Abstract
Background
There are scanty population-based studies investigating the incidence and prevalence rates of inflammatory bowel disease (IBD) in Taiwan.
Aims
This study aimed to estimate the nationwide prevalence and incidence of IBD and identify its noticeable trends in Taiwan between 2016 and 2020.
Methods
A retrospective study by analyzing the data from the National Health Insurance Research Database of Taiwan.
Results
A total of 2595 patients with catastrophic IBD illness were registered from 2016 to 2020 in Taiwan (CD, 880; UC, 1715). The male-to-female ratio in the study sample was 1.83:1 for CD and 1.69:1 for UC. The median age of those registered with CD and UC was 37 and 47 years, respectively. The incidence rate of CD was 0.65 per 100,000 persons in 2016 and it was increased to 0.81 per 100,000 persons in 2020. The incidence rate of UC was 1.16 per 100,000 persons in 2016 and it was increased to 1.53 in 2020. Overall, the incidence of IBD was increase from 1.81 per 100,000 persons to 2.34 per 100,000 persons between 2016 and 2020. Overall, the prevalence rates of IBD was increase from 14.95 per 100,000 persons to 20.02 per 100,000 persons between 2016 and 2020.
Conclusion
The epidemiological stages of IBD in Taiwan was considered in the acceleration in incidence stage, during which incidence rises and prevalence is relatively low. Understanding these geographical differences is important for the rising global burden of IBD.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is characterized by chronic and repetitive inflammation of the gastrointestinal tract [1, 2].Crohn’s disease (CD) and ulcerative colitis (UC) are the two major forms.
IBD is thought to be caused by a complex interactions between diet, environmental factors, genetic predisposition, immune dysregulation, and gut dysbiosis, but comprehensive understanding of the underlying pathophysiological mechanisms is still lacking [1, 2]. Over time, many patients with IBD experience disease progression from primarily inflammation to bowel damage such as intestinal obstruction, strictures, fistula, and abscess.
The characteristics of IBD are different between Asia and Western patients with regard to epidemiology, nature course, phenotype, and genetic susceptibility [3]. Comparison of population-based data in East and West reveals that the incidence of IBD has risen rapidly in East while plateauing in West [4,5,6]. The prevalence and incidence of IBD is increasing in Asia, including Taiwan [5, 7,8,9,10,11]. Today, IBD is recognized as a global disease. The growing number of IBD patients is likely to substantial increase in the burden of health care system.
However, the latest data about epidemiological trend in IBD in Taiwan was 2015. In the current study, we would report the epidemiological trend of IBD in Taiwan from 2016 to 2020.
Materials and Methods
A retrospective study was conducted to analyze data recorded from January 2016 to December 2020 in the registered database compiled by the National Health Insurance and provided by the Ministry of Health and Welfare, Taiwan. The Taiwan National Health Insurance (NHI) is a centralized and compulsory health insurance system covering > 99% of Taiwan’s citizens.
We identified the patients who received catastrophic illness certificates for IBD by their associated International Classification of Diseases, 10th revision (ICD-10) codes. The following ICD-10, Clinical Modification (ICD-10-CM) codes were used to identify patient records in this study: K50.x for CD and K51.x for UC. Catastrophic illness certification is initiated by a physician. Physicians have to submit patients’ histopathological and endoscopic (or radiologic) examination data to the Taiwan National Health Insurance (NHI), and IBD patients would be registered in Registry for Catastrophic Illness (RCI) after approval by the NHI’s Expert Committee.
The prevalence rate of IBD was computed by year. Prevalence rate was calculated as the number of cases between 2016 and 2020 divided by the total number of person-years at risk. Incidence rate was calculated as the number of new cases between 2016 and 2020 divided by the total number of person-years at risk.
The present study was approved by the Ethics Review Board of the Chang Gung Memorial Hospital (IRB No. 202201150B1) and informed consent was waived.
Results
Incidence
Between 2016 and 2020, there were 880 incident cases of CD and 1715 incident cases of UC respectively, corresponding to an overall incidence rate ratio of UC to CD was 1.95 (Table 1).
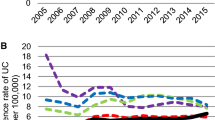
The incidence rate of CD was 0.65 per 100,000 persons in 2016 and it was increased to 0.81 per 100,000 persons in 2020. The incidence rate of UC was 1.16 per 100,000 persons in 2016 and it was increased to 1.53 in 2020. Overall, the incidence of IBD was increase from 1.81 per 100,000 persons to 2.34 per 100,000 persons between 2016 and 2020 (Table 2; Fig. 1).
