed that they are generally as wealthy as natives [11] and represent a very small population subgroup (nearly 4 % of all foreign residents in our case). Italians were the reference group. Other variables considered were: age, gender, calendar year and city of residence.
Outcome
Mortality data was retrieved by individual linkage between the population and the cause of death registers, irrespective of whether the death occurred in Italy or abroad. Deaths resulting only from the population register were classified as “population-register-only” (n = 449): they could either be cases awaiting classification within the cause of death database, or cases identified only by the population registries (possibly occurred abroad) or, finally, the result of unsuccessful linkage between the two sources of information. Deaths that occurred abroad, even if included in the death registry, rarely reported the underlying cause. These cases, along with those with a pending judicial investigation were categorised under “ill-defined conditions” (n = 55). For all the other records, the cause of death was assigned according to the ICD coding system. Since during the follow-up period the 9th edition of the ICD classification was replaced by the 10th, the codes were all aligned back to the 9th (online supplementary Table II).
Causes of death were examined according to all the ICD-9 chapters and the most relevant conditions, such as ischemic heart diseases, cerebrovascular diseases and violence related injuries. Among tumours, those with large numbers (lung, colorectal, breast) or with a priori knowledge of a possible risk excess for immigrants (cancers of the upper aero-digestive tract, stomach, liver, cervix uteri, non-Hodgkin lymphoma, leukaemia [24]) were analysed. Among infectious diseases, tuberculosis (TB) and AIDS were presented separately. Furthermore, a wider group of infectious-related causes of deaths was considered. It included all the conditions belonging to the ICD-9 infections chapter, AIDS, and other diseases that were deemed to be attributable to infections but whose ICD code was not included in the infection chapter (pericarditis, endocarditis, pneumonia, hepatitis, meningitis, encephalitis, septicaemia, tumours with estimated infective population attributable fraction higher than 80 % [25]) (online supplementary Table III).
Statistical analyses
All-cause mortality in Italians and immigrants (as a whole, and for each macro-area group) were compared by means of mortality rate ratios (MRRs), estimated with their 95 % confidence intervals through Poisson regression. The analyses were adjusted for age and calendar year, treated as time-dependent covariates. An assessment of the interaction between immigration status and city of residence was performed using both stratification and the likelihood ratio test (LRT). To investigate cause-specific mortality patterns, given the small numbers in mortality strata, age-standardised mortality ratios (SMRs) per 100,000 person-year were computed using the Italian age-specific mortality rates as standard. All the analyses were stratified by gender and city when interaction by city was relevant. Data analyses were performed using Stata/SE 13.1.
Results
Individuals in the two cohorts contributed to a total of 9,546,564 person-years: the percentage of immigrants increased from 3.8 to 14.8 % in Turin and from 6.6 to 17.1 % in Reggio Emilia from 2001 to 2010 (Fig. 2). Sex ratios varied during the study period: while at baseline (21/10/2001) there were more immigrant men than women in both cities (M/F %: 121.8 % in Turin and 130.0 % in Reggio Emilia), at the end of 2010 the number of women overtook the number of men (M/F %: 96.1 % in Turin and 98.5 % in Reggio Emilia). Across the whole study period and in both cities, the age distribution consistently shifted towards young ages in immigrants compared to Italians. The composition by macro-areas of citizenship was different between the two cities. However, in both of them, the proportion of Central and Eastern European citizens increased over time, mostly since 2007 as a consequence of the enlargement of the European Union in 2004, reaching 55.3 % in Turin and 39.3 % in Reggio-Emilia at the end of 2010. The proportions of other origins decreased over time, with the biggest reduction among the Sub-Saharan Africans in Turin (6.1 % in 2010) and Northern Africans in Reggio Emilia (23.6 % in 2010).
