Abstract
Background
The post-reflux swallow-induced peristaltic wave (PSPW) brings salivary bicarbonate to neutralize residual distal esophageal mucosal acidification.
Aims
To determine if reduced saliva production and esophageal body hypomotility would compromise PSPW-induced pH recovery in the distal esophagus.
Methods
In this multicenter retrospective cross-sectional study, patients with confirmed Sjogren’s syndrome and scleroderma/mixed connective tissue disease (MCTD) who underwent high resolution manometry (HRM) and ambulatory pH-impedance monitoring off antisecretory therapy were retrospectively identified. Patients without these disorders undergoing HRM and pH-impedance monitoring for GERD symptoms were identified from the same time-period. Acid exposure time, numbers of reflux episodes and PSPW, pH recovery with PSPW, and HRM metrics were extracted. Univariate comparisons and multivariable analysis were performed to determine predictors of pH recovery with PSPW.
Results
Among Sjogren’s syndrome (n = 34), scleroderma/MCTD (n = 14), and comparison patients with reflux symptoms (n = 96), the scleroderma/MCTD group had significantly higher AET, higher prevalence of hypomotility, lower detected reflux episodes, and very low numbers of PSPW (p ≤ 0.004 compared to other groups). There was no difference in pH-impedance metrics between Sjogren’s syndrome, and comparison patients (p ≥ 0.481). Proportions with complete pH recovery with PSPW was lower in Sjogren’s patients compared to comparison reflux patients (p = 0.009), predominantly in subsets with hypomotility (p < 0.001). On multivariable analysis, diagnosis of Sjogren’s syndrome, scleroderma/MCTD or neither (p = 0.014) and esophageal hypomotility (p = 0.024) independently predicted lack of complete pH recovery with PSPW, while higher total reflux episodes trended (p = 0.051).
Conclusions
Saliva production and motor function are both important in PSPW related pH recovery.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is characterized by symptoms or complications that result from the retrograde movement of gastric contents into the esophagus [1,2,3]. GERD is one of the most commonly diagnosed digestive disorders, with an increasing worldwide prevalence [4, 5]. The primary mechanism for retrograde reflux is transient lower esophageal sphincter relaxations (tLESRs). Other contributing factors include low lower esophageal sphincter (LES) pressure which can be overcome by increased intra-abdominal pressure during straining, and swallow-associated LES relaxations [6]. A certain number of daily reflux episodes are within physiological limits, with broad agreement that numbers within asymptomatic volunteers and treated GERD patients are < 40 episodes/day [2, 7,8,9]. In healthy subjects, abnormal acid exposure during physiological reflux episodes is partly prevented by the competence of the anti-reflux barrier, from diaphragmatic crural pinch superimposed on the LES, supported by the phrenoesophageal ligament and gastric sling fibers at the gastric cardia [10, 11]. A second mechanism preventing abnormal acid exposure is clearance of the refluxate [6].
Esophageal reflux clearance is a two-step event, initial volume clearance followed by chemical clearance, the purpose of which is remove the refluxate in order to restore intraluminal pH to physiologic levels after an acid reflux episode. Volume clearance occurs through primary and secondary peristalsis, triggered by distension from the refluxate activating mechanoreceptors within the esophageal wall, while chemical clearance requires a vagal esophago-salivary reflex and involves a primary swallow of secreted saliva [12, 13]. This clearing swallow brings salivary bicarbonate, mucin and epidermal growth factor to the distal esophagus to neutralize pH, repair mucosal damage and reduce risk of long-term acid-related complications [14, 15]. The post-reflux swallow-induced peristaltic wave (PSPW) represents the pH-impedance event that defines the clearing swallow, and occurs within 30 s after volume clearance of a reflux episode [16]. In the upright position, gravity participates in volume clearance, while mucosal acidification from gastric acid may require ≥ 1 swallow for full chemical clearance [12], also supported by the fact that a PSPW is not seen following as many as half of reflux episodes in healthy adults [7], with even lower proportions of PSPW in certain GERD phenotypes [17].
In this study, we hypothesized that PSPW would be less effective in chemical clearance when either saliva production or esophageal motor function is compromised. We hypothesized that reduced saliva production in Sjogren’s syndrome and esophageal hypomotility in both Sjogren’s syndrome and scleroderma/mixed connective tissue disease (MCTD) would compromise PSPW-induced pH recovery in the distal esophagus. To test this hypothesis, we compared descriptive and analytical data from pH-impedance tracings and high resolution manometry (HRM) studies in patients with diagnoses of Sjogren’s disease, scleroderma/MCTD and in patients with GERD symptoms.
