Abstract
Purpose
To describe vitamin A deficiency using multimodal functional visual assessments and imaging.
Methods/Case
A 50-year-old female with past medical history significant for Roux-en-Y gastric bypass surgery complained of nyctalopia and “yellowing” of vision.
Results
Vitamin A levels were noted to be < 0.06 mg/L (normal 0.3–0.12 mg/L). Fundus examination was notable for peripheral yellow punctate lesions, superior arcuate defects on HVF 30–2 testing, an indistinct ellipsoid zone on SD-OCT, and absent rod responses and severely reduced amplitudes for the cone photoreceptors on full-field ERG. These findings resolved with initiation of parenteral vitamin A supplementation.
Conclusion
This report documents an example of vitamin A deficiency in the developed world. We aim to provide a comprehensive description of clinical examination and multimodal imaging findings before and after vitamin supplementation for vitamin A deficiency.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vitamin A is a critical fat-soluble compound necessary for visual function. It serves as a vital precursor of the photosensitive visual pigments in the retinal phototransduction cascade [1,2,3]. Vitamin A is also important in maintaining epithelial barriers of the conjunctiva and cornea and plays a vital role in the nourishment of the retinal pigment epithelium [4, 5]
Vitamin A deficiency is more common in developing countries, especially in Africa and South-East Asia, due to chronic malnutrition. The most severe effects are seen in young children and pregnant women [6]. It remains rare in developed countries in the absence of food insecurity, nutritional deficiency, and dietary restrictions. However, in the context of the current obesity epidemic, patients are opting for bariatric surgeries and this has led some patients to develop malabsorption and vitamin deficiencies [7, 8].
Ocular manifestations of vitamin A deficiency include conjunctival and corneal xerosis, rod photoreceptor dysfunction with associated nyctalopia, and retinopathy [9]. Nyctalopia is one of the earliest signs of vitamin A deficiency associated with decreased rhodopsin levels and rod function. Fundus findings in vitamin A have been described as white deposits in the mid-periphery [9]. Classic findings of vitamin A deficiency have been documented using full-field electroretinogram (full-field ERG). These include reduced scotopic responses, variably depressed photopic responses secondary to cone dysfunction, and raised thresholds of rods and cones on dark adaptation [10]. Treatment for vitamin A deficiency includes oral, intravenous (IV), and intramuscular (IM) supplements. Recently, a sublingual formulation that sidesteps poor enteric absorption has become available [11].
In this report, we present a case of a patient who underwent Roux-en-Y gastric bypass surgery to assist with weight loss. The patient subsequently developed vitamin A deficiency with retinal manifestations. While multimodal imaging cases of vitamin A deficiency have previously been published in the literature, this report demonstrates multimodal visual function assessments and imaging at initial presentation as well as resolution of retinal findings at subsequent follow-up visits after vitamin A supplementation [12]. This case adds to our understanding of the findings of treatable vitamin A deficiency, a diagnosis not often encountered in the developed world.
Case presentation
A 50-year-old female with past medical history significant for morbid obesity and Roux-en-Y gastric bypass surgery, type II diabetes mellitus, chronic kidney disease secondary to focal nephritis, and peripheral vascular disease presented for retinal consultation with three weeks of “yellowing” of vision, nyctalopia, and flashes of light in both eyes. Her past ocular history was significant for laser-assisted keratomileusis (LASIK) bilaterally and dry eye syndrome.
At initial presentation, the patient’s visual acuity was 20/20 in the right eye and 20/25 in the left eye. Her examination was significant for punctate epithelial erosions of both eyes. On dilated examination, she had vascular attenuation of the right eye with scattered yellow flecks in all quadrants in both eyes (Fig. 1A). Mottling of the retinal pigment epithelium was noted.
Fundus photographs of right and left eyes, respectively. Pre-treatment (A), one month post-treatment (B), and six months post-treatment (C) with parenteral vitamin A. Note multiple yellow-white punctate dots (pink box) in the mid-periphery in both eyes with a near-confluent appearance. The left column (pink arrow) demonstrates inset higher magnification photographs of the temporal peripheral findings in the right eye. One month after vitamin A therapy with less prominent punctate lesions (B). Six months after initiating vitamin A therapy there was near complete resolution of yellow-white punctate lesions in both eyes (C)
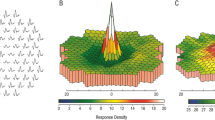
Humphrey visual field (HVF) 30–2 testing demonstrated superior arcuate defects of both eyes (Fig. 2A). Spectral domain OCT (SD-OCT) demonstrated a diffusely blurred ellipsoid zone (EZ) of both eyes (Fig. 3A). Initial full-field ERG showed reduced photopic responses and near-absent scotopic responses (Fig. 4, left column).
