Abstract
Purpose
The electroretinogram (ERG) has proven to be useful in the evaluation and monitoring of patients with posterior uveitis. ERG oscillatory potentials (OPs) are sometimes reduced in many uveitic eyes with otherwise grossly normal ERG responses. This study compares ERG parameters, including OPs, between patients with birdshot chorioretinopathy, other posterior uveitis, and controls.
Methods
This was a retrospective case–control study. Sixty-four patients seen at a clinical practice had a total of 93 visits during which ERG was performed on both eyes. ERG data from 93 age-matched controls were also collected. Root-mean-squared (RMS) energy of the OPs was calculated using Fourier analysis for 88 patients and 88 age-matched controls for whom complete data were available. Photopic flicker amplitudes, photopic flicker latencies, scotopic b-wave amplitudes, and OP RMS values were compared between patients and controls. Diagnostic performance was assessed using receiver operating characteristic (ROC) curves.
Results
The mean ages of patients and controls were 55.9 ± 10.8 (SD) years and 55.1 ± 11.5, respectively. 83% of the patients had a diagnosis of BCR. The mean OP RMS value was significantly different in patients (15.6 µV ± 9.7 µV) versus control eyes (33.0 µV ± 12.7 µV), p < 0.001. Area under the ROC curves (AUROC) was 0.75 for photopic flicker amplitudes, 0.77 for photopic flicker latencies, 0.72 for scotopic b-wave amplitudes, and 0.88 for OP RMS. AUROC was significantly different between OP RMS and photopic flicker amplitudes (p < 0.001), between OP RMS and flicker latencies (p = 0.0032), and between OP RMS and scotopic b-wave amplitudes (p < 0.0001).
Conclusion
Analysis of OPs shows greater sensitivity and specificity in the diagnosis and evaluation of patients with birdshot chorioretinopathy than photopic and scotopic ERG amplitudes and photopic flicker latencies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Electroretinography is widely used in the diagnosis and monitoring of ocular disease [1]. It is an objective test that can detect abnormalities even in the absence of findings on fundus examination. With the use of selected stimulus conditions, responses from specific cells of the retina can be measured [2]. The ERG responses are recorded in the light- and dark-adapted states in response to flashes of red, blue, and white stimuli of different intensities [3].
In recent years, the ERG has been a tool that has proven to be useful in the evaluation and monitoring of uveitis [2, 4]. This is especially true in birdshot chorioretinopathy (BCR), a subtype of uveitis characterized by progressive deterioration of retinal function despite only mild loss of visual acuity in the early stages [5]. It is rare, often bilateral, strongly associated with the HLA-A29 haplotype, and accounts for 6% of posterior uveitis cases [2, 6, 7]. The diagnosis and management of BCR remain a challenge, since in many cases the inflammation is mild. The retina may develop diffuse pigmentary degeneration over time in a slow and chronic course [5, 6]. Reduction of visual acuity occurs late; by the time symptoms manifest and treatment begins, patients may be in relatively advanced stages of the disease with limited treatemtn benefit [4, 6, 8]. ERG is a promising tool that may aid in the earlier diagnosis and monitoring of treatment response in BCR. A unique finding in BCR, not seen in other types of uveitis, is selective b-wave amplitude reduction [2]. 30 Hz flicker implicit time and bright flash scotopic amplitudes have also been shown to be sensitive indicators of BCR and useful in tracking treatment response [9].
A few investigators have studied ERG parameters in BCR specifically. These studies have demonstrated that early BCR eyes demonstrated loss of oscillatory potentials (OPs) and b-wave amplitudes, while a-waves are relatively preserved until the later stages of disease [10, 11]. Tzekov et al. performed a comprehensive literature review on the use of ERG in BCR, which confirmed that light-adapted 30 Hz flicker response peak time has been thought to be the most sensitive parameter in disease monitoring and has become an important outcome measure in clinical trials of drug effectiveness [12]. This review did not specifically consider oscillatory potentials. The mechanism behind the loss of 30 Hz flicker amplitude is still unknown. Other studies investigating the best ERG parameter for BCR diagnosis and evaluation have been inconclusive [4].
