Summary
Background The pivotal RESORCE trial showed that regorafenib was effective as second-line therapy for patients with advanced HCC who progressed on first-line sorafenib. Real-world data are needed to assess clinical outcomes and adverse events in the setting of daily practice. Methods Between April 2017 and August 2017, the Named Patient Program (NPP) was activated to provide controlled, pre-approval access of regorafenib in Korea. This analysis is a multicenter retrospective study of patients who received regorafenib under the NPP. Results A total of 49 patients entered into this NPP, and 40 patients received regorafenib in five Korean institutions. All but one patient received regorafenib as second-line therapy after progression on sorafenib, and 36 (90%) and 34 (85%) patients were classified as Child-Pugh A and BCLC stage C, respectively. The response rate was 10% (n = 4). The median progression-free survival (PFS) was 3.7 months (95% CI, 2.5–4.9 months), and the median overall survival (OS) was not reached. The 1 year OS rate was 54.6%. The time-to-progression (TTP) on prior sorafenib was significantly associated with PFS and OS. The most common grade 3–4 toxicities were hand-foot skin reaction (n = 3, 8%), hypertension (n = 2, 5%), and increased aspartate aminotransferase (n = 2, 5%). Conclusion Regorafenib was well-tolerated and effective in patients with advanced HCC who progressed on first-line sorafenib, with efficacy and safety outcomes consistent with those of the previous RESORCE trial. TTP on first-line sorafenib may predict the efficacy of subsequent regorafenib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most common type of liver cancer. In the last decade, it has become one of the most frequently occurring tumors worldwide and one of the most frequent causes of cancer-related deaths globally and in Korea [1, 2]. Potentially curative treatment options for patients with early-stage localized disease include surgical resection, liver transplantation, and ablative therapy [1]. Chemoembolization is the mainstay of treatment for patients with preserved liver function having HCC confined to the liver [1]. However, prognosis is poor in patients with HCC diagnosed at advanced stages or with HCC that has progressed after locoregional therapy. Sorafenib, a multikinase inhibitor, has been established as a standard first-line systemic chemotherapy for patients with advanced HCC based on the success of pivotal phase III trials [2, 3].
Regorafenib is an oral multikinase inhibitor that targets vascular endothelial growth factor receptors (VEGFRs) 1–3, KIT, RET, RAF-1, BRAF, platelet-derived growth factor receptor (PDGFR), fibroblast growth factor receptor (FGFR), and colony-stimulating factor 1 receptor (CSF1R) [4, 5], and showed preclinical activity in HCC models [6]. After 10 years of failures in the development of systemic treatment for HCC, regorafenib recently demonstrated improved survival in patients who progressed on sorafenib in the randomized phase III RESORCE trial [7]. Following the success of the RESORCE trial, cabozantinib showed a survival benefit in the randomized phase III CELESTIAL trial [8], and anti-PD-1 agents, including nivolumab and pembrolizumab, also showed promising activity in non-comparative single-arm trials [9, 10]. Despite these recent positive clinical results, further evaluation of real-world data is warranted due to discrepancies in patient characteristics between clinical trials and daily practice [11].
Therefore, we performed a multicenter retrospective analysis to evaluate the efficacy and safety of regorafenib after failure of sorafenib in Korean patients with advanced HCC.
Method
This study was a multicenter, open-label, non-comparative study of patients who entered the Named Patient Program (NPP) of regorafenib in Korea. Approval from the institutional review boards of participating centers was necessary for the use of regorafenib in each patient. Efficacy and safety data were retrospectively collected and analyzed. Regorafenib was generously provided by Bayer.
Patients
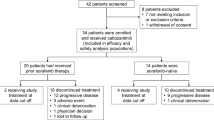
Patients with HCC, confirmed by a pathologic or non-invasive assessment according to the American Association for the Study of Liver Diseases criteria for patients with confirmed cirrhosis, were eligible for inclusion in this NPP if they had evidence of disease progression on sorafenib. Tolerability of first-line sorafenib, which was one of the key inclusion criteria in the RESORCE trial, was not a prerequisite for enrollment in this NPP. A total of 49 patients at five institutions were initially enrolled in the NPP between April and August 2017, and 40 patients received at least one dose of regorafenib. Nine patients did not receive regorafenib at the discretion of their physicians because of deterioration of their medical condition during the approval process.
