Summary
Dysregulation of angiogenesis has been associated with many pathological disorders, including cancer; where angiogenesis has been found to be critical for the maintenance and metastasis of tumours. One of the pathways involved in the regulation of angiogenesis is the phosphatidylinositol3-kinase (PI3K) signalling pathway. The PI3K family consists of enzymes that phosphorylate the 3-OH of the inositol ring of phosphatidyl inositol. There are four isoforms, PI3Kα, PI3Kβ, PI3Kγ and PI3Kδ, that are signalling intermediaries involved in numerous pathways that sustain and maintain the tumours. In this study, we screened eight novel benzoxazine inhibitors of both PI3K isoforms and the related DNA-PK, for their anti-angiogenic effects. Our findings identified the novel benzoxazine (7, 8 (substituted)-2-morpholino-benz (1,3) oxazine: LTUSI122) to be non-toxic at concentrations up to 5 μM, while exhibiting significant inhibition of various aspects of angiogenesis including endothelial proliferation, migration and tube formation. The molecular mechanisms were examined using an angiogenesis array, revealing inhibition of several proliferative and migratory angiogenic factors, including VEGFR, MMP, IL-8, uPAR and MCP; and stimulation of the endogenous inhibitor, endostatin. We hypothesize that these anti-angiogenic effects are mediated by targeting an important signaling intermediary, PI3Kα, and subsequently its action on vascular endothelial growth factor (VEGF, a key growth factor in the process of angiogenesis). If used in combination with more targeted therapies, LTUSI122 could reduce tumour growth and increase the efficacy of these treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer develops when a normally tightly regulated cell transforms, due to genetic alterations or other changes, into a cell with uncontrolled proliferative potential. Following transformation of cells into cancer cells at the primary site, the excessive cell growth demands increased blood supply which triggers the release of growth factors that initiate the development of new blood vessels, a process known as angiogenesis. This process is crucial for further growth of the primary tumour, but also facilitates migration of cancer cells to secondary sites, or metastasis [1].
In a cancerous environment, angiogenesis is triggered by cells under hypoxic stress. Subsequent increase in the levels of hypoxia-inducible factors (HIF), induces transcription of several angiogenic proteins; including Vascular Endothelial Growth Factors (VEGF) and Fibroblast Growth Factor (FGF) [2]. Increase in the levels of these factors stimulates the angiogenic cascade, that attracts inflammatory and endothelial cells to the area, and promotes their proliferation and maturation [3], which supplies the cancerous cells with oxygen and nutrients [2].
The angiogenic cascade begins with the degradation of the extracellular matrix, by matrix metalloproteinases (MMPs), and disruption of cell contacts within a mature blood vessel. This is then followed by the generation of “tip cells” at the outgrowth created by the proliferation of endothelial cells. These newly proliferated endothelial cells then migrate, driven by chemical gradients, to the site of the cancerous mass. Once enough cells have migrated to the area, they align themselves into tube-like structures and are surrounded by a new basement membrane. Finally, the vessels are stabilized by pericytes and then mature into blood vessels [4, 5].
Inhibition of VEGF signalling, either by neutralising antibodies (e.g. Bevacizunab [6]) or VEGF receptor kinase inhibitors (e.g. Suntinib [7]) has proven to be an effective anti-tumour factor. But these molecules have limited use; limited to cancer type, longevity of results and the potential to accelerate metastasis after short term treatment reduces benefits [8]. Another potential target could be the phosphatidylinositol3-kinase (PI3K) family of enzymes, which are involved in many cellular functions; including cell proliferation, differentiation, motility, survival and intracellular signalling [9]. The PI3K family consists of enzymes that phosphorylate the 3-OH of the inositol ring of phosphatidyl inositol. There are four isoforms, PI3Kα, PI3Kβ, PI3Kγ and PI3Kδ. Among the different PI3K isoforms, PI3Kα plays a major role in cancer. It is frequently mutated and over expressed in many human cancers [10]. PI3Kα is also an intracellular signalling intermediary for VEGF [11]. Previous studies have demonstrated the importance of PI3Kα in angiogenesis in vitro by down regulating its expression via short interfering RNA (siRNA), leading to a reduction in migration. The migration inhibition was also evident in vivo, where PI3Kα knockout mice showed significant delay in migration of endothelial tip cells [9].
