Abstract
Purpose
This phase I trial is to determine the recommended dose of the TAS-102, irinotecan plus bevacizumab regimen and assess its safety and efficacy in patients with metastatic colorectal cancer refractory to fluoropyrimidine and oxaliplatin treatment.
Methods
A 3 + 3 designed dose escalation was performed. Patients were administered TAS-102 (30–35 mg/m2 twice daily on days 1–5) and irinotecan (150–165 mg/m2 on day 1) combined with a fixed dose of bevacizumab (5 mg/kg on day 1) every two weeks. The primary endpoint was the determination of the recommended phase II dose.
Results
Eighteen patients were enrolled: 6 at the Level 1 (TAS-102 30 mg/m2 twice daily, irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg), six at the Level 2 (TAS-102 35 mg/m2 twice daily, irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg), and six at the Level 3 (TAS-102 30 mg/m2 twice daily, irinotecan 165 mg/m2 plus bevacizumab 5 mg/kg). Five dose-limiting toxicities occurred: one observed at Level 1 (thrombocytopenia), two at Level 2 (neutropenia and diarrhea), and two at Level 3 (fatigue and neutropenia). The RP2D was established as TAS-102 30 mg/m2 twice daily and irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg. The most frequent grade 3/4 treatment-related adverse events were neutropenia (33.3%), diarrhea (16.7%), and thrombocytopenia (11.1%). No treatment-related death occurred. Two patients (11.1%) experienced partial responses and 14 (77.8%) had stable disease.
Conclusion
The regimen of TAS-102, irinotecan, and bevacizumab is tolerable with antitumor activity for metastatic colorectal cancer patients refractory to first-line fluoropyrimidines and oxaliplatin treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, colorectal cancer (CRC) ranks as the third most common malignancy and the second leading cause of cancer death [1]. However, due to the late diagnosis, patients with CRC usually lose the opportunity for radical surgery. Approximately 50% of patients who received radical resection might subsequently develop recurrence. Metastatic colorectal cancer (mCRC) patients usually have poor prognoses, with a five-year survival rate of approximately 12% [2]. For microsatellite stable (MSS) colorectal cancer, which accounts for 95% of the cases of colorectal cancer, chemotherapy is still considered the mainstay in the treatment of mCRC [3]. Fluoropyrimidines form the backbone of chemotherapy regimens for mCRC, often combined with oxaliplatin or irinotecan. The addition of targeted agents, such as the anti-VEGF antibody or anti-EGFR antibody, to the chemotherapy regimen has been confirmed to significantly improve overall survival (OS) to almost 30 months in the first-line setting of mCRC [4]. Despite these advances, response to second-line chemotherapy is limited, and few treatment options are available. Therefore, it is urgent to refine and design an optimal second-line treatment regimen to improve the response rate and prolong the survival of patients with mCRC.
Recently, several novel agents were approved for treating refractory mCRC, including TAS-102 [5]. TAS-102 is an oral cytotoxic antitumor agent that consists of trifluridine (FTD) and tipiracil hydrochloride (TPI). FTD is the antitumor component of TAS-102, with two mechanisms of action: inhibiting thymidylate synthase and incorporating it into DNA. The monophosphate form of FTD could inhibit thymidylate synthase, and the triphosphate form of FTD is incorporated into DNA in tumor cells, causing DNA dysfunction. The incorporation into DNA is known to have a lasting antitumor effect since the inhibition of thymidylate synthase caused by FTD rapidly disappears after drug elimination. TPI could prevent the degradation of FTD to potentiate the antitumor activity of FTD [6, 7]. Regarding the unique mechanism of action, TAS-102 was considered effective against tumors resistant to other drugs (e.g., fluoropyrimidines). According to several studies, TAS-102 monotherapy could significantly improve the survival benefit of mCRC patients after progressing on standard chemotherapy [5]. Based on these results, TAS-102 was approved for the treatment of mCRC after two previous lines of treatment.