Treatment
The standard dosing regimen for regorafenib consists of 160 mg orally once per day for 3 weeks, followed by 1 week of no treatment per cycle [7]. However, modification of this regimen was allowed at the discretion of attending physicians. Regorafenib treatment continued until patients experienced intolerable toxicity or the occurrence of disease progression.
Doses were reduced or interrupted as described in the protocol of the RESORCE trial. Dose reduction to 80 mg once daily was allowed.
Evaluation
Safety was evaluated during every clinic visit and graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE), version 4.03. Efficacy was measured using radiological assessments, including computed tomography (CT) or magnetic resonance imaging (MRI) scans, and graded according to the Response Evaluation Criteria In Solid Tumors (RECIST) version 1.1.
Statistical analysis
This analysis was based on the full analysis set (FAS), which included patients who received at least one dose of regorafenib. The overall response rate (ORR) and disease control rate (DCR) at 12 weeks were assessed using RECIST v1.1. Progression-free survival (PFS) was defined as the time from the initiation of regorafenib to the date of disease progression, as determined by RECIST v1.1, or death, whichever occurred first. Overall survival (OS) was defined as the time from the initiation of regorafenib to death from any cause. Survival outcomes were estimated using the Kaplan-Meier method and compared using log-rank tests. In the exploratory analysis, the regorafenib survival outcome was estimated from the start of sorafenib treatment.
Results
Patients
A total of 40 patients who received at least one dose of regorafenib were included in this analysis. The baseline patient characteristics are summarized in Table 1. All patients were Korean and had ECOG performance status of 0–1. Their median age was 62 years (range, 39–83 years), and most patients (n = 36, 90%) were male. Hepatitis B virus infection was the most common etiology of HCC (n = 27, 67%). Except for four patients (10%) with Child-Pugh B (n = 3) and C (n = 1), all patients were classified as Child-Pugh A at the time of initiation of regorafenib. Thirty-three (83%) had extrahepatic metastasis, with the most common metastatic site being the lungs (n = 21, 53%), followed by the peritoneum (n = 11, 28%) and lymph nodes (n = 6, 15%).
Except for one patient who received regorafenib after failure of sorafenib and fluoropyrimidine-platinum chemotherapy, all patients were treated with regorafenib as second-line therapy after progression on first-line sorafenib. The best response to first-line sorafenib was partial response (PR) in four patients (10%), followed by stable disease (SD) in 20 (50%) and progressive disease (PD) in 10 (25%). Response was not evaluable in six patients (15%). Median time-to-progression (TTP) on first-line sorafenib was 4.8 months (95% confidence interval [CI], 3.5–6.0). The last doses of sorafenib were 800 mg/day in 19 patients (48%), followed by 400 mg/day (14, 35%), 600 mg/day (5, 12%), and 200 mg/day (2, 5%).
Regorafenib treatment and adverse events
The starting dose of regorafenib was 160 mg once daily in 28 patients (70%) and 120 mg once daily in ten (25%). The other two patients, one each with Child-Pugh B and C, were started on 80 mg regorafenib once daily. The median duration of administration of regorafenib was 2.4 months (range, 0.5–10.8 months). There were no treatment-related deaths. Adverse events led to treatment discontinuation in three patients (8%), one each due to grade 3 pneumonia, fatigue, and gastrointestinal bleeding. Regorafenib doses were interrupted or reduced in 17 patients (43%); the most common cause of dose modification was hand-foot skin reaction (HFSR, n = 4), followed by fatigue (n = 2) and elevated aspartate aminotransferase (AST) (n = 2).
All 40 patients had at least one treatment-related adverse event, and seven patients (18%) had grade 3–4 adverse events (Table 2). The most frequently reported adverse events were HFSR (n = 27, 68%) and diarrhea (n = 11, 28%). The most frequent grade 3–4 adverse events were HFSR (n = 3, 8%), hypertension (n = 2, 5%), and elevated AST (n = 2, 5%).