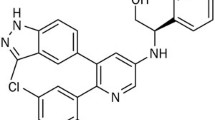
Early PI3K inhibitors, LY294002 and wortmannin, both of which have anti-angiogenic activity were not further explored due to their toxic side effects [12]. However, the anti-angiogenic effect of LY294002 was found be due to inhibition of VEGF signalling and expression [11]. In this study we screened eight, novel 7-and 7,8 (substituted)-2-morpholino-benz (1, 3) oxazines known to act on different PI3K isoforms and the related DNA-PK with varying IC50s (Table 1, [20, 23]), to determine if they have anti angiogenic effects and the molecular mechanisms underlying these processes. Our results show that the novel benzoaxine, LTUSI122, inhibits proliferation, migration and tube formation of endothelial cells (HUVECs) in vitro; and alters the expression of VEGFR2, TGF- β, thrombopoietin, uPAR, MCP-4, ENA-78, MMP-9, IL8 and endostatin following 24 h exposure.
Materials and methods
Compounds and concentrations
The novel benzoxazines being tested were prepared and kindly provided by the chemistry team lead by Dr. Jasim Al-Rawi (Latrobe University, Bendigo, Australia [20, 23]). The PI3K-inhibitor, LY294002, (Cell Signalling, MA) and the DNA-PK inhibitor, NU7026 (Sigma Aldrich, Australia) were included as reference inhibitors. Stock solutions of 1 mM of each test compound were prepared in Dimethyl Sulfoxide (DMSO, Sigma-Aldrich, Australia). Serial dilutions were made from stock solutions to create various concentrations of compounds to be assessed: 0.1 μM, 1 μM and 5 μM. When preparing test compounds dilutions were calculated to ensure that the percentage of DMSO did not exceed the toxic limit 0.5 % v/v. Equivalent concentrations of DMSO were added to the control media.
Cell lines and cell culture
Human umbilical vein endothelial cells (HUVECs, Merck Millipore) were cultured in sterile growth media composed of phenol red free media (Medium200, Life technologies, Australia) enriched with growth factors, hydrocortisone (1 μg/ml), human epidermal growth factor (10 ng/ml), basic fibroblast growth factor (3 ng/ml), heparin (10 μg/ml) (LSGF kit, Life technologies, Australia) and 10 % foetal bovine serum (FBS, Interpath Services, Australia).
Toxicity of compounds
Prior to testing the effect of the novel benzoxazines on HUVECs, an initial toxicity profile of these compounds was completed using CellTox Green Cytotoxicity assay™ (Promega). HUVECs were plated at concentration of 8x103 cells per well in a 96 well plate. When confluent, compounds at different concentrations (0.1 μM, 1 μM and 5 μM) were added, along with 1:500 dilution of cyanine dye to measure fluorescence. After 6 and 24 h, fluorescence was read at 485 nm excitation and 520 nm emission (Flex Station 3, Molecular Devices, California), and expressed as % toxicity compared to the media only control.
Cell Viability - sulphorhodamine blue assay (SRB)
Sulphorhodamine B assay was used to determine compound effect on cell number over time, as described previously with minor alterations [13]. HUVECs were seeded at a concentration of 2x104 cells per well on gelatine coated 24 well plates and allowed to adhere to wells for 24 h. Following incubation, media was removed and cells were resuspended in 1 ml of test media and incubated for a period of 48 h. Control cells where treated with media containing 0.5 % v/v DMSO. Plates were placed in a Flex Station 3 and colour absorbance measured at 540 nm, and expressed as % cell number compared to the media only control.