All-cause mortality
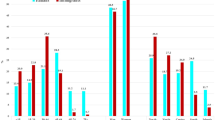
Between 21/10/2001 and 31/12/2013 16,700 deaths occurred. Immigrants accounted for 1,125,563 person-years (12 % of the total observation time) and 787 (5 %) deaths (Fig. 1). Compared to Italians, immigrants showed higher mortality rates at younger ages in both genders (Fig. 3). Starting from the 25–29 age group the mortality pattern reversed, with more pronounced differences as age increased, especially among men. After controlling for age, calendar period and city, immigrants of both genders showed a lower risk of death than Italians (male: MRR = 0.82, CI: 0.75–0.90; female: MRR = 0.71, CI: 0.63–0.81) (Table 1). Mortality by different macro-areas of citizenship revealed a significant risk excess in Sub-Saharan Africans, particularly among women (female: MRR = 1.70, CI: 1.22–2.36; male: MRR = 1.29, CI: 1.03–1.61). Among men, the effect of immigrant status on mortality did not differ by city (LRT: p = 0.57), while it differed significantly among women (LRT: p = 0.01), in particular the excess of mortality risk in Sub-Saharan Africans remained only in Turin and disappeared in Reggio Emilia (MRR = 2.13, CI: 1.49–3.04 and MRR = 0.74, CI: 0.30–1.79, respectively).
Cause-specific mortality
Since cause-specific strata have very small numbers and SMRs among men and women are very similar, Table 2 shows the combined estimates, highlighting any relevant difference by gender. An indication of higher mortality among immigrants was found for the following causes of death: infectious diseases (SMR 1.48, CI: 0.94–2.32) especially TB (SMR 6.60, CI: 2.75–15.87), non-Hodgkin lymphoma (SMR 1.10, CI: 0.65–1.86), leukaemia (SMR 1.14, CI:0.71–1.84); liver cancer (only men: SMR: 1.10, CI: 0.67–1.79), cervical cancer in women (SMR:1.20, CI: 0.45–3.20), musculoskeletal system (only women: SMR 1.56, CI: 0.59–4.17), congenital anomalies, especially among men (men: SMR 1.47, CI: 0.76–2.82) and finally homicides (SMR 3.16, CI: 2.12–4.71). Among immigrants, a significantly higher frequency of deaths was recorded under “ill-defined conditions” (SMR: 2.42, CI: 1.4–4.17) and “population-register-only” (SMR: 3.64, CI: 3.02–4.38) was found. Additionally, to understand the risk excess in total mortality found in Sub-Saharans better, their specific causes of death were analysed: the excess seems to refer to infectious, metabolic blood and circulatory diseases (data not shown).
Discussion
Immigrants resident in Turin and Reggio Emilia showed lower all-cause mortality than Italians. Nevertheless, in Sub-Saharan African men and women an excess mortality risk was found. The results also suggested that immigrants tend to lose their advantage over Italians when mortality from infectious diseases, congenital anomalies, some site-specific tumours and homicide are considered.
Lower all-cause mortality among immigrants compared with natives has been largely reported in literature along with great heterogeneity according to age, country of origin and specific cause of death [2, 12, 13, 26]. We found increased mortality among immigrants in the younger age classes and reduced mortality at older ages. A similar pattern was also documented in The Netherlands [12], in France [26] and elsewhere in Italy [18, 19]. The advantage over Italians that becomes evident among adults may result from the selective migration of healthy individuals (healthy migrant effect), a common feature of the first generations and young adult immigrants. Moreover, the selective unhealthy remigration of a relatively ill subsample of immigrants (salmon bias), which is relevant among elderly immigrants, can play a role, although evidence from literature is inconsistent, depending on the context and appearing more likely in the United States [6] and less likely in Europe [27]. In our data, the high frequency of “ill-defined conditions” and “population-register-only” cases, likely due to deaths that occurred abroad, supports the hypothesis that there is a certain level of salmon bias.