Methods
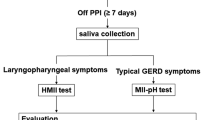
In this retrospective study, data obtained from consecutive adults aged 18 years or older with prior confirmed rheumatologic diagnoses of Sjogren’s syndrome or scleroderma/MCTD at Washington University in St. Louis and Barts and the London School of Medicine and Dentistry over a period of 6 years (2014–2020) were analyzed. Inclusion required esophageal physiologic testing with HRM and ambulatory 24-h pH monitoring off antisecretory therapy. For comparison, a control group was created on a 2:1 ratio matched for age, gender and month of esophageal testing from patients without the above rheumatologic diagnoses being evaluated with similar HRM and ambulatory 24-h pH monitoring for typical and atypical GERD symptoms over the same time frame. Exclusion criteria consisted of prior foregut surgery, artifacts precluding reflux episode and PSPW identification on pH-impedance monitoring, incomplete or critically imperfect HRM studies and unconfirmed rheumatologic diagnoses. Demographic details were extracted from review of the esophageal testing records. Since this study was intended to investigate the specific role of saliva and motor function in pH recovery after reflux events in the esophagus rather than the clinical implications of PSPW, clinical presentations and symptom outcome were not evaluated. The review and analysis of esophageal physiologic studies was approved by institutional review boards at both institutions with a waiver of consent because research only involved existing esophageal studies. Data-sharing agreements were in place such that de-identified patient data could be pooled and analyzed.
Esophageal Testing
HRM was performed using standard methodology as previously described [18]. A trained motility nurse passed a catheter with 36 high-fidelity solid state circumferential sensors (Medtronic, Duluth, GA) through the anesthetized nasal passage, and positioned the catheter such that the three distal sensors were within the stomach. All HRM studies included a resting phase for evaluation of baseline esophagogastric junction (EGJ) tone and morphology, followed by ten standard supine 5 mL swallows for analysis using Chicago classification version 4.0 (CCv4.0) [19]. All HRM studies were analyzed using proprietary analysis and display system (ManoView; Medtronic, Duluth, GA). CCv4.0 diagnoses were determined using standard software tools for the evaluation of the integrated relaxation pressure (IRP), distal latency (DL), and distal contractile integral (DCI). Ineffective esophageal motility (IEM) was defined by the presence of > 70% ineffective swallows or ≥ 50% failed peristalsis; absent contractility required failed peristalsis with every supine swallow with a normal IRP [19].
pH-impedance monitoring (Ohmega, Laborie, formerly Medical Measurement Systems, Enschede, Netherlands, and Diversatek, formerly Sandhill Scientific, Boulder, Colorado as appropriate) was performed immediately following HRM, using HRM localization of the LES to position the pH sensor 5 cm proximal to the LES. All studies were performed off antisecretory therapy, and patients stopped proton pump inhibitor (PPI) therapy for 7 days, anti-histamine-2 receptor antagonists for 3 days, and antacids for 24 h prior to reflux monitoring. Analysis of pH-impedance studies was performed using commercially available software (Ohmega, Medical Measurement Systems, Enschede, Netherlands, and Sandhill Scientific, Boulder, Colorado as appropriate). After excluding meal times, total, upright and supine distal esophageal acid exposure time (AET) were extracted and recorded from the pH-impedance studies. Reflux episodes were automatically identified by the software, and then manually reviewed using Wingate Consensus criteria [20]. This requires a 50% drop in baseline impedance in the distal impedance channels for identification of a reflux episode, which may be difficult to identify in the context of low baseline impedance.
After each reflux episode, in the 30 s time window following return of impedance values to baseline in the distal-most impedance channel, the presence of absence of PSPW was recorded. Identification of PSPW required a primary swallow starting in the most proximal impedance channel, with a 50% impedance drop in the distal impedance channels to signify presence of liquid (saliva) with the swallow (Fig. 1) [20]. For each PSPW, related pH recovery was measured and categorized as follows: full recovery, if pH was restored to baseline value; partial recovery, if pH improved without reaching the baseline value; no recovery, if the PSPW did not have any effect on restoring the pH value (Fig. 1). pH recovery that did not reach the baseline pH value was considered ‘incomplete’.