Migration - Boyden chamber assay
A more quantitative assay to observe the effect of compounds on cell migration is the Boyden chamber. HUVECs were seeded onto cell culture inserts according to manufacturer’s instructions (ThinCertTM, Greiner bio-one Germany) with media containing test compounds and 10 % FBS overnight. Following overnight incubation, cells were harvested and resuspended in low serum supplement media (2 % FBS) to a cell concentration of 106 cells / per ml and added to the culture inserts in the bottom chamber 600 μL/well of media supplemented with the chemo attractant (10 % FBS) and the test compounds at 1 μM or 5 μM. The 24 well plates were then placed in the incubator for 24 h at 37 °C and 5 % CO2. After 24 h, the cell culture medium was removed from each well, and replaced with 450 μl serum-free culture medium containing 8 μM Calcein-AM, and incubated for 45 min. The cell culture inserts were removed, and 200 μl of the solution, now containing the migratory cells, from each well was transferred into a black flat bottom 96 well plate (μ-Clear plate, Interpath, Australia). Fluorescence of Calcein-AM was read using a fluorescence plate reader (Flexstation) at an excitation wavelength of 485 nm and an emission wavelength of 520 nm, and expressed as % migration compared to the media only control.
Tube formation assay
Prior to cell culture, plates were pre-coated with Geltrex (Life technologies, Australia). HUVECs were then added to the Geltrex coated 24 well plates (250 μl, 4 to 5 × 104 cells per well), and 750 μl of test media was added to each well, at either 1 μM or 5 μM. After 24 h exposure, cells were observed and random fields were selected for analysis. Images were captured using a Nikon camera and NIS Elements F 3.0- microscopic imaging software. The number of tubes formed was quantified by counting complete tube-like structures within random fields and expressed % number of tubes compared to the media only control.
Expression of Angiogenic Molecules - Angiogenesis human membrane array
Angiogenesis Human Membrane Antibody Arrays (20 and 23 targets, Sapphire Bioscience) were used to determine the effect of LTUSI122 on proteins expressed during angiogenesis. Manufacturer’s instructions were followed with minor alterations [14, 15]. HUVECs were treated with 1 μM LTUSI122 or media only for 24 h. Cells were then detached and washed twice in PBS. After washing in PBS, cells were resuspended at 1x107 cells / ml in lysis buffer, which was then added to the array membrane. After overnight incubation, membranes were washed with wash buffers. Following the final wash, 1 ml biotin-conjugated anti-cytokines solution (membrane specific) was added to each membrane and incubated at room temperature for 2 h. Following washes with appropriate wash buffers, 2 ml of HRP-SA (Horse Radish peroxidase-streptavidin) was added to each membrane, and incubated at room temperature for 2 h. After washing with wash buffers, detection buffers were added to membranes, and using CCD camera (G-Box, Syngene) membranes were exposed for 30 s, 1, 2 and 4 min to obtain an image with low background and strong positive control. The results were given as pixel density, which was directly proportional to level of expression of the factors investigated. The pixel density was normalised to each membrane positive controls, which then allowed for a comparison between LTUSI122 treated cells and media only control cells.
Statistics and analysis
Data was graphed using the Graph pad prism 5.0 statistical package. The statistical significance was determined using one way ANOVA with Newmanns Keuls Post-test and Student t-test, with the statistical significance indicated with p values less than 0.05.
Results
Toxicity of benzoxazine analogues
The benzoxazine analogues were chosen as they displayed varying inhibitory activity (IC50) to different members of the PIKK family: DNA-PK, PI3Kα, PI3Kβ, PI3Kγ and PI3Kδ. To ensure the compounds had no detrimental effect on the endothelial cells (HUVECs), the toxicity was determined at concentrations between 0.1 and 5 μM. At these concentrations, the activity of different PIKK members would have been inhibited. Of the eight compounds, seven benzoxazine analogues, LTUSI99, LTUSI122, LTUT1, LTUT3, LTUT4, LTUSI118 and LTUT5, did not have a toxic effect on HUVECs in the in vitro environment (Fig. 1). However, the benzoxazine analogue LTUSI58 was found to be extremely toxic at 5 uM compared to the control treated cells. This was almost twice as toxic as comparative inhibitors, LY294002 and NU7026 after 24 h exposure.