Notwithstanding the limited statistical power for cause-specific deaths, some indications can be drawn from this study. For the main mortality drivers in the population (i.e. tumours and circulatory diseases) immigrant mortality was in line with the average lower level observed in all-cause mortality. Consistently with other studies [19, 24] our results suggest increased mortality among immigrants for liver, cervical cancers and non-Hodgkin lymphomas and a lower risk for breast and colorectal cancers. Excesses can be explained by the higher prevalence in many of the countries of origin of human papilloma virus (HPV) [28] and hepatitis B [29, 30], the main causes of cervical and liver cancer, respectively. Moreover, for cervical cancer, lower screening attendance and suboptimal access to cancer treatment may lead to higher mortality among immigrants. The protective effect for breast and colorectal cancers may be due to the absence of risk factors related to the western lifestyle [24]. The excess of mortality from leukaemia and the higher risk of congenital anomalies could be explained with inverse selective immigration to seek health treatment in countries with better health systems, and for congenital anomalies also with higher prevalence of risk factors among immigrant mothers [31, 32].
Among diseases with a priori knowledge of a possible increased risk among immigrants such as injuries, we did not observe any excess. It is worth noting however that the phenomenon of fatal injuries is generally linked to unsafe working conditions and might be more frequent among immigrant workers who do not reside legally in Italy or are not registered as residents [33], therefore not included in our data. Among the other injuries, we found a higher number of deaths from homicide in immigrants than in Italians, likely explained by the greater social vulnerability, as also found in other studies [12–14].
We did not observe any excess of death due to infectious diseases and related causes, except for TB, HPV and viral hepatitis related cancers which have a long latency from infection to disease manifestation. For acute infections, such as meningitis, septicaemia, and pneumonia (Appendix, Table 3), we observed the same lower risk as all-cause mortality. On the other hand, there are some studies reporting higher occurrence of infectious diseases, not only TB [34, 35], but also meningitis [36] and HIV [37] among immigrants. This pattern suggests that immigrants arriving in Italy are protected from the most severe consequences of the acute infections acquired in the host country (healthy migrant effect), but are exposed to a higher prevalence of some infections in their countries of origin which cause diseases later in life.
The total mortality risk excess in Sub-Saharan Africans is also documented in other European countries [1, 13, 19] with a similar pattern of causes of death; in particular, the higher mortality due to circulatory [19, 38] and infectious diseases [19].
We also found a different effect of immigration status on mortality among Sub-Saharan women by city of residence coming from Sub-Saharan Africa. Differences in the population composition can contribute to explaining this finding. In Turin, where Sub-Saharan African women showed a significant higher mortality, Nigerians represent more than half of the total person-years at risk among Sub-Saharans; their M/F % is 57 % which indicates a large proportion of single women probably exposed to higher social vulnerability. In Reggio Emilia instead, where Sub-Saharan African women did not express higher mortality than Italians, the Ghanaian community is the biggest one with a high M/F % (138 %), suggesting a context involving greater social protection.
Strengths and limitations
The study has a longitudinal approach with an open cohort method. This design has important strengths: first, by enrolling all new entries during the follow-up we accounted for the great dynamism of the immigrant population. Second, by linking individual population records with death registries we obtained the exact person-time at risk and avoided the bias due to the numerator-denominator mismatch in ecological cross-sectional studies [13, 14]. However, biases in the data may occur even when microdata from population register and longitudinal studies are used [9], as in the case of unregistered remigration and deaths of immigrants, especially at older ages [22]. To partially overcome this problem, we truncated estimates at 64 years of age. In addition, unsuccessful linkage with the death register could also result in “immortality denominator”. In our study this problem was prevented using the retrieved “population-register-only” deaths, containing all the cases of failed linkage. A direct check made in the Reggio Emilia cohort with alternative local health databases confirmed the dead-status of all the “population-register-only” cases.
Since the study is based on registers of the resident population, immigrants who were legally present but not resident in the two cities and those who were undocumented, who represent a particularly vulnerable sub-population, were not included. However in Italy the estimated percentage of undocumented immigrants is only 0.5 % of the total resident population [39].