Prevalence
The prevalence rates of CD increased from 3.91 in 2016 to 6.06 per 100,000 persons in 2020. The prevalence rates of UC increased from 11.04 in 2016 to 13.96 per 100,000 persons in 2020. Overall, the prevalence rates of IBD was increase from 14.95 per 100,000 persons to 20.02 per 100,000 persons between 2016 and 2020 (Table 3; Fig. 2).
Age
During 2016 to 2020, the median age of those registered with CD and UC was 37 and 47 years, respectively (Table 1).
For CD, the incidence case peaked at age 25–29 and dropped thereafter with a second smaller peak at age 55–69. For UC, the incidence case peaked at age 40–44 and dropped thereafter with a second smaller peak at age 50–59 (Fig. 3).
For CD, 11.02% of patients was registered at age under 20, 44.09% at age 20–39, 25.91% at age 40–59, 18.07% at age 60–79 and 0.91% at age over 80. For UC, 3.91% of patients was registered at age under 20, 30.15% at age 20–39, 43.09% at age 40–59, 21.28% at age 60–79 and 1.57% at age over 80 (Table 1).
Male-to-Female Ratio
The male-to-female ratio in the study sample was 1.83:1 for CD and 1.69:1 for UC. The male-to-female ratio in 2016 was 2.45:1 for CD and 1.44:1 for UC. The male-to-female ratio in 2017 was 1.69:1 for CD and 1.74:1 for UC. The male-to-female ratio in 2018 was 1.45:1 for CD and 1.88:1 for UC. The male-to-female ratio in 2019 was 1.59:1 for CD and 1.84:1 for UC. The male-to-female ratio in 2020 was 2.25:1 for CD and 1.53:1 for UC. A male-predominant pattern for IBD was observed in Taiwan (Table 1).
UC-to-CD Incidence Ratio from 2016 to 2020 in Taiwan Was Steady
We compared the incidence ratio of UC to CD from 2016 to 2020 and no significant difference was observed during this period. UC is twice as common as CD (Fig. 4).
Burden of Biologic Use in IBD Patients Is Increasing
Among CD, the number of patients who received biologics treatment was increased from 231 in 2016 to 574 in 2020 (Table 4). Among UC, the number of patients who received biologics treatment was increased from 73 in 2016 to 594 in 2020 (Table 5).
Among CD, the most prescribed biologics were Adalimumab (52.27%) and Vedolizumab (28.96%) in 2020. Among UC, the most prescribed biologics were Vedolizumab (43.89%) and Adalimumab (35.89%) in 2020.
Discussion
IBD is believed to be related to the activation of the intestinal mucosal immune system in response to dysbiosis of the gastrointestinal tract in genetically susceptible individuals [1]. This disease most commonly occurs in young and middle-aged adults and still has a certain disability rate even with recent advances in treatment.
Taiwan CD and UC incidence and prevalence rates are lower than in the West. However, in recent decades, Taiwan’s CD and UC disease incidence and prevalence rates have been increased rapidly [10, 11]. The crude incidence of CD increased from 0.17 per 100,000 persons in 2001 to 0.47 per 100,000 persons in 2015, whereas that of UC increased from 0.54 per 100,000 persons in 2001 to 0.95 per 100,000 persons in 2015. The prevalence of CD increased from 0.6 per 100,000 persons in 2001 to 3.9 per 100,000 persons in 2015, whereas that of UC increased from 2.1 per 100,000 persons in 2001 to 12.8 per 100,000 persons in 2015 [11]. In our current study, the incidence rate of CD was 0.65 per 100,000 persons in 2016 and it was increased to 0.81 per 100,000 persons in 2020. The incidence rate of UC was 1.16 per 100,000 persons in 2016 and it was increased to 1.53 in 2020. The prevalence of CD increased from 3.91 per 100,000 persons in 2016 to 6.06 per 100,000 persons in 2020, whereas that of UC increased from 11.04 per 100,000 persons in 2016 to 13.96 per 100,000 persons in 2020. In Taiwan, the incidence and prevalence of IBD were increased steadily from 2001 to 2020.
In Western country, the average age of onset in adult incident cases was a median 31–34 years [12,13,14,15,16]. In both CD and UC, incidence peaked in the age interval 20–30 years; however, a second peak between the ages of 60 and 79 years was reported in UC. A similar age distribution has been reported in Asia, where the median age of diagnosis in patients with CD and UC was 34 and 42 years, respectively [17, 18]. In contrast to findings in West, a bimodal distribution was only seen in CD and not in UC in most Asian populations, where the incidence rate of CD peaked in the age ranges of 20–24 years and 40–44 years [19]. In our current study, the bimodal distribution was seen in CD but not obvious in UC.