Post-reflux swallow-induced peristaltic wave (PSPW) occurring within 30 min following an acid reflux episode on pH-impedance monitoring. The black arrow demonstrates a primary swallow with impedance drop indicating liquid content with the swallow extending from the proximal to the distal esophagus. In a control patient, when the swallow arrives at the distal esophagus, the pH drop from the acid reflux episode recovers completely to baseline values (panel A), indicating neutralization of mucosal acidification with salivary bicarbonate. However, in a patient with Sjogren’s syndrome, there is no pH recovery from the PSPW, and it takes a second swallow a full minute after the end of the reflux episode for pH recovery
Statistical Methods
Data are reported as proportions (percentages) or medians (interquartile range, IQR). Categorical data were compared using the Fisher’s exact test for 2 × 2 comparisons and χ-squared test for multiple comparisons, as appropriate. Continuous data were compared using Mann Whitney U test for two-group comparisons, or Kruskal Wallis test for multiple group comparisons. Correlations between continuous data were assessed using correlational analysis (Spearman’s rho). To identify independent predictors of lack of efficacy of PSPW in pH recovery, multivariable logistic regression was performed using variables meeting statistical significance on univariate analyses. Statistical significance required p < 0.05. All statistical analyses were performed using SPSS v28.0 (Armonk, NY).
Results
Of 144 patients, 34 (median age, 52.0 years, 85.3% female) carried a diagnosis of Sjogren’s syndrome, 14 (median age, 53.5 years, 71.4% female) had scleroderma/MCTD, and 96 patients (median age, 52.0 years, 84.4% female) with GERD symptoms in the absence of Sjogren’s syndrome/scleroderma/MCTD formed the symptomatic controls (Table 1).
Esophageal Testing Characteristics
As expected, the scleroderma/MCTD group had the highest prevalence of hypomotility on HRM (p < 0.001 across groups, and p ≤ 0.038 on pairwise comparisons with and between other two groups), particularly absent contractility (p < 0.001 across groups, and on pairwise comparisons with each of the other two groups) (Fig. 2). The proportion of patients with absent contractility was lowest in the control group with GERD symptoms but similar to Sjogren’s syndrome (p = 0.168), while IEM had the lowest prevalence within the Sjogren’s group (p = 0.002 across groups, and p ≤ 0.009 on pairwise comparisons with the control group, Table 1). End-expiratory LES pressures were not different between groups (p = 0.967) including on pairwise comparisons.
Manometric patterns were different across the three patient groups (p = 0.001 across groups). Absent contractility was significantly more common in patients with scleroderma and mixed connective tissue disease (MCTD) compared to either Sjogren’s syndrome or the comparison cohort (p < 0.001). Normal manometry was the predominant finding in patients with Sjogren’s syndrome
On pH-impedance monitoring, proportions of patients with AET > 6% was highest within the scleroderma/MCTD group, while the proportions of patients with reflux episodes > 80 were small overall (Fig. 3). The scleroderma/MCTD group had significantly higher AET, lower detected reflux episodes, and very low numbers of PSPW compared to the other groups (p ≤ 0.017 for each comparison across groups, Table 1), partly related to low baseline impedance impairing detection of reflux episodes and PSPW. On pairwise comparisons between scleroderma/MCTD and Sjogren’s syndrome groups, total AET was higher (p = 0.012), reflux episode numbers were lower (p = 0.006), and PSPW numbers were lower (p = 0.007) in scleroderma/MCTD patients, while lower PSPWI trended toward significance (p = 0.055). Compared to the control group with GERD symptoms, the scleroderma/MCTD group had higher total AET (p = 0.005), lower reflux episodes (p < 0.001) and PSPW numbers (p = 0.003). There was no difference in pH-impedance metrics between Sjogren’s syndrome and the control group with GERD symptoms (p ≥ 0.473 for each pairwise comparison), including between subsets of patients with hypomotility (p ≥ 0.116 for each pairwise comparison). Specifically, within the Sjogren’s syndrome cohort, there was no difference in pH-impedance metrics between patients with and without hypomotility (Table 2).
