Abstract
Purpose
The purpose of this study was to compare electroretinographic (ERG) responses of preterm schoolchildren, with and without a history of retinopathy of prematurity (ROP) with those of full-term schoolchildren by using a portable ERG device (RETeval system).
Methods
Twenty five prematurely born schoolchildren with a mean gestational age of 27 + 1/7w (range 23–30w) and a mean birth weight of 1030 g (range 580–1700 g) who were 6.9 ± 2.2 years old participated in the study (premature group). A further subdivision according to a history of ROP (ROP+ group) or its absence (ROP− group) was introduced. Twenty eight healthy full-term schoolchildren with an average age of 8.6 ± 1.9 years participated as the control group. 30-Hz flicker ERG responses were obtained, and implicit times and amplitudes were compared between the groups.
Results
30-Hz flicker ERG implicit times showed a significant difference between all three groups of children. The mean value of the implicit time in the term group was 25.76 ± 0.9 ms, whereas in the preterm ROP + group it was 28.96 ± 1.0 ms and in the preterm ROP− group it was 26.87 ± 1.5 ms. 30-Hz flicker ERG amplitudes did not show significant difference between term children and children born prematurely with or without ROP.
Conclusions
Prematurely born schoolchildren exhibit longer implicit time of the 30-Hz flicker ERG response compared to controls, suggesting a possible abnormality of the retinal cone system function. Under such circumstances, portable ERG device might be used clinically as a screening tool for retinal function evaluation in prematurely born children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immature cones and rods are already present in mid-gestation. However, they mature, migrate and differentiate well after the child is born [1]. A preterm birth affects both structural and functional characteristics of the developing human retina. Studies have confirmed structural changes of the retina of preterm infants, especially those with a history of retinopathy of prematurity (ROP) [2,3,4,5], characterized mainly by delayed photoreceptor maturation and foveal dysplasia. Visual electrophysiology plays an important role in detecting functional changes of the retina and postretinal visual pathway in the pediatric population [6]. The importance lies in its objectivity. The information obtained with electrophysiological methods is therefore very valuable in the hands of a pediatric ophthalmologist.
Electroretinographic (ERG) responses were previously used to study the functional development of photoreceptors of infants born prematurely [7,8,9]. At 35 weeks of gestation, both rod and cone responses are immature, showing long latency and small amplitude, whereas at 40 weeks of gestation responses of healthy preterm and full-term children are comparable [8].
Children born prematurely often have more severe ocular problems than children born at term primarily caused by ROP as well as cortical visual impairment, mainly due to periventricular leukomalacia. However, healthy preterm children with no history of ROP are also more prone to ocular problems than the general population. In addition, they often show structural retinal changes at school age [10, 11]. Studies investigating ERG responses in schoolchildren who were born preterm [12,13,14] have shown that photoreceptor responses are affected in preterm children even without a history of ROP, rod and combined rod/cone responses being most often affected [14].
There is little known about cone pathway-mediated ERG responses in schoolchildren born prematurely. The innovative approach of the present study is based on the usage of a portable ERG device, which was primarily developed for screening adult diabetic patients, where responses of cone system are known to be affected even before clinically evident diabetic retinopathy [15]. Due to its ease of usage, the portable ERG device might be useful for screening the pediatric population.
The aim of the present study was to investigate cone-mediated 30-Hz flicker ERG responses in preterm and term schoolchildren by using portable ERG device.
Subjects and methods
Children between the age of 6 and 10 years were included in this prospective study from November 2015 to March 2017. The study group consisted of schoolchildren born prematurely, whereas the control group consisted of healthy, age-similar term children. Preterm children were further divided into ROP+ and ROP− groups according to the history of ROP presence. ROP+ children had a history of mild retinopathy of prematurity, mostly grade 1–2 in zones 2–3, which did not require treatment. The demographics of all children included in the study are presented in Table 1.
All the children underwent comprehensive ophthalmic examination, which included fundus examination by indirect ophthalmoscopy. Fundus examination did not reveal any fundus pathology apart from slight vessel tortuosity in some children. The control group consisted of 28 children with no eye problems, with BCVA of 0.0 logMAR acuity. The study group consisted of 25 children born preterm, but with excellent visual development. Though almost half of them used minor spectacle correction (from − 2.5 to + 1.5 diopters), their BCVA was 0.0 logMAR acuity.