Oscillatory potentials (OPs) are small, high-frequency wavelets superimposed on the b-wave, and their reduction has been observed to reflect disturbances in the retinal microcirculation [13,14,15]. Our clinical observations over the past few decades have suggested that the OPs, which may be independent from other components of the ERG, including the a-wave and b-wave, are often reduced in many eyes with grossly normal ERG responses, particularly in cases of uveitis (Fig. 1). This has not been confirmed in the published literature, in part due to the technical difficulties with measuring the multiple oscillations [16].
Comparison of raw DA 3.0 waveforms (top row) and filtered oscillatory potentials (bottom row) from a control patient (left) and patient with birdshot chorioretinopathy (right). Though a-waves and b-waves are comparable in amplitude, oscillatory potentials are reduced by more than 50% in the birdshot chorioretinopathy patient
The OPs are known to arise in the innermost retinal layers, but of course this electrical activity is activated by neural events which arise from the photoreceptors and are transmitted by the retinal interneurons from the outer retina to the inner retina. It is thus to be expected that impairment of outer layer or intermediate layer retinal function would also impair generation of the oscillatory potentials. This raises the possibility that selective injury to the inner neurons which generate the OPs might be better identified after normalization of the OP signal amplitudes by the amplitude of the underlying b-waves or flicker amplitudes.
The goal of this study is to compare ERG parameters, including OPs, in eyes with birdshot chorioretinopathy and controls by means of a retrospective chart review. A smaller cohort of patients with other forms of posterior uveitis (“non-BCR”) was also studied.
Our main tool for comparing the diagnostic effectiveness of the various ERG parameters is the use of ROC (“receiver operating characteristic”) analysis. This procedure plots the sensitivity of a diagnostic test against the “false-positive rate” (1—specificity), parametrically over the range of threshold values of the test parameter. In such a plot, the curve for a test which randomly classified the subjects would fall along the diagonal line from lower left to upper right. The curves for tests with predictive value better than chance bend toward the upper left corner of the plotting region. The area under the ROC curve (AUROC) serves as an overall measure of the diagnostic performance of the test—larger values indicate better performance. The parameter value for which the curve most nearly approaches the upper left corner of the plotting region is effectively the optimal cutoff value for the test parameter and may be determined by the largest value of the “Youden index” (sensitivity + specificity − 1).
Methods
The study design is a retrospective review of patients drawn from the referral practice of one of the authors (SEB) between 2003 and 2018. This retrospective study adhered to the tenets of the declaration of Helsinki and was approved by the NYU Langone IRB.
Study population
Inclusion criteria include a clinical diagnosis of birdshot chorioretinopathy, or other form of posterior uveitis, and at least one ERG with photopic flicker and scotopic b-wave recordings. Age-matched controls were patients who presented for ERG testing between 2003 and 2018 who had ERG studies with normal photopic and scotopic a-wave and b-wave amplitudes, and normal 30 Hz flicker latencies, according to the age-specific norms furnished by Diagnosys LLC for the ISCEV standard ERG protocol as implemented on the Espion electrodiagnostic system. In order to prevent circularity, oscillatory potential amplitudes were not a criterion for inclusion or exclusion in the control cohort. Clinical information collected on patients and controls included demographics, Snellen visual acuity, and ERG. Snellen visual acuities were converted to logarithm of the minimum angle of resolution (logMAR) scores to facilitate statistical analysis.
Electroretinography (ERG)
ERGs were recorded according to the International Society for Clinical Electrophysiology of Vision (ISCEV) protocol [16], using ERG-jet contact lens electrodes and a Diagnosys Espion electrodiagnostic system for all eyes. (An Espion 2 system was used prior to 2011, which was subsequently replaced with an Espion 3 system. The ERG protocols were identical with the two instruments.) The pupils were dilated fully with topical tropicamide 1% and phenylephrine hydrochloride 2.5%. Photopic recordings were performed first, generally after indirect ophthalmoscopy, which assured adequate light adaptation. Photopic background illumination was 30 cd/m2. After photopic single-flash and 30 Hz flicker recordings, patients were dark-adapted for 20 min. Order of testing was thus: LA 3, LA 30 Hz flicker, [dark adaptation for 20 min], DA 0.01, DA 3. Oscillatory potentials were extracted from the DA 3 waveforms (see below)—they were not recorded separately. ERG results were anonymized before further analysis.