Proportions with abnormal, indeterminate and physiologic metrics for acid exposure time (AET) and numbers of reflux episodes in the three patient groups. Proportions of patients with abnormal AET (> 6%) was highest in the scleroderma and mixed connective tissue disease (MCTD) group (p = 0.037 across groups), but AET proportions were not different across the groups (p = 0.126). There were very limited proportions of patients with reflux episodes > 80 within the scleroderma/MCTD group; the Sjogren’s syndrome group and patients with neither abnormality had equivalent proportions with physiologic (< 40) reflux episodes (p = 0.208 across groups)
pH Recovery with PSPW
Proportions with complete pH recovery with PSPW was lower in patients with Sjogren’s syndrome compared to control patients with reflux symptoms (p = 0.009), predominantly in subsets with hypomotility (p < 0.001). On pairwise comparisons, both Sjogren’s syndrome and scleroderma/MCTD groups had lower total pH recovery proportions compared to the control group (p ≤ 0.008 for each comparison). However, among Sjogren’s syndrome with hypomotility, absent contractility was associated with rates of complete pH recovery with PSPW similar to patients with scleroderma/MCTD (0.0% vs. 8.1%, respectively, p = ns), while Sjogren’s syndrome with IEM resembled the control group with IEM (p = ns) although numbers were small. On direct comparison of patients with and without hypomotility features within the Sjogren’s syndrome cohort, there were no differences noted in pH-impedance metrics (Table 2).
Multivariable Analysis
A multivariable logistic regression model was created to identify predictors of lack of complete pH recovery with PSPW where variables of interest consisted of total AET, total reflux episodes, PSPW index, motility pattern and diagnosis. Diagnosis of Sjogren’s syndrome, scleroderma/MCTD or neither (p = 0.014) and hypomotility pattern (0.024) independently predicted lack of complete pH recovery with PSPW, while number of reflux episodes (p = 0.051) trended toward significance (Table 3).
Discussion
In this retrospective study investigating esophageal clearance of refluxate in patients with impaired saliva production and esophageal hypomotility, we demonstrate that despite similar numbers of reflux episodes and PSPW counts, patients with Sjogren’s syndrome had a lower likelihood of complete pH recovery following PSPW compared to symptomatic GERD patients without this diagnosis. Proportions of PSPW with complete pH recovery was variable between individual patients to a similar degree between scleroderma/MCTD and Sjogren’s syndrome, and both were significantly lower than that in symptomatic patients without these disorders. Since Sjogren’s syndrome is characterized by reduced saliva production and scleroderma/MCTD by significant hypomotility, both adequate saliva and intact motor function appear important for optimal PSPW driven chemical clearance of acid reflux. Both esophageal diagnosis and hypomotility pattern remained independent predictors of lack of complete pH recovery with PSPW, indicating the need for adequate saliva as well as adequate peristaltic performance in PSPW efficacy.
The PSPW has been established as an important metric in evaluating chemical clearance of acid refluxate, with lower proportions of PSPW following reflux episodes (PSPW index) in patients with GERD compared to healthy volunteers [16], particularly in patients with erosive or refractory GERD [17, 21, 22]. Characteristics of reflux episodes that have a higher likelihood of PSPW include reflux while awake, higher extent of reflux migration, and gas content within the refluxate [23]. Further, reflux episodes with PSPW are shorter in duration, and the likelihood of a chance association between reflux and PSPW is < 30% when a 30 s window is utilized [23]. There is wide variability in absolute PSPW counts and the PSPW index in healthy volunteers [7], making identification of a reliable diagnostic threshold challenging to say the least. Thus, PSPW index appears to have broader value in phenotyping GERD rather than in diagnosing GERD [24], and therefore augments the clinical value of pH-impedance monitoring. Since the hypothesis underlying chemical clearance is the arrival of saliva in the distal esophagus via a PSPW, this study was undertaken to determine the relative roles of saliva production (or lack thereof) and esophageal motor function in adequacy of chemical clearance as measured by pH recovery following PSPW.
Sjogren’s syndrome is a systemic autoimmune disease characterized by features of inflammatory destruction of secretory exocrine glands, leading to dryness of mouth and eyes [25,26,27]. Scleroderma is an immune-mediated rheumatologic disease characterized by fibrosis, typically affecting skin, gastrointestinal tract and blood vessels [28]. Within the gastrointestinal tract, esophageal involvement leads to hypomotility of the smooth muscle (often absent contractility), and incompetence of the LES [29,30,31]. Mixed connective tissue disease (MCTD) has overlapping features of systemic sclerosis (a variant of scleroderma), systemic lupus erythematosus, polymyositis/dermatomyositis and rheumatoid arthritis, together with the presence of specific serologic findings [32]. Since the esophagus can be involved in a similar fashion in both MCTD and scleroderma [33], these diagnoses were considered together. Thus, models for lack of saliva and impaired esophageal motility were represented by Sjogren’s syndrome and scleroderma/MCTD, respectively. To our knowledge, this is the first study to assess effectiveness of chemical clearance in patients with impaired saliva production, and in whom rates of hypomotility are high.