30-Hz flicker ERG was recorded monocularly in all children using non-mydriatic, hand-held full-field ERG recording system (RETeval, LKC Technologies, Gaithersburg, MD). The details of the device have been previously described [16, 17]. The full-field flash stimuli are presented with a dome of 6 cm in diameter. Stimuli perceived as white (CIE 1931 chromaticity, x = 0.33, y = 0.33) were presented by a combination of three-colored light emitting LED diodes (red: 622 nm; green: 530 nm and blue: 470 nm). The flickering frequency was 28.3 Hz with less than 1-ms pulse duration. A central red fixation spot was presented in the dome. The background luminance was 0 Td.
The pupillary size (in mm2) was automatically measured in real time during the stimulation. The stimulus flash luminance (cd-s/m2) was continuously adjusted to keep a constant flash retinal illuminance (Td-s) according to the equation [16]:
Photopic flash retinal illuminance (Td-s) = photopic flash luminance (cd-s/m2) × pupillary area (mm2).
The skin electrodes, which were placed on the orbital rim of the lower eyelid, were used (Sensor Strip, LKC Technologies, Inc.). In a single adhesive tape, three electrodes are embedded: an active (positive), a reference (negative) and a ground.
The amplitudes and implicit times of the fundamental component were automatically measured and displayed by the RETeval system using a special algorithm of discrete Fourier transformation (DFT) and cross-correlation analysis [18]. In this device, two flicker ERG waveforms, the fundamental component and the reconstructed “whole” flicker ERG waveform using the first eight harmonics, are presented [16].
The data of the right eye only and to 16-Td-s flash strength were taken into statistical analysis. The 30-Hz flicker ERG amplitudes and implicit times were compared between the groups with one-way analysis of variance (ANOVA), after normality of distribution was confirmed for most of the datasets using the Shapiro–Wilk normality test. Post hoc comparison was performed with Bonferroni test. Differences were considered significant at P < 0.05. The data was analyzed using the Origin 7.0 (OriginLab Corp., Northampton, USA).
Results
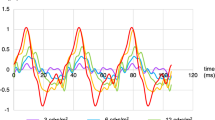
Representative waveforms of 30-Hz flicker ERG in a 7-year-old term boy (A), in an 8-year-old preterm ROP+ boy born at 24th gestational week (B) and in a 7-year-old preterm ROP− boy born at 26th gestational week (C) are shown in Fig. 1. Responses to both 16- and 32-Td-s flash strengths are shown for all three cases.
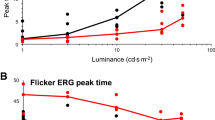
30-Hz flicker ERG amplitudes did not show significant difference between term children and children born preterm with or without ROP (F(2,49) = 1.6, p = 0.2). The mean value of the amplitude in the term group was 25.50 ± 8.2 µV (min 13.10, max 45.40), whereas in the preterm ROP+ group it was 19.48 ± 7.28 µV (min 11.60, max 33.60) and in the preterm ROP− group it was 24.77 ± 5.9 µV (min 13.10, max 35.40). A box plot of the 30-Hz flicker ERG amplitude in term and preterm ROP+ and ROP− children is shown in Fig. 2.
30-Hz flicker ERG implicit times varied significantly between all three groups of children (F(2,49) = 18.4, p < 0.0001). The mean value of the implicit time in the term group was 25.76 ± 0.9 ms (min 24.50, max 27.50), whereas in the preterm ROP+ group it was 28.96 ± 1.0 ms (min 26.90, max 30.30) and in the preterm ROP− group it was 26.87 ± 1.5 ms (min 24.30, max 31.30). A box plot of the 30-Hz flicker ERG implicit time in term and preterm ROP+ and ROP− children is shown in Fig. 3.
30-Hz flicker ERG implicit time in term and preterm ROP+ and ROP− children. The 30-Hz implicit time values of all eyes are shown in the box plots. The lines represent: 5th percentile (the lower line), 25th percentile, median, mean (square), 75th percentile and 95th percentile (the upper line). ****p = 0.0000011, **p = 0.0017, *p = 0.010
Discussion
This study shows that the 30-Hz flicker ERG has different characteristics in the preterm group of schoolchildren compared to the group of schoolchildren born at term. The implicit time of the response is predominantly affected. The preterm group of schoolchildren show markedly prolonged implicit time compared to the control group. Additionally, children with a history of the retinopathy of prematurity (ROP) show even longer ERG implicit times.