Oscillatory potential (OP) analysis
To analyze the oscillatory potentials from the ERG recordings of each eye, a custom computer program, “OPAnalyzer,” updated using MATLAB software (MathWorks Inc., Natick, MA, USA), was used (Fig. 2). OPAnalyzer processes a single ERG waveform at a time under operator supervision. Using the program, the user first crops the waveform if necessary to avoid noise artifacts (such as blinks), as shown in Fig. 3. In most cases, the filtered OP waveform from the Diagnosys software was used (Fig. 4), but when this was not available, the original dark-adapted scotopic b-wave data were used. In this case, the raw waveform was filtered with a simple two-stage RC filter in order to partially suppress the power of the a- and b-waves to allow visual inspection of the energy peak containing the power in the oscillatory potentials [13]. In most cases the high-pass cutoff of this filter was set to 75 Hz [17], but this could be adjusted by the user (Fig. 5). (Filtered OP waveforms were available for all the control subjects, and all but three of the uveitis patients.) Once the frequency band of the OP peak was identified, the power spectrum of the original, unfiltered waveform was integrated across this range of frequencies to obtain the total power of the OPs in the ERG waveform (Plancherel’s Theorem), as shown in Fig. 6. The OPAnalyzer program allows the user to refine the limits of integration to more accurately encompass only the peak representing the OPs. The square root of the total power represents the root-mean-squared (RMS) amplitude of the OPs, with units measured in microvolts.
User interface of the OPAnalyzer program. Waveforms are imported as files exported by electrodiagnostic systems, or through the Windows Clipboard. Imported waveform is shown in the panel at upper left, normalized so as to be easily visualized. The power spectrum of the waveform, normalized to fit into the window for viewing, is shown in the lower panel. Buttons on the right allow for importing new waveforms, selecting a sub-interval of the waveform timebase to omit blink artifacts, etc., filtering of waveform with a high-pass filter to suppress a- and b-waves for better visualization of the oscillatory potentials and identification of the optimal limits of integration of spectral peak corresponding to the energy in the oscillatory potentials, and recovery of the original waveform. Integrated spectral power and the RMS amplitude value are shown in the windows at lower right
Removal of blink artifact. Original filtered oscillatory potential waveform as imported by the OPAnalyzer program is shown at upper left. Note blink artifact beginning at approximately 100 ms after stimulus flash. Power spectrum at lower left is visibly contaminated by the power of the blink artifact event. After upper limit of recording interval has been adjusted to 70 ms, selected portion of waveform, with blink artifact omitted, is shown at upper right. Corresponding power spectrum is shown at lower right, free of blink artifact contamination. RMS amplitude reflects this correction
Isolation of the oscillatory potentials by the Diagnosys Espion 3 OP filter. Normal scotopic DA 3 waveform is shown at upper left as imported into the OPAnalyzer program. The power spectrum, shown at lower left, is dominated by the power in the a- and b-waves, to the extent that the power spectrum peak of the oscillatory potentials cannot be seen at this scale. The oscillatory potential waveform, as isolated by the Diagnosys Espion 3 OP digital filter, is shown at upper right. After application of this filter, with a nominal pass-band from 75 to 300 Hz, the power spectrum, shown at lower right, clearly shows the spectral peak corresponding to the energy in the oscillatory potentials. A small amount of residual power from the a- and b-waves is seen at lower frequencies
Isolation of the oscillatory potentials using a two-stage RC filter. In a few instances, waveforms filtered using the Diagnosys Espion 3 OP filter were not available. For these waveforms, a two-stage RC digital filter was applied, usually with a nominal high-pass cutoff of 75 Hz. This sufficiently suppressed the spectral contributions of the a- and b-waves to allow inspection of the OP energy peak to allow accurate setting of the limits of integration for calculation of the total energy in the oscillatory potentials using the original, unfiltered power spectrum
Comparison of two-stage RC filter with decimation of unfiltered waveform. The effect of the two-stage RC filter as illustrated in Fig. 5 is shown in the left-hand panel and may be compared with the inverse Fourier transform of the frequency band from 100 to 200 Hz of the original unfiltered waveform, shown in the right-hand panel. The RC filter reduces the waveform amplitudes and the RMS value by about 21%. For this reason, RMS amplitudes were calculated from the unfiltered power spectrum, using limits of integration as determined by inspection of the filtered power spectrum
Normalized OP amplitudes were obtained as the quotient of the OP RMS amplitudes divided by the 30 Hz flicker amplitudes and b-wave amplitudes, respectively.