Of the 27 patients who showed progression on regorafenib, eight (30%) received subsequent systemic treatment, including five who were treated with nivolumab, one treated with doxorubicin, one entered into a clinical trial of a FGFR inhibitor, and one entered into a clinical trial of an anti-PD-1 agent.
Efficacy
As best response, four patients (10%) achieved PR, whereas none achieved a complete response, resulting in an ORR of 10% (Table 3). SD and PD were the best responses in 19 (48%) and 15 (37%) patients, respectively. The DCR at 12 weeks was 58.2% (95% CI, 42.5–73.9%). All patients who achieved PR were started on a daily dose of 160 mg regorafenib.
With a median follow-up duration of 11.4 months (95% CI, 11.3–11.4 months), the median PFS was 3.7 months (95% CI, 2.5–4.9 months) and the median OS was not reached at the time of analysis (Fig. 1). The 1 year OS rate was 54.6% (95% CI, 39.6–69.6%). For patients with Child-Pugh A, the median PFS was 3.7 months (95% CI, 2.3–5.1 months) and the 1 year OS rate was 60.7% (95% CI, 44.6–76.8%). PFS and OS were not associated with the last dose of sorafenib (p = 0.28 and p = 0.87, respectively), the starting dose of regorafenib (p = 0.68 and p = 0.08, respectively), baseline alpha fetoprotein levels (< 400 vs ≥ 400 ng/mL; p = 0.64 and p = 0.52, respectively), extrahepatic metastasis (p = 0.84 and p = 0.90, respectively), or etiology of HCC (p = 0.60 and p = 0.94, respectively). However, TTP on first-line sorafenib (≥ median [4.8 months] vs < median) was significantly associated with PFS (median, 9.2 months [95% CI, 4.2–14.2] vs 2.5 months [95% CI, 1.3–3.6 months]; p = 0.003) and OS (median, not reached vs 4.7 months [95% CI, 4.2–5.1 months]; p = 0.007; Fig. 2).
Kaplan-Meier analyses of (a) progression-free survival and (b) overall survival during treatment with regorafenib. The median progression-free survival was 3.7 months (95% CI, 2.5–4.9 months). The 1 year overall survival rate was 54.6% (95% CI, 39.6–69.6%), while the median overall survival was not reached at the time of analysis
In the exploratory analysis of outcomes since the start of sorafenib treatment, the median time from the start of prior sorafenib to progression on regorafenib was 10.2 months (95% CI, 3.6–16.9 months) and the median OS from the start of prior sorafenib was not reached. The 2 year OS rate from the start of prior sorafenib was 51.5% (95% CI, 35.2–67.8%).
Discussion
This study was a multicenter, retrospective analysis of Korean patients who received regorafenib in the setting of NPP. This study indicates that regorafenib was well-tolerated and active as second-line therapy after progression on sorafenib in Korean patients with advanced HCC. Regorafenib also showed favorable safety profiles in this study population, in line with the results of the RESORCE trial [7]. Most adverse events were of grade 1 or 2 and manageable with appropriate supportive care. HFSR and diarrhea, the most frequent adverse events, occurred in 68% and 28% of the patients, respectively, whereas HFSR (8%), hypertension (5%), and AST elevation (5%) were the most frequent grade 3–4 adverse events. Although the clinical characteristics of these patients were less favorable than those in the RESORCE trial, including 10% with Child-Pugh B/C and inclusion regardless of tolerability to prior sorafenib, the safety profile of regorafenib in this study was consistent with that in the prior trial. For example, any grade HFSR, diarrhea, and hypertension rates in the RESORCE trial were 52%, 33%, and 23%, respectively, while grade 3–4 rates of these adverse events were 13%, 2%, and 13%, respectively. Although the incidence of HFSR in the present study was greater than that in the RESORCE trial (68% vs 52%), our finding is similar to the results of subgroup analysis of patients of Asian ethnicity included in the RESORCE trial, with any grade and grade 3–4 HSFR rates of 69% and 13%, respectively [12]. Higher HFSR rates in Asian patients than in patients of other ethnicities have also been reported with other multikinase inhibitors [2, 3, 13].