The 30-Hz flicker ERG represents the cone-driven retinal response. The results of the present study show relatively prolonged implicit time of the response, which could suggest that the cone pathway is affected due to premature birth. It is known that foveal maturation takes place well in the school-age period, and structural changes of the macular area captured with optical coherence tomography (OCT) can also be observed in older children born prematurely [19, 20]. The central cone function is therefore expected to be altered in preterm children. However, a full-field flicker ERG response represents predominantly function of peripheral cone system, since central cones account only for about 1% of the total number of cones [21]. The results of the present study suggest that overall cone system function is affected due to preterm birth.
On the other hand, the 30-Hz flicker ERG response amplitude did not show significant difference between term and preterm schoolchildren when measured with the portable ERG system. The study of adult patients with diabetic retinopathy showed similar characteristics—the implicit time of the response correlated well with the severity of the diabetic retinopathy—whereas the amplitude did not [15]. The reason for the implicit time being predominantly affected probably lies in the circulatory disturbances due to diabetes. Previous studies have shown that the 30-Hz flicker ERG response depends on contributions from the cone photoreceptors, dominated by the bipolar cell contribution [22, 23] and other post-receptor cells [24]. Furthermore, Fulton et al. [25] reported that there is an overlap in activation parameters for the cone photoreceptors between preterm children and controls. The results of the present study may therefore imply on a damage of retinal circuitry associated with the preterm birth. However, a recent study on multifocal ERG (mfERG) in children with a history of preterm birth with or without ROP has also shown no difference in amplitude between children with a mild form of ROP and those with no ROP [26]. This can imply that the effect of ROP on the neurosensory retina may not depend solely on the appearance of abnormal retinal vasculature.
For full-field, single-flashed photopic stimuli, Fulton et al. [25] found no significant difference between responses of children born preterm without a history of ROP and age-similar controls, but reported difference from the prematurely born children who had ROP as infants. On the other hand, Akerblom et al. [14] reported that prematurity alone leads to reduced photopic ERG responses. The results of the present study showed significantly longer 30-Hz implicit time in preterm ROP− children compared to controls, but the difference was even more significant when the child had ROP as an infant.
Furthermore, 30-Hz flicker ERG was shown to be dominated by cone system ON- and OFF-bipolar cell activity [23]. Recent findings of Hansen et al. [27] showed that OFF-bipolar cells mature later than ON-bipolar cells. The prolongation of the OFF-pathway-mediated responses in healthy 10-week-old term infants was their main finding that implied the possibility of relatively delayed maturation of the OFF-bipolar cells. It is therefore possible, that prolongation of the 30-Hz flicker responses, found in our preterm children, might be at least partially caused by disturbances of the OFF-bipolar cells maturation due to preterm birth. However, a recording of the retinal ON- and OFF-responses in term and preterm schoolchildren would be needed to address this issue.
The present study has also shown that a portable ERG device can be used to assess differences in ERG responses between different pediatric populations. The major advantages are: no need of mydriasis, the use of skin electrodes which can be attached without local anesthesia and short total recording time. This makes portable ERG device a useful tool in everyday clinical practice of a pediatric ophthalmologist, especially in screening prematurely born schoolchildren. Previous studies have shown that a portable ERG system is very useful in recording ERGs in various ocular pathologies in adults [15, 28, 29], a more recent one also in testing the pediatric population [30]. However, the portable system cannot replace the sensitivity and specificity of standard ISCEV full-field ERG.
Prematurity is well known to affect photoreceptor function [8, 9, 13]. Cones are more differentiated and mature earlier during the infancy compared to rods in healthy human infants born at term [1]. Therefore, cone-mediated ERG responses are more mature at a younger age compared to rod-mediated ERG responses in term children [7]. Very little is known about peripheral cone-mediated ERG responses in prematurely born children and the effect of preterm birth on the maturation of these responses. However, a recent study by Molnar et al. [31] has reported that both rod and cone functions are reduced in children born extremely preterm when compared with the controls at the age of 6.5. The present study confirmed affected cone function in preterm schoolchildren with and without ROP.