Outcome measures and statistical analysis
The ERG parameters of interest in this study were the photopic (light-adapted) 30 Hz flicker amplitudes, 30 Hz flicker peak time latency, scotopic (dark-adapted) 3.0 cd s/m2 b-wave amplitudes, and calculated OP RMS amplitudes as determined using OPAnalyzer. 30 Hz flicker amplitudes were measured using the cursoring system provided in the Espion 3 software. Measurements were made peak-to-trough of a single typical oscillation, usually the 4th peak, unless it was necessary to use a different peak to minimize the effects of unsteadiness of the waveform baseline. Latencies were measured from the 4th peak in the wavetrain, referenced to the stimulus marker at 99 ms. These were compared between patient and control eyes. The results were further stratified between BCR and non-BCR uveitis patients. The diagnostic performance of the ERG parameters was evaluated by comparison of the area under the receiver operating characteristic (ROC) curves. Optimal threshold values were determined as those ERG parameter values corresponding to the maximal Youden index for each parameter.
Analyses were based on data from the right eye of each patient, to avoid the statistical difficulties created by the lack of independence of the two eyes from a single patient. Statistical comparisons of ERG parameters between patients and controls were performed using two-tailed, unpaired t tests. ROC curves were generated using the NCSS statistical software package. Comparison of ROC curves was based on a z test according to the method of McClish [18]. ERG data from patients with repeat visits were treated as separate events, to allow for the possibility of deterioration or recovery of retinal function with progression of disease or therapy.
Results
Patient characteristics
A total of 64 patients met the inclusion criteria. Seventeen of these patients had repeat visits (mean 1.7 repeat visits, range 1–6). ERG data from the 93 visits were collected, along with data from 93 age-matched controls. Five visits did not have the complete set of parameters recorded, so a total of 88 visits were analyzed and compared with the 88 age-matched control subject studies previously identified for these visits.
The mean ages of patients and controls during the ERG visits were 55.9 ± 10.8 (SD) years and 55.1 ± 11.5, respectively. Of the 88 patient studies available for analysis, 73 studies (83%) were of patients who had the diagnosis of birdshot chorioretinopathy (Table 1).
ERG
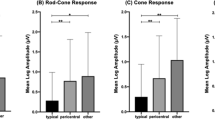
Photopic flicker amplitudes (30 Hz), flicker latencies, dark-adapted scotopic b-wave amplitudes, and OP RMS values for patient and control eyes are shown in Table 2. Results were significantly different between patients and controls for all comparisons, except for scotopic b-wave amplitudes and 30 Hz flicker latency between non-BCR posterior uveitis eyes and controls.
The mean OP RMS value was significantly different in patients (15.6 µV ± 9.7 µV) versus control eyes (33.0 µV ± 12.7 µV), p < 0.001. The significance persisted when patient eyes were stratified by diagnosis of BCR vs non-BCR posterior uveitis. OP RMS values showed little dependence on age in patients or controls (Fig. 7).