Even though TAS-102 monotherapy was approved for mCRC third-line treatment, it is expected to be combined with other drugs to reinforce efficacy, which brings a novel regimen for mCRC in a second-line setting. Based on several preclinical studies, the combination of TAS-102 and irinotecan or bevacizumab demonstrated synergistic effects in human colorectal cancer xenograft models [7, 8]. An in vitro study indicated that trifluorothymidine can enhance SN38-induced cytotoxicity (e.g., inducing DNA strand breaks and G2/M arrest) in colon cancer cells, synergizing TAS-102 and irinotecan [9]. Several preclinical studies also showed that TAS-102 exerted antitumor activity against fluorouracil‐resistant cell lines [10,11,12]. Antitumor efficacy of TAS-102 to 5-fluorouracil (5-FU) resistance was also confirmed in the RECOURSE study. In this study, even though approximately 50% of patients received 5-FU in their most recent treatment and had disease progression, the TAS-102 group showed a significant improvement in OS compared to the placebo group [5]. Considering the antitumor activity of TAS-102 even in a 5-FU resistant population, it is logical to apply TAS-102 in combination with irinotecan than to continue administering 5-FU as second-line therapy after failure of fluoropyrimidine treatment. Moreover, the phase III SUNLIGHT study showed that TAS-102 plus bevacizumab could bring longer overall survival for patients with refractory mCRC than TAS-102 alone [13]. Based on these studies, the combination of TAS-102, bevacizumab, and irinotecan might be a new option for mCRC refractory to first-line 5-FU-based chemotherapy.
Another phase II study conducted by our team preliminarily demonstrated that irinotecan, TAS-102 plus bevacizumab regimen could bring promising efficacy with a tolerable safety profile for patients with mCRC as a third-line or beyond treatment. As of January 31st, 2023, efficacy was assessed in 9 patients with an objective response rate (ORR) of 33.3% (unpublished data). Furthermore, two recent studies evaluated this regimen in the second-line treatment setting for mCRC conducted by American and Japanese teams, respectively, which suggested this regimen was feasible [14, 15].
This phase I dose escalation study was aimed to determine the recommended phase II dose (RP2D) of the combination of TAS-102, irinotecan, and bevacizumab for future clinical trials in patients with mCRC refractory to both fluoropyrimidine and oxaliplatin and to evaluate its safety and preliminary efficacy (ClinicalTrials.gov Identifier: NCT06202001).
Patients and methods
Patient eligibility
The main inclusion criteria were as follows: histologically confirmed adenocarcinoma of the colon or rectum; clinically diagnosed with metastatic colorectal cancer based on computed tomography (CT) and magnetic resonance imaging (MRI) according to AJCC 8th edition; previously received oxaliplatin-based first-line treatment; no prior treatment with irinotecan; age from 18 to 70 years old; Eastern Cooperative Oncology Group Performance Status (ECOG PS) of 0 or 1 with no obvious deterioration within two weeks before the administration of the first dose; adequate organ function (bone marrow, liver, and kidney). The key exclusion criteria were as follows: hypersensitive to irinotecan, TAS-102, or bevacizumab; prior exposure to irinotecan; recent major surgery (within four weeks prior to initiating therapy); other concurrent cancer; a severe illness or medical condition.
The study followed the Declaration of Helsinki and good clinical practice guidelines. This protocol was approved by the institution’s ethics committees. Written informed consent was obtained from all patients.
Study design
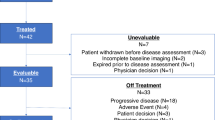
This was a single-arm, open-label, phase I, dose-escalation study to establish the recommended phase II dose (RP2D) for the combination of TAS-102, irinotecan, and bevacizumab and evaluate its safety. This study followed a classic 3 + 3 design, in which patients received escalating doses of TAS-102 (20, 25, 30, or 35 mg/m2/dose, administered twice daily for days 1–5) and irinotecan (135, 150, 165, or 180 mg/m2 on day 1) with a fixed dose of bevacizumab (5 mg/kg on day 1), repeated every 14 days. The flow chart for the dose escalation procedure is illustrated in Fig. 1. Initially, three patients will receive therapy at dose level 1. If dose-limiting toxicity (DLT) occurred, an additional three patients were enrolled at the same dose level. If none of the first three patients or less than two of the six patients exhibited DLT, then the study regimen was escalated to a higher dose level. If two or more DLTs occurred, the study regimen was reduced to a lower dose level. The maximum tolerated dose (MTD) was defined as the highest dose level at which less than one-third of evaluable patients treated had a DLT during the first or second cycle of drug administration. The RP2D was defined as the MTD. At least six patients at the MTD or RP2D were needed to estimate these doses accurately.