The proportion of IBD cases diagnosed in older adults in each population has practical implications and will vary not only with changes in age-specific incidence rates but also with changes in the age structure of the population. In the Danish National cohort [20], 21% of UC cases and 17% of CD cases were diagnosed above 60 years of age. In our current study, 22.85% of UC cases and 18.98% of CD cases were diagnosed above 60 years of age. In the future, the health care system will face increasing IBD patent number while simultaneously managing an aging population that will have a mixture of complications of longstanding IBD and age-related comorbidities [6].
The overall incidence of UC in Western country is independent of gender. In CD, less consistent findings have been reported, with some cohorts suggesting a female predominance in the incidence of CD and others failing to find any gender difference [12,13,14,15,16]. In a pooled analysis of studies in the West, females predominated among CD patients from adolescence to middle-age, while a higher risk of UC was found among males aged 45 years and older [21]. These findings contrast with those from Asia, where male gender was associated with a higher risk of both CD and UC. In mainland China, the risk ratio of CD and UC in males versus females is 1.15:1 and 2.4:1, respectively [22]. An increased risk of UC among males was also found in Korea [23]. A pooled analysis confirmed the association between male Asians and an increased risk of both CD and UC among those in the range of 10–50 years old [24]. In our current study, male-to-female ratio of CD and UC is 1.83:1 and 1.69:1, respectively. The male-to-female ratio in Taiwan from 2001 to 2015 was 2.19 for CD and 1.62 for UC. The trend of male predominance continued between 2016 and 2020 [10] The precise mechanism underlying the differences in the sex distributions between Asian and Western IBD patients is still unknown.
As we known, the UC/CD ratio in East Asian countries has reduced because of the accelerating incidence of CD. According to previous study [10], the UC/CD ratio decreased from 4.32 in 2001–2005 to 4.17 in 2006–2010 to 2.03 in 2011–2015 in Taiwan and decreased to 1.95 in 2016–2020 in present data. In Korea, the UC/CD ratio was 5.03 in 1986–1990, and it reduced to 2.57 in 2006–2010, to 2.39 in 2011–2015[25]. The decreasing slope of UC/CD ratio has became flattened. We compared the incidence ratio of UC to CD from 2016 to 2020 and no significant difference was observed during this period. Currently, UC is twice as common as CD in Taiwan.
The definite reason for decrease of UC/CD ratio after 2000 is not clear, but may reflect the improvement of diagnosis for CD. Capsule endoscopy, which was introduced in 2000, and double-balloon enteroscopy, which was introduced in 2001, had made it possible to explore the entire small intestine. The diagnosis of CD is more complex and improvement of diagnostic methods make physician more aware of CD.
IBD is a global disease and its evolution can be divided into four epidemiological stages: emergence, acceleration in incidence, compounding prevalence and prevalence equilibrium. In the stage of acceleration in incidence, there is a dramatic increase in the number of incident cases but overall prevalence remains low [6].
Incidence of IBD is increasing in emerging populations in Asia suggesting that changing environmental factors play an important part. Various environmental risk factors have been implicated in the pathogenesis of IBD, including diet and lifestyle which may perturbations of the gut microbiota [26, 27] Certain nutrients and food additives can impact on the gut microbiome and their interactions with the host may play a role in the pathogenesis of IBD [28] Consumption of ultra-processed food had increased over the last decade in industrialized countries, and epidemiological studies had found associations between ultra-processed food consumption and chronic diseases [29]. Understanding the underlying determinants of development of IBD is very important. By modification of the underlying determinants, particularly around diet and other modifiable behaviors, may prevent disease development in subject with genetic susceptibility.
The epidemiological stage of IBD in Taiwan was considered in the acceleration in incidence stage. High cost of caring for patients with IBD will have a considerable financial effect on the health care system.
Limitations
By analyzing data from the National Health Insurance registration system, we found a steady increase in the incidence and prevalence of IBD in Taiwan from 2016 to 2020. The strength of this study was the availability of a nationwide cohort that provides access to healthcare and registration for near all its citizens. But the incidence and prevalence level may be underestimated due to relatively strict criteria by using the number of patients who completed a catastrophic disease registry, which required clinical records, endoscopic images, and pathological findings. Additionally, there was no information about the disease phenotype.
Conclusion
The epidemiological stages of IBD in Taiwan was considered in the acceleration in incidence stage, during which incidence rises and prevalence is relatively low. Understanding these geographical differences is important for the rising global burden of IBD.
Data availability
No datasets were generated or analysed during the current study.
References
Chang JT. Pathophysiology of inflammatory bowel diseases. N Engl J Med 2020;383:2652–2664.
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med 2009;361:2066–2078.
Ng SC, Bernstein CN, Vatn MH et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut 2013;62:630–649.
Mak WY, Zhao M, Ng SC, Burisch J. The epidemiology of inflammatory bowel disease: east meets west. J Gastroenterol Hepatol 2020;35:380–389.
Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res 2016;14:111–119.
Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol 2021;18:56–66.
Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol 2008;103:3167–3182.