Our results demonstrate evidence supporting the hypothesis that PSPW brings saliva to the distal esophagus to neutralize mucosal acidification. Lack of full recovery of distal esophageal acidification with a PSPW was highest with Sjogren’s syndrome, which was an independent predictor of lack of resolution of acidification on multivariable analysis. While poor motor function also appeared to matter, with very low rates of complete pH recovery in the scleroderma/MCTD group, this will need to be interpreted with caution, as both reflux episodes and PSPW are difficult to identify in the extremely low baseline impedance prevalent in scleroderma/MCTD. Thus, we conclude that saliva production is a key determinant of PSPW effectiveness, along with integrity of peristalsis, and lack of saliva as well as esophageal hypomotility compromise pH recovery in the distal esophagus.
Our study suffers from the limitations typically encountered with retrospective studies where protocolized symptom information, therapy and outcomes were not available. We intended for our study to be a pathophysiologic comparison of esophageal mechanisms underlying PSPW efficacy rather than a clinical assessment of symptoms or management. Therefore, presenting symptoms, concurrent medications (including immunosuppressants, opiates, anticholinergics, smooth muscle relaxants and antidepressants) and treatment outcome were not analyzed as part of this study, and we acknowledge that some of these factors could have contributed to the findings. However, patients with concurrent foregut surgery, comorbid esophageal disorders and unconfirmed Sjogren’s syndrome/scleroderma/MCTD were carefully excluded. We utilized a patient cohort without these disorders presenting for evaluation of GERD symptoms within the same study time frame for comparison. Although not a normative population, these patients underwent pH impedance monitoring, which allowed us to make appropriate comparisons in patients without Sjogren’s syndrome or scleroderma/MCTD. Low baseline impedance in the scleroderma/MCTD cohort may have contributed to difficulty in detection of reflux episodes, leading to the low numbers of reflux episodes and PSPW in this cohort. A healthy volunteer cohort would potentially have provided additional perspective on the role of saliva and motor function in PSPW efficacy. Nevertheless, despite these limitations, our results add to the understanding of the esophageal clearance mechanisms in the context of PSPW in a field where similar literature is scarce.
In conclusion, we demonstrate the importance of saliva production in PSPW efficacy, as well as integrity of motor function. There remain gaps in understanding the actual esophago-salivary reflux and specific triggers within reflux episodes that increase the likelihood of this reflex, and further studies are needed.
References
Vakil N, van Zanten SV, Kahrilas P et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006;101:1900–1943.
Gyawali CP, Kahrilas PJ, Savarino E et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018;67:1351–1362.
Gyawali CP, Yadlapati R, Fass R et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut. 2023. https://doi.org/10.1136/gutjnl-2023-330616.
Locke GR 3rd, Talley NJ, Fett SL et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County Minnesota. Gastroenterology 1997;112:1448–1456.
El-Serag HB, Sweet S, Winchester CC et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014;63:871–880.
Tack J, Pandolfino JE. Pathophysiology of Gastroesophageal Reflux Disease. Gastroenterology 2018;154:277–288.
Sifrim D, Roman S, Savarino E et al. Normal values and regional differences in oesophageal impedance-pH metrics: a consensus analysis of impedance-pH studies from around the world. Gut. 2020. https://doi.org/10.1136/gutjnl-2020-322627.
Rogers BD, Valdovinos LR, Crowell MD et al. Number of reflux episodes on pH-impedance monitoring associates with improved symptom outcome and treatment satisfaction in gastro-oesophageal reflux disease (GERD) patients with regurgitation. Gut 2021;70:450–455.
Gyawali CP, Tutuian R, Zerbib F et al. Value of pH Impedance Monitoring While on Twice-Daily Proton Pump Inhibitor Therapy to Identify Need for Escalation of Reflux Management. Gastroenterology 2021;161:1412–1422.
Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med 1997;336:924–932.
Vegesna AK, Sloan JA, Singh B et al. Characterization of the distal esophagus high-pressure zone with manometry, ultrasound and micro-computed tomography. Neurogastroenterol Motil 2013;25(53–60):e6.
Helm JF, Dodds WJ, Pelc LR et al. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med 1984;310:284–288.
Helm JF, Dodds WJ, Riedel DR et al. Determinants of esophageal acid clearance in normal subjects. Gastroenterology 1983;85:607–612.
Sarosiek J, Rourk RM, Piascik R et al. The effect of esophageal mechanical and chemical stimuli on salivary mucin secretion in healthy individuals. Am J Med Sci 1994;308:23–31.