Treatment was continued until RECIST-defined disease progression or clinical disease progression, unacceptable toxicity, patient request to withdraw treatment, and a treatment-free period of > 30 consecutive days.
Toxicity assessments
Toxicity assessments were performed in all patients who received at least one dose of the study regimen from the first dose until 30 days after the last dose of the study drug. Adverse events (AEs) were graded based on the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), version 5.0.
A DLT was defined as, during the period starting from drug administration on day 1 of the first course to before drug administration on day 1 of the third course, the occurrence of any toxicities that met one of the following criteria: grade 4 neutropenia lasting > 7 days; febrile neutropenia, grade 4 thrombocytopenia, or grade 3 thrombocytopenia requiring platelet transfusion; drug-related toxicity resulting in a > 14-day delay in starting cycle 2 or 3; and grade ≥ 3 non-hematologic toxicity except for the following AEs: grade ≥ 3 gastrointestinal symptoms that could be controlled by supportive care; electrolyte and γGTP abnormalities; and grade ≥ 3 hypertension that could be controlled.
Efficacy assessment
Imaging examination for tumor assessment was performed at baseline and every three cycles or as clinically necessary. The response was assessed by the investigator according to RECIST version 1.1. Patients who had completed one or more cycles of study medication and had undergone radiologic/clinical progression assessments were evaluated for efficacy assessment.
Statistical analyses
The number of patients was based on a standard 3 + 3 design for dose-escalation studies. Descriptive statistics were used to summarize patient baseline characteristics and the safety and efficacy of the treatment. Overall survival (OS) was defined as the time from the date of beginning receiving this regimen to the date of death resulting from any cause. Progression-free survival (PFS) was defined as the time from the date of the first administration of this regimen to the date of the first documented disease progression or death due to any cause. OS and PFS were analyzed using the Kaplan-Meier method. The 95% CIs for median OS and PFS were generated using the Brookmeyer and Crowley method. All statistical analyses were performed using the SPSS version 29.0 (IBM Corp., Armonk, NY, United States). All statistical tests were two-sided; P < 0.05 will be considered statistically significant.
Results
Patient characteristics
Between November 1st, 2022, and September 30th, 2023, 18 patients were recruited and treated. All 18 patients received at least three cycles of the study regimen. The median age was 58.5 years (34–70 years), and ten (55.6%) were female. Fifteen patients (83.3%) had an ECOG PS of 1, and 3 had a PS of 0. Sixteen patients (88.9%) had left-sided colon cancer, and 2 (11.1%) had right-sided colon cancer. Of the 18 patients, fourteen had recurrent disease, and four had unresectable disease. Twelve patients had liver metastasis, and 7 had lung metastasis. Baseline KRAS/NRAS/BRAF gene status analysis was performed in 17 pts. RAS mutations were present in 12 patients, and only one harbored BRAF gene mutation. In terms of prior therapy, ten patients had a history of bevacizumab administration, and two received anti-epidermal growth factor receptor monoclonal antibody in the first-line treatment. Table 1 shows patients’ baseline characteristics and prior therapy in each dose level group.