Summary of cell toxicity analysis using Cell tox™ green assay. HUVECs were culture in the presence of compounds at varying concentrations (0.1 μM, 1 μM and 5 μM) for 24 h. Graph indicates mean of three replicates ± SEM. (* compound vs. control p < 0.001, **compound vs. control p < 0.0001) indicating toxicity from 3 independent experiments
Benzoaxine analogues have different effects on cell viability
Since endothelial proliferation is important for the formation of new blood vessels, we examined the effect of the benzoaxine analogues on cell number. As LTUSI58 was found to be toxic it was eliminated from any further testing. The remaining seven compounds were tested for their effect on cell number (Fig. 2). After 48 h exposure, LTUSI122 significantly decreased cell number, at 1 μM and 5 μM, when compared to control. The benzoxazine analogues LTUT1, LTUT4 and LTUSI118 caused significant increase in cell number, while NU7026, LTUT3 and LTUSI99 had no effect on cell number. Some of the compounds: LTUT1, LTUT4 LTUSI118 and LTUT3, displayed a different effect on cell number at 5 μM, compared to the trend at the lower concentrations, these cell displayed abnormal morphology (images not shown).
Effect of benzoaxines on HUVECs proliferation, using Sulphorhodamine B assay (SRB). HUVECs were cultured in the presence of compounds at various concentrations 0.1 μM, 1 μM and 5 μM, for 48 h. Graph indicates mean of 3 replicates ± SEM, from 3 independent experiments. (* compound inhibition vs. control p < 0.001, **compound stimulation vs. control p < 0.0001, # compound inhibition vs. control p < 0.05 but shows morphological abnormalities)
Benzoaxine analogues have different effects on migration
Since cell migration is an important process for endothelial cells to form new blood vessels during angiogenesis, we next examined the effect of the benzoaxine analogues on cell migration toward an attractant (10 % FBS) using the quantifiable Boyden chamber assay (Fig. 3). LTUSI122 and LTUT3 significantly inhibited migration of endothelial cells through the gel matrix membrane toward the attractant after treatment for 24 h. All other benzoxazine analogues had no significant effect on migration.
Effect of benzoaxines on cell migration using the Boyden chamber assay. HUVECs were cultured in the presence of compounds at 1 μM or 5 μM, for 24 h. The number of cells that have migrated was colourimetrically assessed and expressed graphically as % migration compared to control ± SEM, of 3 or more replicates, from 2 independent experiments. * indicates significant difference between test compound and control (p < 0.05)
The effect of benzoaxine analogues on tube formation
The realignment of endothelial cells into tube like structures is the final process during angiogenesis. We examined the effect of the benzoxaxine analogues using 3-D matrix (Geltrex). After 24 h in the presence of media only (containing growth factors), the HUVECs reorganise into tube-like structures, characterized by the elongation and connection of cells (Fig. 4a). In the presence of 1 μM and 5 μM of the benzoxazine analogue LTUSI122, Fig. 4b and c respectively, there was a reduction in the formation of tube-like structures. Other compounds, for example LTUSI118 at 1 μM and 5 μM, Fig. 4d and e respectively, showed an increase in the formation of tube-like structures. The visual observations were quantified by counting complete (enclosed) tube-like structures. The number of tubes formed in the presence of LTUSI122 was significantly less when compared to control containing media alone (Fig. 4f). LTUT1 and LTUSI118 both stimulated the number of tubes formed, while other benzoxazine analogues had no effect.
Effect of benzoxazines on tube formation - comparison in the morphology of HUVECs forming tubes after exposure to (a) media with growth factors, (b)1 μM and (c) 5uM of LTUSI112, (d) 1 μM and (e) 5 μM LTUSI118 for 24 h on Geltrex (scale bar: 100 μm). (f) Summary of the number of tube-like structures formed on Geltrex media in the presence of benzoaxines at 1uM or 5uM after 24 h in culture. Graph indicates mean of 3 replicates ± SEM, from 2 independent experiments. * indicates significant difference between test compound and control (p < 0.05)
LTUSI122 alters the expression of several angiogenic molecules
Rapid proliferation of cancerous cells, leads to localised hypoxia, in response cells increase the expression of several angiogenic factors, which stimulate endothelial cells during angiogenesis. The novel benzoxazine, LTUSI122, exhibited an inhibitory effect on several stages of angiogenesis: proliferation, migration and tube formation. To determine the molecular pathways involved, or in this case inhibited by LTUSI122, human membrane antibody arrays were used to assess changes in the levels of 43 known angiogenic molecules. Following treatment with 1 μM LTUSI122, only 9 molecules displayed a change in expression (summarised in Table 2). The levels of the angiogenic factors: VEGFR2, TGF-β, Thrombopoietin, uPAR, MMP-9, IL-8, MCP4 and ENA-78 all decreased expression; while there was an increase in the expression of endostatin, an endogenous inhibitor of angiogenesis.