In the present study, only the 30-Hz flicker stimulus, which selectively tests cone function, was used. The use of dark adapted stimuli, which predominantly test rod function, would give additional information on the whole photoreceptor functional status in prematurely born schoolchildren. Additionally, preterm children included in the present study only had mild forms of ROP, since none of them were treated due to ROP. Among ROP− children, there were three born extremely premature (before the 27th week of gestation), but they showed significantly longer 30-Hz flicker ERG implicit time in comparison with ROP− children born after the 27th gestational week. Therefore, it can be speculated that prematurity itself can be the reason for changes in cone-mediated ERG responses demonstrated in the present study, which is in accordance with the recent study by Molnar et al. [31].
The results of the 30-Hz flicker ERG implicit time and amplitude can also be affected by axial length of the globe and by female sex as previously stated in healthy young adults [32]. The axial length was not measured in the present study, but only some prematurely born schoolchildren from this study had moderate myopia up to only − 2.5 diopters.
In summary, the results of the present study show prolonged cone-driven 30-Hz flicker ERG response implicit time in prematurely born schoolchildren in comparison with schoolchildren born at term. The results were obtained with the use of a portable ERG device, which proved its usefulness in testing the pediatric population.
References
Hendrickson A, Drucker D (1992) The development of parafoveal and mid-peripheral human retina. Behav Brain Res 49:21–31
Recchia FM, Recchia CC (2007) Foveal dysplasia evident by optical coherence tomography in patients with a history of retinopathy of prematurity. Retina 27:1221–1226
Tariq YM, Burlutsky G, Mitchell P (2012) Macular parameters and prematurity: a spectral domain coherence tomography study. J AAPOS 16:382–385
Wang J, Spencer R, Leffler JN, Birch EE (2012) Critical period for foveal fine structure in children with regressed retinopathy of prematurity. Retina 32:330–339
Vajzovic L, Rothman AL, Tran-Viet D, Cabrera MT, Freedman SF, Toth CA (2015) Delay in retinal photoreceptor development in very preterm compared to term infants. Invest Ophthalmol Vis Sci 56:908–913
Thompson DA, Liasis A (2016) Visual electrophysiology: how it can help you and your patient. In: Lambert S, Lyons C (eds) Taylor &Hoyt´s Pediatric ophthalmology and strabismus, 5th edn. Elsevier-Saunders, London, pp 68–75
Fulton AB, Hansen RM, Westall CA (2003) Development of ERG responses: the ISCEV rod, maximal and cone responses in normal subjects. Doc Ophthalmol 107:235–241
Zhou X, Huang X, Chen H, Zhao P (2010) Comparison of electroretinogram between healthy preterm and term infants. Doc Ophthalmol 121:205–213
Hansen RM, Fulton AB (2005) Development of the cone ERG in infants. Invest Ophthalmol Vis Sci 46:3458–3462
Holmstrom G, Larsson E (2008) Long-term follow-up of visual functions in prematurely born children: a prospective population-based study up to 10 years of age. J AAPOS 12:157–162
Akerblom H, Larsson E, Eriksson U, Holmstrom G (2011) Central macular thickness is correlated with gestational age at birth in prematurely born children. Br J Ophthalmol 95:799–803
Birch DG, Anderson JL (1992) Standardized full-field electroretinography. Normal values and their variation with age. Arch Ophthalmol 110:1571–1576
Harris ME, Moskowitz A, Fulton AB, Hansen RM (2011) Long-term effects of retinopathy of prematurity (ROP) on rod and rod-driven function. Doc Ophthalmol 122:19–27
Akerblom H, Andreasson S, Larsson E, Holmstrom G (2014) Photoreceptor function in school-aged children is affected by preterm birth. Tran Vis Sci Tech 3(6):1–7
Fukuo M, Kondo M, Hirose A, Fukushima H, Ikesugi K, Sugimoto M, Kato K, Uchigata Y, Kitano S (2016) Screening for diabetic retinopathy using new mydriasis-free, full-field flicker ERG recording device. Sci Rep 6: Article number 36591