Determination of the RP2D
One DLT was observed at dose level 1 (TAS-102 30 mg/m2 twice daily, irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg): this patient developed grade 4 thrombocytopenia in cycle 1. At dose level 2 (TAS-102 35 mg/m2 twice daily, irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg), two DLTs were observed. One patient developed grade 4 neutropenia and grade 3 diarrhea in cycle 1, and another developed grade 4 neutropenia in cycle 2.Therefore, this dose was not tolerable. Based on the results of dose level 1 and dose level 2, dose level 3 was designed as TAS-102 30 mg/m2 twice daily and irinotecan 165 mg/m2 plus bevacizumab 5 mg/kg. Two DLTs were observed: one patient developed grade 3 fatigue in cycle 1, and another developed grade 4 neutropenia in cycle 2. Therefore, this dose was also intolerable. On this basis, the RP2D for phase II was established as TAS-102 30 mg/m2 twice daily and irinotecan 150 mg/m2 plus bevacizumab 5 mg/kg (dose level 1).
Safety
Among all patients, 13 (72.2%) experienced one or more treatment-related adverse effects (TRAEs) of any grade. Grade 3/4 TRAEs occurred in 10 patients (55.6%). AEs were predominantly hematologic or gastrointestinal-related. The most common TRAEs were neutropenia (55.6%), diarrhea (22.2%), thrombocytopenia (11.1%), and nausea (11.1%). The most frequently occurring grade 3/4 TRAEs were neutropenia (33.3%), diarrhea (16.7%), and thrombocytopenia (11.1%). In dose level 1, a grade 4 neutropenia occurred in a patient, and a grade 4 thrombocytopenia occurred in another patient. Two cases of grade 4 neutropenia, 2 cases of grade 3 diarrhea, and a grade 3 thrombocytopenia occurred at Level 2. Four serious TRAEs (3 cases of neutropenia and 1 case of fatigue) occurred in 4 patients at Level 3.
Most AEs were reversible and managed with appropriate treatment. No patients discontinued the study due to treatment-related adverse events. At the time of data cutoff, none of the patients died in this study. The common TRAEs are summarized in Table 2.
Efficacy
As of September 30th, 2023, efficacy was assessed in all 18 participants with an overall response rate (ORR) of 11.1% (2 had partial response, PR; 14 had stable disease, SD; 2 had progression disease, PD). Of the 14 patients with SD, 12 patients experienced tumor decrease. As shown in Table 3, the response rate was 33.3% at Level 1, while no response at Level 2 and Level 3. The disease control rate (DCR) was 83.3% at Level 1, 83.3% at Level 2, and 100% at Level 3. The median PFS and median OS were not reached.
Discussion
The primary objective of this dose-escalation phase I study was to evaluate the safety of the combination of TAS-102, irinotecan, and bevacizumab in mCRC patient refractory to fluoropyrimidine and oxaliplatin and to determine the recommended dose for phase II trial. This study preliminarily demonstrated that the biweekly triplet combination was safe and showed modest efficacy in Chinese mCRC patients pretreated with fluoropyrimidine and oxaliplatin. To our knowledge, this is the first study to evaluate such a regimen in Chinese patients.