As mentioned above, an attempt was made to adjust the OP RMS values for the overall integrity of the outer and intermediate retinal layers by normalizing the OP amplitudes by dividing the RMS values by the photopic flicker amplitudes and scotopic b-wave amplitudes. This did not improve the results; moreover, these normalizations obliterated the significance between non-BCR posterior uveitic eyes and controls. Normalized OP RMS values were still significantly different between BCR eyes and controls (Table 2).
Visual acuity
The mean logMAR visual acuity in all patient eyes was 0.26 ± 0.37 (approximately Snellen 20/36). In BCR eyes the mean logMAR visual acuity was 0.19 ± 0.30 (roughly Snellen 20/30), while in non-BCR posterior uveitic eyes the mean logMAR visual acuity was 0.57 ± 0.53 (roughly Snellen 20/75). The mean logMAR visual acuity in control eyes was 0.44 ± 0.73 (roughly Snellen 20/55). These results are shown in Table 3.
Comparison of OP RMS values with visual acuity in the patient groups showed a stronger correlation in patient eyes than in control eyes (Fig. 8). The correlation coefficient was slightly stronger for BCR eyes (R = − 0.375) than for non-BCR posterior uveitic eyes (R = − 0.366). The correlation coefficient for control eyes was insignificant, with R = 0.054.
ROC analysis of ERG parameters
Figure 9 shows receiver operating characteristic (ROC) curves derived by plotting the proportion of patient eyes flagged as abnormal at a given ERG parameter value (“sensitivity”) against the proportion of control eyes flagged at the same criterion value (i.e., false-positive rate). ROC curves are shown for the four ERG outcome variables observed in this study: OP RMS values, scotopic DA 3 b-wave amplitudes, photopic 30 Hz flicker amplitudes, and photopic 30 Hz flicker latencies. Curves are plotted separately for the entire cohort of patients, for patients with birdshot chorioretinitis only, and for patients with non-BCR posterior uveitis.
ROC curves are shown for each ERG response parameter, OP RMS values, scotopic DA 3 b-wave amplitudes, 30 Hz flicker amplitudes, and 30 Hz flicker latency. Curves which more closely approximate the right angle at upper left of each plot indicate better diagnostic performance. ROC curves are plotted separately for the entire cohort of patients, patients with birdshot chorioretinitis, and patients with non-BCR posterior uveitis
Results of the ROC analysis are shown in Table 4. All ERG parameters performed significantly better than chance (p < 0.001) for the detection of disease, with the exception of the scotopic b-wave amplitudes and 30 Hz flicker latency, which failed to reach significance for non-BCR uveitic eyes. Table 5 shows the paired comparisons between ROC curves in terms of the area under the ROC curves (“AUROC”). OP RMS values performed better than scotopic b-wave amplitudes and 30 Hz flicker amplitudes and 30 Hz flicker latencies for all patient eyes and for eyes with birdshot chorioretinitis. Comparisons for non-BCR eyes were not statistically significant except for OP RMS vs scotopic DA 3 b-wave amplitudes (OP RMS better) and DA 3 b-wave amplitudes versus 30 Hz flicker amplitudes (30 Hz flicker amplitudes better).
We were unable to confirm better ROC performance for 30 Hz flicker latencies compared with DA 3 b-wave amplitudes or 30 Hz flicker amplitudes, as has been suggested in earlier studies.
Suggested cutoff values for separating uveitis patients from controls on the basis of these ERG measurements are given by the cutoff values at greatest Youden index shown in Table 4. The suggested criterion values for our OP RMS values are 21.33 µV for our entire cohort and for the subset of patients with non-BCR posterior uveitis and 17.05 µV for the cohort of patients with birdshot chorioretinitis. The cutoff value for 33 Hz flicker latency was 31 ms for the entire cohort of patients, as well as for patients with birdshot chorioretinitis, which is similar to the usual threshold for 30 Hz flicker latency (33 ms) commonly used for ERG interpretation.