In this study, regorafenib showed an ORR of 10%, a median PFS of 3.7 months, and a 1 year OS rate of 54.6%. When only patients with Child-Pugh A were analyzed, the 1 year OS rate was 60.7%. These results are comparable to those of the RESORCE trial [7], which reported ORRs of 11% by modified RECIST and 7% by RECIST v1.1, a median PFS of 3.1 months, and a median OS of 10.6 months. Our subgroup analysis found that improved TTP on first-line sorafenib was significantly associated with better PFS and OS on regorafenib. Although these findings should be interpreted cautiously, as they are based on a non-comparative analysis and may just reflect the indolent nature of this tumor subgroup, these results may help guide treatment decisions.
An exploratory analysis of the efficacy of the treatment sequence sorafenib-regorafenib for patients in the RESORCE trial found that the median time from the start of prior sorafenib to progression on regorafenib was 14.9 months (95% CI, 13.8–16.6 months) and the median OS from the start of sorafenib was 26.0 months (95% CI, 22.6–28.1 months) [14]. The present study showed similar outcomes, with a median time from the start of prior sorafenib to progression on regorafenib of 10.2 months and a 2 year OS rate from the start of sorafenib of 51.5%. Although this type of exploratory analysis does not represent the outcome of the overall patient population that require systemic treatment, it is clinically meaningful, showing that survival can be prolonged by optimized sequential treatment with sorafenib and regorafenib.
Recently, several novel agents have shown promising outcomes in the second-line setting after failure of sorafenib in patients with advanced HCC. In the randomized phase III CELESTIAL trial, cabozantinib was investigated as second- or third-line therapy for advanced HCC patients who had received prior sorafenib [8]. Cabozantinib significantly prolonged survival compared with placebo, with patients treated with cabozantinib having a median PFS of 5.2 months (95% CI, 4.0–5.5 months) and a median OS of 10.2 months (95% CI, 9.1–12.0 months). Nivolumab, an anti-PD-1 agent, showed an ORR of 15% and a median PFS of 4 months in the phase I/II Checkmate-040 trial [9]. Pembrolizumab, another anti-PD-1 agent, showed similar results, including an ORR of 16% and a median PFS of 4.8 months, as second-line therapy in the single-arm phase II KEYNOTE-224 trial [10] and is under investigation in a randomized phase III trial. The emergence of these promising agents in patients with advanced HCC who progressed on sorafenib raises the issue of the optimal systemic treatment sequence. Future analyses of biomarker and real-world data are warranted.
Despite a retrospective study design and small sample size, our findings are clinically meaningful, inasmuch as this is the largest real-world study to date of regorafenib in patients with advanced HCC.
In conclusion, regorafenib is effective and tolerable in Korean patients with advanced HCC after failure of sorafenib. Our finding is similar to that of the RESORCE trial. TTP on prior sorafenib may predict the outcome of subsequent regorafenib treatment.