In recent years, several studies explored the dosing schedule for the irinotecan containing doublet or triplet combination. A Japanese phase I study combining standard TAS-102 regimen (40–70 mg/m2/day on days 1–5 and 8–12, every four weeks) with irinotecan showed preliminary antitumor activity but high incidence of grade 3/4 neutropenia (100%) and febrile neutropenia (30%) [16]. The severe hematological adverse effects hindered the clinical application of this regimen. Therefore, the dosing schedule of this regimen requires optimization. In 2020, results of the BiTS study indicated that biweekly TAS-102 (twice daily on days 1–5, every two weeks) with bevacizumab yielded efficacy similar to that of standard TAS-102 dosing schedule but with reduced toxicity [17]. In other words, the biweekly schedule of TAS-102 combined with bevacizumab could maintain dose intensity and antitumor activity but with better safety. Varghese et al. conducted a phase I study in America evaluating the safety and recommended dose of a biweekly TAS-102-irinotecan-bevacizumab regimen (NCT01916447) [14]. The recommended dose was TAS-102 25 mg/m2 plus irinotecan 180 mg/m2 combined with 5.0 mg/kg of bevacizumab. At the recommended dose, lower frequencies of TRAEs were observed compared to other similar studies. Another Japanese phase I pilot study, the first study evaluating the triple combination of biweekly TAS-102 plus irinotecan and bevacizumab in Asian patients, determined that the RP2D could be defined as TAS-102 35 mg/m2 (administered twice per day on days 1–5) plus irinotecan 150 mg/m2 combined with bevacizumab (5.0 mg/kg) for two weeks [15]. Compared with the other studies exploring second-line irinotecan containing triplet combination, grade 3/4 neutropenia in this study was observed more frequently. However, the incidence of non-hematological toxicities was similar to other studies. It is potentially because of the differences in ethnicity, doses of TAS-102 and irinotecan, and the definition of DLT. On this basis, in our study, lower starting doses of biweekly TAS-102 administration were used, and the recommended dose was defined as TAS-102 30 mg/m2 (twice daily on days 1–5 of a 14-day cycle) plus irinotecan 150 mg/m2 (on day 1 of a 14-day cycle) combined with bevacizumab 5.0 mg/kg (on day 1 of the 14-day cycle).
Concerning safety, in this study, any-grade TRAEs were reported in 13 patients (72.2%). The most common TRAEs were neutropenia, diarrhea, thrombocytopenia, and nausea. Neutropenia, diarrhea, and thrombocytopenia were the major grade 3/4 TRAEs. The safety profile of the regimen of TAS-102 plus irinotecan and bevacizumab was similar to that in TAS-102 monotherapy or other irinotecan containing doublet or triplet combination [14,15,16, 18,19,20,21]. In these previous studies, the rate of all-grade neutropenia ranged from 46 to 100%, and grade 3/4 neutropenia ranged from 24 to 100%. The reported incidence of all-grade diarrhea ranged from 38 to 99.2%, and the incidence in grades ≥ 3 ranged from 0 to 83.4%. The rate of all-grade thrombocytopenia ranged from 14 to 70%, and grade 3/4 neutropenia ranged from 0 to 10%. Notably, compared with two similar studies conducted in the United States and Japan, our study showed decreased all-grade toxicity [14, 15]. None of the patients in our study experienced febrile neutropenia. Most hematological AEs could be managed by delay in the treatment schedule, dose reduction, and basic supportive care. Non-hematological toxicities such as diarrhea, nausea, fatigue, and vomiting were mainly related to TAS-102 and irinotecan, which were also reversible and within our expectations. No TRAE was leading to the discontinuation of treatment or treatment-related deaths. Overall, this triple combination is tolerable, and its overall safety profile is consistent with the individual agents without unanticipated safety concerns.
This study showed modest antitumor activity of the combination of TAS-102 plus irinotecan and bevacizumab in patients refractory to 5-FU and oxaliplatin. In the entire population, the ORR was 11.1%, and the DCR was 88.9%. The median PFS and the median OS were not reached. A previous study reported that the antitumor effect of TAS-102 was dose-dependent [22]. In this study, interestingly, patients in the RP2D cohort with lower dose levels achieved an ORR of 33.3%, which is numerically better than previous trials for other irinotecan containing doublet or triplet combination as second-line therapy. For reference, in several phase III studies conducted in patient refractory to first-line treatment for mCRC, FOLFIRI (leucovorin, fluorouracil, and irinotecan) plus ramucirumab resulted in an ORR of 13.4% and median PFS of 5.7 months, while FOLFIRI plus aflibercept resulted in an ORR of 19.8% and median PFS of 6.9 months [20, 21]. Another multicenter, phase II/III trial showed that the ORR and PFS of TAS-102 plus bevacizumab regimen were 3.8% and 4.5 months, while FOLFIRI plus bevacizumab regimen as second-line treatment for mCRC resulted in an ORR of 7.1% and median PFS of 6.0 months [23]. In addition, two similar phase I trials explored the same regimen in mCRC patients as second-line treatment. The ORR and median PFS reported in the American study were 12% and 7.9 months, and that in the Japanese study were 19% and 7.1 months [14, 15]. Notably, most patients (77.8%, including 2 PR and 12 SD) experienced tumor decrease during their first three treatment cycles, and tumors might decrease further in the subsequent treatment courses. Therefore, the efficacy of this regimen will be further evaluated in the phase II study.