Discussion
The purpose of this study was to retrospectively review the diagnostic capabilities of ERG parameters, including oscillatory potentials, in a dataset of ERG recordings of patients with posterior uveitis. The impact is twofold. First, our results show that the OPs are a somewhat stronger indicator of disease than scotopic or photopic ERG amplitudes or 30 Hz flicker latencies. Second, we demonstrate a robust technique for isolating and quantifying the OPs, a challenge that has been the subject of debate in previous years. We were unable to confirm a similar diagnostic utility for OP RMS values in our small cohort of non-BCR uveitis patients.
Our main outcome measure is the use of ROC analysis, which allows for the simultaneous assessment of both sensitivity and specificity of a diagnostic test, and also suggests optimal cutoff values for distinguishing between affected subjects and unaffected individuals. This approach has not appeared in previous studies of ERG parameters in uveitis patients, which may explain some of the differences between our conclusions and those of previous authors.
For this project, a novel, custom computer program was utilized to derive the OP wave train and measure its energy by means of Fourier analysis. To our knowledge, this is the first study of its size that confirms that OP analysis may be a particularly useful ERG parameter in the diagnosis and monitoring of patients with posterior uveitis. This is particularly true for patients with BCR, in whom visible indications of active inflammation and visual acuity are known to be unreliable [6]. This discrepancy between visual acuity and our direct measures of retinal function in BCR and other forms of uveitis is well reflected in our dataset.
Our OP analysis showed ROC characteristics superior to measurements of the latency of the 30 Hz flicker response peaks. Comparison with previous studies is difficult: most previous comparative studies of ERG parameters in birdshot chorioretinitis have monitored responses to therapy rather than sensitivity and specificity in distinguishing between birdshot patients and controls, and none have previously used ROC analysis. In contrast with previous studies, our ROC analysis did not find 30 Hz flicker latencies superior to ERG amplitudes in the detection of BCR.
Three decades ago, Priem et al. undertook a study of 16 patients with BCR that revealed that the origin of disease was the inner retina, marked by reduction of b-wave amplitudes and OPs, along with preservation of a-waves [10]. Though the OPs have long been known to be reduced in uveitis, there has been considerable debate over the years about how to best measure them [16, 17]. In many previous studies, the preferred method has been to apply high-pass filtering to better visualize the OP peaks and then to sum the trough-to-peak amplitude of at least the 3 major peaks [16]. Gauthier et al. pointed out the importance of choosing a filtering cutoff and technique with care, since these choices exert a large influence on the OP measurements [17].
We have addressed many of the concerns about how to best isolate and measure OPs using the novel OPAnalyzer program, which may provide a more robust approach. The OPAnalyzer displays each ERG waveform and allows a trained user to quickly adjust the boundaries of the OPs to omit from the analysis any spurious waveform events, such as blink artifacts, and apply the optimal limits of integration so that the OPs are maximally isolated from the a- and b- waves. This is a more accurate method than simply applying a standard filter to all the data, which would lead to over-attenuation of OP waveforms in some eyes and inadequate signal suppression from a- and b- waves in other eyes. The Fourier technique also eliminates the need to resolve the inevitable uncertainty as to whether or not small oscillations at the beginning and the end of the OP wavetrain should be included in a sum-of-oscillations calculation. Finally, the Fourier technique is not subject to degradation by 50 or 60 Hz interference from electrical power sources (“line noise” or “mains hum”), as these signals fall outside the power band of the oscillatory potentials.
ERG data can be noisy, and using FFT to analyze OPs captures all the ERG activity regardless of when it occurs relative to the stimulus. This was pointed out by Gauvin et al. in their recent study that uses continuous wavelet transforms to analyze OPs, which adds temporal resolution and allows for selection of only “evoked” oscillations and minimizes noise contaminants [19]. Though one can argue that the FFT analysis we used in this study does not specifically address the timing of observed frequency components, the ERG waveforms in our study were truncated using the OPAnalyzer to focus solely on the waveform segment where the OPs are located, also having the effect of minimizing noise.