Kato K, Kondo M, Sugimoto M, Ikesugi K, Matsubara H (2015) Effect of pupil size on flicker ERGs recorded with RETeval system: new mydriasis-free full-field ERG system. Invest Ophthalmol Vis Sci 56:3684–3690
Maa AY, Feuer WJ, Davis CQ, Pillow EK, Brown TD, Caywood RM, Chasan JE, Fransen SR (2016) A novel device for accurate and efficient testing for vision-threatening diabetic retinopathy. J Diabetes Complicat 30:524–532
Severns ML, Johnson MA, Merritt SA (1991) Automated estimation of implicit time and amplitude from the flicker electroretinogram. Appl Opt 30:2106–2112
Hammer DX, Iftimia NV, Ferguson RD et al (2008) Foveal fine structure in retinopathy of prematurity: an adaptive optics Fourier domain optical coherence tomography study. InvestOphthalmol Vis Sci 49:2061–2070
Akerblom H, Holmstrom G, Eriksson U, Larsson E (2012) Retinal nerve fibre layer thickness in school-aged prematurely-born children compared to children born at term. Br J Ophthalmol 96:956–960
Curcio CA, Sloan KR, Kalina RE, Hendrickson AE (1990) Human photoreceptor topography. J Comp Neurol 292:497–523
Kondo M, Sieving PA (2001) Primate photoreceptor sine-wave flicker ERG: vector modeling analysis of component origins using glutamate analogs. Invest Ophthalmol Vis Sci 42(1):305–312
Bush RA, Sieving PA (1996) Inner retinal contributions to the photopic fast flicker electroretinogram. J Opt Soc Am A 13:557–565
Viswanathan S, Frishman LJ (2002) Robson JG (2002) Inner-retinal contributions to the photopic sinusoidal electroretinogram of macaques. Doc Ophthalmol 105(2):223–242
Fulton AB, Hansen RB, Moskowitz A (2008) The cone electroretinogram in retinopathy of prematurity. Invest Ophthalmol Vis Sci 49(2):814–819
Altschwager P, Moskowitz A, Fulton AB, Hansen RM (2017) Multifocal ERG responses in subjects with a history of preterm birth. Invest Ophthalmol Vis Sci 58:2603–2608
Hansen RM, Moskowitz A, Akula JD, Fulton AB (2017) The neural retina in retinopathy of prematurity. Prog Retin Eye Res 56:32–57
Yasuda S, Kachi S, Ueno S, Piao CH, Terasaki H (2015) Flicker electroretinograms before and after intravitreal ranibizumab injection in eyes with central retinal vein occlusion. Acta Ophthalmol 293:465–468
Miura G, Nakamura Y, Sato E, Yamamoto S (2016) Effects of cataracts on flicker electroretinograms recorded with RETeval system: new mydriasis-free ERG device. BMC Ophthalmol 16:22
Grace SF, Lam BL, Feuer WJ, Osigian CJ, Cavuoto KM, Capo H (2017) Nonsedated handheld electroretinogram as a screening test of retinal dysfunction in pediatric patients with nystagmus. J AAPOS 21(5):384–388
Molnar AEC, Andreasson SO, Larsson EKB, Akerblom HM, Holmstrom GE (2017) Reduction in rod and cone function in 65-year-old children born extremely preterm. JAMA Ophthalmol 135(8):854–861
Kato K, Kondo M, Nagashima R, Sugawara A, Sugimoto M, Matsubara H, McCulloch DL, Ikesugi K (2017) Factors affecting mydriasis-free flicker ERGs recorded with real-time correction for retinal illuminance: study of 150 young healthy subjects. Invest Opthalmol Vis Sci 58:5280–5286
Acknowledgements
This study was supported by the Slovenian Research Agency (P3-0333) and a research grant from Medical Centre Ljubljana.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Manca Tekavčič Pompe and Maja Šuštar declare that they have no conflict of interest.
Data availability
Data generated during the course of the current study are available from the corresponding author on reasonable request.
Statement of human rights
This study adhered to the tenets of the World Medical Association’s Declaration of Helsinki and was approved by the Ethics Committee of the Medical Faculty, University of Ljubljana, Slovenia (Number 151/08/14).
Statement on the welfare of animals
No animals were used in this study.
Informed consent
Informed consent was obtained from all parents or caregivers of children included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tekavčič Pompe, M., Šuštar, M. Flicker electroretinogram recorded with portable ERG device in prematurely born schoolchildren with and without ROP. Doc Ophthalmol 139, 59–65 (2019). https://doi.org/10.1007/s10633-019-09695-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-019-09695-6