Discussion
Inhibition of tumor angiogenesis, as a means of reducing the growth of cancers, has become a promising target for adjuvant therapies. In particular, direct inhibition of the VEGF signaling has proven extremely successful, but has limitations [16, 17]. Inhibition of PI3K, which is important for both VEGF signaling and angiogenesis, is a potential alternative [18]. Recently several novel 7-and 7,8 (substituted)-2-morpholino-benz (1, 3) oxazines have been developed, with differing inhibitory effects on the PI3K isoforms and the related DNA-PK [20, 23]. This study evaluated their effect in vitro as potential anti-angiogenic inhibitors using the endothelial cell line HUVECs. Of the benzoaxines selected, only LTUSI122 inhibited all aspects of angiogenesis examined; endothelial proliferation, migration toward an attractant and realignment into tube like structures. LTUSI122 also had a significant effect on the expression of several angiogenic factors, which could attribute to its anti-angiogenic effect.
Seven of the benzoxazine analogues selected, LTUSI99, LTUSI122, LTUT1, LTUT3, LTUT4, LTUSI118 and LTUT5, were not toxic towards HUVECs at the concentrations tested, 0.1 μM, 1 μM or 5 μM. However, LTUSI58, and the control compounds NU7026 and LY294002 were found to be toxic. NU7026, even though it is DNA-PK specific, it is known to have a growth inhibitory effect on HUVECs [19]. LY294002 toxicity has been described previously and may be linked to its lack of specificity [12]. LTUSI58 was found to be even more toxic than both NU7026 and LY294002. The structure of LTUSI58 is very similar to LY294002 [20], with the exception of a phenyl group attached at the 8th position and a Nitrogen atom at 3rd position, identifying these chemical modifications as detrimental to endothelial cell viability. LTUSI58 has significant inhibitory action on all PIKK members and was almost twice as toxic as NU7026 and LY294002, suggesting its toxicity could be an additive effect of inhibition of all PIKK members.
Several in vitro assays were utilised to assess the effect of compounds on endothelial proliferation, migration and tube formation, which are the significant stages of the angiogenic cascade. Of the non-toxic benzoxazines, only LTUSI122 significantly inhibited proliferation of HUVECs. Analogues LTUT1, LTUT4 and LTUSI118 stimulated proliferation, which has been similarly reported for other benzoxazine compounds [21]. This stimulatory effect could be further explored in treatments for ischemic pathologies. The analogues LTUT3 and LTUSI99, and the DNA-PK inhibitor NU7026, had no effect on the proliferation of HUVECs. The effect of NU7026 contradicts previous results by Mannell et al. where a stimulatory effect in HMECs was observed after the same exposure time. They concluded that the fibroblast growth factor (FGF-2) was using DNA-PK in endothelial signaling to regulate proliferation in a negative feedback mechanism to prevent excessive growth [22]. The difference in results could be explained by the different expression patterns of DNA-PK in HUVECs and HMEC, with HMEC expressing significantly more DNA-PK [22].
The final major physiological stage in angiogenesis, tube formation, occurs when the newly formed endothelial cells align into tube-like structures. Using the 3-D Matrigel system, LTUSI122 caused a significant inhibition of tube-like structures formed, both quantitative and histologically. Analogues LTUT1 and LTUSI118 caused an increase in the number of tubes formed, while there was no effect seen on the number of tubes formed with analogues LTUT5, LTUT3, LTUT4 and LTUSI99. A similar effect has been described in HUVECs and HMEC cells treated with LY294002, the PI3K inhibitor, and NU7026, the DNA-PK specific inhibitor. They both inhibited tube formation when PI3K was inhibited, by 10 μM LY294002 and 0.3 mM NU7026 (at this concentration PI3K is also inhibited). But when only DNA-PK was inhibited, at low concentration 0.3 μM NU7026, no effect was observed. These results point to the importance of PI3K over DNA-PK in the process of tube formation. Furthermore, at the concentrations that were used, LY294002 at 10 μM and NU7026 at 3 mM, are both known to cause significant toxicity, so their use as angiogenic inhibitors would not be ideal [22].