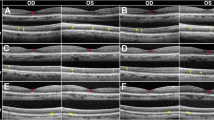
Optical coherence tomography of right and left eyes, respectively: prior to treatment (A), one month post-treatment (B), and six months post-treatment (C). Note the transition from a less distinct ellipsoid zone (EZ) at presentation to a more distinct EZ by six months post-treatment highlighted by the yellow arrow. The external limiting membrane is highlighted with the red arrow, and the retinal pigment epithelium layer is highlighted with the green arrow
Serial full-field ERG pre-treatment (left column), one month post-treatment (middle column), and six months post-treatment (right column). Absent rod responses and severely reduced amplitudes for the cone photoreceptors were noted. One month after treatment, improvement in amplitudes was observed, with further restoration of rod and cone responses at six months. ERG signals were extracted from noisy records due to vigorous lid clenching by means of signal averaging. Amplitude and time scales are provided
Serum vitamin A level was drawn at her initial presentation which yielded a value of < 0.06 (nl 0.3 – 1.2 mg/L). The patient was started on intramuscular injections of vitamin A.
One month and six months after treatment, the patient’s fundus abnormalities resolved (Fig. 1B-C); the superior defects on visual field testing diminished (Fig. 2B-C); the EZ became more distinct on SD-OCT (Fig. 3B-C); and the patient’s photopic and scotopic responses normalized on full-field ERG (Fig. 4, middle and right column). The patient was placed on sublingual vitamin A supplementation and maintained normal levels of vitamin A.
Fundus autofluorescence images were normal at presentation and remained unchanged throughout the treatment course (Supplemental Fig. 1).
Discussion
A recent study based on body mass index within the USA found that 65% of adults are overweight and 30% are obese. In response to the obesity epidemic, there has been a rise in the number of bariatric surgeries performed [14]. Those patients who undergo biliopancreatic diversion and Roux-en-Y gastric bypass surgery, as our patient had, are at higher risk of deficiencies in fat soluble vitamins (A, D, E, and K) and vitamin B12 compared to those with restrictive procedures such as gastric banding or gastric sleeve surgery [13]. The incidence of vitamin A deficiency after Roux-en-Y gastric bypass has been reported as high as 11% [14]. Vitamin A deficiency can lead to a well-known array of ocular complications, including nyctalopia, xerosis with Bitot spots, and xanthopsia. Studies have estimated approximately 3% of patients undergoing bariatric surgery subsequently report nyctalopia [15].
Retinal manifestations of vitamin A deficiency—most notably the punctate deposits on peripheral examination—have been documented and are consistent with this case [12, 16, 17]. Here, a careful history and simple laboratory testing showed deficient vitamin A levels and was sufficient to reveal the underlying cause of the patient’s symptoms. The ophthalmologic manifestations of hypovitaminosis A are well documented in the literature. With this case, we demonstrate the recovery of symptoms, visual function examination findings, and imaging findings with the implementation of vitamin supplementation.
Some limitations of this case are that the presence of noise in the post-treatment ERGs, particularly in the light-adapted 3.0 and 30 Hz flicker, which make it difficult to convincingly appreciate ERG changes before and after treatment. (ERG signals were successfully extracted using extensive signal averaging.) In addition, it is possible that the resolution of the superior visual field defects seen on the pre-treatment HVF 30–2 may reflect an initial learning curve or lid artifact as opposed to true recovery of visual field defects.
We highlight a case of vitamin A deficiency in the developed world, an entity which may continue to become more common as bariatric surgery remains an option for the treatment of recalcitrant obesity. We detail the symptoms, visual field and ERG examination findings, and findings on multimodal imaging to raise awareness among clinicians in developed countries where vitamin A deficiency is traditionally rarely seen.