Molodecky NA, Soon IS, Rabi DM et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46-54.e42.
Ng SC, Shi HY, Hamidi N et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2017;390:2769–2778.
Kuo CJ, Yu KH, See LC et al. The trend of inflammatory bowel diseases in Taiwan: a population-based study. Dig Dis Sci 2015;60:2454–2462.
Yen HH, Weng MT, Tung CC et al. Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study. Intest Res 2019;17:54–62.
Shivashankar R, Tremaine WJ, Harmsen WS, Loftus EV. Incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota From 1970 Through 2010. Clin Gastroenterol Hepatol 2017;15:857–863.
Lakatos L, Kiss LS, David G et al. Incidence, disease phenotype at diagnosis, and early disease course in inflammatory bowel diseases in Western Hungary, 2002–2006. Inflamm Bowel Dis 2011;17:2558–2565.
Vegh Z, Burisch J, Pedersen N et al. Incidence and initial disease course of inflammatory bowel diseases in 2011 in Europe and Australia: results of the 2011 ECCO-EpiCom inception cohort. J Crohns Colitis 2014;8:1506–1515.
Rönnblom A, Holmström T, Tanghöj H, Karlbom U, Thörn M, Sjöberg D. Low colectomy rate five years after diagnosis of ulcerative colitis. Results from a prospective population-based cohort in Sweden (ICURE) diagnosed during 2005–2009. Scand J Gastroenterol 2016;51:1339–1344.
Su HY, Gupta V, Day AS, Gearry RB. Rising incidence of inflammatory bowel disease in Canterbury, New Zealand. Inflamm Bowel Dis 2016;22:2238–2244.
Ng SC, Leung WK, Shi HY et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territory-wide population-based registry in Hong Kong. Inflamm Bowel Dis 2016;22:1954–1960.
Yang SK, Yun S, Kim JH et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: a KASID study. Inflamm Bowel Dis 2008;14:542–549.
Ng SC, Tang W, Ching JY et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology 2013;145:158-165.e152.
Nørgård BM, Nielsen J, Fonager K et al. The incidence of ulcerative colitis (1995–2011) and Crohn’s disease (1995–2012)—based on nationwide Danish registry data. J Crohns Colitis 2014;8:1274–1280.
Shah SC, Khalili H, Gower-Rousseau C et al. Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from western countries. Gastroenterology 2018;155:1079-1089.e1073.
Zeng Z, Zhu Z, Yang Y et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study. J Gastroenterol Hepatol 2013;28:1148–1153.
Kim HJ, Hann HJ, Hong SN et al. Incidence and natural course of inflammatory bowel disease in Korea, 2006–2012: a nationwide population-based study. Inflamm Bowel Dis 2015;21:623–630.
Shah SC, Khalili H, Chen CY et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from the Asia-Pacific region. Aliment Pharmacol Ther 2019;49:904–911.
Park SB, Yoon JY, Cha JM. What are the different phenotypes of inflammatory bowel disease in Asia? Gut Liver 2022;16:676–685.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol 2015;12:205–217.
Ananthakrishnan AN, Kaplan GG, Bernstein CN et al. Lifestyle, behaviour, and environmental modification for the management of patients with inflammatory bowel diseases: an international organization for study of inflammatory bowel diseases consensus. Lancet Gastroenterol Hepatol 2022;7:666–678.
Levine A, Rhodes JM, Lindsay JO et al. Dietary guidance from the international organization for the study of inflammatory bowel diseases. Clin Gastroenterol Hepatol 2020;18:1381–1392.
Lo CH, Khandpur N, Rossato SL et al. Ultra-processed foods and risk of Crohn’s disease and ulcerative colitis: a prospective cohort study. Clin Gastroenterol Hepatol 2022;20:e1323–e1337.
Acknowledgments
The authors received grant support from Chang Gung Memorial Hospital, Linkou, Taiwan (CMRPG3L0451, CPRPG3L0042, CMRPG3N0271, CORPG3N0201, CORPG3L0191).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions as following: Developed the study concept and design: CT Chiu, CJ Chang, CJ Kuo, PH Le. Provided the critical revision of the manuscript for important intellectual content: WR Lin, ML Chang, MY Su. Wrote the main manuscript text: CJ Kuo, CY Lin. Prepared figures : YW Kuo, CM Hsu, MW Lai. All authors approved the final version of the manuscript. The authors thank Yu-Yang Lin and Tse-Chih Chou for their assistance with statistical analysis
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuo, CJ., Lin, CY., Le, PH. et al. Temporal Trends of Inflammatory Bowel Diseases in Taiwan from 2016 to 2020: A Population-Based Study. Dig Dis Sci 69, 3172–3179 (2024). https://doi.org/10.1007/s10620-024-08518-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08518-2