Another limitation of the study is the absence of data on socioeconomic status and on time since arrival in Italy. Several studies showed that health inequalities of immigrants compared to natives are widely attributable to their socio-economic conditions [11, 40]. Thus, taking into account socio-economic status might increase the overall protection observed for immigrants and may have contributed to the higher mortality of Sub-Saharans. Furthermore, the length of time of residence in the host country may be a proxy for acculturation, accumulation of social disadvantage and ageing of cohorts of immigrants: all factors that could jeopardise the health advantage of immigrants [10] and should be taken into account. During the study period, however, most of the immigrants were new arrivals as shown in Fig. 2 and therefore the length of follow-up did not fully account for the complex interactions between gender, social class, place of origin and length of stay [11]. Future analyses with a longer follow-up will allow for more in depth understanding of these mechanisms.
Conclusions
The open cohort approach is a powerful tool for studying the epidemiological profile of immigrants. Although an overall mortality advantage was observed for immigrants compared to Italians, our study highlighted heterogeneity of risks by cause and by macro-area of citizenship; in particular, Sub-Saharan Africans emerged as a vulnerable population. The future availability of other open cohorts within the IN-LiMeS network will increase the power of the study allowing more in-depth evaluations of immigrants’ and vulnerable groups’ health conditions.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- HMPC:
-
High migratory pressure countries
- HDC:
-
Highly developed countries
- ICD:
-
International classification of diseases
- IN-LiMeS:
-
Italian Network of Longitudinal Metropolitan Studies
- LRT:
-
Likelihood ratio test
- MRR:
-
Mortality rate ratio
- SMR:
-
Standardised mortality ratio
- TB:
-
Tuberculosis
- UADT:
-
Upper aero-digestive tract
References
Norredam M, Olsbjerg M, Petersen JH, et al. Inequalities in mortality among refugees and immigrants compared to native Danes–a historical prospective cohort study. BMC Public Health. 2012;12:757.
Gadd M, Johansson S-E, Sundquist J, et al. Are there differences in all-cause and coronary heart disease mortality between immigrants in Sweden and in their country of birth? A follow-up study of total populations. BMC Public Health. 2006;6:102.
Razum O, Twardella D. Time travel with Oliver Twist–towards an explanation foa a paradoxically low mortality among recent immigrants. Trop Med Int Health. 2002;7:4–10.
Parkin DM. Studies of cancer in migrant populations: methods and interpretation. Rev Epidemiol Sante Publique. 1992;40:410–24.
Razum O, Zeeb H, Rohrmann S. The ‘healthy migrant effect’–not merely a fallacy of inaccurate denominator figures. Int J Epidemiol. 2000;29:191–2.
Ullmann SH, Goldman N, Massey DS. Healthier before they migrate, less healthy when they return? The health of returned migrants in Mexico. Soc Sci Med. 2011;73:421–8.
Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, et al. The Latino mortality paradox: a test of the ‘salmon bias’ and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–8.
Razum O. Commentary: of salmon and time travellers–musing on the mystery of migrant mortality. Int J Epidemiol. 2006;35:919–21.
Wallace M, Kulu H. Low immigrant mortality in England and Wales: A data artefact? Soc Sci Med. 2014;120:100–9.
Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97.
Malmusi D, Borrell C, Benach J. Migration-related health inequalities: showing the complex interactions between gender, social class and place of origin. Soc Sci Med. 2010;71:1610–9.
Bos V, Kunst AE, Keij-Deerenberg IM, et al. Ethnic inequalities in age- and cause-specific mortality in The Netherlands. Int J Epidemiol. 2004;33:1112–9.
Regidor E, de La Fuente L, Martínez D, et al. Heterogeneity in cause-specific mortality according to birthplace in immigrant men residing in Madrid, Spain. Ann Epidemiol. 2008;18:605–13.