Novel benzoxazine LTUSI122 potential angiogenesis inhibitor acting through VEGF / PI3Kα pathway
The benzoxazine analogue, LTUSI122, exhibited anti-angiogenic effects over all the processes of angiogenesis examined, significantly inhibiting proliferation of HUVECs, inhibited migration following a chemotactic signal using the Boyden chamber assay and inhibited the realignment of endothelial cells into tube-like structures, making it an ideal candidate as an angiogenic inhibitor. This inhibitory effect was due to a decrease in the expression of several pro-angiogenic factors; VEGFR2, ENA-78, IL-8, MMP-9, uPAR, MCP-4, TGF- β and thrombopoietin, as well as an increase in one endogenous anti-angiogenic factor, endostatin. We hypothesis the effect of LTUSI122; inhibition of proliferation, migration and tube formation; and the altered expression of angiogenic factors to be linked, directly or indirectly, to signaling of VEGF using P13Kα as a signaling intermediary.
We can hypothesis that LTUSI122 is working primarily through inhibiting PI3Kα, based on the IC50 values in purified enzyme assays, and the expression patterns of the PIKK family in HUVECs. LTUSI122 had weak inhibitory effects on PI3Kβ (IC50 = 14.6) and PI3Kγ (IC50 = 18.1). While strongly inhibiting P13Kδ (IC50 = 1.62), PI3Kα (IC50 = 5.2) and DNA-PK (IC50 = 0.62) in purified enzyme assays [23], so it could be assumed that LTUSI122 inhibition of angiogenesis is through one of these molecules. The weak inhibitory effect on PI3Kβ would exclude this molecule as the primary target. The low levels of expression of P13Kδ and DNA-PK in HUVECs [22] could also rule these molecules out as functional targets. While the strong inhibition PI3Kα (IC50 = 5.20) and the high levels of expression in HUVECs [22] suggest the most promising target for the anti-angiogenic effects. This could be confirmed using Western analysis examining the expression and activity of the PIKK family in HUVECs following treatment with LTUSI122.
To confirm the hypothesized effects of LTUSI122 and the functional pathway, there are several in vitro and in vivo studies that could be completed. In vitro studies, using other endothelial cells lines, which have different PIKK family expression profiles, would confirm the inhibitory effect of PI3Kα. Small interfering RNA (siRNA) knockdown of PI3Kα in HUVECs, followed by culture in the presence of LTUSI122, to examine changes in the absence of PI3Kα. In vivo effects of LTUSI122 could be examined using a Matrigel plug assay implanted in mice.
In the presence of LTUSI122, the stimulatory effects of VEGF on endothelial cells would potentially be abolished, leading to a reduction in the growth and potential induction of apoptosis in the cancerous cells. Following further examination of the effects of LTUSI122 on both endothelial and the cancerous cells, LTUSI122 could be an effective anti-angiogenic molecule used to treat various types of cancers, by inhibiting the formation of new blood vessels, starving the cancer cells. This could enhance the effect of other treatments that more directly target the cancer cells.