Xu H, Ye B, Ding Y et al. Factors of Reflux Episodes With Post-reflux Swallow-induced Peristaltic Wave in Gastroesophageal Reflux Disease. J Neurogastroenterol Motil 2020;26:378–383.
Frazzoni M, Manta R, Mirante VG et al. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease–a 24-h impedance-pH monitoring assessment. Neurogastroenterol Motil 2013;25:399–406.
Frazzoni M, Bertani H, Manta R et al. Impairment of chemical clearance is relevant to the pathogenesis of refractory reflux oesophagitis. Dig Liver Dis 2014;46:596–602.
Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am 2014;24:527–543.
Yadlapati R, Kahrilas PJ, Fox MR et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil 2021;33:e14058.
Gyawali CP, Rogers B, Frazzoni M et al. Inter-reviewer Variability in Interpretation of pH-Impedance Studies: The Wingate Consensus. Clin Gastroenterol Hepatol 2021;19:1976–1978.
Frazzoni M, Savarino E, de Bortoli N et al. Analyses of the Post-reflux Swallow-induced Peristaltic Wave Index and Nocturnal Baseline Impedance Parameters Increase the Diagnostic Yield of Impedance-pH Monitoring of Patients With Reflux Disease. Clin Gastroenterol Hepatol 2016;14:40–46.
Frazzoni L, Frazzoni M, de Bortoli N, et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterol Motil 2017;29.
Zhang M, Yaman B, Roman S et al. Post-reflux swallow-induced peristaltic wave (PSPW): physiology, triggering factors and role in reflux clearance in healthy subjects. J Gastroenterol 2020;55:1109–1118.
Gyawali CP, Yadlapati R, Fass R, et al. Updates to the modern diagnosis of GERD: Lyon Consensus 2.0. Gut 2023:in press.
Thomas E, Hay EM, Hajeer A et al. Sjogren’s syndrome: a community-based study of prevalence and impact. Br J Rheumatol 1998;37:1069–1076.
Ramos-Casals M, Tzioufas AG, Font J. Primary Sjogren’s syndrome: new clinical and therapeutic concepts. Ann Rheum Dis 2005;64:347–354.
Baldini C, Pepe P, Quartuccio L et al. Primary Sjogren’s syndrome as a multi-organ disease: impact of the serological profile on the clinical presentation of the disease in a large cohort of Italian patients. Rheumatology (Oxford) 2014;53:839–844.
Lepri G, Guiducci S, Bellando-Randone S et al. Evidence for oesophageal and anorectal involvement in very early systemic sclerosis (VEDOSS): report from a single VEDOSS/EUSTAR centre. Ann Rheum Dis 2015;74:124–128.
Denton CP, Khanna D. Systemic sclerosis. Lancet 2017;390:1685–1699.
Crowell MD, Umar SB, Griffing WL et al. Esophageal Motor Abnormalities in Patients With Scleroderma: Heterogeneity, Risk Factors, and Effects on Quality of Life. Clin Gastroenterol Hepatol 2017;15:207–213.
Shreiner AB, Murray C, Denton C et al. Gastrointestinal Manifestations of Systemic Sclerosis. J Scleroderma Relat Disord 2016;1:247–256.
Sharp GC, Irvin WS, Tan EM et al. Mixed connective tissue disease–an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med 1972;52:148–159.
Gutierrez F, Valenzuela JE, Ehresmann GR et al. Esophageal dysfunction in patients with mixed connective tissue diseases and systemic lupus erythematosus. Dig Dis Sci 1982;27:592–597.
Funding
This study was funded in part by the Jewish Heritage Fund for Excellence (BDR).
Author information
Authors and Affiliations
Contributions
Guarantor of the article: CPG. Author roles: LM, TH: data collection, data analysis, manuscript review; BDR: data analysis, manuscript preparation and review; DS, CPG: study concept, data collection and analysis, manuscript preparation and review, and critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LM, TH: no disclosures; BDR: Braintree Labs (consulting); DS: Reckkit Benkiser, UK, Jinshang China (honorarium, research grants); CPG: Consulting: Medtronic, Diversatek; speaking: Carnot.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marchetti, L., Rogers, B.D., Hengehold, T. et al. Saliva Production and Esophageal Motility Influence Esophageal Acid Clearance Related to Post-reflux Swallow-Induced Peristaltic Wave. Dig Dis Sci 69, 1714–1721 (2024). https://doi.org/10.1007/s10620-024-08315-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08315-x