Ikram UZ, Mackenbach JP, Harding S, et al. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. Published Online First: 11 Sep 2015.
Ott JJ, Paltiel AM, Winkler V, et al. Chronic disease mortality associated with infectious agents: a comparative cohort study of migrants from the Former Soviet Union in Israel and Germany. BMC Public Health. 2008;8:110.
ISTAT. Indicatori demografici.Stime per l’anno 2014. 2015. http://www.istat.it/it/archivio/149003. Accessed 6 Jun 2016.
AGENAS, La salute della popolazione immigrata: il monitoraggio da parte dei Sistemi Sanitari Regionali. 2013. http://www.agenas.it/lea-spesa-sanitaria/la-salute-della-popolazione-immigrata-il-monitoraggio-da-parte-dei-sistemi-sanitari-regionali. Accessed 6 Jun 2016.
Martini A, Chellini E, Sala A. Mortality in immigrants in Tuscany. Epidemiol Prev. 2011;35:275–81.
Fedeli U, Ferroni E, Pigato M, et al. Causes of mortality across different immigrant groups in Northeastern Italy. PeerJ. 2015;69:e975.
Stringhini S, Spadea T, Stroscia M, et al. Decreasing educational differences in mortality over 40 years: evidence from the Turin Longitudinal Study (Italy). J Epidemiol Community Health. 2015;69:1208–16.
Candela S, Cavuto S, Luberto F, et al. Condizioni socioeconomiche e mortalità nella popolazione di Reggio Emilia. http://www.epicentro.iss.it/territorio/CondizioniocioeconomicheMortalit%E0_ReggioEmilia.pdf. Accessed 6 Jun2 016.
Kibele E, Scholz R, Shkolnikov VM. Low migrant mortality in Germany for men aged 65 and older: Fact or artifact? Eur J Epidemiol. 2008;23:389–93.
Ministero dell’Interno. Diritti, doveri, identità, partecipazione. Come diventare cittadini italiani. http://www.interno.gov.it/it/temi/cittadinanza-e-altri-diritti-civili/cittadinanza. Accessed 6 Jun 2016.
Arnold M, Razum O, Coebergh JW. Cancer risk diversity in non-western migrants to Europe: an overview of the literature. Eur J Cancer. 2010;46:2647–59.
de Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13:607–15.
Boulogne R, Jougla E, Breem Y, et al. Mortality differences between the foreign-born and locally-born population in France (2004–2007). Soc Sci Med. 2012;74:1213–23.
Norredam M, Hansen OH, Petersen JH, et al. Remigration of migrants with severe disease: myth or reality?–a register-based cohort study. Eur J Public Health. 2015;25:84–9.
Bruni L, Barrionuevo-Rosas L, Albero G, Aldea M, Serrano B, Valencia S, Brotons M, Mena M, Cosano R, Muñoz J, Bosch FX, de Sanjosé S, Castellsagué X. ICO information centre on HPV and cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary report 2016-02-25. http://www.hpvcentre.net/statistics/reports/XWX.pdf. Accessed 6 June 2016.
Sharma S, Carballo M, Feld JJ, et al. Immigration and viral hepatitis. J Hepatol. 2015;63:515–22.
Coppola N, Alessio L, Pisaturo M, et al. Hepatitis B virus infection in immigrant populations. World J Hepatol. 2015;7:2955–61.
Rondelli R, Dini G, De Rosa M, et al. Foreign children with cancer in Italy. Ital J Pediatr. 2011;37:44.
Cacciani L, Asole S, Polo A, et al. Perinatal outcomes among immigrant mothers over two periods in a region of central Italy. BMC Public Health. 2011;11:294.
Mastrangelo G, Rylander R, Buja A, et al. Work related injuries: estimating the incidence among illegally employed immigrants. BMC Res Notes. 2010;3:331.