References
Brooks SA, Lomax-Browne HJ, Carter TM, Kinch CE, Hall DM (2010) Molecular interactions in cancer cell metastasis. Acta Histochem 112(1):3–25
Semenza GL (2012) Hypoxia-inducible factors: mediators of cancer progression and targets for cancer therapy. Trends Pharmacol Sci 33(4):207–14
Krock BL, Skuli N, Simon MC (2011) Hypoxia-induced angiogenesis: good and evil. Genes Cancer 2(12):1117–33
Chen HH, Zhou HJ, Fang X (2003) Inhibition of human cancer cell line growth and human umbilical vein endothelial cell angiogenesis by artemisinin derivatives in vitro. Pharmacol Res: Off J Ital Pharmacol Soc 48(3):231–6
Sieczkiewicz GJ, Hussain M, Kohn EC (2002) Angiogenesis and metastasis. Cancer Treat Res 107:353–81
Shih T, Lindley C (2006) Bevacizumab: an angiogenesis inhibitor for the treatment of solid malignancies. Clin Ther 28(11):1779–802
Roskoski R Jr (2007) Sunitinib: a VEGF and PDGF receptor protein kinase and angiogenesis inhibitor. Biochem Biophys Res Commun 356(2):323–8
Hyunseung L, Kyung J, Yujeong J, Sungwoo H, Soon-Sun H (2013) HS-173, a novel phosphatidylinositol 3-kinase (PI3K) inhibitor, has anti-tumor activity through promoting apoptosis and inhibiting angiogenesis. Cancer Lett 328(1):152–9
Graupera M, Guillermet-Guibert J, Foukas LC, Phng L-K, Cain RJ, Salpekar A et al (2008) Angiogenesis selectively requires the p110α isoform of PI3K to control endothelial cell migration. Nature 453(7195):662–6
Engelman JA, Luo J, Cantley LC (2006) The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat Rev Genet 7:606–619
Cook KM, Figg WD (2010) Angiogenesis inhibitors: current strategies and future prospects. CA Cancer J Clin 60(4):222–43
Karar J, Maity A (2011) PI3K/AKT/mTOR pathway in angiogenesis. Front Mol Neurosci 4:51
Fitzgibbon C, Ihmaid S, Al-Rawi J, Meehan-Andrews T, Bradley C (2013) Chemo-sensitisation of HeLa cells to etoposide by a benzoxazine in the absence of DNA-PK inhibition. Investig New Drugs 31(6):1466–75
Abcam. Human Angiogenesis Antibody Array-Membrane (23 Target) 2014 Available from: http://www.abcam.com/human-angiogenesis-antibody-array-membrane-23-targets-ab169808.html
Abcam. Human Angiogenesis Antibody Array - Membrane (20 Targets) 2014 Available from: http://www.abcam.com/human-angiogenesis-antibody-array-membrane-20-targets-ab134000.html
Folkman J (2007) Angiogenesis: an organising principle for drug discovery? Nat Rev Drug Discov 6:273–286
Samant RS, Shevde LA (2011) Recent advances in anti-angiogenic therapy of cancer. Oncotarget 2(3):122–134
Xue Y, Li N-L, Yang J-Y, Chen Y, Yang L-L, Liu W-C (2011) Phosphatidylinositol 3′-kinase signaling pathway is essential for Rac1-induced hypoxia-inducible factor-1α and vascular endothelial growth factor expression. Am J Physiol Heart Circ Physiol 300(6):H2169–H76
Nutley BP, Smith NF, Hayes A, Kelland LR, Brunton L, Golding BT et al (2005) Preclinical pharmacokinetics and metabolism of a novel prototype DNA-PK inhibitor NU7026. Br J Cancer 93(9):1011–8
Ihmaid SK, Al-Rawi JMA, Bradley CJ, Angove MJ, Robertson MN (2012) Synthesis, DNA-PK inhibition, anti-platelet activity studies of 2-(N-substituted-3-aminopyridine)-substituted-1,3-benzoxazines and DNA-PK and PI3K inhibition, homology modelling studies of 2-morpholino-(7,8-di and 8-substituted)-1,3-benzoxazines. Eur J Med Chem 57:85–101
Dong Z, Cheng Y, Zhao J, Su L, Zhao B, Zhang Y et al (2010) Discovery of a benzoxazine derivative promoting angiogenesis in vitro and in vivo. J Cell Physiol 223(1):202–8
Mannell H, Hammitzsch A, Mettler R, Pohl U, Krotz F (2010) Suppression of DNA-PKcs enhances FGF-2 dependent human endothelial cell proliferation via negative regulation of Akt. Cell Signal 22(1):88–96
Morrison R, Belz T, Ihmaid S, Al-Rawi JA, Angove M (2014) Dual and/or selective DNA-PK, PI3K inhibition and isoform selectivity of some new and known 2-amino-substituted-1,3-benzoxazines and substituted-1,3-naphthoxazines. Med Chem Res 24:1–12
Conflict of interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Rawi, S., Meehan-Andrews, T., Bradley, C. et al. Novel benzoxazines as inhibitors of angiogenesis. Invest New Drugs 33, 45–52 (2015). https://doi.org/10.1007/s10637-014-0172-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-014-0172-8