References
Liou GI, Bridges CDB, Alvarez RA, Gonzalez-Fernandez F (1982) Vitamin a transport between retina and pigment epithelium—an interstitial protein carrying endogenous retinol (interstitial retinol-binding protein). Vision Res 22(12):1457–1467. https://doi.org/10.1016/0042-6989(82)90210-3
Noell WK, Albrecht R (1971) Irreversible effects of visible light on the retina: role of vitamin A. Science 172(3978):76–80. https://doi.org/10.1126/science.172.3978.76
Wolf GE (1984) Multiple functions of vitamin A. Physiol Rev 64(3):873–937. https://doi.org/10.1152/physrev.1984.64.3.873
Thompson DA, Gal A (2003) Vitamin A metabolism in the retinal pigment epithelium: genes, mutations, and diseases. Prog Retin Eye Res 22(5):683–703. https://doi.org/10.1016/s1350-9462(03)00051-x
McCullough FSW, Northrop-Clewes CA, Thurnham DI (1999) The effect of vitamin A on epithelial integrity. Proc Nutr Soc 58(2):289–293. https://doi.org/10.1017/s0029665199000403
Johnson LM, Ikramuddin S, Leslie DB, Slusarek B, Kileen AA (2019) Analysis of vitamin levels and deficiencies in bariatric surgery patients:a single-institutional analysis. Surg Obes Relat Dis 15(7):1146–1152. https://doi.org/10.1016/j.soard.2019.04.028
Bhakhri R, Ridder WH, Adrean S (2019) Case report: delayed vitamin a retinopathy secondary to bariatric surgery. Optom Vis Sci 96(3):227–232. https://doi.org/10.1097/opx.0000000000001346
Chow CC, Mieler WF (2014) Vitamin A deficiency and xerophthalmic fundus in autoimmune hepatitis and cirrhosis. Retin Cases Brief Rep 8:164–166. https://doi.org/10.1097/ICB.0000000000000031
Anastasakis A, Plainis S, Giannakopoulou T et al (2013) Xerophthalmia and acquired night blindness in a patient with a history of gastrointestinal neoplasia and normal serum vitamin A levels. Doc Ophthalmol 126:159–162. https://doi.org/10.1007/s10633-012-9370-x
Spits Y, De Laey JJ, Leroy BP (2004) Rapid recovery of night blindness due to obesity surgery after vitamin A repletion therapy. Br J Ophthalmol 88(4):583–585. https://doi.org/10.1136/bjo.2003.022459
Singer JR, Bakall B, Gordon GM, Reddy RK (2016) Treatment of vitamin A deficiency retinopathy with sublingual vitamin A palmitate. Doc Ophthalmol 132(2):137–145. https://doi.org/10.1007/s10633-016-9533-2
Aleman TS, Garrity ST, Brucker AJ (2013) Retinal structure in vitamin A deficiency as explored with multimodal imaging. Doc Ophthalmol 127(3):239–243. https://doi.org/10.1007/s10633-013-9403-0
Clements RH, Katasani VG, Palepu R et al (2006) Incidence of vitamin deficiency after laparoscopic Roux-en-Y gastric bypass in a university hospital setting. Am Surg 72(12):1196–1204. https://doi.org/10.1177/000313480607201209
Lupoli R, Lembo E, Saldalamacchia G, Avola CK, Angrisani L, Capaldo B (2017) Bariatric surgery and long-term nutritional issues. World J Diabetes 8(11):464–474. https://doi.org/10.4239/wjd.v8.i11.464
Scopinaro N, Adami GF, Marinari GM, Gianetta E, Traverso E, Friedman D, Camerini G, Baschieri G, Simonelli A (1998) Biliopancreatic diversion. World J Surg 22(9):936–946. https://doi.org/10.1007/s002689900497
Patel S (2017) Posterior segment findings in vitamin A deficiency. Ophthalmol Retina 1(2):173. https://doi.org/10.1016/j.oret.2016.10.015
Berkenstock MK, Castoro CJ, Carey AR (2020) Outer retina changes on optical coherence tomography in vitamin A deficiency. Int J Retina Vitreous 6:23. https://doi.org/10.1186/s40942-020-00224-1
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
All procedures performed in this study involving human participants were approved by and in accordance with the ethical standards of the New York University Langone Health Institutional Review Board (NYU IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all participants or their parents prior to examination.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of NYU Langone Health and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Verbal and written consent was obtained from the patient.
Ethical approval
Institutional Review Board exemption was obtained given this was a retrospective case report. We certify that this report was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Verbal and written informed consent was obtained from the patient.
Consent to participate
Not applicable as this was a retrospective case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, S., Pandit, S., Patil, S.A. et al. Documentation of recovery from vitamin A deficiency-related retinopathy via multimodal imaging and electroretinogram testing. Doc Ophthalmol 145, 157–162 (2022). https://doi.org/10.1007/s10633-022-09888-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-022-09888-6