References
Bruix J, Sherman M, American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022. https://doi.org/10.1002/hep.24199
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J, SHARP Investigators Study Group (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359:378–390. https://doi.org/10.1056/NEJMoa0708857
Cheng A-L, Kang Y-K, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z (2009) Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 10:25–34. https://doi.org/10.1016/S1470-2045(08)70285-7
Wilhelm SM, Dumas J, Adnane L, Lynch M, Carter CA, Schütz G, Thierauch KH, Zopf D (2011) Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer 129:245–255. https://doi.org/10.1002/ijc.25864
Abou-Elkacem L, Arns S, Brix G, Gremse F, Zopf D, Kiessling F, Lederle W (2013) Regorafenib inhibits growth, angiogenesis, and metastasis in a highly aggressive, orthotopic colon cancer model. Mol Cancer Ther 12:1322–1331. https://doi.org/10.1158/1535-7163.MCT-12-1162
Kissel M, Berndt S, Fiebig L, Kling S, Ji Q, Gu Q, Lang T, Hafner FT, Teufel M, Zopf D (2017) Antitumor effects of regorafenib and sorafenib in preclinical models of hepatocellular carcinoma. Oncotarget 8:107096–107108. https://doi.org/10.18632/oncotarget.22334
Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G (2017) Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389:56–66. https://doi.org/10.1016/S0140-6736(16)32453-9
Abou-Alfa GK, Meyer T, Cheng A-L, el-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen YH, Park JW, Blanc JF, Bolondi L, Klümpen HJ, Chan SL, Zagonel V, Pressiani T, Ryu MH, Venook AP, Hessel C, Borgman-Hagey AE, Schwab G, Kelley RK (2018) Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med 379:54–63. https://doi.org/10.1056/NEJMoa1717002
El-Khoueiry AB, Sangro B, Yau T et al (2017) Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389:2492–2502. https://doi.org/10.1016/S0140-6736(17)31046-2
Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, Verslype C, Zagonel V, Fartoux L, Vogel A, Sarker D, Verset G, Chan SL, Knox J, Daniele B, Webber AL, Ebbinghaus SW, Ma J, Siegel AB, Cheng AL, Kudo M, Alistar A, Asselah J, Blanc JF, Borbath I, Cannon T, Chung K, Cohn A, Cosgrove DP, Damjanov N, Gupta M, Karino Y, Karwal M, Kaubisch A, Kelley R, van Laethem JL, Larson T, Lee J, Li D, Manhas A, Manji GA, Numata K, Parsons B, Paulson AS, Pinto C, Ramirez R, Ratnam S, Rizell M, Rosmorduc O, Sada Y, Sasaki Y, Stal PI, Strasser S, Trojan J, Vaccaro G, van Vlierberghe H, Weiss A, Weiss KH, Yamashita T (2018) Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol 19:940–952. https://doi.org/10.1016/S1470-2045(18)30351-6
Kudo M, Lencioni R, Marrero JA, Venook AP, Bronowicki JP, Chen XP, Dagher L, Furuse J, Geschwind JFH, Ladrón de Guevara L, Papandreou C, Sanyal AJ, Takayama T, Yoon SK, Nakajima K, Lehr R, Heldner S, Ye SL (2016) Regional differences in sorafenib-treated patients with hepatocellular carcinoma: GIDEON observational study. Liver Int 36:1196–1205. https://doi.org/10.1111/liv.13096
Kudo M, Meinhardt G, Bruix J (2017) Regorafenib as second-line treatment of patients with hepatocellular carcinoma (HCC) who progressed on Sorafenib: subgroup analysis of patients from Asia in the phase 3 RESORCE trial. Liver Cancer 6:S8–1. https://doi.org/10.1159/000478029
Yoo C, Kim JE, Lee J-L, Ahn JH, Lee DH, Lee JS, Na S, Kim CS, Hong JH, Hong B, Song C, Ahn H (2010) The efficacy and safety of sunitinib in korean patients with advanced renal cell carcinoma: high incidence of toxicity leads to frequent dose reduction. Jpn J Clin Oncol 40:980–985. https://doi.org/10.1093/jjco/hyq073
Finn RS, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Gerolami R, Caparello C, Cabrera R, Chang C, Sun W, LeBerre MA, Baumhauer A, Meinhardt G, Bruix J (2018) Outcomes of sequential treatment with sorafenib followed by regorafenib for HCC: additional analyses from the phase III RESORCE trial. J Hepatol 69:353–358. https://doi.org/10.1016/j.jhep.2018.04.010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Yoo C, honorarium from Bayer.
Other authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was acquired from all patients.
Rights and permissions
About this article
Cite this article
Yoo, C., Park, JW., Kim, Y.J. et al. Multicenter retrospective analysis of the safety and efficacy of regorafenib after progression on sorafenib in Korean patients with hepatocellular carcinoma. Invest New Drugs 37, 567–572 (2019). https://doi.org/10.1007/s10637-018-0707-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-018-0707-5