There were several limitations associated with this study. First, this was a nonrandomized prospective study with a limited sample size. As only 18 patients were in the dose-escalation cohort, it was difficult to accurately assess efficacy in such a heterogeneous group with various prognostic factors such as RAS/BRAF status and previous treatment. Second, the pharmacokinetic study was not planned in this study, leaving the safety issues without a rational pharmacokinetic explanation. In addition, as a prospective study, only selected, fit patients were enrolled. Therefore, the findings of our study cannot be extrapolated to unfit or older patients with poor general conditions.
Our study indicated that the combination of TAS-102, irinotecan, and bevacizumab produced a lower rate of myelosuppression. The preliminary efficacy results, especially in the R2PD cohort, showed comparable antitumor activity to the standard second-line treatment regimen. Currently, the phase II study is ongoing, and its results are eagerly anticipated.
Conclusion
In conclusion, this phase I dose escalation trial suggested that the triplet combination of TAS-102, irinotecan, and bevacizumab is feasible with tolerable toxicity for mCRC resistant to first-line therapy with fluoropyrimidines and oxaliplatin. Further investigation of this regimen is warranted.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM et al (2019) Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 69(5):363–385
Lin S, Chen W, Chen Z, Liang J, Zhong L, Jiang M (2022) Efficacy of sintilimab and fruquintinib combination treatment in the management of microsatellite-stable metastatic colorectal cancer: a case report. Ann Transl Med 10(6):380
Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA et al (2017) Effect of First-Line Chemotherapy Combined with Cetuximab or Bevacizumab on overall survival in patients with KRAS Wild-Type Advanced or metastatic colorectal Cancer: a Randomized Clinical Trial. JAMA 317(23):2392–2401
Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N et al (2015) Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med 372(20):1909–1919
Tanaka N, Sakamoto K, Okabe H, Fujioka A, Yamamura K, Nakagawa F et al (2014) Repeated oral dosing of TAS-102 confers high trifluridine incorporation into DNA and sustained antitumor activity in mouse models. Oncol Rep 32(6):2319–2326
Nukatsuka M, Nakagawa F, Saito H, Sakata M, Uchida J, Takechi T (2015) Efficacy of combination chemotherapy using a novel oral chemotherapeutic agent, TAS-102, with irinotecan hydrochloride on human colorectal and gastric cancer xenografts. Anticancer Res 35(3):1437–1445
Tsukihara H, Nakagawa F, Sakamoto K, Ishida K, Tanaka N, Okabe H et al (2015) Efficacy of combination chemotherapy using a novel oral chemotherapeutic agent, TAS-102, together with bevacizumab, cetuximab, or panitumumab on human colorectal cancer xenografts. Oncol Rep 33(5):2135–2142
Temmink OH, Hoebe EK, Fukushima M, Peters GJ (2007) Irinotecan-induced cytotoxicity to colon cancer cells in vitro is stimulated by pre-incubation with trifluorothymidine. Eur J Cancer 43(1):175–183
Emura T, Murakami Y, Nakagawa F, Fukushima M, Kitazato K (2004) A novel antimetabolite, TAS-102 retains its effect on FU-related resistant cancer cells. Int J Mol Med 13(4):545–549
Emura T, Suzuki N, Yamaguchi M, Ohshimo H, Fukushima M (2004) A novel combination antimetabolite, TAS-102, exhibits antitumor activity in FU-resistant human cancer cells through a mechanism involving FTD incorporation in DNA. Int J Oncol 25(3):571–578
van der Velden DL, Opdam FL, Voest EE (2016) TAS-102 for treatment of Advanced Colorectal cancers that are no longer responding to other therapies. Clin Cancer Res 22(12):2835–2839