Farchi S, Mantovani J, Borgia P, et al. Tuberculosis incidence, hospitalisation prevalence and mortality in Lazio, Italy, 1997–2003. Int J Tuberc Lung Dis. 2008;12(6):193–8.
Arshad S, Bavan L, Gajari K, et al. Active screening at entry for tuberculosis among new immigrants: a systematic review and meta-analysis. Eur Respir J. 2010;35:1336–45.
Giorgi Rossi P, Mantovani J, Ferroni E, et al. Incidence of bacterial meningitis (2001–2005) in Lazio, Italy: the results of a integrated surveillance system. BMC Infect Dis. 2009;9:13.
Porta D, Perucci CA, Forastiere F, et al. Temporal trend of HIV infection: an update of the HIV surveillance system in Lazio, Italy, 1985–2000. Eur J Public Health. 2004;14:156–60.
Regidor E, Astasio P, Calle ME, et al. The association between birthplace in different regions of the world and cardiovascular mortality among residents of Spain. Eur J Epidemiol. 2009;24:503–12.
Centro Studi e Ricerche IDOS. Dossier Statistico Immigrazione 2015. Roma: IDOS Edizioni 2015. http://www.dossierimmigrazione.it/libro.php?cid=47_100&pid=180 Accessed 6 Jun 2016.
Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health. 2003;93:277–84.
Acknowledgments
Luberto Ferdinando, Massimo Vicentini (Interinstitutional Epidemiology Unit, Azienda Unita Sanitaria Locale di Reggio Emilia, Reggio Emilia, Italy, Arcispedale S. Maria Nuova, National Institute for Research and Treatment, Reggio Emilia, Italy), Silvia Franceschi (IARC), Delia Furio (University of Bologna), Lorenza Catellani (Population register office, Municipality of Reggio Emilia).
IN-LiMeS Group
- Alessio:
-
Petrelli
- Anna Maria:
-
Bargagli
- Annibale:
-
Biggeri
- Barbara:
-
Pacelli
- Concetta:
-
Mirisola
- Cristina:
-
Canova
- Ferdinando:
-
Luberto
- Gianfranco:
-
Costanzo
- Gianna:
-
Terni
- Giulia:
-
Cesaroni
- Giuseppe:
-
Costa
- Laura:
-
Bonvicini
- Laura:
-
Cacciani
- Laura:
-
Cestari
- Laura:
-
Grisotto
- Lorenzo:
-
Simonato
- Luisa:
-
Mondo
- Marina:
-
Davoli
- Nera:
-
Agabiti
- Nicola:
-
Caranci
- Nicolás:
-
Zengarin
- Paola:
-
Ballotari
- Paolo:
-
Carnà
- Paolo Giorgi:
-
Rossi
- Serena:
-
Broccoli
- Teresa:
-
Spadea
Contributors
BP, NZ, SB, NC, TS, CDG, AP and PGR contributed to the study concepts and study design. BP, LCacciani and TS retrieved initial references for the background. BP and NZ worked on quality control of data and linkage between datasets and BP analysed data. All the authors participated to the interpretation of the results. BP drafted the manuscript and NZ, SB, NC, TS, CDG, LB, AP, LCacciani, PB and PGR revised important contents in the article. BP worked on manuscript editing. All the authors have seen and approved the final version of the manuscript. BP is the guarantor.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
The record linkage procedures were performed with an anonymized individual key, complying with privacy protection rules. The IN-LiMeS is included in the Italian Statistical Program; privacy and ethical issues has been assessed by the Italian Data Protection Authority and the State and Region Conference.
Funding
This study was funded by the National Institute for Health, Migration and Poverty (INMP).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See the Table 3.
Rights and permissions
About this article
Cite this article
Pacelli, B., Zengarini, N., Broccoli, S. et al. Differences in mortality by immigrant status in Italy. Results of the Italian Network of Longitudinal Metropolitan Studies. Eur J Epidemiol 31, 691–701 (2016). https://doi.org/10.1007/s10654-016-0177-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-016-0177-z