A limitation of this study is that it is a retrospective data analysis, so several factors could not be controlled for, such as comorbid conditions or therapeutic interventions received, if any, prior to ERG. Future studies using OP outcomes taking these factors into account appear warranted. Longitudinal studies monitoring patient’s response to treatment would also be useful in assessing the utility of OP analysis in monitoring the benefits and toxicity of uveitis treatment.
References
Brown TK (1968) The electroretinogram: its components and their origins. Vis Res 8:633–677
Moschos MM, Gouliopoulos NS, Kalogeropoulos C (2014) Electrophysiological examination in uveitis: a review of the literature. Clin Ophthalmol 8:199–214
Perlman I (1983) Relationship between the amplitudes of the b wave and the a wave as a useful index for evaluating the electroretinogram. Br J Ophthalmol 67(7):443–448
Sobrin L, Lam BL, Liu M, Feuer WJ, Davis JL (2005) Electroretinographic monitoring in birdshot chorioretinopathy. Am J Ophthalmol 140(1):52.e18–52.e51
Ryan SJ, Maumenee AE (1980) Birdshot retinochoroidopathy. Am J Ophthalmol 89(1):31–45
Oh KT, Christmas NJ, Folk JC (2002) Birdshot retinochoroiditis: long term follow-up of a chronically progressive disease. Am J Ophthalmol 133(5):622–629
Wakefield D, Chang JH (2005) Epidemiology of uveitis. Int Ophthalmol Clin 45(2):1–13
Rothova A, Berendschot TTJM, Probst K, van Kooij B, Baarsma GS (2004) Birdshot chorioretinopathy: long-term manifestations and visual prognosis. Ophthalmology 111(5):954–959
Zacks DN, Samson MC, Loewenstein J, Foster SC (2002) Electroretinograms as an indicator of disease activity in birdshot retinochoroidopathy. Graefe’s Arch Clin Exp Ophthalmol 240(8):601–607
Priem HA, De Rouck A, De Laey J-J, Bird AC (1988) Electrophysiologic studies in birdshot chorioretinopathy. Am J Ophthalmol 106(4):430–436
Hirose T, Katsumi O, Pruett RC, Sakaue H, Mehta M (1991) Retinal function in birdshot retinochoroidopathy. Acta Ophthalmol 69(3):327–337
Tzekov R, Madow B (2015) Visual electrodiagnostic testing in birdshot chorioretinopathy. J Ophthalmol 2015, Article ID 680215
Speros P, Price J (1981) Oscillatory potentials. History, techniques and potential use in the evaluation of disturbances of retinal circulation. Surv Ophthalmol 25(4):237–252
Wachtmeister L (1998) Oscillatory potentials in the retina: what do they reveal. Prog Retinal Eye Res 17(4):485–521
Algvere P, Westbeck S (1972) Human ERG in response to double flashes of light during the course of dark adaptation: a fourier analysis of the oscillatory potentials. Vis Res 12(2):195–214
McCulloch DL, Marmor MF, Brigell MG et al (2015) ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol 130(1):1–12
Gauthier M, Gauvin M, Lina J-M, Lachapelle P (2019) The effects of bandpass filtering on the oscillatory potentials of the electroretinogram. Doc Ophthalmol 138:247–254
McClish DK (1989) Analyzing a portion of the ROC curve. Med Decis Making 9:190–195
Gauvin M, Lina J-M, Lachapelle P (2014) Advance in ERG analysis: from peak time and amplitude to frequency, power, and energy. Biomed Res Int 2014:246096
Funding
This study was supported in part by an unrestricted Grant to the NYU Langone Department of Ophthalmology from Research to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Medical Ethical Research Committee of the University Medical Centre Utrecht and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This was a retrospective chart review. Informed consent was not obtained from study subjects, as approved by the NYU Langone IRB.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the NYU Langone Institutional Review Board (Study Number 18-01348_CR2) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
No animals were used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, D., Nair, A., Goldberg, N. et al. Oscillatory potentials in patients with birdshot chorioretinopathy. Doc Ophthalmol 141, 293–305 (2020). https://doi.org/10.1007/s10633-020-09776-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-020-09776-x