Prager GW, Taieb J, Fakih M, Ciardiello F, Van Cutsem E, Elez E et al (2023) Trifluridine-tipiracil and Bevacizumab in Refractory Metastatic Colorectal Cancer. N Engl J Med 388(18):1657–1667
Varghese AM, Cardin DB, Hersch J, Benson AB, Hochster HS, Makris L et al (2020) Phase I study of Trifluridine/Tipiracil plus irinotecan and Bevacizumab in Advanced gastrointestinal tumors. Clin Cancer Res 26(7):1555–1562
Taniguchi H, Yamazaki K, Masuishi T, Kawakami T, Onozawa Y, Honda K et al (2023) Bevacizumab, Irinotecan, and Biweekly Trifluridine/Tipiracil for metastatic colorectal Cancer: MODURATE, a phase ib study. Oncologist 28(11):e1108–e13
Doi T, Yoshino T, Fuse N, Boku N, Yamazaki K, Koizumi W et al (2015) Phase I study of TAS-102 and irinotecan combination therapy in Japanese patients with advanced colorectal cancer. Invest New Drugs 33(5):1068–1077
Satake H, Kato T, Oba K, Kotaka M, Kagawa Y, Yasui H et al (2020) Phase Ib/II study of Biweekly TAS-102 in combination with Bevacizumab for patients with metastatic colorectal Cancer refractory to standard therapies (BiTS study). Oncologist 25(12):e1855–e63
Yoshino T, Mizunuma N, Yamazaki K, Nishina T, Komatsu Y, Baba H et al (2012) TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol 13(10):993–1001
Muro K, Boku N, Shimada Y, Tsuji A, Sameshima S, Baba H et al (2010) Irinotecan plus S-1 (IRIS) versus fluorouracil and folinic acid plus irinotecan (FOLFIRI) as second-line chemotherapy for metastatic colorectal cancer: a randomised phase 2/3 non-inferiority study (FIRIS study). Lancet Oncol 11(9):853–860
Tabernero J, Yoshino T, Cohn AL, Obermannova R, Bodoky G, Garcia-Carbonero R et al (2015) Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): a randomised, double-blind, multicentre, phase 3 study. Lancet Oncol 16(5):499–508
Van Cutsem E, Tabernero J, Lakomy R, Prenen H, Prausová J, Macarulla T et al (2012) Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol 30(28):3499–3506
Doi T, Ohtsu A, Yoshino T, Boku N, Onozawa Y, Fukutomi A et al (2012) Phase I study of TAS-102 treatment in Japanese patients with advanced solid tumours. Br J Cancer 107(3):429–434
Kuboki Y, Terazawa T, Masuishi T, Nakamura M, Watanabe J, Ojima H et al (2023) Trifluridine/tipiracil + bevacizumab (BEV) vs. fluoropyrimidine-irinotecan + BEV as second-line therapy for metastatic colorectal cancer: a randomised noninferiority trial. Br J Cancer 128(10):1897–1905
Funding
This work was supported by Beijing Hope Run Special Fund of Cancer Foundation of China (LC2022A10) and Spark Plan (XH-B051).
Author information
Authors and Affiliations
Contributions
S.Y. and W.G. were responsible for the experimental design. Z. J., Y. W., L.J., W.N., R.Z., Y.T., and X.G. were members of the trial management group and were responsible for clinical trial execution and data collection. S.Y. and W.G. contributed to the provision of study material and patients. Z. J. and Y. W. were responsible for writing the original draft and data analysis. S.Y. and W.G. contributed to the supervision and supported final approval of the article. All authors contributed to the manuscript revision and approved the published version of the manuscript. The work reported in the paper has been performed by the authors unless specified in the text.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, J., Yang, W., Liu, J. et al. Phase I study of trifluridine/tipiracil (TAS-102) plus irinotecan in combination with bevacizumab as a second-line therapy for patients with metastatic colorectal cancer. Invest New Drugs 42, 454–461 (2024). https://doi.org/10.1007/s10637-024-01443-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-024-01443-1